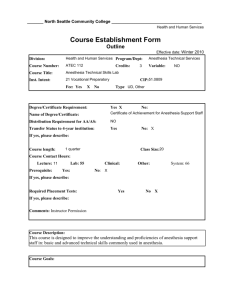
the anesthesia gas machine revsed july 2012
advertisement

Page 1 [Type text] Abbrevition : Page 2 APL adjestable pressure limiting AGM anesthesia Generic machines ANSI american national standards institute AST american society for testing and materials BC before critsmas CGO common gases outlet CMV controll –mode ventilation DISS diameter index safety system ETT endo tracheal tube OSHA occupational safty and health adminestration OFFD oxygen failure protection device ORMC oxygen ratio monitor controller PISS pin index safety system PCV pressure controlled ventilation PSV pressure support ventilation PSIG pound /square inch gauge SIMV synchronized intermitant mandatory ventilation TWA time weighted average WAGS waste anesthesia gases NIOSH national institute for occupational safty and health PPM parts per million FSV fail safe valve MAC minimal alveoler concentration [Type text] . Contents: Chater 1 anesthesia and history ……………………..…….8 How is anesthesia …………………………………………...….........8 Types ofanesthesia ………………………………………...…………8 History of anesthesia …………………………………… ……. .……8 Complication of general anesthesia ……………………................12 Chapter 2 anesthesia machines ………………………....…14 History of anesthesia machines …………………………………..…14 Introduction ………………………………………………………...…15 Generic anesthesia machines ……………………………………....17 Pipeline supply………………………………………………………...22 Cylinder supply source ……………………………………..……..…23 Flow meter assemblies…………………………………………….…27 Oxygen flush valve……………………………………………………31 Chapter 3 vaporizer……………………………….……………..33 Introduction ……………………………………………………………33 Physical principles ……………………………………………………33 Factors influencing vaporizer output……………………………..…35 Current models……………………………………………………...…41 Chpter 4 anesthetic circuits …………………..………………45 Mapleson systems………………………………………..……………45 Bain circuit ……………………………………………………..………46 Chapter 5 carbon dioxide absorption………..………….… 48 Absorber canister …………………………………………………..….48 Chemistry of absorbents………………………………………..….….49 Page 3 [Type text] Absorptive capacity ………………………………………………....…50 Intractions of inhaled anesthetics with absorbents ………………... 50 Chapter 6 ventilators…………….…………………………...…...53 Classification …………………………………………………….……53 Typical ventilator alarms ………………………………..…………….58 New features of modern ventilators ……………………….…………58 Compliance and leak testing …………………………………….……61 Current models …………………………………………………………64 Chapter 7 scavenging and waste anesthetic gases …...68 Definition …………………………………………………………..……68 Types ……………………………………………………………….……68 Components of the scavenger system ……………………………….69 Hazards of scavenging …………………………………………….…..70 Controlling occuptional exposure to waste anesthetic gases……... 70 Appendix ………………………………………………………………71 Summary ………………………………………………………………73 Key point ………………………………………………………………73 Ref ……………………………………….…………………………………………………75 Page 4 [Type text] Chapter 1 : anesthesia and history How is anesthesia Anesthesia, or anaesthesia (from Greek , an-, "without"; and aisthēsis, "sensation"), traditionally meant the condition of having sensation (including the feeling of pain) blocked or temporarily taken away. It is a pharmacologically induced and reversible state of amnesia, analgesia, loss of responsiveness, loss of skeletal muscle reflexes or decreased stress response, or all simultaneously. These effects can be obtained from a single drug which alone provides the correct combination of effects, or occasionally a combination of drugs (such as hypnotics, sedatives, paralytics and analgesics) to achieve very specific combinations of results. This allows patients to undergo surgery and other procedures without the distress and pain they would otherwise experience. An alternative definition is a "reversible lack of awareness," including a total lack of awareness (e.g. a general anesthetic) or a lack of of awareness of a part of the body such as a spinal anesthetic. The pre-existing word anesthesia was suggested by Oliver Wendell Holmes, Sr. in 1846 as a word to use to describe this state. Types of anesthesia Types of anesthesia include local anesthesia, regional anesthesia, general anesthesia, and dissociative anesthesia. Local anesthesia inhibits sensory perception within a specific location on the body, such as a tooth or the urinary bladder. Regional anesthesia renders a larger area of the body insensate by blocking transmission of nerve impulses between a part of the body and the spinal cord. Two frequently used types of regional anesthesia are spinal anesthesia and epidural anesthesia. General anesthesia refers to inhibition of sensory, motor and sympathetic nerve transmission at the level of the brain, resulting in unconsciousness and lack of sensation. Dissociative anesthesia uses agents that inhibit transmission of nerve impulses between higher centers of the brain (such as the cerebral cortex) and the lower centers, such as those found within the limbic system. History of anesthesia Page 5 [Type text] Attempts at producing a state of general anesthesia can be traced throughout recorded history in the writings of the. ancient Sumerians, Babylonians, Assyrians, Egyptians,Greeks, Romans, Indians, and Chinese. During the Middle Ages, which correspond roughly to what is sometimes referred to as, the Islamic Golden Age, scientists and other scholars made significant advances in science and medicine in the Muslim world and Eastern world, while their European counterparts also made important advance. The first attempts at general anesthesia were probably herbal remedies administered in prehistory. Alcohol is the oldest known sedative; it was used in ancient Mesopotamia thousands of years ago. (fig 1-1 ) Re-enactment of the first public demonstration of general anesthesia byWilliam T. G. Morton on October 16, 1846 in the Ether Dome at Massachusetts General Hospital, Boston. Surgeons John Collins Warren and Henry Jacob Bigelow are included in this daguerrotype by Southworth & Hawes. OP I UM (Fig 1 -2) Opium poppy, Papaver somniferum It has long been written that the Sumerians cultivated and harvested the opium poppy (Papaver somniferum)( fig 1-2 ) in lower Mesopotamia as early as 3400 BC, though this has been Page 6 [Type text] disputed. The most ancient testimony concerning the opium poppy found to date was inscribed in cuneiform script on a small white clay tablet at the end of the third millennium BC. This tablet was discovered in 1954 during excavations at Nippur, and is currently kept at the University of Pennsylvania Museum of Archaeology and Anthropology. Deciphered bySamuel Noah Kramer and Martin Leve, it is considered to be the most ancientpharmacopoeia in existence. Some Sumerian tablets of this era have an ideograminscribed upon them, "hul gil", which translates to "plant of joy", believed by some authors to refer to opium. The term gil is still used for opium in certain parts of the world. The Sumerian goddess Nidaba is often depicted with poppies growing out of her shoulders. Bian Que (Chinese) was a legendary Chineseinternist and surgeon who reportedly used general anesthesia for surgical procedures. It is recorded in the Book of Master Han Fei the Records of the Grand Historian and the Book of Master Lie that Bian Que gave two men, named "Lu" and "Chao", a toxic drink which rendered them unconscious for three days, during which time he performed a gastrostomy upon them. Hua Tuo (Chinese)Fig 1-3) was a Chinese surgeon of the 2nd century AD. According to the Records of Three Kingdoms and the Book of the Later Han Hua Tuo performed surgery under general anesthesia using a formula he had developed by mixing wine with a mixture of herbal extracts he called mafeisan Hua Tuo reportedly used mafeisan to perform even major operations such as resection ofgangrenous intestines. Before the surgery, he administered an oral anestheticpotion, probably dissolved in wine, in order to induce a state of unconsciousness and partialneuromuscular blockade. (Fig1-3 )Hua Tuo, Chinese surgeon, c. AD 200 Others have suggested the potion may have also contained hashish, bhang, shang-luh, or opium. Victor H. Mair wrote thatmafei "appears to be a transcription of some IndoEuropean word related to "morphine". Some authors believe that Hua Tuo may have discovered surgical analgesia by acupuncture, and that mafeisan either had nothing to do with or was simply an adjunct to his strategy for anesthesia. Many physicians have attempted to re-create the same formulation based on historical records but none have achieved the same clinical efficacy as Hua Tuo's. In any event, Hua Tuo's formula did not appear to be effective for major operations. Other substances used from antiquity for anesthetic purposes include extracts of juniper and coca. Arabic and Persian physicians may have been among the first to utilize oral as well as inhaled anesthetics. Ferdowsi (940–1020) was aPersian poet who lived in the Abbasid Caliphate. In Shahnameh, his national epic poem, Ferdowsi described a caesarean sectionperformed Page 7 [Type text] on Rudaba A special wine prepared by a Zoroastrian priest was used as an anesthetic for this operation. Although Shahnameh is fictional, the passage nevertheless supports the idea that general anesthesia had at least been described inancient Persia, even if not successfully implemented. The European Renaissance saw significant advances in anatomy and surgical technique. However, despite all this progress, surgery remained a treatment of last resort. Largely because of the associated pain, many patients with surgical disorders chose certain death rather than undergo surgery. Although there has been a great deal of debate as to who deserves the most credit for the discovery of general anesthesia, it is generally agreed that certain scientific discoveries in the late 18th and early 19th centuries were critical to the eventual introduction and development of modern anesthetic techniques. Two "quantum leaps" occurred in the late 19th century, which together allowed the transition to modern surgery. An appreciation of the germ theory of disease led rapidly to the development and application of antiseptic techniques in surgery. Antisepsis, which soon gave way to asepsis, reduced the overall morbidity and mortality of surgery to a far more acceptable rate than in previous eras. Concurrent with these developments were the significant advances in pharmacology andphysiology which led to the development of general anesthesia and the control of pain. In the 20th century, the safety and efficacy of general anesthesia was improved by the routine use of tracheal intubation and other advanced airway management techniques. Significant advances in monitoring and new anesthetic agents with improvedpharmacokinetic and pharmacodynamic characteristics also contributed to this trend. Finally, standardized training programs foranesthesiologists and nurse anesthetists emerged during this period. (1783–1841) first isolated morphine from opium in 1804 he named it morphin after Friedrich Sertürner Morpheus, the Greek god of dream. (1733–1804) was an English polymath who discovered nitrouspoxide, nitric Joseph Priestley oxide, ammonia, hydrogen chloride and (along with Carl Wilhelm Scheele and Antoine Lavoisier) oxygen. On 30 March 1842, he administered diethyl ether by inhalation to a man named James Venable, in order to remove a tumor from the man's neck. Long later removed a second tumor from Venable, again under ether anesthesia. He went on to employ ether as a general anesthetic for limb amputations and parturiti. On 10 December 1844, Gardner Quincy Colton held a public demonstration of nitrous oxide in Hartford, Connecticut. One of the participants, Samuel A. Cooley, sustained a significant injury to his leg while under the influence of nitrous oxide. On october 16 , 1846 using a hastily devised glass reservior incorporating the drawover principle of vaporization . morton anasthetized edward gilbert abbott a young printer while warren deftly ligateda congelital venous malformation in the left cervical triangle (Fig 1-1) without noticing the injury. Horace Wells, a Connecticut dentist present in the audience that day, immediately seized upon the significance of this apparent analgesic effect of nitrous oxide. In 1847, Scottish obstetrician James Young Simpson (1811–1870) of Edinburgh was the first to use chloroform as a general anesthetic. The use of chloroform anesthesia expanded rapidly thereafter in Europe. Chloroform began to replace ether as an anesthetic in the United States at the beginning of the 20th century, It was soon abandoned in favor of ether when its hepatic and cardiac toxicity, especially its tendency to cause potentially fatalcardiac dysrhythmias, became apparent. In 1902, Hermann Emil Fischer (1852–1919) and Joseph von Mering (1849– 1908) discovered that diethylbarbituric acid was an effective hypnotic agent. In 1913, Chevalier Jackson (1865–1958) was the first to report a high rate of success fo r the use of direct laryngoscopy as a means to intubate the trachea . Page 8 [Type text] Theory of the mechanism of anesthesia Although scientists are not sure exactly how anesthesia works, there are many theories that have been proposed. In addition, different anesthetics may have different mechanisms of action. One theory proposes a relationship between the solubility of the anesthetic agent into the fat cells of the body (lipid solubility) as determining the degree of its potency as an anesthetic agent. Induction of anesthesia Administration of the anesthetic is usually accomplished by the insertion of a cannula (small tube) into a vein. Sometimes a gas anesthetic may be introduced through a mask. If a muscle relaxant is used, the patient may not be able to breathe on his own, and a breathing tube is passed into the windpipe (trachea). The tube then serves either to deliver the anesthetic gases or to ventilate (oxygenate) the lungs. During the course of the surgery, the anesthesiologist maintains the level of anesthetic needed to keep up the patient's level of anesthesia to the necessary state of unawareness while monitoring vital functions, such as heart beat, breathing, and blood/gas exchange. . COMPLICATIONS OF GENERAL ANESTHES There are a number of possible complications that can occur under general anesthesia. They include loss of blood pressure, irregular heart beat, heart attack, vomiting and then inhaling the vomit into the lungs, coma, and death. Although mishaps do occur, the chance of a serious complication is extremely low. Avoidance of complications depends on a recognition of the condition of the patient before the operation, the choice of the appropriate anesthetic procedure, and the nature of the surgery itself. Page 9 [Type text] List of drugs used for General Anesthesia Halothane Halothane is an inhalational general anesthetic, prescribed for the induction and maintenance of general anesthesia.... Trade Names :Fluothane Fluothane (200 ml) Fluothane (250 ml) Fluothane (30 ml) Succinylcholine Succinylcholine is a depolarizing muscle relaxant, induction and maintenance of general anesthesia by relaxing muscles.... Trade Names Succin Succinyl Choline Chloirde Succinyl Choline Chloride Sucol Propofol Propofol is a general anesthetic, prescribed for induction and maintenance of general anaesthesia.... Trade Names Celofol Celofol (20 ml) Critifol Critifol (20 ml) Critifol (50 ml) Diprivan Fresofol Sevoflurane Sevoflurane is a halogenated hydrocarbon, acts as a general anesthetic during surgery either alone or combined with others. It is given by inhalation. This helps produce more effective anesth... Trade Names Sevorane Enflurane Enflurane is a structural isomer of isoflurane, prescribed for induction and maintenance of general anesthesia.... Atracurium Atracurium is a neuromuscular-blocking agent, used as an adjuvant in anesthesia. This medication provides relaxation of skeletal muscles during surgery. ... Trade Names Artacil -100 Isoflurane Isoflurane is halogenated ether, used for maintenance of general anesthesia. ... Trade Names Isorane Isorane (250 ml) Desflurane Desflurane is a general anesthetic, prescribed for induction of anesthesia during surgery.... Thiopental Thiopental is a barbiturate general anesthetic, prescribed for induction of anesthesia. It depresses the central nervous system, causing mild sleep.... Trade Names Anesthal Anesthal (1 gm) Intraval Sodium Intraval Sodium (1 gm) Intraval Sodium (500 mg) Pentone Pentone (1 gm) Pentothal Pentothal ( 1gm) Thiosal Thiosal (1 gm) Thiosol Thiosol (1 gm) Thipen Thipen (1 gm) Page 10 [Type text] Chapter 2 Anesthesia machine History of anesthesia machines The anaesthetic machine (UK English) or anesthesia machine (US English) is used by anaesthesiologists, nurse anaesthetists, and anaesthesiologist assistants to support the administration of anaesthesia. The most common type of anaesthetic machine in use in the developed world is the continuous-flow anaesthetic machine, which is designed to provide an accurate and continuous supply of medical gases (such as oxygen and nitrous oxide), mixed with an accurate concentration of anaesthetic vapour (such as isoflurane), and deliver this to the patient at a safe pressure and flow. Modern machines incorporate a ventilator, suction unit, and patient monitoring devices. The original concept of Boyle's machine was invented by the British anaesthetistHenry Boyle (1875–1941) in 1917. Prior to this time, anaesthetists often carried all their equipment with them, but the development of heavy, bulky cylinder storage and increasingly elaborate airway equipment meant that this was no longer practical for most circumstances. The anaesthetic machine is usually mounted on anti-static wheels for convenient transportation. Simpler anaesthetic apparatus may be used in special circumstances, such as theTriService Apparatus, a simplified anaesthesia delivery system invented for the Britisharmed forces, which is light and portable and may be used effectively even when no medical gases are available. This device has unidirectional valves which suck in ambient air which can be enriched with oxygen from a cylinder, with the help of a set of bellows. A large number of draw-over type of anaesthesia devices are still in use in India for administering an air-ether mixture to the patient, which can be enriched with oxygen. But the advent of the cautery has sounded the death knell to this device, due to the explosion hazard.the old anesthesia machines that used in some contry yet (Fig 2-1). Many of the early innovations in U.S. anaesthetic equipment, including the closed circuit carbon-dioxide absorber (aka: the Guedel-Foregger Midget) and diffusion of such equipment to anaesthetists within the United States can be attributed toRichard von Foregger and The Foregger Company. In dentistry a simplified version of the anaesthetic machine, without a Page 11 [Type text] ventilator or anaesthetic vaporiser, is referred to as a relative analgesia machine. By using this machine, the dentist can administer a mild inhalation sedation with nitrous oxide and oxygen, in order to keep his. patient in a conscious state while depressing the feeling of pain. old anesthesia machines( Fig 2-1) Introduction The anesthesia gas machine is a device which delivers a precisely-known but variable gas mixture, including anesthetizing and life-sustaining gases. The components and systems as described in this document are typical for a hypothetical generic anesthesia gas machine. The differences between older gas machines -such as the Ohmeda Modulus, Excel, or Aestiva and the Dräger Narkomed GS, Mobile, MRI, 2B, 2C, 3 or 4are less than their similarities. Therefore only the differences with the most impact on clinical practice are described for this generation of machines. However, this generation of gas machines is becoming less common as they approach the time when they will no longer be supported by the manufacturer's technical support and service. Differences between models have more clinical impact with the latest generation of gas machines because of the higher degree of computer-controlled basic systems, and monitor and electronic medical record integration. So the differences are more fully described here for new models from GE Healthcare (Aisys, Aespire, Avance, ADU) and Dräger (Apollo, Fabius GS ). Page 12 [Type text] Figure2-2 Dräger Narkomed 6000 anesthesia workstation Over the years, the anesthesia delivery system has evolved from a simple pneumatic device to a complex multisystem workstation, and new technologies continue to advance its development at a rapid pace (Fig 2-2 andFig 2-3 ). These continuing changes to one of the most important pieces of equipment used by anesthesia care providers can make maintaining a current knowledge base (sufficient for their safe use) difficult for many to achieve. To prevent mishaps, providers must be aware of the functional anatomy of the anesthesia workstation. Furthermore, this knowledge base must even. Fortunately, include the newer systems as they become available, to the extent that they are represented in an individual's practice the most basic workstation components are generally fairly consistent from one platform to another. These basic component systems include what was formerly referred to as the anesthesia machine proper (i.e., the pressure-regulating and gas-mixing components), the vaporizers, the anesthesia breathing circuit, the ventilator, the scavenging system, and respiratory and physiologic monitoring systems. . Figure2-3 GE/Datex-Ohmeda S/5 Anesthesia Delivery Unit (ADU) workstation Page 13 [Type text] Generic Anesthesia Machine A diagram of a generic two-gas anesthesia machine is shown in Figure2 -4 . The pressures within the anesthesia machine can be divided into three circuits: a high-pressure, an intermediate-pressure, and a low-pressure circuit (see Fig. 2-4 ). The high-pressure circuit is confined to the cylinders and the cylinders' primary pressure regulators. For oxygen, the pressure range of the high-pressure circuit extends from a high of 2200 pounds per square inch gauge (psig) to 45 psig, which is the regulated cylinder pressure. For nitrous oxide in the high-pressure circuit, pressures range from a high of 750 psig in the cylinder to a low of 45 psig. The intermediate-pressure circuit begins at the regulated cylinder supply sources at 45 psig, includes the pipeline sources at 50 to 55 psig, and extends to the flow control valves. Depending on the manufacturer and specific machine design, second-stage pressure regulators may be used to decrease the pipeline supply pressures to the flow control valves to even lower pressures, such as 14 or 26 psig within the intermediate-pressure circuit the low-pressure circuit extends from the flow control valves to the common gas outlet. The low-pressure circuit includes the flow tubes, the vaporizers, and a one-way check valve on most Datex-Ohmeda machines. Both oxygen and nitrous oxide have two supply sources: a pipeline supply . Figure 2-4 Diagram of a generic two-gas anesthesia machine source and a cylinder supply source. The pipeline supply source is the primary gas source for the anesthesia machine The hospital piping system provides gases to the machine at approximately 50 psig, which is the normal working pressure of most machines The cylinder supply source serves as a backup if the pipeline fails. The oxygen oxygen cylinder source is regulated from 2200 to approximately 45 psig, and the nitrous oxide cylinder source is regulated from 745 to approximately 45 psig A safety device traditionally referred to as the failsafe valve is located downstream from the nitrous oxide supply source. It serves as an interface between the oxygen and nitrous oxide supply sources. This valve shuts off or proportionally decreases the supply of nitrous oxide (and other gases) if the oxygen supply pressure decreases. Contemporary machines have an alarm device to monitor the oxygen supply pressure. A high-priority alarm is actuated when the oxygen supply pressure declines to a predetermined threshold, such as 30 psig. Most Datex-Ohmeda machines have a second-stage oxygen regulator located downstream from the oxygen supply source in the intermediate-pressure circuit. It is adjusted to a precise pressure level, such as 14 psig. This regulator supplies a constant pressure to the oxygen flow control valve, regardless of fluctuating oxygen pipeline pressures. For example, the Page 14 [Type text] flow from the oxygen flow control valve remains constant if the oxygen supply pressure is greater than 14 psig. The flow control valves represent an important landmark because they separate the intermediate pressure circuit from the low-pressure circuit. The low-pressure circuit is the part of the machine that is downstream from the flow control valves. The operator regulates flow entering the low-pressure . Numbers to remember The hospital pipeline is the primary gas source at 50 psi, which is the normal working pressure of most machines. Cylinders - Oxygen is supplied at around 2000 psi (regulated to approximately 45 psi after it enters the machine). Oxygen flush is a "straight shot" from supply to delivery point, 35-75 L/min. OSHA links on Waste Anesthetic Gases (WAGs) gives the NIOSH recommendation to OSHA occupational exposure should be limited to (an eight hour time-weighted average of) not more than 2 ppm halogenated agents (0.5 ppm if nitrous oxide in use), and not more than 25 ppm nitrous oxide. Read the 1977 NIOSH recommendation on waste gases. Tubing sizes- scavenger 19 or 30 mm, ETT or common gas outlet (CGO) 15 mm, breathing circuit 22 mm. . . Page 15 [Type text] General features of all anesthesia gas machines The basic pneumatic-mechanical design of the anesthesia gas machine has become familiar to a generation of providers. The basic design has been called upon to perform more complicated functions since 1990, with the advent of computer-controlled monitors into the operating room, especially pulse oximetry, capnography, and gas analysis. Our gas machines have become topheavy with the monitors we have added to their basic design. Now, the advent of the computer gives us a new generation of anesthesia gas machines, which have a great deal of added functionality in a small package, designed from the start to be microprocessor controlled. The prototypes of this new wave are the ADU, Aisys, Apollo, and Fabius GS. These gas machines are being purchased because they o o o o enhance patient safety more accurate basic components such as ventilators, vaporizers, flowmeters integrated, computer-controlled alarms feature advanced ventilation modes pressure control ventilation (PCV) pressure control ventilation with volume guarantee (PC-VG) synchronized intermittent mandatory ventilation (SIMV) with pressure- or volume-controlled breaths (called. respectively, SIMV-PS, and SIMV-PSV on the Aisys) o pressure support ventilation (PSV) perform compliance and leak testing of the breathing circuit, and compensate for these to produce unprecedented accuracy in delivered tidal volumes, which may lessen the need for non-rebreathing circuits. for children are smaller and lighter (in some cases) because they have integrated monitoring allow automated record keeping more easily than traditional designs o electronic capture of fresh gas flow o microprocessor integration feature improved monitors,and innovative new monitoring capabilities (spirometry, and flow-time waveforms) . R EQUI RED COMPONENTS OF AN ANE STHESI A WORKSTATION The current anesthesia gas machine (workstation) standard is ASTM F1850 (a standard promulgated by American Society for Testing and Materials). The European standard is EN740. F1850 specifies what is needed for an anesthesia workstation. The components are typically built into new gas machines, or they may be added to older machines. Required components include: o o Battery backup for 30 minutes Alarms Grouped into high, medium, and low priority. High priority alarms may not be silenced for more than 2 minutes. Page 16 [Type text] o o o o o o o o o o o o o o o o o o o o o o o o o o Certain alarms and monitors must be automatically enabled and functioning prior to use, either through turning the machine on, or by following the pre-use checklist: breathing circuit pressure, oxygen concentration, exhaled volume or carbon dioxide (or both). A high-priority pressure alarm must sound if user-adjustable limits are exceeded, if continuing high pressure is sensed, or for negative pressure. Disconnect alarms may be based on low pressure, exhaled volume, or carbon dioxide. Required monitors Exhaled volume Inspired oxygen, with a high priority alarm within 30 seconds of oxygen falling below 18% (or a user-adjustable limit). Oxygen supply failure alarm A hypoxic guard system must protect against less than 21% inspired oxygen if nitrous oxide is in use. Anesthetic vapor concentration must be monitored. Pulse oximetry, blood pressure monitoring, and EKG are required Pressure in the breathing circuit is limited to 12.5 kPa (125 cm water). The electrical supply cord must be non-detachable or resistant to detachment. The machine must have at least one oxygen cylinder attached. The hanger yoke must be pin-indexed, have a clamping device that resists leaks, and contain a filter. It must have a check valve to prevent transfilling, and a cylinder pressure gauge. There must be cylinder pressure regulators. The machine must use pipeline gas as long as pipeline pressure is greater than 345 kPa (50 psi). Flowmeters: Single control for each gas Each flow control next to a flow indicator Uniquely shaped oxygen flow control knob Valve stops (or some other mechanism) are required such that excessive rotation will not damage the flowmeter. Oxygen flow indicator is to the right side of a flowmeter bank Oxygen enters the common manifiold downstream of other gases An auxiliary oxygen flowmeter is strongly recommended An oxygen flush is present, capable of 35-75 L/min flow which does not proceed through any vaporizers. Vaporizers Concentration-calibrated An interlock must be present Liquid level indicated, designed to prevent overfilling "Should" use keyed-filler devices No discharge of liquid anesthetic occurs from the vaporizer even at maximum fresh gas flow Only one common gas outlet at 22 mm outer diameter, 15 mm inner diameter, which is designed to prevent accidental disconnection pipeline gas supply Pipeline pressure gauge PInlets for at least oxygen and nitrous oxide DISS protected In line filter Check valve Checklist must be provided (it may be electronic, or performed manually by the user) A digital data interface must be provided Path of gases within the machine Oxygen has five "tasks"Fig( 2-5) in the AGM; it powers the Page 17 [Type text] 1. 2. 3. 4. 5. ventilator driving gas flush valve oxygen pressure failure alarm oxygen pressure sensor shut-off valve ("fail-safe") flowmeters. It also plays a role in the hypoxic guard system, which guard system which maintains the correct proportion between flows of oxygen and nitrous oxide. The machine components can also be logically conceptualized by the amount of pneumatic pressure they are exposed to: Fig 2-5 Diagram of the five tasks of oxygen 1.The High-pressure circuit consists of those parts which receive gas at cylinder pressure hanger yoke (including filter and unidirectional valve) yoke block cylinder pressure gauge cylinder pressure regulators 2. The Intermediate pressure circuit receives gases at low, relatively constant pressures (37-55 psi, which is pipeline pressure, or the pressure downstream of a cylinder regulator) o pipeline inlets and pressure gauges o ventilator power inlet o Oxygen pressure-failure device (fail-safe) and alarm o flowmeter valves o oxygen and nitrous oxide second-stage regulators o oxygen flush valve 3. The Low-pressure circuit includes components distal to the flowmeter needle o valves o flowmeter tubes o vaporizers o check valves (if present) o common gas outlet o o o o Page 18 [Type text] M ANUF ACTURERS There are two major manufacturers of anesthesia gas machines in the United States. Dräger Medical Inc. (Telford, Pennsylvania) currently offers the Apollo, Fabius (GS Premium, MRI), Tiro (and Tiro M). o o o o o o o o Apollo Fabius GS Fabius MRI Fabius Tiro "Developed to be used in facilities where space is a premium" Fabius Tiro M ("mobile") "The Fabius Tiro M is a compact anesthesia system that offers the full spectrum of anesthesia ventilation to military anesthesiologists/ CRNAs in the field of operations. This unit can be used in a variety of mobile and stationary military applications where general anesthesia is required. The modular design allows all standard system components to be stored in a single container ..." Narkomed 6000 / 6400 Narkomed GS Narkomed Mobile, 2C, 3, 4 GE Healthcare (Madison, Wisconsin) currently offers the first four gas machines listed. Aisys Aespire Avance Aestiva Aestiva models are available for MRI o ADU o Modulus o Excel o o o o Pipeline Supply Source The pipeline supply source is the primary gas source for the anesthesia machine. Most hospitals have a central piping system to deliver medical gases such as oxygen, nitrous oxide, and air to the operating room. The central piping system must supply the anesthesia machine with the correct gases at the appropriate pressure for the anesthesia workstation to function properly(Fig2-6 ). Unfortunately, this does not always occur The operator must take two actions if a pipeline crossover is suspected, First, the backup oxygen . Page 19 [Type text] cylinder should be turned on. Second, the pipeline supply must be disconnected. This step is mandatory because the machine preferentially uses the inappropriate 50 psig pipeline supply source instead of the lower-pressure (45 psig) oxygen cylinder source. Gas enters the anesthesia machine through the pipeline inlet connections (see Fig.2-4). Cylinder Supply Source Anesthesia machines have reserve E cylinders (Fig 2-6) if a pipeline supply source is not available or if the pipeline fails. Color-coded cylinders are attached to the anesthesia machine through the hanger yoke assembly. The hanger yoke assembly orients and supports the cylinder, provides a gas-tight seal, and ensures a unidirectional flow of gases into the machine. Each hanger yoke is equipped with the Pin Index Safety System (PISS) . (Fig 2-7) The PISS is a safeguard introduced to eliminate cylinder interchanging and the possibility of accidentally placing the incorrect gas on a yoke designed to accommodate another gas. Two pins on the yoke are arranged so that they project into the cylinder valve. Each gas or combination of gases has a specific pin arrangement. Gas travels from the high-pressure cylinder source to the anesthesia machine when the cylinder is turned on (see Fig.1-4 ). A check valve is located downstream from each cylinder if a double-yoke assembly is used. The check valve has several functions. First, it minimizes gas transfer from a cylinder at high pressure to one with lower pressure. Second, it allows an empty cylinder to be exchanged for a full one while gas flow continues from the other cylinder into the machine with minimal loss of gas. Third, it minimizes leakage from an open cylinder to the atmosphere if one cylinder is absent. A cylinder gauge indicating supply pressure is located downstream from the check valves. The gauge indicates the pressure in the cylinder having the higher pressure when two reserve cylinders of the same gas are opened at the same time. Each cylinder supply source has a pressure-reducing valve known as the cylinder's pressure regulator . It reduces the high and variable storage pressure in a cylinder to a lower, more constant pressure suitable for use in the anesthesia machine. The oxygen cylinder's pressure regulator reduces the ylinder's oxygen pressure from a high of 2200 psig to approximately 45 psig. The nitrous oxide cylinder's pressure regulator receives pressure of up to 745 psig and reduces it to approximately 45 psig. The cylinders should be turned off except during the preoperative machine checking period or when a pipeline source is unavailable. If left on, the reserve cylinder supply can be silently depleted whenever the pressure inside the machine decreases to a value lower than the regulated cylinder pressure. Oxygen pressure within the machine can decrease below 45 psig with oxygen flushing or with ventilator use, particularly at high peak flow rates. The pipeline supply pressures of all gases can be less than 45 psig if problems exist in the central piping system. If the cylinders are left on, they will eventually become depleted, and no reserve supply will be available if a pipeline failure occurs. Page 20 [Type text] E Tank (Fig 2-6) pipeline & cylinder of oxygen ) High Pressure System-Fig 2-8 ) )Fig2-7(Hanger Yoke: 1- orients and supports the cylinder 2- Providing a gas-tight seal 3-Ensuring a unidirectional gas flow into the machine ž ž Page 21 [Type text] Safety Devices for Oxygen Supply Pressure Failure Oxygen and nitrous oxide supply sources existed as independent entities in older models of anesthesia machines, and they were not pneumatically or mechanically interfaced. Abrupt or insidious oxygen pressure failure could lead to the delivery of a hypoxic mixture. The 2000 ASTM F1850-00 standard states, "The anesthesia gas supply device shall be designed so that whenever oxygen supply pressure is reduced to below the manufacturer specified minimum, the delivered oxygen concentration shall not decrease below 19% at the common gas outlet." Contemporary anesthesia machines have a number of safety devices that act together in a cascade manner to minimize the risk of hypoxia as oxygen pressure decreases. Several of these devices are described in the following sections. Pneumatic and Electronic Alarm Devices Many older anesthesia machines have a pneumatic alarm device that sounds a warning when the oxygen supply pressure decreases to a predetermined threshold value such as 30 psig. The 2000 ASTM F1850-00 standard mandates that medium priority alarm shall be activated within 5 seconds when the oxygen pressure decreases below a manufacturer-specified threshold pressure. alarm devices are used to meet this guideline. Electronic Fail-Safe Valves A fail-safe valve is present in the gas line supplying each of the flow meters except that for oxygen. Controlled by oxygen supply pressure, the valve shuts off or proportionally decreases the supply pressure of all other gases (e.g., nitrous oxide, air, carbon dioxide, helium, nitrogen) as the oxygen supply pressure decreases. Unfortunately, the misnomer "fail-safe" has led to the misconception that the device prevents administration of a hypoxic mixture. This is not the case. Machines that are not equipped with a flow proportioning system (see "Proportioning Systems") can deliver a hypoxic mixture under normal working conditions. The oxygen flow control valve can be closed intentionally or accidentally. Normal oxygen pressure keeps other gas lines open so that a hypoxic mixture can result. Datex-Ohmeda machines are equipped with a fail-safe valve known as the pressure sensor's shut-off valve ( Fig.2-9 ). The valve operates on a threshold principle, and it is open or closed. Oxygen supply pressure opens the valve, and the valve's return spring closes the valve. Figure2-9 shows a nitrous oxide pressure sensor's shut-off valve with a threshold pressure of 20 psig. In Figure(2-9A ) , an oxygen supply pressure greater than 20 psig is exerted on the mobile diaphragm. This pressure moves the piston and pin upward, and the valve opens. Nitrous oxide flows freely to the nitrous oxide flow control valve. In Figure(2-9 B ), the oxygen supply pressure is less than 20 psig, and the force of the valve's return spring completely closes the valve. Nitroux oxide flow stops at the closed fail-safe valve, and it does not advance to the nitrous oxide flow control valve. Dr ger Medical uses a fail-safe valve known as the oxygen failure protection device (OFPD) to interface the oxygen pressure with that of other gases, such as nitrous oxide or other inert gases. It differs from Datex-Ohmeda's oxygen pressure sensor's shut-off valve because the OFPD is based on a proportioning principle rather than a threshold principle. The pressure of all gases controlled by the OFPD decreases proportionally with the oxygen pressure. The OFPD consists of a Page 22 [Type text] seat-nozzle assembly connected to a spring-loaded piston ( Fig.2-10 ) .The oxygen supply pressure (see Fig.2-10, left panel ) is 50 psig. This pressure pushes the piston upward, forcing the nozzle away from the valve seat. Nitrous oxide and other gases advance toward the flow control valve at 50 psig. The oxygen pressure in the right panel is 0 psig. The spring is expanded and forces the nozzle against the seat, preventing flow through the device. The center panel shows an intermediate oxygen pressure of 25 psig. The force of the spring partially closes the valve. The nitrous oxide pressure delivered to the flow control valve is 25 psig. There is a continuum of intermediate configurations between the extremes (0 to 50 psig) of oxygen supply pressure. These intermediate valve configurations are responsible for the proportional nature of the OFPD. It is important to understand the differences of these fail-safe devices; the Datex-Ohmeda pressure sensor's shut-off valve is an all-or-nothing threshold device, whereas the Dr ger OFPD is a variable-flow proportioning system Second-Stage Pressure Regulator for Oxygen Most contemporary Datex-Ohmeda workstations have a second-stage pressure regulator for oxygen that is set at a specific value between 12 and 19 psig. The oxygen flow meter's output is constant when the oxygen supply pressure exceeds the threshold value. The Datex-Ohmeda pressure sensor's shut-off valves are set at a higher threshold value (20 to 30 psig). This ensures that oxygen is the last gas flow to decrease if oxygen pressure fails The amount of time The amount of time that an anesthesia machine can operate from E-cylinder supplies is commonly of concern. This is becoming particularly important to anesthesia care providers now that anesthesia machines are being used more frequently in the setting of office-based and remote (outside the operating room) anesthesia care within hospitals. For oxygen, the volume of gas remaining in the Approximate remaining time# oxygen cylinder(psig) 200 . oxygen flow rate (L/ min) cylinder is proportional to cylinder pressure. One author has proposed the following equation to help estimate the time remaining , It should be noted that this calculation will provide a gross estimate of the time remaining and may not be exact. Furthermore, users should be cautioned that use of a pneumatically driven mechanical ventilator will dramatically increase oxygen utilization rates, thus decreasing the time remaining until depletion of the cylinder. Hand ventilation at low fresh gas flow rates may consume less than 5% of the amount of oxygen consumed by intermediate flow meter settings coupled with the use of pneumatically powered Dräger Medical Fabius GS and Narkomed 6000 series do not affect oxygen consumption rates, they may be preferable to conventional gas-driven ventilators in practice settings that are dependent on the use of compressed gas cylinders as the primary gas source. Page 23 [Type text] Figure2-9 Shut-off valve of the pressure sensor. A, The valve is open because the oxygen supply pressure is greater than the threshold value of 20 psig. B, The valve is closed because of inadequate oxygen pressure . Figure2-10 The oxygen failure protection device (OFPD) responds proportionally to changes in oxygen su pply pressure. The OFPD consists of a seat-nozzle assembly connected to a spring-loaded piston Flow Meter Assemblies The flow meter assembly ( Fig. 2-11) precisely controls and measures gas flow to the common gas outlet. With traditional glass flow meter assemblies, the flow control valve regulates the amount of flow that enters a tapered, transparent flow tube known as a Thorpe tube . A mobile indicator float Page 24 [Type text] inside the flow tube indicates the amount of flow passing through the associated flow control valve. The quantity of flow is indicated on a scale associated with the flow tube. Physical Principles of Conventional Flow Meters Opening the flow control valve allows gas to travel through the space between the float and the flow tube. This space is known as the annular space ( Fig.2-12 ). The indicator float hovers freely in an equilibrium position where the upward force resulting from gas flow equals the downward force on the float resulting from gravity at a given flow rate. The float moves to a new equilibrium position in the tube when flow is changed. These flow meters are commonly referred to as constant-pressure flow meters because the pressure decrease across the float remains constant for all positions in the tube. Flow tubes are tapered, with the smallest diameter at the bottom of the tube and the largest diameter at the top. The term variable orifice designates this type of unit because the annular space between the float and the inner wall of the flow tube varies with the position of the float. Flow through the constriction created by the float can be laminar or turbulent, depending on the flow rate ( Fig.2-13). The characteristics of a gas that influence its flow rate through a given constriction are viscosity (i.e., laminar flow) and density (i.e., turbulent flow). Because the annular space is tubular at low flow rates, laminar flow is present, and viscosity determines the gas flow rate. The annular space simulates an orifice at high flow rates, and turbulent gas flow then depends predominantly on the density of the gas. Figure2- 11 Oxygen flow meter assembly. The oxygen flow meter assembly is composed of the flow control valve assembly plus the flow meter subassembly Page 25 [Type text] Figure2-12 The clearance between the head of the float and the flow tube is known as the annular space. It can be considered an equivalent to a circular channel of the same cross-sectional area . Figure2-13 Flow tube constriction. The lower portion of the illustration represents the lower portion of two flow tubes. The clearance between the head of the float and the flow tube is narrow. The equivalent channel is tubular because its diameter is less than its length. Viscosity is dominant in determining gas flow rate through this tubular constriction. The upper portion of the illustration represents the upper portion of a flow tube. The equivalent channel is orificial because its length is less than its width. Density is dominant in determining gas flow rate through this o rificial constriction. . Page 26 [Type text] Components of Flow Meter Assemblies Flow Control Valve Assembly The assembly of the flow control valve (see Fig2-11) is composed of a flow control knob, a needle valve, a valve seat, and a pair of valve stops. The assembly can receive its pneumatic input directly from the pipeline source (50 psig) or from a second-stage pressure regulator. The location of the needle valve in the valve seat changes to establish different orifices when the flow control valve is adjusted. Gas flow increases when the flow control valve. Flow Meter Subassembly The flow meter subassembly (see Fig.2-11) consists of the flow tube, the indicator float with float stops, and the indicator scale. FLOW TUBES. Contemporary flow tubes are made of glass. Most have a single taper in which the inner diameter of the flow tube increases uniformly from bottom to top. Manufacturers provide double flow tubes for oxygen and nitrous oxide to provide better visual discrimination at low flow rates. A fine flow tube indicates flow from approximately 200 mL/min to 1 L/min, and a coarse flow tube indicates flow(Fig 2-12) from approximately 1 L/min to between 10 and 12 L/min. The two tubes are connected in series and supplied by a single flow control valve. The total gas flow is that shown on the higher flow meter. INDICATOR FLOATS AND FLOAT STOPS. Contemporary anesthesia machines use several different types of bobbins or floats, including plumbbob floats rotating, skirted floats and ball floats. Flow is read at the top of plumb-bob and skirted floats and at the center of the ball on the ball-type floats. Flow tubes are equipped with float stops at the top and bottom of the tube. The upper stop prevents the float from ascending to the top of the tube and plugging the outlet. It also ensures that the float is visible at maximum flows instead of being hidden in the manifold. The bottom float stop provides a central foundation for the indicator when the flow control valve is turned off. Scale .The flow meter scale can be marked directly on the flow tube or located to the right of the tube. Gradations corresponding to equal increments in flow rate are closer together at the top of the scale because the annular space increases more rapidly than does the internal diameter from bottom to top of the tube. Rib guides are used in some flow tubes with ball-type indicators to minimize this compression effect. They are tapered glass ridges that run the length of the tube. There are usually three rib guides that are equally spaced around the inner circumference of the tube. In the presence of rib guides, the annular space from the bottom to the top of the tube increases almost proportionally with the internal diameter. This results in a nearly linear scale. Rib guides are employed on North American Dr ger flow tubes. SAFETY FEATURES. The flow meter subassembly for each gas on the Datex-Ohmeda Modulus I, Modulus II, Modulus II Plus, CD, and Aestiva is housed in an independent, color-coded, pin-specific module. The flow tubes are adjacent to a gas-specific, color-coded backing. The flow scale and the chemical formula or name of the gas are permanently etched on the backing to the right of the flow tube. Page 27 [Type text] ž ž ž ž ž ž ž ž ž Flow meter scales are individually hand-calibrated using the specific float to provide a high degree of accuracy. The tube, float, and scale make an inseparable unit. The entire set must be replaced if any component is damaged. North American Dr ger does not use a modular system for the flow meter subassembly. The flow scale, the chemical symbol, and the gas-specific color codes are etched directly onto the flow tube. The scale in use is obvious when two flow tubes for the same gas are used. Electronic Flow Meters Some newer anesthesia machines such as the Datex-Ohmeda S/5 ADU and the North American Dr ger Fabius GS have conventional control knobs and flow control valves,(Fig2-13) but have digital flow meters. The output from the flow control valve is represented graphically or numerically, or both, in liters per minute on the workstation's integrated user interface. These systems depend on electrical power to provide a precise display of gas flow. However, even when electrical power is totally interrupted, because the flow control valves are not electronic, oxygen should continue to flow. Because these machines do not have individual flow tubes that ph ysically quantitate the flow of each gas, a small, conventional, pneumatic fresh gas or total flow indicator is provided that indicates the total fresh gas flow from all flow control valves. This miniature flow tube informs the user of the approximate quantity of gas that is leaving the anesthesia workstation's common gas outlet. Fig 2-12 fine&coarse tube ž Fig 2-13 Oxygen Flush Valve The oxygen flush valve allows direct communication between the oxygen high-pressure circuit and the low-pressure circuit (see Fig.2-4 ). Flow from the oxygen flush valve enters the low-pressure circuit downstream from the vaporizers and downstream from the Datex-Ohmeda machine outlet check valve. The spring-loaded oxygen flush valve stays closed until the operator opens it by depressing the oxygen flush button. Actuation of the valve delivers 100% oxygen at a rate of 35 to 75 L/min to the breathing circuit. The oxygen flush valve can provide a high-pressure oxygen source suitable for jet ventilation when Page 28 [Type text] the anesthesia machine is equipped with a one-way check valve positioned between the vaporizers and the oxygen flush valve and when a positive-pressure relief valve exists downstream of the vaporizers; this pressure relief valve must be upstream of the outlet check valve. Because the Ohmeda Modulus II has such a one-way check valve and its positive-pressure relief valve is upstream from the check valve, the entire oxygen flow of 35 to 75 L/min is delivered to the common gas outlet at a high pressure of 50 psig. However, the Ohmeda Modulus II Plus and some Ohmeda Excel machines are not capable of functioning as an appropriate oxygen source for jet ventilation. The Ohmeda Modulus II Plus, which does not have the check valve, provides only 7 psig at the common gas outlet because some oxygen flow travels retrograde through an internal relief valve located upstream from the oxygen flush valve. The Ohmeda Excel 210, which does have a one-way check valve, also has a positive-pressure relief valve downstream from the check valve and is therefore unsuitable for jet ventilation.The older North American Dr ger Narkomed 2A, which does not have the check valve, provides an intermediate pressure of 18 psig to the common gas outlet because some oxygen flow travels retrograde through a pop-off valve located in the vaporizers. The oxygen flush valve is associated with several hazards. A defective or damaged valve can stick in the fully open position, resulting in barotrauma. A valve sticking in a partially open position can result in awareness by the patient because the oxygen flow from the incompetent valve dilutes the inhaled anesthetic. Imprope use of normally functionin oxygen flash valves also can result in problems overzealous intraoperative oxygen flashing can dilute inhaled anesthetics. Oxygen flashing during the inspiratory phase of positive- pressure ventilation can produce barothroma in patients if the anesthesia machine does not incorporate fresh gas decoupling or an appropriately adjusted inspiratory pressure limiter. Anesthesia systems (i.e., Dr ger Narkomed 6000, Julian, and Fabius GS and Datascope Anestar) with fresh gas decoupling are inherently safer from the standpoint of minimizing the chance of producing barotrauma from inappropriate use of an oxygen flush valve (see "Fresh Gas Decoupling"). With traditional anesthesia breathing circuits, excess volume cannot be vented during the inspiratory phase of mechanical ventilation because the ventilator's relief valve is closed and the adjustable pressure-limiting (APL) valve is "out of circuit" or closed. One caveat is illustrated by the Datex-Ohmeda S/5 ADU and Aestiva. These circle systems use an integrated, adjustable pressure limiter. If this device is properly adjusted, it functions like the APL valve to limit the maximum airway pressure to a safe level, thereby reducing the possibility of barotrauma. If a machine is equipped with a freestanding vaporizer downstream from the common gas outlet, oxygen flushing can deliver large quantities of inhaled anesthetic to the patient. Inappropriate preoperative use of the oxygen flush to evaluate the low-pressure circuit for leaks can be misleading, particularly on DatexOhmeda machines with a one-way check valve at the common outlet. Because backpressure from the breathing circuit closes the one-way check valve air-tight, major leaks in the low-pressure-circuit can go undetected with this leak test . . Page 29 [Type text] CHAPTER 3 : V APORIZERS introduction Through the years, vaporizers have evolved from rudimentary ether inhalers and copper kettles to the present temperature-compensated, variable-bypass vaporizers. In 1993, with the clinical introduction of desflurane, an even more sophisticated vaporizer was introduced to handle the unique physical properties of this agent. A newer generation of anesthesia vaporizers blending the older, copper kettle-like technology and innovative, computer-controlled technology has emerged in the Datex-Ohmeda Aladin Cassette Vaporizer system. Before the discussion of variable-bypass vaporizers, the Datex-Ohmeda Tec 6 desflurane vaporizer, and the Datex-Ohmeda Aladin cassette vaporizer, certain physical principles are reviewed to facilitate understanding of the operating principles, construction, and design of contemporary vaporizers. P HYSIC AL PRINCIPLES Vapor Pressure Contemporary inhaled volatile anesthetics exist in the liquid state below 20°C. When a volatile liquid is in a closed container, molecules escape from the liquid phase to the vapor phase until the number of molecules in the vapor phase is constant. These molecules bombard the wall of the container and create a pressure known as the saturated vapor pressure . As the temperature increases, more molecules enter the vapor phase, and the vapor pressure increases ( Fig. 3-1 ). Vapor pressure is independent of atmospheric pressure and is contingent only on the temperature and physical characteristics of the liquid. The boiling point of a liquid is the temperature at which the vapor pressure equals atmospheric pressure. At 760 mm Hg, the boiling points for desflurane, isoflurane, halothane, enflurane, and sevoflurane are approximately 22.8°C, 48.5°C, 50.2°C, 56.5°C, and 58.5°C, respectively. Unlike other contemporary inhaled anesthetics, desflurane boils at temperatures that may be encountered in clinical settings such as pediatric and burn operating rooms. This unique physical characteristic alone mandates a special vaporizer design to control the delivery of desflurane. If agent-specific vaporizers are inadvertently misfilled with incorrect liquid anesthetic agents, the resulting mixtures of volatile agents may demonstrate unique properties from those of the individual component agents. Latent heat of vaporization is the number of calories needed to convert 1 g of liquid to vapor, without temperature change in the remaining liquid. Thus, the temperature of the remaining liquid will drop as vaporization proceeds, lowering VP, unless this is prevented. Specific heat is the number of calories needed to increase the temperature of 1 g of a substance by 1 degree C. Manufacturers select materials for vaporizer construction with high specific heats to minimize temperature changes associated with vaporization. Thermal conductivity - a measure of how fast a substance transmits heat. High thermal conductivity is desirable in vaporizer construction. Variable-Bypass Vaporizers The Datex-Ohmeda Tec 4, Tec 5, and Tec 7 and the North American Dr ger Vapor 19.n and 20.n vaporizers are classified as variable-bypass, flow-over, temperature-compensated, agent-specific, out-of-breathing-circuit vaporizers. Variable bypass refers to the method for regulating output concentration. As gas flow enters the vaporizer's inlet, the setting of the concentration control dial Page 30 [Type text] determines the ratio of flow that goes through the bypass chamber and through the vaporizing chamber. The gas channeled to the vaporizing chamber flows over a wick system saturated with the liquid anesthetic and subsequently becomes saturated with vapor. Flow-over refers to the method of vaporization and is in contrast to a bubble-through system like that of a copper kettle vaporizer. The Tec 4, the Tec 5, Tec 7 and the Vapor 19.n and 20.n are classified as temperature-compensated because they are equipped with an automatic temperature-compensating device that helps maintain a constant vaporizer output over a wide range of temperatures. These vaporizers are agent specific and out of circuit because they are designed to accommodate a single agent and to be located outside the breathing circuit. Variable-bypass vaporizers are used to deliver halothane, enflurane, isoflurane, and sevoflurane, but not desflurane. Basic Operating Principles A diagram of a generic variable-bypass vaporizer is shown in Figure 3-2 . Vaporizer components include the concentration control dial, the bypass chamber, the vaporizing chamber, the filler port, and the filler cap. Using the filler port, the operator fills the vaporizing chamber with liquid anesthetic. The maximum safe fill level is predetermined by the position of the filler port, which is positioned to minimize the chance of overfilling. If a vaporizer is overfilled or tilted, liquid anesthetic can spill into the bypass chamber, causing an overdose. The concentration control dial is a variable restrictor, and it can be located in the bypass chamber or the outlet of the vaporizing chamber. The function of the concentration control dial is to regulate the relative flow rates through the bypass and vaporizing chambers. ž ž ž ž ž Figure 3 -1 Vapor pressure versus temperature curves for desflurane, isoflurane, halothane, enflurane, and sevoflurane. The vapor pressure curve for desflurane is steeper and shifted to higher vapor pressures compared with the curves for other contemporary inhaled anesthetics ž ž ž ž ž Page 31 Figure 3-2 Generic variable-bypass vap orizer. Vaporizer components include the concentration control dial, the bypass chamber with liquid anesthetic. The maximum safe fill [Type text] ž ž ž ž level is predetermined by the position of the filler port, which is positioned to minimize the chance of o verfilling. If a vaporizer is overfilled or tilted, liquid anesthetic can spill into the bypass chamber, causing an overdose. The concentration control dial is a variable restrictor, which can be located in the bypass chamber, causing an overdose. The concentration control dial is a variable restrictor, which can be located in the relative flow rates through the bypass and vaporizing chambers ž ž ž ž ž ž ž ž ž ž ž ž ž ž ž ž ž ž ž ž ž ž ž ž ž ž ž ž ž ž ž Flow from the flow meters enters the inlet of the vaporizer. More than 80% of the flow passes straight through the bypass chamber to the vaporizer outlet, and this accounts for the name bypass chamber . Less than 20% of the flow from the flow meters is diverted through the vaporizing chamber. Depending on the temperature and vapor pressure of the particular inhaled anesthetic, the flow through the vaporizing chamber entrains a specific flow of inhaled anesthetic. All three flows— flow through the bypass chamber, flow through the vaporizing chamber, and flow of entrained anesthetic—exit the vaporizer at the outlet. The final concentration of inhaled anesthetic is the ratio of the flow of the inhaled anesthetic to the total gas flow. The vapor pressure of an inhaled anesthetic depends on the ambient temperature (see Fig. 3-1) For example, at 20°C, the vapor pressure of isoflurane is 238 mm Hg, whereas at 35°C, the vapor pressure almost doubles (450 mm Hg). Variable-bypass vaporizers have an internal mechanism to compensate for different ambient temperatures. The temperature-compensating valve of the DatexOhmeda Tec-type vaporizer 4 is shown in Figure 3-3 . At high temperatures, such as those commonly used in pediatric or burn operating rooms, the vapor pressure inside the vaporizing chamber is high. To compensate for this increased vapor pressure, the bimetallic strip of the temperature-compensating valve leans to the right. This movement allows more flow to pass through the bypass chamber and less flow to pass through the vaporizing chamber. The net effect is a constant vaporizer output. In a cold operating room environment, the vapor pressure inside the vaporizing chamber decreases. To compensate for this decrease in vapor pressure, the bimetallic strip swings to the left, causing more flow to pass through the vaporizing chamber and less to pass through the bypass chamber. The net effect is a constant vaporizer output. ž Factors Influencing Vaporizer Output The output of an ideal vaporizer with a fixed dial setting would be constant, regardless of varied flow rates, temperatures, backpressures, and carrier gases. Designing such a vaporizer is difficult because, as ambient conditions change, the physical properties of gases and of vaporizers themselves can change. Contemporary vaporizers approach the ideal situation but still have some limitations. Several factors discussed in the following sections can influence vaporizer output. ž ž ž ž ž ž ž ž ž ž ž ž ž ž ž ž ž Flow Rate With a fixed dial setting, vaporizer output can vary with the rate of gas flowing through the vaporizer. This variation is particularly notable at extremes of flow rates. The output of all variablebypass vaporizers is less than the dial setting at low flow rates (<250 mL/min). This results from the relatively high density of inhaled volatile anesthetics. Insufficient turbulence is generated at low flow rates in the vaporizing chamber to upwardly advance the vapor molecules. At extremely high flow rates (e.g., 15 L/min), the output of most variable-bypass vaporizers is less than the dial setting. This Page 32 [Type text] discrepancy is attributed to incomplete mixing and saturation in the vaporizing chamber. The resistance characteristics of the bypass chamber and the vaporizing chamber can vary as flow increases, and these changes can decrease the output concentration. ž ž ž ž ž ž ž ž ž ž ž ž ž ž ž ž ž ž ž ž ž Temperature Because of improvements in design, the output of contemporary temperature-compensated vaporizers is almost linear over a wide range of temperatures. Automatic temperature-compensating mechanisms in bypass chambers maintain a constant vaporizer output with varying temperatures. A bimetallic strip (see Fig. 3-3 ) or an expansion element ( Fig. 3-4 ) directs a greater proportion of gas flow through the bypass chamber as temperature increases. Wicks are placed in direct contact with the metal wall of the vaporizer to help replace heat used for vaporization. Vaporizers are constructed with metals having relatively high specific heat and high thermal conductivity to minimize heat loss. ž ž Intermittent Backpressure Intermittent backpressure associated with positive-pressure ventilation or with oxygen flushing can cause higher vaporizer output concentration than the dialed setting. This phenomenon, known as the pumping effect , is more pronounced at low flow rates, low dial settings, and low levels of liquid anesthetic in the vaporizing chamber. The pumping effect is increased by rapid respiratory rates, high peak inspired pressures, and rapid drops in pressure during expiration. The Datex-Ohmeda Tec 4, Tec 5, and Tec 7 and the North American Dr ger Vapor 19.1 and 20.n ž ž ž ž ow Figure 3-3 Simplified schematic drawing of the Ohmeda Tec-type vaporizer. At high temperatures, the vapor pressure inside the vaporizing chamber is high. To compensate for the increased vapor pressure, the bimetallic strip of the temperature-co mpensating valve leans to the right, allowing more flow through the bypass chamber and less fl through ž the vaporizing chamber. The net effect is a constant vaporizer output. In a cold operating room environment, the vapor pressure inside the vaporizing chamber decreases. To compensate for the decreased vapor pressure, the bimetallic ž the vaporizing chamber. The net effect is a constant vaporizer output. In a cold operating room environment, the ž vapor pressure inside the vaporizing chamber decreases. To compensate for the decreased vapor pressure, the bimetallic ž strip swings to the left, causing more flow through the vaporizing chamber and less through the bypass chamber. The net effect is a constant vaporizer outputstrip swings to the left, causing more flow through the vaporizing chamber and less through the bypass chamber. The net effect is a constant vaporizer output ž ž ž . ž Page 33 [Type text] ž ž ž ž ž systems are relatively immune from the pumping effect. One proposed mechanism for the pumping effect depends on retrograde pressure transmission from the patient's circuit to the vaporizer during the inspiratory phase of positive-pressure ventilation. Gas molecules are compressed in the bypass and vaporizing chambers. When the backpressure is suddenly released during the expiratory phase of positive. ž ž ž ž ž ž ž Figure 3-4 Simplified schematic drawing of the North American Dr ger Vapor 19.1 vaporizer. Automatic temperaturecompensating mechanisms in bypass chambers maintain a constant vaporizer output with varying temperatures. An expansion element directs a greater proportion of gas flow through the bypass chamber as temperature increases pressure ventilation, vapor exits the vaporizing chamber through the vaporizing chamber outlet and retrograde through the vaporizing chamber inlet. This occurs because the output resistance of the bypass chamber is lower than that of the vaporizing chamber, particularly at low dial settings. The enhanced output concentration results from the increment of vapor that travels in the retrograde direction to the bypass chamber To decrease the pumping effect, the vaporizing chambers of newer systems are smaller than those of older variable-bypass vaporizers such as the Fluotec Mark II (750 mL). No substantial volumes of vapor can be discharged from the vaporizing chamber into the bypass chamber during the expiratory phase. The North American Dr ger Vapor 19.1 and 20.n and the Datex-Ohmeda Tec 5 and Tec 7 (see Fig. 3-4 ) has a long, spiral tube that serves as the inlet to the vaporizing chamber. When the pressure in the vaporizing chamber is released, some of the vapor enters this tube but does not enter the bypass chamber because of the tube's length. The Tec 4 (see Fig. 3-3 ) has an extensive baffle system in the vaporizing chamber, and a one-way check valve has been inserted at the common gas outlet to minimize the pumping effect. This check valve attenuates but does not eliminate the pressure increase because gas still flows from the flow meters to the vaporizer during the inspiratory phase of positive-pressure ventilation. Carrier Gas composition Vaporizer output is influenced by the composition of the carrier gas that flows through the vaporizer. When the carrier gas is quickly switched from 100% oxygen to 100% nitrous oxide, there is a rapid transient decrease in vaporizer output followed by a slow increase to a new steady-state value The transient decrease in vaporizer output is attributed to Page 34 [Type text] nitrous oxide's being more soluble than oxygen in halogenated liquid. The quantity of gas leaving the vaporizing chamber is transiently diminished until the anesthetic liquid is totally saturated with nitrous oxide. The mechanism for the new steady-state output value is less well understood. With contemporary vaporizers such as the North American Dr ger Vapor 19.1 and the Ohmeda Tec 4, the steady-state output value is less when nitrous oxide rather than oxygen is the carrier gas. CONVERSELY, THE OUTPUT OF SOME OLDER VAPORIZERS IS ENHANCED WHEN NITROUS OXIDE IS THE CARRIER GAS INSTEAD OF OXYGEN. CL ASSI FIC ATION Dräger Vapor 19.1, Vapor 2000, Penlon Sigma, Aladin vaporizers (Aisys, ADU), and Tec 4, 5, 7 are classified as. Variable bypass Fresh gas flow from the flowmeters enters the inlet of any vaporizer which is on. The concentration control dial setting splits this stream into bypass gas (which does not enter the vaporizing chamber), and carrier gas (also called chamber flow, which flows over the liquid agent). . Flow over Carrier gas flows over the surface of the liquid volatile agent in the vaporizing chamber, as opposed to bubbling up through it (as in the older copper kettle and Vernitrol). Temperature compensated Equipped with automatic devices that ensure steady vaporizer output over a wide range of ambient temperatures . Agent-specific Only calibrated for a single gas, usually with keyed fillers that decrease the likelihood of filling the vaporizer with the wrong agent . Out of circuit Out of the breathing circuit, as opposed to (much) older models such as the Ohio #8 (Boyle's bottle) which were inserted within the circle system. . The copper kettle and Vernitrol are measured-flow, bubble-through, non-temperature compensated, multiple agent, and out of circuit. V APORIZER INTERLOCK The vaporizer interlock ensures that Only one vaporizer is turned on Gas enters only the one which is on Trace vapor output is minimized when the vaporizer is off Vaporizers are locked into the gas circuit, thus ensuring they are seated correctly. O PER ATI NG Page 35 PRI NCIPLES OF V ARI ABLE BYP ASS V APO RI ZERS [Type text] Total fresh gas flow (FGF) enters and splits into carrier gas (much less than 20%, which becomes enriched- saturated, actually- with vapor) and bypass gas (more than 80%). These two flows rejoin at the vaporizer outlet. The splitting ratio of these two flows depends on the ratio of resistances to their flow, which is controlled by the concentration control dial, and the automatic temperature compensation valve. Effect of flow rate: The output of all current variable-bypass vaporizers is relatively constant over the range of fresh gas flows from approximately 250 mL/min to 15 L/min, due to extensive wick and baffle system that effectively increases surface area of vaporizing chamber. All sevoflurane vaporizers are less accurate (due to the low vapor pressure of the agent) at high fresh gas flows (> 10 L/min) and high vaporizer concentration settings typical after induction, where they deliver less than the dial setting (Anesth Analg 2000;91:834-6 notes that this tendency is accentuated if the vaporizer is nearly empty). Clinically this is relatively unimportant, since we titrate to effect (end tidal agent concentration) and use overpressure. Effect of ambient temperature: The output of modern vaporizers is linear from 20-35 degrees C, due to 1. Automatic temperature compensating devices that increase carrier gas flow as liquid volatile agent temperature decreases 2. Wicks in direct contact with vaporizing chamber walls 3. Constructed of metals with high specific heat and thermal conductivity 4. Effect of intermittent back pressure transmitted from breathing circuit : The pumping effect is due to positive pressure ventilation or use of the oxygen flush valve. It can increase vaporizer output. Modern vaporizers are relatively immune (older vaporizers were certainly N O T immune) due to check valves between the vaporizer outlet and the common gas outlet, smaller vaporizing chambers, or tortuous inlet chambers. Any of these design features prevent gas which has left the vaporizers from re-entering it. The check valves are why a negative pressure leak check was recommended by the 1993 FDA checklist (step 5), since it works for all machines. The ADU has check valves in the vaporizer control mechanisms. 5. The effect of altitude on vaporizer performance is controversial. Dorsch and Dorsch (Understanding Anesthesia Equipment 5th ed. 2008) state that one should consult the operator's manual. Some sources state that variable bypass types need not be adjusted for moderate changes in barometric pressure, but the Tec 6 must be dialed up beyond the desired dose at higher altitudes. Other sources disagree (see Ehrenwerth and Eisenkraft Anesthesia Equipment 1993). 6. H OW T O FI L L V A P O RI Z E R S Filling a funnel-type vaporizer. Filling a keyed vaporizer. Page 36 [Type text] For either funnel or keyed filler types, fill the vaporizer only to the top etched line within the sight glass. Do N O T hold the bottle up on a keyed filler until it stops bubbling (this will overfill the chamber, particularly if the concentration control dial is "on", or if leaks are present). The O N L Y current vaporizer which can be filled while it is operating is the Tec 6 Desflurane (but even that vaporizer is safer to fill in the "off" position). H OW MUCH LIQUI D AGEN T DOES A V APORIZER U SE PER HOUR Ehrenwerth and Eisenkraft (1993) give the formula: 3 x Fresh gas flow (FGF) (L/min) x volume % = mL liquid used per hour Or one can determine the volume (mL) of saturated vapor needed to provide 1% (ie 4000 x 0.01 = 40 mL); then use Avogadro's hypothesis, the molecular weight, the liquid density, and molar volume (22.4 L at 20 degrees C) to determine how many mL of liquid become 40 mL vapor per minute. Typically, 1 mL of liquid volatile agent yields about 200 mL vapor. This is why tipping is so hazardous- it discharges liquid agent into the control mechanisms, or distal to the outlet. And minute amounts of liquid agent discharged distal to the vaporizer outlet result in a large bolus of saturated vapor delivered to the patient instantaneously. H AZ A R D S A N D S A F E T Y F E A T U R E S O F C O N T E M P O R A R Y V AP O R I Z E R S H AZ A R D S o o Incorrect agent Tipping (does not apply to Aladin vaporizers or the Draeger 2000 set to "T") If tipped more than 45 degrees from the vertical, liquid agent can obstruct valves. Treatment: flush for 20-30 minutes at high flow rates with high concentration set on dial. Please note that this is the recommended treatment for the Tec 4 vaporizer. The correct approach for other models differs, so their individual operating manuals must be consulted. Simultaneous inhaled agent administration o If removing the central vaporizer from a group of three on an Ohmeda Modulus machine, move the remaining two so that they are adjacent. On models which were manufactured prior to 1995, removing the center vaporizer of three defeats the interlock, and allows the outer two vaporizers to be turned on simultaneously. Reliance on breath by breath gas analysis rather than preventive maintenance o Problem: failure of temperature compensation device may result in a rapid onset, high output failure of the vaporizer o Failure of renewable components such as seals and O-rings may have the same effect Overfilling o May be prevented by following the manufacturer's guidelines for filling: fill only to the top etched line on the liquid level indicator glass, and fill only when the vaporizer is off. A N AE S T H E S I A 2002;57:288 Leaks o Leaks are relatively common, often due to malposition of vaporizers on the back bar (A N A E S T H E S I A 2002;57:299-300), or loss of gaskets, and these leaks may not be detected with the standard checklist unless the negative pressure check is performed. Page 37 [Type text] o Tec 6 vaporizers can also leak liquid while being filled, if the desflurane bottle is missing the white rubber O-ring near its tip. This can be mistaken for a defective vaporizer (A N E S T H A N A L G 2003;96:1534-5) Electronic failure o As vaporizers incorporate electronics, they are susceptible to electronic failure. Two case reports detail ADU vaporizers failing due to "fresh gas unit failure", and from copious emesis soaking the machine (A N AE S T H E S I A 2000;55:1214-5, A N A E S T H E S I A 2000;55:1215). S AF E T Y F E AT U R E S Important safety features include: Keyed fillers Low filling port Secured vaporizers (less ability to move them about minimizes tipping) Interlocks Concentration dial increases output in all when rotated counterclockwise (as seen from above) C URRENT H AZARDS MODELS AND SAFET Y FE ATURES OF CONTEMPORA RY VAPORIZERS GAS/VAPOR BLENDERS Penlon Sigma is similar to the Tec vaporizers, and can be found on either type (GE, Dräger) of machine. The Penlon Sigma Delta sevoflurane vaporizer fits on Dräger machines. Page 38 [Type text] Dräger Vapor 19.1 is similar to Tec 4, 5: all are variable bypass types. The interlock on Dräger machines continues to function if any vaporizers are removed, but one must attach a short-circuit block to prevent leaks if any vaporizer is removed. There is no outlet check valve- the tortuous inlet arrangement protects from the pumping effect. The Sevotec 5 is used in a similar fashion to the other Tec 5 vaporizers. Note that in December 1997 the product labeling for sevoflurane was changed to allow fresh gas flow as low as 1 L/min (for not greater than 2 MAC-hours). Tec 5 vaporizers Tec 4 vaporizers Ohmeda Tec 4, 5 With the center vaporizer removed (if three are mounted side by side), one can activate both outer vaporizers simultaneously (in machines manufactured after 1995, this fault is corrected). Vaporizer outlet has check valve. Page 39 [Type text] Tec 6 desflurane vaporizer: Because of the volatility of this agent, new systems were designed to contain, transfer, and vaporize it. The saturated vapor pressure at room temperature (20 degrees C) is 664 torr- 87% of one atmosphere. This means that desflurane is nearly boiling at room temperature. The vaporizer is a gas/vapor blender, not a variable bypass type. Note that not all desflurane vaporizers are Tec 6 type. The Aladin cassette (Aisys, ADU) is a variable bypass vaporizer. Aladin vaporizer (Aisys, ADU) Cassettes containing each volatile liquid anesthetic are inserted into a port containing the central electronic control mechanism, which recognizes the contents of the cassette and dispenses agent into the stream of fresh gas flow. Because each cassette is only a liquid sump without control mechanisms, they can be tipped in any orientation without danger, and they are maintenance free. The cassette and the control mechanisms are checked as part of the electronic equipment checklist daily. The Aladin will not deliver volatile agent without mains power or battery backup, and adequate oxygen (or air) pressure. The output of older vaporizers varies slightly with changes in fresh gas mixture, whereas the Aladin compensates for this automatically. The ADU features a low agent alarm for desflurane (but NOT the other agents!), the hypoxic guard system takes the desflurane concentration into account along with nitrous oxide, and the desflurane cassette works without added heat. The Aisys has low agent alarms on all vaporizers. The cassettes are extremely light, and may be removed with one hand. For a study of this vaporizer's performance, see Anesth Analg 2001;93:391-5. Page 40 [Type text] Chapter 4 : ANESTHETIC CIRCUITS Gas exits the anesthesia machine at the common gas outlet and then enters an anesthetic circuit. The function of the anesthesia breathing circuit is to deliver oxygen and anesthetic gases to the patient and to eliminate carbon dioxide. Carbon dioxide can be removed by washout with adequate inflow of fresh gas or by the use of carbon dioxide absorbent media (e.g., soda lime absorption). This discussion is limited to semiclosed rebreathing circuits and the circle system. Mapleson Systems In 1954, Mapleson described and analyzed five different semiclosed anesthetic systems, which are classically referred to as the Mapleson systems and designated A to E. Willis and colleagues added the F system to these five original. The Mapleson systems are shown in Figure 4-1. System components can include a facemask, a spring-loaded pop-off valve, reservoir tubing, fresh gas inflow tubing, and a reservoir bag. Three distinct functional groups emerge, and they include the A, the BC, and DEF groups. The Mapleson A, also known as the Magill circuit, has a spring-loaded, pop-off valve located near the facemask, and the fresh gas flow enters the opposite end of the circuit near the reservoir bag. In the B and C systems, the spring-loaded, pop-off valve is located near the facemask, but the fresh gas inlet tubing is located near the patient. The reservoir tubing and breathing bag serve as a blind limb where fresh gas, dead space gas, and alveolar gas can collect. In the Mapleson DEF group, or the T-piece group, the fresh gas enters near the patient, and excess gas is popped off at the opposite end of the circuit. Even though the component arrangement and components are simple, functional analysis of the Mapleson systems can be complex. The amount of carbon dioxide rebreathing associated with each system is multifactorial, and variables that dictate the ultimate carbon dioxide concentration include the following: (1) the fresh gas inflow rate, (2) the minute ventilation, (3) the mode of ventilation (spontaneous or controlled), (4) the tidal volume, (5) the respiratory rate, (6) the inspiratory to expiratory ratio, (7) the duration of the expiratory pause, (8) the peak inspiratory flow rate, (9) the volume of the reservoir tube, (10) the volume of the breathing bag, (11) ventilation by mask, (12) ventilation through an endotracheal tube, and (13) the carbon dioxide sampling site. Performance of the Mapleson systems is best understood by studying the expiratory phase of the respiratory cycle (see Fig. 4-1 ). During spontaneous ventilation, the Mapleson A has the best efficiency of the six systems, requiring a fresh gas inflow rate of only one times the minute ventilation to prevent rebreathing of carbon dioxide. However, it has the worst efficiency during controlled ventilation, requiring minute ventilation of as much as 20 L/min to prevent rebreathing. Systems D, E, and F are slightly more efficient than systems B and C. To prevent rebreathing carbon dioxide, systems D to F require a fresh gas inflow rate of approximately 2.5 times the minute ventilation, whereas the fresh gas inflow rates required for systems B and C are somewhat higher. The following summarizes the relative efficiency of different Mapleson systems with respect to prevention of rebreathing, during spontaneous ventilation: A > DFE > CB. During controlled ventilation, DFE > BC > A. The Mapleson A, B, and C systems are rarely used today, but the D, E, and F systems are commonly employed. In the United States, the most popular representative from the DEF group is the Bain circuit. Page 41 [Type text] Bain Circuit The Bain circuit is a modification of the Mapleson D system. It is a coaxial circuit in which the fresh gas flows through a narrow inner tube within the outer corrugated tubing. The central tube originates near the reservoir bag, but the fresh gas enters the circuit at the patient's end ( Fig4-2 ). Exhaled gases enter the corrugated tubing and are vented through the expiratory valve near the reservoir bag. The Bain circuit may be used for spontaneous and controlled ventilation. The fresh gas inflow rate necessary to prevent rebreathing is 2.5 times the minute ventilation. This circuit has many advantages. It is lightweight, convenient, easily sterilized, and reusable. Scavenging of the gases from the expiratory valve is facilitated because the valve is located away from the patient. Exhaled gases in the outer reservoir tubing add warmth to inspired fresh gases. Hazards of the Bain circuit include unrecognized problems can cause hypercarbia from inadequate gas flow or increased respiratory resistance. An obstructed bacterial filter positioned Figure 4-1 Gas disposition at end expiration during spontaneous ( left ) and controlled ( right ) ventilation in circuits A through F. FGF, fresh gas flow Page 42 [Type text] . Figure 4-2 The Bain circuit. (Adapted from Bain JA, Spoerel WE: A streamlined anaesthetic system. Can Anaesth between the Bain circuit and the endotracheal tube can cause hypoxemia and mimic the signs and symptoms of severe bronchospasm. inadequate gas flow or increased respiratory resistance. An obstructed bacterial filter positioned between the Bain circuit and the endotracheal tube can cause hypoxemia and mimic the signs and symptoms of severe bronchospasm. The outer tube should be transparent to allow inspection of the inner tube. The integrity of the inner tube can be assessed as described by Pethick. High-flow oxygen is fed into the circuit while the patient's end is occluded until the reservoir bag is filled. The patient's end is opened, and oxygen is flushed into the circuit. If the inner tube is intact, the Venturi effect occurs at the patient's end, decreasing. pressure within the circuit, and the reservoir bag deflates. Conversely, a leak in the inner tube allows the fresh gas to escape into the expiratory limb, and the reservoir bag remains inflated. This test is recommended as a part of the preanesthesia check if a Bain circuit is used Page 43 [Type text] Chapter 5 : CARBON DIOXIDE ABSORPTION Different anesthesia systems eliminate carbon dioxide with various degrees of efficiency. The closed and semiclosed circle systems require carbon dioxide absorption. Desirable features of carbon dioxide absorbents include lack of toxicity with common anesthetics, low resistance to airflow, low cost, ease of handling, and efficiency. Absorber Canister On modern anesthesia machines, the absorber canister is composed of two clear plastic canisters arranged in series. (Fig 5-1) The canisters can be filled with bulk absorbent or with absorbent supplied by the factory in prefilled plastic disposable cartridges called prepacks . Free granules from bulk absorbent can create a clinically significant leak if they lodge between the clear plastic canister and the O-ring gasket of the absorber. Leaks have also been caused by defective prepacks that were larger than factory specifications. Prepacks can also cause total obstruction of the circle system if the clear plastic shipping wrapper is not removed before use. (Fig 5-1) absorber canister Page 44 [Type text] Chemistry of Absorbents Three formulations of carbon dioxide absorbents are commonly available: soda lime, Baralyme, and calcium hydroxide lime (Amsorb). Of these agents, the most commonly used is soda lime. All serve to eliminate carbon dioxide from the breathing circuit with various degrees of efficiency. By weight, the approximate composition of "high-moisture" soda lime is 80% calcium hydroxide, 15% water, 4% sodium hydroxide, and 1% potassium hydroxide (an activator). Small amounts of silica are added to produce calcium and sodium silicate. This addition produces a hard compound and reduces dust formation. The efficiency of the soda lime absorption varies inversely with the hardness; therefore, little silicate is used in contemporary soda lime. Sodium hydroxide is the catalyst for the carbon dioxide absorptive properties of soda lime. Baralyme is a mixture of approximately 20% barium hydroxide and 80% calcium hydroxide. It may also contain some potassium hydroxide. Calcium hydroxide lime is one of the newest commercially available carbon dioxide absorbents. It consists primarily of calcium hydroxide and calcium chloride and contains two setting agents: calcium sulfate and polyvinylpyrrolidine. The latter two agents enhance the hardness and porosity of the agent. The most significant advantage of calcium hydroxide lime over other agents is its lack of sodium and potassium hydroxides. The absence of these chemicals eliminates the undesirable production of carbon monoxide and the nephrotoxic substance known as compound A. The size of the absorptive granules has been determined by trial and error, which represents a compromise between resistance to airflow and absorptive efficiency. The smaller the granules, the more surface area is available for absorption. However, air flow resistance increases. The granular size of soda lime and Baralyme in anesthesia practice is between 4 and 8 mesh, a size at which resistance to airflow is negligible. Mesh refers to the number of openings per linear inch in a sieve through which the granular particles can pass. A 4-mesh screen means that there are four 0.25-inch openings per linear inch. An 8-mesh screen has eight 0.125-inch openings per linear inch. The absorption of carbon dioxide by soda lime is a chemical process, not a physical process. Carbon dioxide combines with water to form carbonic acid. Carbonic acid reacts with the hydroxides to form sodium (or potassium) carbonate and water. Calcium hydroxide accepts the carbonate to form calcium carbonate and sodium (or potassium) hydroxide. The equations for the reaction steps are as follows 1. CO 2 + H2 O = H 2 CO3 2. H2 CO3 + 2NaOH (KOH) = Na2 CO3 (K2 CO3 ) + 2H2 O + Heat 3. Na2 CO3 (K 2 CO3 ) + Ca(OH)2 = CaCO 3 + 2NaOH (KOH) Some carbon dioxide may react directly with Ca(OH)2 , but this reaction is much slower. The reaction with Baralyme differs from that of soda lime because more water is liberated by a direct reaction of barium hydroxide and carbon dioxide. 1. Ba(OH)2 + 8H 2 O + CO2 = 2. 9H2 O + 9CO2 = BaCO3 + 9H2 O + Heat 9H2 CO3 Then by direct reactions and by KOH and NaOH, 3. 9H 2 CO3 + 9Ca(OH) 2 CaCO3 + 18H 2 O + Heat Page 45 [Type text] Absorptive Capacity The maximum amount of carbon dioxide that can be absorbed by soda lime is 26 L of carbon dioxide per 100 g of absorbent. The absorptive capacity of calcium hydroxide lime has been reported at 10.2 L per 100 g of absorbent. However, channeling of gas through granules of soda lime or calcium hydroxide lime may substantially decrease this efficiency and allow only 10 to 20 L or less of carbon dioxide to be absorbed per 100 g of absorbent. Ethyl violet, the pH indicator added to soda lime and Baralyme to help assess the functional integrity of the absorbent, is a substituted triphenylmethane dye with a critical pH of 10.3. Ethyl violet hanges in color from colorless to violet when the pH of the absorbent decreases as a result of carbon dioxide absorption. The pH of fresh absorbent exceeds the critical pH, and the dye exists in its colorless form ( Fig5-1 A ). As absorbent becomes exhausted, however, the pH decreases below 10.3, and ethyl violet changes to its violet form (see Fig. 5-1 B ) through alcohol dehydration. Ethyl violet is not always a reliable indicator of the functional status of absorbent. Fluorescent lights can deactivate the dye so that the absorbent appears white even though it is exhausted. Interactions of Inhaled Anesthetics with Absorbents It is important and desirable to have carbon dioxide absorbents that are neither intrinsically toxic nor toxic when exposed to common anesthetics. Soda lime and Baralyme generally fit this description, but inhaled anesthetics do interact with absorbents to some extent. An uncommon anesthetic, trichloroethylene, reacts with soda lime to produce toxic compounds. In the presence of alkali and heat, trichloroethylene degrades into the cerebral neurotoxin dichloroacetylene, which causes cranial nerve lesions and encephalitis. Phosgene, a potent pulmonary irritant, is also produced, and phosgene can cause adult respiratory distress syndrome (ARDS). Sevoflurane produces degradation products on interaction with carbon dioxide absorbents. The major degradation product produced is an olefin compound known as fluoromethyl-2,2-difluoro-1(trifluoromethyl)vinyl ether, or compound A. During sevoflurane anesthesia, factors apparently leading to an increase in the concentration of compound A include low-flow or closed-circuit anesthetic techniques, the use of Baralyme rather than soda lime, higher concentrations of sevoflurane in the anesthetic circuit, higher absorbent temperatures, and fresh absorbent. Baralyme dehydration increases the concentration of compound A, and soda lime dehydration decreases the concentration of compound A. The degradation products apparently do not cause toxic effects in humans, even during low-flow anesthesia, but further studies are needed to verify this. Desiccated soda lime and Baralyme can degrade contemporary inhaled anesthetics to clinically significant concentrations of carbon monoxide, which can produce carboxyhemoglobin concentrations reaching 30% or more. Higher levels of carbon monoxide are more likely after prolonged contact between absorbent and anesthetics and after disuse of an absorber for at least 2 days, especially over a weekend. Case reports describing carbon monoxide poisoning have been most common for patients anesthetized on Monday morning, presumably because continuous flow from the anesthesia machine dehydrated the absorbents over the weekend. A fresh gas flow rate of 5 L/min or more through absorbent (without a patient) is sufficient to cause critical drying of the absorbent, particularly if the breathing bag is left off the breathing circuit. Absence of the bag facilitates retrograde flow through the circle system ,Because the inspiratory valve leaflet produces some resistance to flow, the fresh gas flow takes the retrograde path of least resistance through the absorbent and out the 22-mm breathing bag terminal. Several factors appear to increase the production of carbon monoxide and carboxyhemoglobin: 1. The inhaled anesthetic used (for a given MAC multiple, the magnitude of carbon monoxide production from greatest to least is desflurane enflurane > isoflurane halothane = sevoflurane) Page 46 [Type text] 2. The absorbent dryness (completely dry absorbent produces more carbon monoxide than hydrated absorbent) 3. The type of absorbent (at a given water content, Baralyme produces more carbon monoxide than does soda lime) 4. The temperature (a higher temperature increases carbon monoxide production) 5. The anesthetic concentration (more carbon monoxide is produced from higher anesthetic concentrations) 6. Low fresh gas flow rates 7. Reduced animal size per 100 g of absorbent Interventions have been suggested to reduce the incidence of carbon monoxide exposure in humans undergoing general anesthesia : 1. Educating anesthesia personnel regarding the cause of carbon monoxide production 2. Turning off the anesthesia machine at the conclusion of the last case of the day to eliminate fresh gas flow, which dries the absorbent 3. Changing carbon dioxide absorbent if fresh gas was found flowing during the morning machine check 4. Rehydrating desiccated absorbent by adding water to the absorbent 5. Changing the chemical composition of soda lime (e.g., Dragersorb 800 plus, Sofnolime, Spherasorb) to reduce or eliminate potassium hydroxide 6. Using absorbent materials such as calcium hydroxide lime that are free of sodium and potassium hydroxides The elimination of sodium and potassium hydroxides from desiccated soda lime diminishes or eliminates degradation of desflurane to carbon monoxide and sevoflurane to compound A but does not compromise carbon dioxide absorption. In late 2003, Abbott Laboratories, North Chicago, IL, makers of sevoflurane, in conjunction with the FDA, published a revised package insert and circulated a letter to anesthesia care providers that explained the potential for fires in the respiratory circuit with the use of sevoflurane. The revised sevoflurane package insert (Abbott Laboratories, reference 58-7208) describes this rare phenomenon occurring when sevoflurane is used in combination with a desiccated carbon dioxide absorbent such as dehydrated Baralyme. A poorly characterized chemical reaction between the sevoflurane and the absorbent reportedly has produced sufficient heat and combustible degradation products to lead to spontaneous generation of fires within the absorber canister subassembly and the breathing circuit. The combination of a rapid color change of the carbon dioxide absorbent (especially Baralyme) and an unusually slow increase in inhaled sevoflurane concentration, compared with the vaporizer concentration control dial setting, may indicate that a decomposition reaction with sevoflurane and the absorbent is occurring. If this happens, the potential for excessive heating or fire may be present within the respiratory circuit. To avoid this, anesthesia care providers should make every effort not to use desiccated carbon dioxide absorbents. Whenever there is a question of whether the absorbent is fresh and adequately hydrated, it should be replaced to avoid the possible occurrence of fire in the respiratory circuit. C LINI C AL SIGNS O F EXH AUSTIO N Newer gas machines which measure inspired carbon dioxide (often with alarms) allow us to change canisters when inspired carbon dioxide exceeds a known threshold (2-3 cm H2O). Rise (later a fall) in heart rate and blood pressure Page 47 [Type text] o o o Hyperpnea Respiratory acidosis Dysrhythmia Signs of SNS activation Flushed Cardiac irregularities Sweating Increased bleeding at surgical site Increased end tidal carbon dioxide NOT dark or cherry-red blood! Figure 5-1 ;Ethyl violet ch anges from colorless to violet when the pH of the absorbent decreases as a result of carbon dioxide absorption.A The pH of fresh absorbent exceeds the critical level, and the dye exists in its colorless form. B As absorbent becomes exhausted, the pH decreases below 10.3, and ethyl violet changes to its violet form through alcohol dehydration Page 48 [Type text] C HAPTER 6 : V ENTILATORS C LASSIFI CATION Power source is either compressed gas, electricity or both (contemporary bellows ventilators require both; piston ventilators do not require driving gas). Drive mechanism - modern bellows vents classified as double-circuit, pneumatically driven. Double-circuit means that a pneumatic force compresses a bellows, which empties its contents (gas from flowmeters and vaporizer) into the patient. Driving gas is oxygen, air, or a venturi mix of O2 and air (older Dräger Narkomed). Piston ventilators (Apollo, Narkomed 6000, Fabius GS) do not require driving gas . They are driven by compression from an electric motor. Cycling mechanism - time cycled, control mode. Newer ventilators feature pressure control, SIMV, and other modes. Modern ventilators use solid state electronics for timing. In volume control mode, driving gas flow ceases when the set tidal volume is delivered to the breathing circuit (not necessarily the patient- the two quantities may differ due to compliance losses or leaks!) or when a certain pressure is reached (peak pressure varies). In pressure control mode, the target pressure is established and maintained for a certain time (allowing delivered tidal volume to vary B ELLOWS CL ASSIFIC ATIO N "Hanging" bellows. To remember the classification: "ascend" and "descend" have "e" in them - so look at them during expiration. Ascending bellows ("standing") ascend during expiration (modern type preferred by many) and descending bellows ("hanging") descend during expiration. Ventilator relief valve gives 2 - 3 cm water pressure positive end-expiratory pressure (PEEP) (true for almost all mechanical ventilators with standing bellows- exceptions are the new Dräger piston ventilators, and any double-circuit ventilator which has a hanging bellows such as the Anestar). The ventilator relief valve (spill valve) allows scavenging ONLY during the expiratory phase. Page 49 [Type text] "Hanging" bellows on the Anestar. The compactness and ease of sterilization The newer hanging bellows housing, internal weight, and senses when the full "down" position. These factors, plus alarms based on chemical mechanical (pressure, volume, and detection, make piston or hanging However, the placement of the hanging surface makes visual detection of less easy to determine if the patient is addition to the rate set on the user must rely more on the pressure as opposed to the bellows. Water may bellows (lessening tidal volume and this tendency should be counteracted by heating the absorber head. C HOOSING hanging design is chosen for of the entire breathing circuit. unlike older designs, lacks an bellows do not return to the integration of disconnect (capnograph), and flow sensors) apnea bellows designs safe. bellows below the writing disconnects difficult. Also it is breathing spontaneously in mechanical ventilator. The and capnography waveforms gather in the descending creating an infection risk) but VENTI LATO R M ODES AND SETTI NGS Besides increased accuracy (due to compliance and leak compensation- see below on this page), the biggest improvement in current ventilators is their flexibility in modes of ventilation. Offering pressure controlled ventilation (PCV) allows more efficient and safe ventilation of certain types of patients. The improvement in tidal volume accuracy afforded by modern ventilators means that switching of circuits (for example, to a non-rebreather for small children) is not as necessary. (This is safer because potential misconnects are avoided, and quicker besides.) The latest direction the manufacturers have taken is offering modes (such as pressure support) that will support spontaneous ventilation, seen in anesthesia with much greater frequency due to the advent of the laryngeal mask airway and more frequent ambulatory procedures. The Aisys offers the following modes of ventilation: 1. Manual/Spontaneous 2. Volume control VCV 3. Pressure control PCV 4. SIMV-PSV o SIMV with volume-control breaths; Pressure support may be added for any small breaths the patient may take in between 5. SIMV-PC o SIMV with pressure-control breaths; Pressure support may be added for any small breaths the patient may take in between 6. Pressure Support o PSV-Pro; the "Pro" is short for "Protect," meaning that after 10 to 30 seconds of apnea (apnea delay is adjustable), the mode will revert to PCV. o If the patient begins breathing again in the PCV backup mode, the ventilator will switch back to PSVPro. 7. PC-VG Pressure control with Volume Guarantee Page 50 [Type text] V OLUME C ONTROLLED V ENTI L ATIO N (VCV) Waves- CMV. All ventilators offer volumed controlled ventilation (VCV). In this mode, the set volume is delivered at a constant flow. The peak inspiratory pressure is allowed to vary, and it does, according to the patient's compliance and airway resistance. Volume is adjusted to avoid atelectasis, and rate is adjusted for reasonable end-tidal carbon dioxide while monitoring the peak inspiratory pressure. S E T T I N G S F O R VCV I N A N A D U L T VT 5-10 mL/kg RR 6-12 breaths per minute (bpm) PEEP 0 cm H2O to start (add if trouble oxygenating, or especially at the lower end of the tidal volume range above) SYNCHRONIZED INTERMITTENT MANDATORY VENTILATION-VOLUME (SIMV-VOL) Page 51 [Type text] SIMV-Volume is VCV which detects spontaneous breaths (if any) and delivers volume-controlled breaths in synch with the patient's inspiratory efforts. This helps maintain minute ventilation, while avoiding breath-stacking or bucking. If too many (or too few) synchronized breaths are delivered, adjust trigger window and sensitivity. Trigger window- what percentage of the expiratory pause the vent monitors for patient effort Sensitivity- How much negative inspiratory force the patient must generate to trigger a breath from the ventilator . Patients may breathe at will between ventilator breaths. Some ventilators support these spontaneous breaths with pressure support ventilation (PSV), resulting in a mode called SIMV-PS. P R E S S U R E C O N T R O L V E N T I L AT I O N (PCV) Waves- PCV. Pressure control ventilation (PCV) controls inspiratory pressure, and allows inspired volume to vary (and it does, with changes in compliance and airway resistance). The flow generated varies. Flow is high at first to produce the set pressure early in inspiration, and it is less later in inspiration to maintain the set pressure through the inspiratory time. Target pressure is adjusted to produce a reasonable VT (reasonable to avoid the extremes of atelectasis and volu-trauma). Rate is adjusted to a reasonable endtidal carbon dioxide. The result (in many instances where peak inspiratory pressure [PIP] had been high when employing VCV [e.g. laparoscopy]) is often that PCV delivers increased tidal volume at a lower PIP. How is it possible to get greater tidal volumes at a lower PIP? The answer is that the flow of gas is greater early in inspiration (see waveforms above). Overall this may result in greater delivered volume with the same (or lower) pressure. INDICATIONS If there is a danger of high PIP, use PCV to limit pressure within the airway and lungs. Page 52 laryngeal mask airway o PCV may be used with an LMA (Anesthesiology 2000;92:1621-3). emphysema neonates/infants [Type text] If compliance is low, use PCV to obtain a higher tidal volume. pregnancy laparoscopic surgery (pneumoperitoneum) morbid obesity ARDS PCV is also used to compensate for leaks Uncuffed endotracheal tubes LMA S E T T I NGS FOR PCV I N AN AD U LT Pressure Limit ~20 cm H2O (adjust so that VT is high enough to prevent atelectasis e.g. 5-10 mL/kg) RR 6-12 breaths per minute (bpm) PEEP 0 cm H2O to start (add if trouble oxygenating) P R E S S U RE C ON T R OL WITH V O LU M E G U AR AN T E E (PC-VG) New mode in which the ventilator operates as PCV, but a tidal volume target is also set. The ventilator then dynamically adjusts the inspiratory pressure (while staying within the set maximum pressure [Pmax]) to achieve the desired VT breath-by-breath. Advantages include control of PIP (through the basic pressure-controlled mode) AN D control of arterial CO2 (through guarantee of VT and thus minute ventilation). SYNCHRONIZED INTERMITTENT MANDATORY VENTILATION- PRESSURE CONTROL (SIMV-PC) SIMV can be pressure controlled, resulting in a mode called SIMV-PC. M ODE S F O R S P O N T A N E OU S V E N T I L AT I ON -PRESSURE SUPPORT VENTILATION (PSV) With the advent of the LMA, spontaneous (unassisted) breathing is much more common during general anesthesia. But it is difficult to maintain a light enough plane of anesthesia to permit spontaneous ventilation, while retaining sufficient depth for surgery to proceed. Too deep, and respiratory acidosis will occur; too light, and bucking and awareness are risks. Ventilation modes which support the spontaneously breathing patient are useful to provide normocapnia without bucking. Many ventilators currently incorporate pressure support ventilation (PSV). Continuous positive airway pressure (CPAP), and airway pressure release ventilation (APRV) are probably on the horizon, but are not yet implemented in current equipment. Settings for PSV are simple- just pressure support level (12 cm H2O is the default on the ADU). Note that PSV R E Q U I R E S A S P O N TA N E O U S L Y B R E A T H I N G P A TI E N T as there is no (or very low) default backup respiratory rate. PSV senses patient inspiratory effort (volume or flow) and delivers pressure support while it is present. This tends to result in larger VT than the patient would produce on their own. PSV is useful to support minute ventilation and control arterial carbon dioxide for spontaneously-breathing patients during maintenance or emergence. In the Aisys, PSV-Pro ("protect") is found. If no breaths are detected during an adjustable apnea delay period (10-30 sec), the ventilator switches to the backup mode (PCV, at whatever settings are chosen when PSV-Pro is selected). If resumption of spontaneous breaths occurs later, the veniltor will return to PSV-Pro mode. Page 53 [Type text] T YPIC AL VENTI L ATOR AL ARMS All current gas machines have VPO (volume, pressure, oxygen) monitoring built in the breathing circuit. Most have agent monitoring as well. Some have spirometry and capnography. High pressure Pressure below threshold for 15 to 30 seconds (apnea or disconnect) Continuing high pressure Subatmospheric pressure Low tidal or minute volume High respiratory rate Reverse flow (may indicate incompetence of expiratory unidirectional valve in the breathing circuit) Apnea/disconnect alarms may be based on 1. Chemical monitoring (lack of end tidal carbon dioxide) 2. Mechanical monitoring Failure to reach normal inspiratory peak pressure, or Failure to sense return of tidal volume on a spirometer 3. Visual monitoring Failure of standing bellows to fill during mechanical ventilator exhalation Failure of manual breathing bag to fill during mechanical ventilation (machines with fresh gas decoupling- the Apollo, Fabius GS, Narkomed 6000) 4. Auditory monitoring - lack of breath sounds in precordial, lack of sound from ventilator cycling, etc. 5. Optic monitoring - Failure of the hanging bellows to fill completely (the "garage door" electronic eye sensor on the Julian) NEW FE AT URE S OF M OD E R N V E N T I L AT ORS PISTON V E NT I L AT OR S Piston ventilators use an electric motor to compress gas in the breathing circuit, creating the motive force for mechanical ventilator inspiration to proceed. The motor's force compresses the gas within the piston, raising the pressure within it, which causes gas to flow into the patient's lungs. Thus a piston ventilator uses no driving gas, and may be used without depleting the oxygen cylinder in case of oxygen pipeline failure. NM 6000 piston bellows In the Narkomed 6000, the bellows are occult, being placed horizontally under the writing surface. Although they can be viewed by lifting the writing surface, their to-and-fro movement is not normally visible during mechanical ventilation. The anesthetist relies on flow, pressure, and capnography Page 54 [Type text] waveforms (and the movement of the breathing bag during mechanical ventilation as a result of freshgas decoupling[see section on fresh gas decoupling below on this page]) to guard against disconnects or other problems. Apollo waveforms - ETCO2, Flow-time, Pressure The Apollo is similar, in that the bellows are hidden. Piston ventilator window Fabius GS. The Fabius GS has a piston ventilator similar to the Divan, but the bellows travel vertically, and their movement is continuously visible through a window to the left of the flowmeter bank. The piston ventilator has positive and negative pressure relief valves built in. If the pressure within the piston reaches 75 + 5 cm H2O, the positive pressure relief valve opens. If the pressure within the piston declines to -8 cm H2O, the negative pressure relief valve opens, and room air is drawn into the piston, protecting the patient from NEEP (negative end-expiratory pressure). There are several advantages to the piston ventilator system (Apollo, NM 6000 & Fabius GS): Page 55 Quiet No PEEP (2-3 cm water are mandatory on standing bellows ventilators due to the design of the ventilator spill valve) Greater precision in delivered tidal volume due to compliance and leak compensation, fresh gas decoupling, and the rigid piston design. [Type text] o There are less compliance losses with a piston as compared to a flexible standing bellows compressed by driving gas. Measuring compliance and leaks with a transducer near the piston eliminates a bulky, costly sensor close to the patient's airway (such as the D-Lite sensor on the ADU). Electricity is the driving force for the piston, so if oxygen pipeline pressure fails and one must rely on oxygen from the emergency cylinder, mechanical ventilation may continue (without exhausting the cylinder oxygen simply to drive the bellows). The disadvantages of the piston design include: Loss of the familiar visible behavior of a standing bellows during disconnects, or when the patient is breathing over and above the ventilator settings. Quiet (less easy to hear regular cycling) The piston ventilator design cannot easily accommodate nonrebreathing circuits (although the same can be validly argued in regards to traditional absorber heads like the Ohmeda GMS, or newer ascending bellows ventilators like the ADU). Potential for NEEP FLEXIBILITY The appearance of pressure control ventilation is a major advantage, allowing patients to be ventilated efficiently who were very difficult with volume control mode, such as patients with ARDS or morbid obesity. PCV also allows safe ventilation when excessive pressure must be strictly avoided; such as neonates and infants, and emphysematous patients. The appearance of modes like PSV which are capable of supporting the patient with spontaneous respirations extends our capabilities further. AC C U R ACY AT L OWE R TID AL V OL UMES Factors contributing to a discrepancy between set and delivered tidal volumes are especially acute in pediatrics and include . large compression volume of the circle system relative to the infant's lung volume leaks around uncuffed endotracheal tubes effects of fresh gas flow on delivered tidal volume mechanical difficulty of setting a small tidal volume using an adult bellows asembly Because of the greatly increased accuracy in tidal volume delivery achieved through compliance and leak testing and compensation, modern ventilators have an unprecedented tidal volume range. They are able to ventilate smaller patients much more accurately than any previous anesthesia ventilator could (A N E S T H A N A L G 2008;106:1392-1400). This will undoubtedly lessen the need for non-rebreathing (Mapleson & Bain) circuits, and make care safer, since anesthetists will no longer have to disassemble and reconfigure to a non-rebreathing circuit for a child in the middle of several adult cases. However, it is mandatory to substitute a pediatric circuit for tidal volumes less than 200 mL (Anesthesiology 2001;94:543-4) on all ventilators. Smaller filters and a pediatric D-Lite sensor must be used on the ADU for VT < 150 mL. Page 56 Ventilator Tidal volume mL Narkomed 6000 101400 Fabius GS 201400 Apollo 201400 Aestiva 20- [Type text] 1500 C OM P LI AN C E ADU 201400 Aisys 201500 AN D L E AK T E S T I N G The accuracy comes with a price. An electronic leak and compliance test must be repeated every time the circuit is changed, particularly if changing to a circuit with a different configuration (adult circle to pediatric circle, or adult to long circuit). This test is part of the electronic morning checklist. Photograph of the Aestiva flow sensor The placement of the sensor used to compensate tidal volumes for compliance losses and leaks has some interesting consequences. The Aestiva flow sensors are placed between the disposable corrugated breathing circuit limbs and the absorber head. Here they are able to compensate tidal volumes for fresh gas flow, compliance losses and leaks internal to the machine and absorber head- but not in the breathing hoses. Photograph of the D-Lite sensor. The GE D-Lite sensor is placed just distal to the Y-piece on the ADU. In this position, it can compensate for all leaks and compliance losses out to the Y piece (thus including the breathing circuit hoses). However, at this point it adds appreciable and perhaps objectionable bulk and weight close to the patient's face. This may make mask ventilation a bit more cumbersome. Further, a sensor closer to the patient is exposed to more exhaled moisture, but the impact can be lessened with a heat and moisture exchanger between patient and sensor. Unfortunately, this adds further bulk and weight. The Narkomed 6000 tests compliance and leaks of all components to the Y-piece via a pressure transducer within the internal circuitry near the bellows. Here the sensor is relatively protected from moisture. F RESH G AS DECO UPLI NG VERSUS COMPENS ATION A final factor adding to modern ventilator accuracy is that they compensate delivered tidal volume for changes in fresh gas flow (FGF). In traditional ventilators, which are not fresh gas decoupled, the Page 57 [Type text] delivered tidal volume is the sum of the volume delivered from the ventilator bellows, and the fresh gas flow delivered during the inspiratory phase of each breath. Thus, delivered tidal volume may change as FGF is changed. For example, consider a patient with a FGF of 4 L/min, a respiratory rate of 10, inspiratory:expiratory (I:E) ratio of 1:2, and a tidal volume of 700 mL. During each minute, the ventilator spends 20 seconds in inspiratory time and 40 seconds in expiratory time (1:2 ratio). During this 20 seconds, the fresh gas flow is 1,320 mL (4000 mL/min FGF times 1/3). Each of the 10 breaths of 700 mL is augmented by 132 mL of fresh gas flowing while the breath is being delivered, so the total delivered tidal volume is 832 mL/breath. This 19% increase is reasonably unimportant. But what happens if we decrease to lower fresh gas flow? Assume the same parameters, but a FGF of 1,000 mL/min. During each minute, the ventilator spends 20 seconds in inspiratory time and 40 seconds in expiratory time (1:2 ratio). During this 20 seconds, the fresh gas flow is 330 mL (1000 mL/min FGF times 1/3). Each of the 10 breaths of 700 mL is augmented by 33 mL of fresh gas flowing while the breath is being delivered, so the total delivered tidal volume is 733 mL/breath. This means that changing FGF from 4,000 mL/min to 1,000 mL/min, without changing ventilator settings, has resulted in a 14% decrease in delivered tidal volume (832 to 733 mL). It would not be surprising if the end tidal carbon dioxide rose as a result. The situation is more acute with a traditional anesthesia ventilator in children. Assume a 20 kg patient with a FGF of 4 L/min, a respiratory rate of 20, inspiratory:expiratory ratio of 1:2, and a tidal volume of 200 mL. During each minute, the ventilator spends 20 seconds in inspiratory time and 40 seconds in expiratory time (1:2 ratio). During this 20 seconds, the fresh gas flow is 1,320 mL (4000 mL/min FGF times 1/3). Each of the 20 breaths of 200 mL is augmented by 66 mL of fresh gas flowing while the breath is being delivered, so the total delivered tidal volume is 266 mL/breath. This is a 33% increase above what is set on the ventilator. We now decrease the FGF from 4 to 1 L/min for the same 20 kg child, (RR 20, I:E ratio of 1:2, and VT 200 mL). During each minute, the ventilator spends 20 seconds in inspiratory time and 40 seconds in expiratory time (1:2 ratio). During this 20 seconds, the fresh gas flow is 333 mL (1000 mL/min FGF times 1/3). Each of the 20 breaths of 200 mL is augmented by 16.5 mL of fresh gas flowing while the breath is being delivered, so the total delivered tidal volume is 216 mL/breath. This is a 23% decrease in VT (266 to 216 mL/breath) caused solely by changing FGF, and without altering vent settings. Page 58 [Type text] Fabius GS ventilator schematic. There are two approaches to dealing with the problem. The Dräger Apollo, Narkomed 6000 and Fabius GS use fresh gas decoupling. Fresh gas is diverted by a decoupling valve to the manual breathing bag, and is thus not added to the delivered tidal volume. Thus, fresh gas decoupling helps ensure that the set and delivered tidal volumes are equal. This is most clearly visualized by visiting the Virtual Fabius GS Simulation. The action of the piston closes a one-way (decoupling) valve, diverting FGF to the manual breathing bag during the inspiratory cycle. The visual appearance is unusual: the manual breathing bag, normally quiescent during mechanical ventilation, moves with each breath the manual breathing bag movement is opposite to the movement seen in a mechanical ventilator bellows- the manual breathing bag inflates during inspiration (due to fresh gas flow), and deflates during expiration as the contents empty into the absorbent and move on towards the patient. With fresh gas decoupling, if there is a disconnect, the manual breathing bag rapidly deflates, since piston retraction draws gas from it. The second approach is fresh gas compensation, which is utilized in the Aisys, Aestiva, Avance, Aespire, and ADU. The volume and flow sensors provide feedback which allows the ventilator to adjust the delivered tidal volume so that it matches the set tidal volume, in spite of changes in the total fresh gas flow. S U I T AB I LI T Y F OR L O W F L OW S Low fresh gas flow is desirable to reduce pollution and cost of volatile agents and nitrous oxide, preserve tracheal heat and moisture, prevent soda lime granules from drying, and preserve patient body temperature. Factors which enhance the safety and efficiency of low flows in modern ventilators include: o Compliance and leak testing Automatic leak detection Fresh gas compensation or decoupling Warmed absorber heads (NM 6000) Accumulation of condensed exhaled water vapor is a problem for most breathing circuits. Use of low flows can make the problem more acute. Page 59 [Type text] o o Low volume absorber heads allows faster equilibration of dialed and delivered agent concentration Apollo 1500 mL canister NM 6000 1500 mL canister Fabius GS 1500 mL (2800 mL + bag for entire breathing system) ADU 750 mL canister Aisys, AVance, Aespire 800 g absorbent (entire breathing circuit volume 2.7 L including absorbent in mechanical ventilator mode, 1.2 L in bag mode) As you can see, a traditional sized absorber head like the Aestiva (2700 mL in canisters alone) is roughly twice the volume of any of the newer designs. Low fresh gas flows allowed by gas machine- most no longer have mandatory minimum oxygen flows of 200-300 mL/min Electronic detection of bellows not filling (Julian) Low flow wizard- an electronic monitor that gives indications when fresh gas flow is excessive or too low by monitoring gas volume passing through the scavenger (Apollo, NM 6000) C URRENT MODELS D R ÄG E R D I V AN V E N T I L AT O R NM 6000 piston bellows and ventilator controls (front panel). Divan Controls (front panel). The Dräger Divan ventilator is a modern ventilator, offering features such as: pressure control mode, SIMV, correction for compliance losses, and integrated electronic PEEP. Unlike the ADU, newer Dräger absorber heads warm the gases in the breathing circuit. Also unique is that fresh gas flow does not add to delivered tidal volume ("fresh gas decoupling"- see New features above on this page). The Divan is limited to a pressure of 70 cm water- so it cannot ventilate patients in VCV mode beyond this pressure (although, again, it is possible and even perhaps preferable to ventilate the ARDS patient with pressure control mode). It is installed on the Narkomed 6000/6400. Unlike most other anesthesia ventilators, there are no visible bellows on the NM6000 Divan ventilator. It is unique among current models in having a horizontal piston which is hidden within the writing surface of the gas machine. To provide a visible indication of lung inflation, fresh gas is diverted to the manual breathing bag, which inflates during mechanical ventilator inspiration, and deflates during expiration. A disconnect will cause the manual breathing bag to gradually lose volume (in addition to activating other apnea alarms). A pressure transducer within the ventilator measures compliance losses and leaks in the total breathing circuit (absorber head and corrugated limbs). Page 60 [Type text] The Fabius GS has a piston ventilator as well, but the piston is mounted vertically to the left of the flowmeters and is visible through a window. D R Ä G E R F A B I U S GS V E N TI L A TO R Fabius GS ventilator controls and piston window (left of flowmeters). The Fabius GS ventilator is an electronically controlled, electrically driven piston ventilator. It consumes no drive gas. The piston is continuously visible. Operating parameters include VT 20-1400 mL Freq 4-60 bpm I:E ratio 4:1 to 1:4 Inspiratory Pause 0-50% PEEP to 20 cm H2O Adjustable Peak flow, plateau time, insp flow (max 75 L/min) Pressure limit 15-70 cm H2O Inspiratory pressure (pressure control mode) 5-60 cm H2O Inspiratory flow (pressure control mode) 10-75 L/min Page 61 [Type text] D R ÄG E R A P O L L O Apollo. Apollo controls The Apollo is a modern piston ventilator with spirometry monitoring. It is electrically driven and electronically controlled, fresh gas decoupled. Ventilation modes Manual, spontaneous, VCV, PCV, SIMV-Vol, SIMV-PC, PSV. Optional/Synchronization: Pressure Support (PS). VT 20-1400 mL Freq 3-80 bpm I:E ratio 5:1 (max) Inspiratory Pause 0-60% PEEP to 20 cm H2O Adjustable Peak flow, plateau time Pressure limit 70 cm H2O Inspiratory flow (pressure control mode) up to 150 L/min . O LDE R O R OB S OLE T E M OD E LS A 2004 document called "Guidelines for determining anesthesia machine obsolescence" is available. The link is under the heading "Anesthesia Machine" at ASA Standards, Guidelines and Statements. D R ÄG E R AV-E AN D AV-2 AV2 controls Classification: pneumatically and electrically powered, double circuit, pneumatically driven, ascending bellows, time cycled, electronically controlled, VT-preset vent. Incorporates Pressure Limit Controller (PLC) which allows maximum peak inspiratory pressure (PIP) Page 62 [Type text] adjustment from 10-110 cm water. Inspiratory flow control must be set properly (like the Ohmeda 7800), so that driving gas flow does not create an inspiratory pause. Standard on Narkomed 2A, 2B, 2C, 3, 4, and Narkomed (not Fabius) GS. O H M E D A 7000 Ohmeda 7000 controls Same classification as Dräger AV-E E X C E P T it is minute-volume preset (unique among anesthesia ventilators). VT C AN N O T be set directly, it is calculated from settings of VE and respiratory rate (VE = RR x VT). Inspiratory flow stops when set VT worth of driving gas has been delivered to the driving circuit side of the bellows chamber or if pressure greater than 65 cm water is attained. Thus, a patient requiring peak inspiratory pressure > 65 cm water cannot be mechanically ventilated with this ventilator. O HM E D A 7800 Ohmeda 7800 controls This ventilator or the older Ohmeda 7900 Smart-VentTM were standard on newer Excel or Modulus machines. Same classification as Dräger AV2 ventilator; VT preset. Tidal volume, respiratory rate, inspiratory flow and pressure limit controls are present. O LDER O HM ED A 7900 "S M ART V ENT " Ohmeda 7900 controls. Same classification as Dräger AV ventilator, VT preset. Microprocessor control delivers set VT, in spite of changes in fresh gas flow, small leaks, and absorber or bellows compliance losses proximal to the sensors. These flow sensors are placed between corrugated plastic breathing circuit and the absorber head, in both limbs. These are connected to pressure transducers in the ventilator. Compliance Page 63 [Type text] losses in the breathing circuit corrugated hoses are not corrected, but these are a relatively small portion of compliance losses. The first "modern" ventilator- it offered such desirable features as integrated electronic PEEP control, and pressure-controlled ventilation (PCV) mode. It has been reported that the sensors can be quite sensitive to humidity, causing ventilator inaccuracy or outright failure. The problem may be more likely when active airway humidifiers are used- read more at: Anesth Analg 1998;86:231-2 Anesth Analg 1999;88:234 Anesth Analg 2002;96:766-8 Controls are similar to the 7800. Users should be vigilant for cracked tubing in the flow sensors, which are located where the breathing circuit corrugated hoses attach to the absorber head. Leaks here have been reported to cause inability to ventilate, either mechanically or manually. When these failures occur, the ventilator may indicate alarm messages like "VT" or "Apnea", rather than "Check sensor". Flow sensor tubing must be vertical, must be changed regularly, and sensors must be in the proper side (inspiratory or expiratory). Although the sensor plugs are keyed by size and shape, if both sensors come off the absorber head when the circuit is changed they can be inadvertently replaced on the wrong side. C HAPTER 7 : S CAVENGING AND W ASTE A NESTHETIC G ASES (WAG S ) Definition Scavenging is the collection and removal of vented anesthetic gases from the OR. Since the amount of anesthetic gas supplied usually far exceeds the amount necessary for the patient, OR pollution is decreased by scavenging. If a fresh gas flow-sized volume enters the breathing circuit each minute, the same flow must leave it, or barotrauma will result. Scavenger and operating room ventilation efficiency are the two most important factors in reduction of waste anesthetic gases (WAGs). T YPES Scavenging may be active (suction applied) or passive (waste gases proceed passively down corrugated tubing through the room ventilation exhaust grill of the OR). Active systems require a means to protect the patient's airway from the application of suction, or buildup of positive pressure. Passive systems require that the patient be protected from positive pressure buildup only. Another important distinction is that scavenger interfaces may be open (to the atmosphere) or closed (gases within the interface may communicate with the atmosphere only through valves; the older type). The different types of interface have clinical implications. Clearly, open interfaces are safer for the patient. From being relatively unknown 10 years ago, they are becoming almost universal on new equipment, so patient (and anesthetists') safety demands user's attention to the distinctions. Open interfaces are found on most newer gas machines (e.g. Aisys, Apollo, Fabius GS, ADU). Aestiva may have an open or closed interface. Page 64 [Type text] P R ACTICE GUIDELI NES JCAHO requires scavenging. AANA published recommendations in 1992, available through the Bookstore at AANA). ASA published WAGs guideline and fact sheet. NIOSH recommendation to OSHA: Workers should not be exposed to an eight hour time-weighted average of > 2 ppm halogenated agents (not > 0.5 ppm if nitrous oxide is in use) or > 25 ppm nitrous oxide. C OMPONENTS OF THE SC AVENGER SYSTEM 1. 2. 3. 4. Gas collection assembly, (tubes connected to APL and vent relief valve) Transfer tubing (19 or 30 mm, sometimes yellow color-coded) Scavenging interface Gas disposal tubing (carries gas from interface to disposal assembly) 5. Gas disposal assembly (active or passive - active most common, uses the hospital suction system). The scavenger interface is the most important component. It protects the breathing circuit from excess positive or negative pressure. Positive-pressure relief is mandatory to vent excess gas in case of occlusion distal to a closed interface. If active disposal system, must have negative pressure relief as well. Reservoir highly desirable with active systems. Dräger open scavenging interface Dräger open scavenging interface Page 65 [Type text] Diagram of the closed scavenging interface (Ohmeda). Inset: external appearance of the interface. Interfaces can be open or closed types. Open interface has no valves, and is open to atmosphere (allows both negative and positive pressure relief). Should be used O N L Y with active systems. Keep the suction indicator between the white etched lines. Remember that hissing from an open interface is normal- there is no audible indication of waste gas leaks. While safer for the patient (no hazard of positive or negative pressure being applied to the airway as a result of scavenger failure), the risk of occupational exposure for providers ignorant of their proper use is higher with the open interface (Anesth Analg 1992;75:1073). Closed interface communicates with atmosphere only through valves. Should adjust vacuum so that reservoir bag neither flat not over-distended. H AZ AR DS OF S C AV E N G I N G Obstruction distal to interface causes barotrauma or excess negative pressure (action: disconnect gas collection tubing from back of popoff valve [APL], or turn off suction at scavenger interface). Occupational exposure Barotrauma or inability to ventilate C ONTROLLING OCCUP ATIO N AL EXPOSURE TO W ASTE ANESTHETI C G ASES EFFECTIVENESS: U N S C A V E N G E D O P E R A T I N G R O O MS S H OW 10-70 P P M H A L O TH A N E , A N D 4003000 P P M N2O. M I N I MA L S C A V E N G I N G B R I N G S TH E S E L E V E L S D O W N TO 1 A N D 60 P P M R E S P E C T I V E L Y ; A D D I N G C A R E F U L A T TE N TI O N T O L E A K S A N D TE C H N I Q U E C A N YI E L D L E V E L S A S L OW A S 0.005 A N D 1 P P M . Avoiding waste gas exposure: Evidence of harm to anesthesia personnel from waste gases is suggestive but unproved (strongest relationship is N2O and reproductive difficulties). There are D E F I N I T E hazards to patients when scavenging systems fail- so consider the scavenger part of the breathing system and check it each day. The smell of gas during a case is abnormal and the cause should be sought. Good technique will also help lessen exposure: Good mask fit Avoid unscavengeable techniques if possible (insufflation) Prevent flow from breathing system into room air (only turn on agent and nitrous oxide after mask is on face, turn them off before suctioning) Page 66 [Type text] Washout anesthetics (into the breathing circuit) at the end of the anesthetic Don’t spill liquid agent Use low flows Use cuffed tracheal tubes when possible Check the machine regularly for leaks Disconnect nitrous oxide pipeline connection at wall at the day’s end (beginning?) Total intravenous anesthesia APPENDIX: Anesthesia Apparatus Checkout Recommendations, 1993 This checkout list or a reasonable equivalent should be conducted before administration of anesthesia. These recommendations are valid only for an anesthesia system that conforms to current and relevant standards and that includes an ascending bellows ventilator and at least the following monitors: capnograph, pulse oximeter, oxygen analyzer, respiratory volume monitor (i.e., spirometer), and breathing system pressure monitor with high-pressure and low-pressure alarms. Users are encouraged to modify these guidelines to accommodate differences in equipment design and variations in local clinical practice. Such local modifications should have appropriate peer review. Users should refer to the operator's manual for the manufacturer's specific procedures and precautions, especially the manufacturer's low-pressure leak test (step 5). EMERGENCY VENTILATION EQUIPMENT *1. Verify Backup Ventilation Equipment Is Available and Functioning HIGH-PRESSURE SYSTEM *2. Check Oxygen Cylinder Supply a. Open O2 cylinder and verify that it is at least half full (about 1000 psi). b. Close cylinder. *3. Check Central Pipeline Supplies a. Check that hoses are connected and that pipeline gauges read about 50 psi. LOW-PRESSURE SYSTEM *4. Check Initial Status of the Low-Pressure System a. Close flow control valves, and turn vaporizers off. b. Check the fill level, and tighten the vaporizers' filler caps. *5. Perform a Leak Check of the Machine's Low-Pressure System a. Verify that the machine master switch and flow control valves are OFF. b. Attach a suction bulb to the common (fresh) gas outlet. c. Squeeze the bulb repeatedly until fully collapsed. d. Verify bulb stays fully collapsed for at least 10 seconds. e. Open one vaporizer at a time, and repeat steps c and d above. f. Remove the suction bulb, and reconnect the frésh gas hose. *6. Turn on the Machine's Master Switch and All Other Necessary Electrical Equipment. *7. Test Flow Meters a. Adjust flow of all gases through their full range, checking for smooth operation of floats and undamaged flow tubes. b. Attempt to create a hypoxic O2 /N2 O mixture, and verify correct changes in the flow and/or alarms. Page 67 [Type text] SCAVENGING SYSTEM *8. Adjust and Check the Scavenging System a. Ensure proper connections between the scavenging system and both the adjustable pressure limiting (APL) (pop-off) valve and the ventilator's relief valve. b. Adjust the waste gas vacuum (if possible). c. Fully open the APL valve and occlude the Y-piece. d. With minimum O2 flow, allow the scavenger reservoir bag to collapse completely, and verify that the absorber pressure gauge reads about zero. e. With the O2 flush activated, allow the scavenger reservoir bag to distend fully, and then verify that absorber pressure gauge reads <10 cm H2 O. BREATHING SYSTEM *9. Calibrate the O 2 Monitor a. Ensure the monitor reads 21% in room air. b. Verify that the low O2 alarm is enabled and functioning. c. Reinstall the sensor in the circuit, and flush the breathing system with O 2 d. Verify that monitor now reads greater than 90%. . 10. Check Initial Status of Breathing System a. Set the selector switch to Bag mode. b. Check that the breathing circuit is complete, undamaged, and unobstructed. c. Verify that the carbon dioxide absorbent is adequate. d. Install the breathing circuit accessory equipment (e.g., humidifier, PEEP valve) to be used during the case. 11. Perform a Leak Check of the Breathing System a. Set all gas flows to zero (or minimum). b. Close the APL (pop-off) valve, and occlude the Y-piece. c. Pressurize the breathing system to about 30 cm H 2 O with an O 2 flush. d. Ensure that pressure remains fixed for at least 10 seconds. e. Open the APL (pop-off) valve, and ensure that the pressure decreases. MANUAL AND AUTOMATIC VENTILATION SYSTEMS 12. Test the Ventilation Systems and Unidirectional Valves a. Place a second breathing bag on the Y-piece. b. Set appropriate ventilator parameters for the next patient. c. Switch to automatic ventilation mode (i.e., Ventilator). d. Turn the ventilator ON, and fill the bellows and breathing bag with an O 2 flush. e. Set the O2 flow to minimum and other gas flows to zero. f. Verify that the bellows deliver an appropriate tidal volume during inspiration and that the bellows fill completely during expiration. g. Set the fresh gas flow to about 5 L/min. h. Verify that the ventilator's bellows and simulated lungs fill and empty appropriately without sustained pressure at end expiration. i. Check for proper action of unidirectional valves. j. Exercise breathing circuit accessories to ensure proper function. k. Turn the ventilator off, and switch to manual ventilation mode (i.e., Bag/APL). l. Ventilate manually, and ensure inflation and deflation of artificial lungs and appropriate feel of system resistance and compliance. m. Remove second breathing bag from the Y-piece. MONITORS 13. Check, Calibrate, and/or Set Alarm Limits of all Monitors Page 68 [Type text] a. Capnometer b. Oxygen analyzer c. Pressure monitor with alarms for high and low airway pressure d. Pulse oximeter e. Respiratory volume monitor (i.e., spirometer) FINAL POSITION 14. Check Final Status of the Machine a. Vaporizers are off. b. APL valve is open. c. Selector is switched to Bag mode. d. All flow meters are set to zero (or minimum). e. Suction level is adequate for the patient. f. Breathing system is ready to use. *If an anesthesia provider uses the same machine in successive cases, these steps need not be repeated or may be abbreviated after the initial checkout. SUMMARY Rapid advances in the anesthesia industry make it increasingly difficult for the anesthesia care provider to keep up with anesthesia machine technology. Nevertheless, a thorough understanding of the machine is mandatory for the safe practice of anesthesia. Machines are equipped with dozens of safety features, but none of them is foolproof. The anesthesia care provider still must check the machine preoperatively using appropriate checkout procedures. . KEY POINTS 1. In the event of a pipeline crossover, two actions must be taken. The backup oxygen cylinder must be on, and the wall supply sources must be disconnected. 2. Fail-safe valves and proportioning systems help minimize delivery of a hypoxic mixture, but they are not foolproof. Delivery of a hypoxic mixture can result from the wrong supply gas, a defective or broken safety device, leaks downstream from the safety devices, inert gas administration, and dilution of the inspired oxygen concentration by high concentrations of inhaled anesthetics. 3. Because of desflurane's low boiling point and high vapor pressure, controlled vaporization of desflurane requires special, sophisticated vaporizers such as the Datex-Ohmeda Tec 6 and the Aladin Cassette Vaporizer. 4. Misfilling an empty variable-bypass vaporizer with desflurane could be catastrophic, resulting in delivery of a hypoxic mixture and a massive overdose of inhaled desflurane anesthetic. 5. Inhaled anesthetics can interact with carbon dioxide absorbents and produce toxic compounds. During sevoflurane anesthesia, compound A can be formed, particularly at low rates of fresh gas flow, and during desflurane anesthesia, carbon monoxide can be produced, particularly with desiccated absorbents. 6. Anesthesia ventilators with ascending bellows (i.e., bellows that ascend during the expiratory phase) are safer than those with descending bellows because disconnections readily manifest with ascending bellows. 7. When using anesthesia ventilators with ascending bellows, during the inspiratory phase, fresh gas flow and oxygen flushing contribute to the patient's tidal volume because the ventilator's relief valve is closed. Oxygen flushing during the inspiratory phase can cause barotrauma, particularly in pediatric patients. The anesthesiologist must never activate the oxygen flush during the inspiratory phase of mechanical ventilation. 8. New ventilators that use FGD technology virtually eliminate the possibility of barotrauma by Page 69 [Type text] oxygen flushing during the inspiratory phase because fresh gas flow and oxygen flush flow are diverted to the reservoir breathing bag. However, if the breathing bag has a leak or is absent, the patient may become aware while under anesthesia, and a lower than expected oxygen concentration may be delivered because of entrainment of room air. 9. With newer Ohmeda anesthetic ventilators such as the 7100 and 7900 SmartVent, the gas from the patient and the drive gas are scavenged, resulting in substantially increased volumes of scavenged gas. The scavenging systems must be set appropriately to accommodate the increased volume, or pollution of the operating room environment can result. 10. The low-pressure circuit is the vulnerable area of the anesthesia machine because it is most subject to breakage and leaks. The low-pressure circuit is located downstream from all anesthesia machine safety features except the oxygen analyzer, and it is the portion of the machine that is missed if an inappropriate leak test for a low-pressure circuit is performed. 11. It is mandatory to check the low-pressure circuit for leaks before an anesthetic is delivered because leaks in the circuit can cause delivery of a hypoxic mixture or cause the patient to become aware during anesthesia, or both. 12. Because most Ohmeda anesthesia machines have a one-way check valve in the low-pressure circuit, a negative-pressure leak test is required to detect leaks. A positive-pressure leak test cannot detect leaks in the low-pressure circuit of most Datex-Ohmeda products. 13. Internal vaporizer leaks can be detected only with the vaporizer turned on. 14. Before an anesthetic is administered, the circle system must be checked for leaks and for flow. To test for leaks, the circle system is pressurized to 30 cm H O, and the circle system's airway pressure gauge is observed (i.e., static test). To check for appropriate flow to rule out obstructions and faulty valves, the ventilator and a test lung (e.g., breathing bag) are used (i.e., dynamic test). 15. Newer anesthesia workstation self-tests do not detect internal vaporizer leaks unless each vaporizer is individually turned on during the self-test. Page 70 [Type text] Reference list : Miller: miller,s Anesthesia 7th edition 2009 Ronald D miller Editor consulting Editors Roy F Cucchiara Edward D. Miller,Jr. J.G.Reves Michael F. Roizen JohnJ. Savarese. T H E AN E S T H E S I A G AS M AC H I N E R E V S E D J U L Y MICHAEL P . DOS CH CRNA PHD 2 01 2 university of Detroit Mercy Graduate Program in Nurse Anesthesiology This site is http://www.udmercy . edu/cma/ag Small, MR (1962). Oliver Wendell Holmes. New York: Twayne Publishers. p. 55. ISBN 978-0-8084-0237-4. OCLC 273508. "In a letter to dentist William T. G. Morton, Holmes wrote: "Everybody wants to have a hand in a great discovery. Serturner FWA (1817). Gilbert's Ann. d. Physik. 25, 56-89. Serturner FWA (1806). J. Pharm. f. Arzte. Apoth. Chem. 14, 47-93. Powell MA (1996). "9: Wine and the vine in ancient Mesopotamia: the cuneiform evidence". In McGovern PE, Fleming SJ, Katz SH. The origins and ancient history of wine (Food and nutrition in history and anthropology). 11 (1 ed.). Amsterdam: Gordon and Breach Publishers. pp. 96–124. ISBN 978-90-5699-552-2. ISSN 0275-5769. http://books.google.com/?id=aXX2UcT_yw8C&pg=PA97&lpg=PA97&dq=Wine+and+the+vine+in+ancient+Mesopota mia:+the+cuneiform+evidence#v=onepage&q=Wine%20and%20the%20vine%20in%20ancient%20Mesopotamia%3 A%20the%20cuneiform%20evidence&f=false. Retrieved 2010-09-15. Evans, TC (1928). "The opium question, with special reference to Persia (book review)". Transactions of the Royal Society of Tropical Medicine and Hygiene 21 (4): 339. doi:10.1016/S0035-9203(28)90031-0. http://www.tropicalmedandhygienejrnl.net/article/S0035-9203(28)90031-0/abstract. Retrieved 2010-09-18. ""The earliest known mention of the poppy is in the language of the Sumerians, a non-Semitic people who descended from the uplands of Central Asia into Southern Mesopotamia Booth M (1996). "The discovery of dreams". Opium: A History. London: Simon & Schuster, Ltd.. p. 15. ISBN 0-31220667-4. http://books.google.com/?id=8XHV8JAoAi4C&dq=Opium:+A+History&printsec=frontcover#v=onepage&q&f=false . Retrieved 2010-09-18. Krikorian, AD (1975). "Were the opium poppy and opium known in the ancient Near East?". Journal of the History of Biology 8 (1): 95–114. doi:10.1007/BF00129597. PMID 11609871. Chu NS (2004). "Legendary Hwa Tuo's surgery under general anesthesia in the second century China" (in Chinese). Acta Neurol Taiwan 13 (4): 211–6. ISSN 1028-768X. PMID 15666698. http://www.neuro.org.tw/magz/doc/134p211.pdf. Retrieved 2010-09-18. Chen J (2008). "A Brief Biography of Hua Tuo". Acupuncture Today 9 (8). ISSN 1526-7784. http://www.dynamicchiropractic.com/mpacms/at/article.php?id=31781. Retrieved 2010-09-18. Meyer, K (2004). "Dem Morphin auf der Spur" (in German). Pharmazeutischen Zeitung. GOVI-Verlag. http://www.pharmazeutische-zeitung.de/index.php?id=26551. Retrieved 2012-06-12. Page 71 [Type text] ., . . Page 72 [Type text] Page 73 [Type text] . - . Page 74 [Type text] . . Page 75 [Type text] . , . . Page 76 [Type text] Page 77 [Type text]