Respiratory Lab #2 &3 (please print out)
advertisement
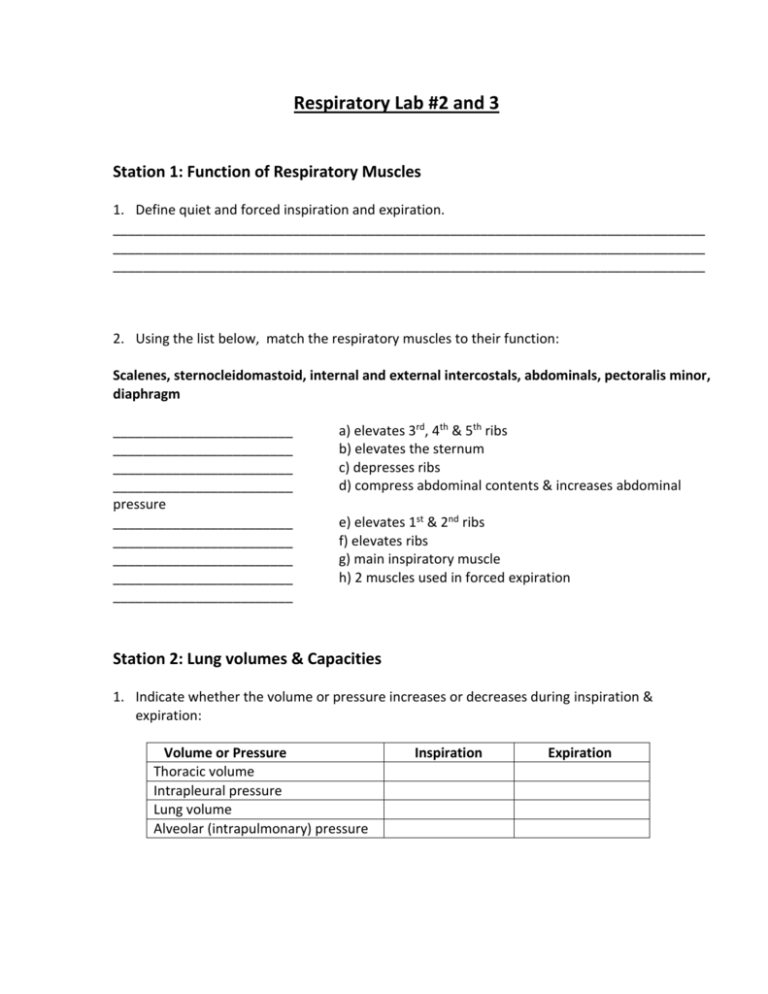
Respiratory Lab #2 and 3 Station 1: Function of Respiratory Muscles 1. Define quiet and forced inspiration and expiration. _______________________________________________________________________________ _______________________________________________________________________________ _______________________________________________________________________________ 2. Using the list below, match the respiratory muscles to their function: Scalenes, sternocleidomastoid, internal and external intercostals, abdominals, pectoralis minor, diaphragm ________________________ ________________________ ________________________ ________________________ pressure ________________________ ________________________ ________________________ ________________________ ________________________ a) elevates 3rd, 4th & 5th ribs b) elevates the sternum c) depresses ribs d) compress abdominal contents & increases abdominal e) elevates 1st & 2nd ribs f) elevates ribs g) main inspiratory muscle h) 2 muscles used in forced expiration Station 2: Lung volumes & Capacities 1. Indicate whether the volume or pressure increases or decreases during inspiration & expiration: Volume or Pressure Thoracic volume Intrapleural pressure Lung volume Alveolar (intrapulmonary) pressure Inspiration Expiration 2. Using list below, match lung volumes & capacities with the appropriate definition or equation: Total lung capacity. Residual volume, inspiratory capacity, expiratory reserve volume, vital capacity, functional residual capacity, inspiratory reserve volume, tidal volume ________________________ ________________________ ________________________ ________________________ ________________________ a) the volume of air inhaled and exhaled per breath b) = RV + ERV c) = TV + IRV + ERV d) volume of air remaining in lungs after normal expiration e) maximum amt of air that can be exhaled after a normal expiration ________________________ f) maximum amt of air that can be exhaled after a maximal inspiration ________________________ g) = VC + RV ________________________ h) volume of air that can be exhaled in 1 sec with maximal effort following a maximal inhalation Station 3 Label the following diagrams Hint for the diagrams –Look the “airway” presentation on your course (a and P) web page under “extras” Station 4 Do the two chart exercises attached. Look at the differences between inspiration and expiration. What are the driving forces behind these two processes. How would this differ when YOU re ventilating a patient. i.e what is meant by “Positive pressure ventilation” Station 5 Using the respiratory lab materials a) Using a clean and disinfected mouthpiece, Measure your tidal volume (Vt) and fill out your Tv on the chart provided. Look at the variety of Vt’s in the class. Clean the mouthpieces with alcohol once you are done! Let dry b) c) What is your FEV? Over what time period is it measured in? Measure resting breath rate and active breath rate. Put it on the chart provided d) Now, since you know your Tv, and RR (at rest) what is your minute ventilation? How does this change during exercise. d) What is meant by “ breath control”. When would it be useful? Try the breath control exercise – please clean well with alcohol after use Station 6 Fill in the following chart Station 7 Label the following diagram Station 8 Checkpoints B9 Write the correct term next to each description. (a) Inflammation of the pleura: _________ (b) Excess fluid in the pleural space: _________ (c) Procedure to remove fluid from the pleural space: _________ (d) Air in the pleural space: _________ (e) Collapse of a lung, possibly due to pneumothorax or hemothorax: _________ C1 (a) Label the first phase of respiration at (1) on the figure. This process involves transfer of air from your environment to (alveoli? pulmonary capillaries?) in your lungs. Inflow of air rich in (O2? CO2?) is known as _________ -halation (inspiration), whereas outflow of air concentrated in (O2? CO2?) is known as _________ -halation (expiration). (b) Phase 2 of respiration involves exchange of gases between _________ in alveoli and _________ in pulmonary capillaries. This process is known as (external? internal?) respiration (or diffusion). Label phase 2 on the figure. (c) After oxygenated blood returns to your heart via your pulmonary (artery? veins?), blood is pumped to your tissues where gas exchange occurs between _________ and _________ . This process is known as (external? internal?) respiration. Label phase 3 on the figure. (d) Blood high in CO2, then returns to the heart where it passes directly into the pulmonary (artery? vein?) to reach the lungs. Here diffusion of CO2 from pulmonary capillaries to alveoli occurs; this is another effect of (external? internal?) respiration (phase _________ ). Finally, you exhale this air, a process that is part of (external respiration? pulmonary ventilation?) (phase _________ ). (e) Which process takes place within tissue cells, utilizing O2 and producing CO2 as a waste product? (Cellular? Internal?) respiration. Checkpoint 2 (a) In diagram (a), just before the start of inspiration, pressure within the lungs (called _________ ) is _________ mm Hg. This is (more than? less than? the same as?) atmospheric pressure at sea level. (b) At the same time, pressure within the pleural cavity (called _________ pressure) is _________ mm Hg. This is (more than? less than? the same as?) alveolar and atmospheric pressure at sea level. (c) The first step in inhalation occurs as the muscles in the floor and walls of the thorax contract. These are the _________ and _________ muscles. Note that the size of the thorax (increases? decreases?). Because the two layers of pleura tend to adhere to one another, the lungs will (increase? decrease?) in size also. (d) Increase in volume of a closed space such as the pleural cavity causes the pressure there to (increase? decrease?) to _________ mm Hg. Because the lungs also increase in size (due to pleural cohesion), alveolar pressure also (increases? decreases?) to _________ mm Hg. This inverse relationship between volume and pressure is a statement of _________ 's law. (e) A pressure gradient is now established. Air flows from high pressure area (alveoli? atmosphere?) to low pressure area (alveoli? atmosphere?). So air flows (into? out of?) lungs. Thus (inhalation? exhalation?) occurs. By the end of inhalation, sufficient air will have moved into the lungs to make pressure there equal to atmospheric pressure, that is, _________ mmHg. (f) Inhalation is a(n) (active? passive?) process, whereas exhalation is normally a(n) (active? passive?) process resulting from _________ recoil. Identify two factors that contribute to this recoil. During exhalation, the diaphragm moves (inf? sup?)-eriorly and the sternum moves (ant? post?)-eriorly. (g) During labored breathing, accessory muscles help to force air out. Name two of these sets of muscles. C8Of the total amount of air that enters the lungs with each breath, about (99%? 70%? 30%? 5%?) actually enters the alveoli. The remaining amount of air is much like the last portion of a crowd trying to rush into a store: it does not succeed in entering the alveoli during an inhalation but just reaches airways and then is quickly ushered out during the next exhalation. Such air is known as anatomic _________ and constitutes about _________ mL of a typical breath. C9 Maureen, who weighs 150 pounds, is breathing at the rate of 15 breaths/minute. Her tidal volume is 480 mL/breath. Her minute ventilation is _________ mL. Her alveolar ventilation rate is likely to be about _________ mL/mm.