polymyositis and dermatomyositis (pm & dm)
advertisement
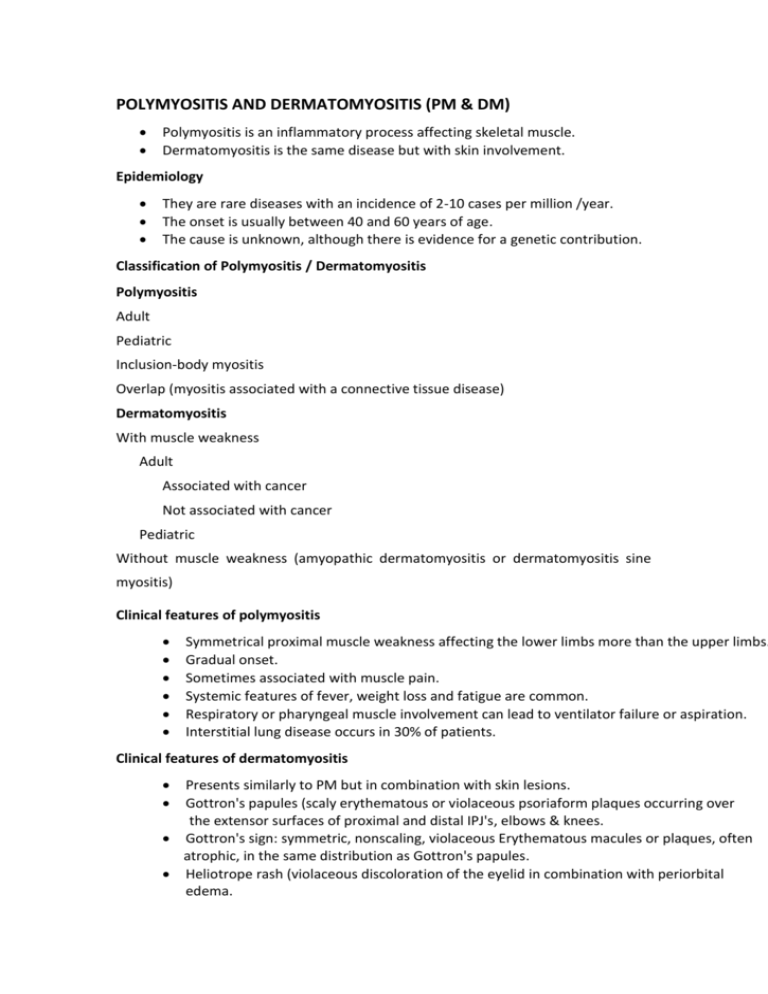
POLYMYOSITIS AND DERMATOMYOSITIS (PM & DM) Polymyositis is an inflammatory process affecting skeletal muscle. Dermatomyositis is the same disease but with skin involvement. Epidemiology They are rare diseases with an incidence of 2-10 cases per million /year. The onset is usually between 40 and 60 years of age. The cause is unknown, although there is evidence for a genetic contribution. Classification of Polymyositis / Dermatomyositis Polymyositis Adult Pediatric Inclusion-body myositis Overlap (myositis associated with a connective tissue disease) Dermatomyositis With muscle weakness Adult Associated with cancer Not associated with cancer Pediatric Without muscle weakness (amyopathic dermatomyositis or dermatomyositis sine myositis) Clinical features of polymyositis Symmetrical proximal muscle weakness affecting the lower limbs more than the upper limbs. Gradual onset. Sometimes associated with muscle pain. Systemic features of fever, weight loss and fatigue are common. Respiratory or pharyngeal muscle involvement can lead to ventilator failure or aspiration. Interstitial lung disease occurs in 30% of patients. Clinical features of dermatomyositis Presents similarly to PM but in combination with skin lesions. Gottron's papules (scaly erythematous or violaceous psoriaform plaques occurring over the extensor surfaces of proximal and distal IPJ's, elbows & knees. Gottron's sign: symmetric, nonscaling, violaceous Erythematous macules or plaques, often atrophic, in the same distribution as Gottron's papules. Heliotrope rash (violaceous discoloration of the eyelid in combination with periorbital edema. Rash on the upper back, chest and shoulders (shawl distribution). There is about a three-fold increased risk of malignancy in patients with DM & PM. Systemic Manifestations and Complications of Polymyositis and Dermatomyositis -----------------------------------------------------------------------------------------------------------------------Systemic manifestations Common: proximal muscle weakness, dysphonia, dysphagia Less common: respiratory muscle weakness, visual changes, abdominal pain Systemic complications/associations Cardiomyopathy Cardiac conduction defects Aspiration pneumonia secondary to respiratory muscle weakness Diffuse interstitial pneumonitis/fibrosis Large-bowel infarction secondary to vasculopathy has occurred in juvenile patients with myositis Muscle atrophy Muscle calcification Ocular complications including iritis, nystagmus, cotton-wool spots, optic atrophy, conjunctival edema and pseudopolyposis Internal malignancy Investigations ---------------------------------------------------------------------------------------------------------------------------------Muscle enzyme elevation Serum creatine phosphokinase (CPK), aldolase, ALT and LDH Autoantibodies ANA levels: elevated in 60 to 80 percent of patients with classic DM/PM Antisynthetase antibodies Jo-1: most common antisynthetase found; 20 percent of patients with DM may have positive result ESR: elevated in approximately 50 percent of patients, does not correlate well with disease activity Rheumatoid factor: elevated in 20 percent of patients, most often in those with overlap syndromes EMG: myopathic pattern, 10 percent are false-negative Muscle biopsy: fiber necrosis, regeneration and inflammatory cell infiltrate Screening for underlying malignancy (chest / abdomen / pelvis CT, gastrointestinal tract imaging and mammography for women) Treatment Modalities for Dermatomyositis Treatment modality Oral prednisone Dosage 0.5 to 1.5 mg per kg Side effects Gastrointestinal Comments Initial daily until serum symptoms, adrenal pharmacologic creatine kinase suppression, agent; consider normalizes, then slowly immunosuppression, adjunctive therapy if taper over 12 months avascular necrosis, no improvement in osteoporosis objective muscle strength after three months of therapy. Methotrexate Oral: 7.5 to 10 mg per Stomatitis, hepatic First-line adjuvant week, increased by 2.5 fibrosis, cirrhosis, therapy in patients mg per week to total of nausea, abdominal unresponsive to 25 mg per pain, neutropenia, steroids. weekIntravenous: 10 thrombocytopenia, mg per week, increased pruritus, fever, by 2.5 mg per week to pneumonitis, and total of 0.5 to 0.8 mg gastrointestinal per kg Children: 1 mg symptoms per kg. As dosage increases, taper off steroid dose. Give 3 mg daily of folic acid to minimize side effects of methotrexate. Azathioprine 2 to 3 mg per kg per Lymphoma, nausea, day tapered to 1 mg per vomiting, hepatotoxicity, kg per day once steroid leukopenia, oral ulcers, is tapered to 15 mg per thrombocytopenia day. Reduce dosage monthly by 25-mg intervals. Maintenance dosage is 50 mg per day. Cyclophosphamide Oral: 1 to 3 mg per kg Increased risk for In refractory cases per dayIntravenous: 2 malignancy, leukopenia, only to 4 mg per kg per day, thrombocytopenia, in conjunction with hemorrhagic cystitis, prednisone anorexia, nausea, vomiting, alopecia, sterility, congestive heart failure and stomatitis Treatment modality Mycophenolate Dosage 2 g /day Side effects Bone marrow Comments suppression, Mofetil hepatotoxicity Cyclosporine 2.5 to 10 mg per kg per day* Impairs T-cell proliferation; nephrotoxicity, lymphoma, hypertension, hypertrichosis, gingival hyperplasia, hepatotoxicity, paresthesias, fatigue, hyperesthesias, depression and seizures Hydroxychloroquine 200 mg twice daily in Myopathy, differentiated Adjunctive adults; 2 to 5 mg per kg by biopsy; hematologic treatment to reduce per day in children rash toxicity, hepatotoxicity, antimalarial retinopathy, dizziness, ataxia and weight loss Intravenous 2 g per kg in divided Pancytopenia, death, Showed immunoglobulin doses once per month lymphoma improvement in 70 for three months percent of patients; limited by high cost Topical steroids Physical therapy Class I (super-high — For further control of potency) or class II the erythematous (high potency) topical and pruritic skin steroid is recommended changes — — Directed at preventing atrophy andcontractures; technique should focus initially on passive stretching and splinting; more aggressive strengthbuilding therapy once inflammation is controlled Treatment modality Sun avoidance Dosage — Side effects — Comments Broad-spectrum sunscreen, protective clothing, avoiding ultraviolet light exposure SJOGREN'S SYNDROME (SS) Sjogren's syndrome is a chronic, slowly progressive, inflammatory autoimmune disorder characterized by the infiltration of lymphocytes (T-cells in the majority of cases), monocytes and plasma cells into the parotid (salivary) glands and lacrimal (tear) glands. This chronic lymphocytic infiltration interferes with the normal function of these glands and eventually results in a significant reduction or cessation in the production and secretion of saliva and tears. The condition is named after Henry Sjogren, an ophthalmologist, who first described the primary clinical features of this disorder in 1933. In approximately 40% of patients, Sjogren's syndrome progresses beyond the exocrine glands and systemic (extraglandular) features develop. Classification Two distinct forms of Sjogren's syndrome have been recognized: Primary Sjogren's syndrome - defined as dry eye and dry mouth that occurs by itself and is not associated with another autoimmune disorder. Primary Sjogren's syndrome occurs in approximately 50% of cases Secondary Sjogren's syndrome - characterized by dry eye and dry mouth that occurs in the presence of a major underlying autoimmune disease such as rheumatoid arthritis, systemic lupus erythematosus, scleroderma, primary biliary cirrhosis, chronic active hepatitis, or myasthenia gravis. Epidemiology The overall prevalence of Sjogren's syndrome in the general population has been estimated to range from 0.5% to 3%. Sjogren's syndrome is a condition that affects primarily women with a female to male ratio of about 9:1. Symptoms of the disorder most often begin between the ages of 40-60. Pathogenesis The theories regarding the underlying causes of Sjogren's syndrome include: o Chronic inflammation o Cellular apoptosis (self-death of a cell) o Autonomic nervous system dysfunction o Neurotransmitter abnormality o Genetic predisposition (HLA-B8/DR3 association) Clinical features The classic signs and symptoms of Sjogren's syndrome affecting the oral cavity (dry mouth, patients need water to swallow food) and the eyes (dry eye, conjunctivitis, blepharitis and filamentary keratitis). The signs and symptoms of Sjogren's syndrome that affects other areas of the body, known as systemic or extraglandular features of Sjogren's, which may include: o Salivary gland enlargement o Non-erosive arthritis o Raynaud's phenomenon o Fatigue o Low-grade fever o Interstitial lung disease o Cryoglobulinemia, Vasculitis o Peripheral neuropathy o Lymphadenopathy o Lymphoreticular lymphoma o Glomerulonephritis o Renal tubular acidosis Investigations - Anemia, leucopenia, thrombocytopenia - High ESR, hypergammaglobulinemia - Patients typically have a positive ANA, RF, anti SS-A (anti-Ro) and anti SS-B (anti-La) antibodies. - Special laboratory tests that are used to confirm the diagnosis of Sjogren's syndrome that are designed to measure abnormalities in the production of saliva and tears (Srmer tear test, Rose Bengal staining). - Lip biopsy Treatment Currently there is no known cure for Sjogren's syndrome. The major goals of treatment are to control the symptoms and prevent or limit the involvement of other organs of the body. The treatment options that are available to better manage the symptoms associated with dry mouth, including: o Saliva substitutes o Saliva stimulants (sugar-free chewing gum or lozenges) o Good oral hygiene practices o Lifestyle modifications The treatment options that are available to better manage dry eye symptoms, including: o Artificial tears o Methylcellulose inserts o Eye ointments o Soft contact lenses o Muscarinic agonist drugs o Punctual occlusion surgery The treatment options for the management of patients with Sjogren's syndrome who manifest systemic or extraglandular involvement of other body organs such as the skin, joints, lungs, kidney or nervous system. Steroids Immunosuppressive drugs