Jul 19, 2010 - School of Medicine
advertisement

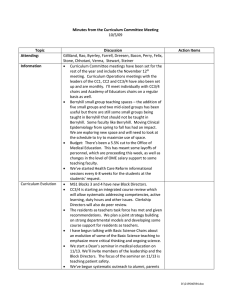
Minutes from the Curriculum Committee Meeting 7/19/10 Topic Attending: Minutes Information Items Discussion Bacon, Bynum, Colford (guest), Cross, Dreesen, Gilliland, Newton, Serra, Shaheen , Stone, Wood; by phone: Felix, Fields, White Minutes were reviewed. The only significant addition from the first draft was inclusion of the discussion around standards for Honors – 25%, not more than 35% with a review of data regularly during the year. Please see agenda. Points of emphasis include: Action Items Consent Agenda Kurt Gilliland has been appointed as Interim Director of Curriculum. He’ll be working on improving small group teaching effectiveness, improving quality of examinations and a teaching certificate. The Asheville shelf exams have come out and the students have done quite well. The numbers are small but in aggregate, they had tested at approximately 2530th percentile of UNC students on Step I and at the end of their third year tested well above average for UNC students – a greater than expected jump. While the numbers are too small to be definitive, it is certainly reassuring. Conference room Scheduling – We are trying to develop a systematic solution for conference rooms across the school. The LCME Task Force is being set up. The kick off and charge will be August 24th – 7:30-8:30am with a LCME consultant to kick off the subcommittees on September 17th . An announcement will come out. A couple of comments in the aggregate: 1. Peer review system developed in the third year, CC3/4 is very positive; will be extending this to CC1 and CC2 in the next year. 2. Occasional comments about “threatening” in transition and in Surgery. What does this mean? Where does it go? The comments in the Transition course were actually quite rare. In Surgery, it may be valuable to bring up again to GME and other settings. We have in place a super structure including the new undergraduate medical directors which we’ll be adding to this in this coming year. We’ll review all of this plus the Document1 latest data on mistreatment on an annual basis. Core Competencies Tracking Curricular Outcomes The first draft of the milestones were reviewed. We’ve established overarching and enabling competencies. Now, we want to focus on the transitions and year by year outcomes. Issues raised included: 1. In general, the committee reaffirmed pushing as much clinical reasoning into the first and second year as possible. This needs to be made more consistent across competencies. An example is procedures – of which perhaps, more should be done in the first year and which later. 2. A second issue is Pediatrics. Again, the committee affirmed the sense that as much can be done with first and second years as possible but the logistics might be appropriate. It’s difficult to get competence in all aspects of the physical examination and clinical examination of children but the more the better: this would allow further development in the clinical clerkship. Cam mentioned that other schools had used family physicians for this also. 3. Question: There are huge holes in the curriculum – human development, population management. How will those be dealt with? Indeed, this is the process by which we identify and fill huge holes. The overall timeframe is that once we establish what we think students at the end of each year should know, then each year we will review the core competencies and say what they can and can’t do – what courses are doing and what needs to be different. Finding the gaps will be critical. 4. As a general comment, many of the competencies use the same language to get from 3 to 4 without a sense of the progression of the skills. This program needs to be explicit. In some cases, it can be reframed in terms of kind of patients. Review the draft email. General points were made: 1. We need to think about what metrics we need to use in order to evaluate particular outcomes at the curriculum and student level. 2. In addition, we need to talk about the process and the infrastructure necessary. 3. We need to be careful about building too much infrastructure. We need to be pragmatic about what we do. The committee will give specific line by line feedback to Cam and Lisa by the end of the week. They will revise and bring to the Curriculum Committees for their input over the course of the month of August. Then, we’ll revise and in this group and review in advance of the discussion in September. Newton will send out the email asking for volunteers to participate in the curriculum outcomes session, have a single meeting and then report back at the retreat. Document1 Improving Comparability Across Sites Introduction to Clinical Medicine 4. At the same time, much of what we do in terms of competencies isn’t really targeted on competencies. We can improve the efficiency of the process. Please see summary. This represents a collection of various policy items that we’ve put in place to underscore comparability across sites. The only addition at this point is incorporation of the Campus Directors in Charlotte and Asheville on this group, which affects a LCME standard. Deb Bynum and Cristin Colford presented briefly what they are trying to do. Comments included: 1. Wonderful to open up tutors broadly – impressive that there are many people who want to do this course; we need to figure out a way of incorporating Obstetricians and Pediatricians into it in some way. 2. Students reported that they very much appreciated putting more clinical skills including chest x-rays and EKGs into the first year and that better integration within the ICM blocks is desirable. 3. It’s important to try to push smaller groups and experiments in next year. 4. Better integration of community weeks if possible. The group encouraged new thinking about community weeks, both in better integration of other first year materials but also whether or not they are accomplishing the purpose. A major challenge is the variability; the added value is the continuity of teaching and some of the individual settings. 5. Another issue is the opportunity for actual clinical experience in the first two years. It’s quite variable according to ICM. In some of the tutor groups, there isn’t enough direct clinical experience. 6. For the next year, ICM will use the current title and will be changing the name in 2011-2012 as they pilot other pieces. There was broad consensus that all of these were appropriate. Newton will invite White and Heck to participate in the Curriculum Committee and set up the technical support for doing that. They’ve already been invited to the Curriculum Retreat in September. The Curriculum Committee endorsed the general direction of the new course leaders for ICM – including the standardization approach of recruiting and hiring tutors, the general direction of getting more clinical reasoning in the first year and many of the pilots. The committee supported more sweeping redesign of the course including smaller group size and seeing what is possible with ongoing clinical work. The course will bring the proposal back for further input from the Curriculum Committee in the early fall. Document1 MD-PhD Changes Newton and Shaheen gave context for the specific proposal. This represents the last piece of a series of changes in the curriculum designed to improve the quality of the MD-PhD curriculum as well as shorten the overall program. The proposal acknowledges that the MD-PhD program satisfies the Integration Selective. The current proposal is a new mechanism for a longitudinal clerkship, patterned on the successful experience at Asheville, in which students will continue to have clinical experience during their MD-PhD program. The initial 40 week segment will take the place of the APS. Students can also get ongoing additional credit for 40 weeks at a time. The 40 week rotations like other clinical rotations will have evaluation of clinical skills and mid-course feedback. The committee voted unanimously to support the current proposals with the added proviso of limiting the number of lecture credits that can be fulfilled. In addition, we will try to make available clerkships right before graduate school starts. The committee was supportive of these changes. Remediation There are capacity limitations in the summer. It is important to maintain breadth while students are in the MD-PhD program (i.e., no more than the APS being fulfilled by working with the MD-PhD mentor). The Office of Medical Education has engaged Arrel Toews, Teacher of the Year from last year, to help with two specific issues: 1) remediation with students failing a course and 2) the development of common basic science teachers. We’d like input and guidance about directions of putting this in place. Several people have observed that a challenge in the first two years is that the individual course directors may feel hesitant about failing somebody giving the complexity of what remediation is. The goal is for Arrel to work with individual course directors and the year directors to develop a system. The goal is not to replace the early warning and tracking process; in addition, this is complementary to the discussion about standards for failure in the first and second years. Nevertheless, we need to pull together the area of activities into a more consistent process. Kurt and Arrel will work with CC1, CC2, Debbie Ingersoll and others to clarify the issues and develop consensus about a comprehensive plan around remediation. Comments on this issue included: There’s a strong sense that this was indeed a problem and this is in part because of the variation in what Document1 Common Basic Science Teachers Berryhill Curriculum Retreat people do. Lecture Capture is new and may make remediation easier technically and a little bit different. We also will need to personalize. Some students have a particular area of weakness that needs remediation – this is the basis for some conditional grades. Others are skimming along at the borderline level throughout the course. It will be valuable to get Al Parker’s perspective on this from promotion. Another barrier here is the stigma associated with failure. There will be some value of facilitating the process. The tone of the interaction with the Block Directors is important. It needs to be helping them rather than imposing it at the Dean’s level. Focus should be competency, not punishing the students. It’s important to set consistent standards for remediation across courses. One element of this might be what kinds of exams we’re going to use and the like. Brief discussion – there was unanimous support among the Curriculum Committee for trying to develop core basic science teachers across disciplines. There is a question of how broadly people can teach – using a visible spectrum analogy, some people will be able to do red, yellow and orange and others will be at the other end of the spectrum but more breadth is possible. TBL emphasizes facilitation of information, not just personal knowledge. Space continues. We will continue to push for improvements and space. The biggest issue is getting appropriate space for clinical exams. The retreat will be on September 3rd. We will be focusing heavily on outcomes data and the curriculum competencies. Newton will be following up with the Basic Science Chairs in September. The trick will be to come up with a financial mechanism that they will endorse. Document1