Cross Contamination Article
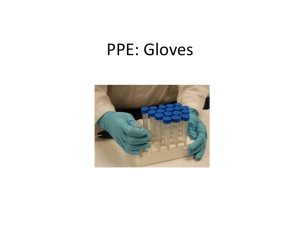
advertisement
Features - Business Management [Employee Training] Cross Contamination 10/8/2008 QA managers must teach employees not only how their actions prevent food contamination, but also why each is important. “I don’t need to wash my hands, I wear gloves.” “The line is clean enough; the food doesn’t touch the other areas anyway.” “I’m not that sick….” “We need our workers out on the floor, not in a training room.” If you’ve ever heard these or similar comments from your employees — or managers — you should consider taking an in-depth, objective look at the food safety and training practices in your plant. Plants need to focus not only on if and how their practices prevent food contamination, but also on whether their employees understand why each is important. WHY? If nothing else has caused your management team to take a detailed look at the potential points of cross contamination in your plant, consider the recent Listeria monocytogenes contamination at the Maple Leaf Foods meat plant in Toronto, where plant equipment has been implicated as the likely cause. Despite rigorous, daily sanitization of the equipment following or exceeding manufacturer recommendations, “upon full disassembly, areas were found where bacteria may accumulate deep inside the slicing machines and avoid the sanitization process,” said company president and CEO Michael McCain. As a result of the outbreak, to which Canadian health officials had linked 49 cases of listeriosis and 19 confirmed deaths as of this writing, Maple Leaf shut down operations at its Toronto plant and recalled all products made at that plant since Jan. 1. After six intensive plant sanitizations and complete disassembly, deep cleaning and multiple testings of the implicated slicing equipment, the plant reopened Sept. 17. However, the fact that the extensive outbreak occurred despite Maple Leaf’s “rigorous sanitation” practices should put all plants on alert that focused sanitation, inspection and training can never be too rigorous when one considers all possible points of contamination and the impacts of an outbreak. Suzanne Driessen, a food science educator for the University of Minnesota Extension, promotes self inspection in plants, with the specific goal of observing what employees are actually doing on the floor and whether food safety practices are being followed. “If you take the time to walk and observe what people are doing,” Driessen said, “you can identify those training gaps.” Observe what is really happening, how — and if — your employees are implementing plant practices on a regular basis, she said. It can be even more beneficial to trade routes with a member from another department — walk each other’s areas and see what you discover. “Sometimes people are just too close to it. If you get a person from another department or division to (walk) it, you will get a fresh perspective.” THE HUMAN ELEMENT. In her inspections, Minnesota Department of Agriculture Food Inspector III Jan Kelly sees that “the human element is often overlooked,” she said. Person-to-food contamination is of primary concern, with viral pathogens, such as Norovirus, recognized as causing more than half of all food-borne illness. In such situations, Kelly said, there are three preventive opportunities that are generally missed: Employee illness — even if an employee does not come to work when his symptoms are active, he could be carrying the viral germs for some time afterward. Handwashing — viral pathogens can be transferred from humans not only directly to foods or food-contact surfaces, but across non-food-contact surfaces, such as door handles or to another person who then contacts the food or food-contact surface. Gloves — as Kelly graphically relates to employees, “Gloves are a barrier between poopy fingers and the food.” Being blunt with the information, she explained, can have more impact and better hold employees’ attention. TRAINING. “The training part of it is the greatest issue,” Kelly said. “I think a lot of places do training, but how effective is the training?” Not only must education for employees cover the topic being trained, it also needs to be specific to the employees’ job duties, be conducted in such a way as to meet people’s various learning styles and include follow-through. People learn in different ways, Kelly said. Some learn best through visual training, others through auditory or kinesthetic (hands on) methods. To be most effective for the most employees, training should include multiple methods which address each of the learning styles. Follow-through on the training is just as important as the initial education. Kelly said she often finds among her own staff that people who have been trained in an area forget certain skills if there is no additional follow-through or retraining. ASK WHY. Driessen said that when you find that safe-food procedures are being neglected, you need to find out why. Employees may have been trained initially in a practice but have since forgotten it, or they may simply have never learned how to best implement a practice, such as line cleaning or even hand washing. “Let’s not just assume that people know how,” she said. “Sometimes we forget to tell them how, and we expect them to do it the way we want.” It also is beneficial to ask employees why they are doing what they’re doing. An employee may not realize that the action has an impact on food safety, “We know that knowing and doing are two different things,” Driessen said. “We need to know if (the employee) really believes it is a risky behavior.” Another employee may enact a certain behavior as a carryover from his or her culture or home life. “It’s easy to tell someone what to do, but it’s difficult to change lifelong habits,” Driessen said. Once you know why something is happening, corrective action should include discussion of — and training or retraining on — what the proper method is for the procedure, as well as why it is important, and why the employee’s current method causes food-safety risks. “Take time to do that and you will save time in the long run,” Driessen said. “Too often, we just talk about the what.” CONCLUSION. Buy-in on the training from both employees and upper management is also critical for success. For employees, training should be positioned as a part of continuing education for the job, not as punishment for wrongdoing, Driessen added. And upper management — who hold the financial strings — need to understand that successful training will sometimes involve taking people from the floor to the classroom. “Having a realistic plan and clear objective of what you want to accomplish will help you get the budget and management support,” she said. “Yes, it will take people off the floor, but you have to do that if you want to do it right.” The author is staff editor of QA magazine. Employee Knowledge and Practices It may come as no surprise that workers who prepare food while experiencing gastrointestinal (GI) symptoms are frequently linked to food-borne illness outbreaks. What may be a bit more alarming is that 61 percent of workers who experience GI symptoms do not request time off from work, but continue to come in — and work with food. This statistic was among the findings of a 2007 study conducted by the Partnership and Workforce Development Unit of the Minnesota Department of Health in St. Paul, Minn. The study focused primarily on foodservice workers, but food manufacturers should take the findings into account in assessing the rationale and motivation of their own food workers. The study included two parts: a survey of 350 restaurant workers and focus groups conducted in English and Spanish. To estimate the prevalence of food-borne disease symptoms in workers and the likelihood that they would work with symptoms, workers completed a brief questionnaire asking if they or family members had experienced nausea, vomiting, diarrhea or fever in the last two weeks. Symptomatic workers were asked if they had requested time off because of their symptoms. Of those who responded: 19 percent had at least one food-borne disease symptom. 7 percent reported that household members were also ill. 39 percent of symptomatic workers requested time-off. CONCLUSIONS. Discussions were held to assess food worker knowledge of food-borne disease transmission, the role of the worker in its spread, barriers to recognizing and reporting symptoms and best strategy for education on the topics. The findings showed a: reluctance to stay home from work with mild gastrointestinal symptoms. lack of management support for workers who call in to report illness. lack of awareness of food code provisions related to employee health. need for diverse educational methods and strategies. Answering the Why 1. Why wash your hands before putting on gloves? When putting on gloves, a worker touches numerous surfaces that can be contaminated by unclean hands, and lead to contamination of food. Ungloved hands must pull single-use gloves from the box — at which point pathogens from unclean hands can be transferred to the box itself, contaminating each successive glove; hands then carry the gloves, potentially contaminating the surface being held; then the hands pull on the gloves, further transferring pathogens to more points of the glove. With the gloved hands then used to touch foods and food-contact surfaces, transferred pathogens can pass directly to the foods. 2. Why break down and thoroughly clean and sanitize all equipment regularly? As the Maple Leaf Foods situation exemplifies, pathogens can transfer even from hidden cracks and crevices. In addition, accumulated debris can attract pests, which carry their own range of food-borne disease bacteria. 3. Why wash your hands before sanitizing them? Hand washing is particularly important when a person is working with food as the scrubbing and friction of washing is needed to remove proteins and oils. “You have to have clean hands before you put on sanitizer,” said Suzanne Driessen, a food science educator for the University of Minnesota Extension. “Sanitizing never replaces hand washing.” 4. Why not cross from raw to prepared meat areas? “Bacteria is everywhere and can transfer very easily,” Driessen said. Not only can bacteria transfer from hands or gloves, but they can get on an apron or sleeve. Because pathogens often can’t be seen, a worker who does not realize he is carrying a contaminant can inadvertently rub against a clean surface and transfer the pathogen. Since food manufacturing plants have such a busy atmosphere, food-borne illness prevention must always be top of mind. 5. Why not come in to work if you are ill? Norovirus affects the stomach and intestines, causing flu-like symptoms. Highly contagious, Norovirus is easily spread by direct person-to-person contact, eating food touched by an infected person, touching a surface containing the virus or through contaminated food. According to the Minnesota Department of Health, Norovirus has caused more than half the food-borne illness outbreaks in the state for the past 20 years, and the Centers for Disease Control and Prevention considers it the leading cause of food-borne illness in the United States. By: Lisa Lupo