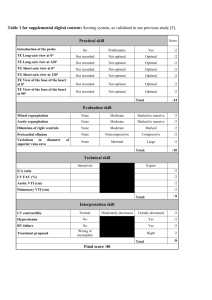
Simple tests
advertisement

Simple tests 1. The pain of peptic ulcer disease characterized by A. * arise through 1,5-2 h, gradually increases as the evacuation of the contents of the stomach arise through 0,5-1 h, gradually picking up, is stored within 1,5-2 h, the decrease and disappear as the intestinal contents is moved into duodenal ulcer B. C. arise through 2,5-4 hours, disappearing after a meal D. arise in 4-6 hours, gradually increases as the evacuation of the contents of the stomach E. occur at night 2. Night pain in peptic ulcer disease characterized by A. * arise through 2,5-4 hours, disappearing after a meal B. arise through 1,5-2 h, gradually increases as the evacuation of the contents of the stomach arise through 0,5-1 h, gradually picking up, is stored within 1,5-2 h, the decrease and disappear as the intestinal contents is moved into duodenal ulcer C. D. arise in 4-6 hours, gradually increases as the evacuation of the contents of the stomach E. occur during the day 3. Diet for gastritis type A A. 2,4,15 B. 5,9,15 C. 5,11,15 D. 9,11,15 E. * 1,2, 15 4. In the treatment of chronic gastritis type which B blockers are used A. * All of the above B. Omeprazole C. Lansoprazole D. Pantoprazole E. Rabeprazole 5. Diet for GERD A. * number 1 B. 2 C. 4 D. 5 E. 9 6. Breath test for determination of Helicobacter pylori is effective for A. * Noninvasive monitoring the effectiveness of Helicobacter therapy B. Invasive monitoring the effectiveness of Helicobacter therapy C. Non-invasive selection of drugs Helicobacter therapy D. Invasive selection of drug therapy of Helicobacter E. All the above listed 7. Breath test for determination of Helicobacter pylori based on A. * Urease activity B. Protease activity C. Activity of citrate D. Carbonate activity E. Inactivity Which infectious agent plays an important role in the pathogenesis of chronic gastritis and peptic ulcer disease? 8. A. Yersinia B. Klebsiella C. Clostridia D. * Helicobacter E. Salmonella 9. Factors that increase resistance of gastric mucosa include: A. * All of the above B. Proteins of gastric mucus C. The local immunity and microcirculation D. Small doses of gastrin and histamine E. Level prostaglandines in mucous membrane of the stomach 10. Among the factors that reduce resistance of gastric mucosa include: A. * All of the above B. bile acid C. Lisoletsitin D. Hydrochloric acid E. Pepsin 11. The most typical complaints for diseases of the stomach: A. * Pain in epigastrium B. Dysphagia and burping C. Bitter taste in the mouth D. Vomiting E. Pain around the navel 12. Increased appetite occurs: A. * All listed correctly B. during a duodenal ulcer C. In chronic gastritis improve the acidogenic function of the stomach D. In diabetes E. during insulomy 13. Sour morning vomiting is characteristic: A. * Diseases that are accompanied by night hypersecretion (peptic ulcer) B. Cholelithiasis C. Hypertensive disease D. Conventional vomiting E. Cancer of the stomach body 14. Sanatorium treatment in gastroenterological profile is shown at: A. * chronic gastroduodenitis in remission B. chronic gastroduodenitis in acute phase C. Barrett esophagus D. peptic ulcer in acute phase E. acute erosive gastritis 15. How long will the patient with stomach disease have surgeries? A. 1 year B. 2 years C. * Lifelong D. 3 years E. 5 years Patient feels "hungry", has epigastric pain at night, nausea. There is a seasonal exacerbation of the disease (spring-falling).Which diagnostic methods are the most informative in this case? 16. A. * Fibrogastroduodenoscopy with biopsy B. X-ray of the stomach with barium C. Cholecystography D. intragastral pH-metry E. Duodenal intubation The patient complains of feeling heaviness in the epigastrium, belching, nausea. An objective study on an empty stomach in the stomach is determined by a splashing sound. What does the presence of a splashing noise on an empty stomach make us suspect? 17. A. * fasting hypersecretion . B. hyposecretion. C. strengthening the gastric motility. D. ventroptosia. E. an inflammatory process in the stomach 18. In what sequence should be carried out deep palpation of the bowel? A. sigmoid, cecum, iliac, lumbar-colon, ascending, descending, B. iliac, sigmoid, ascending, transverse colon, descending and cecum. C. sigmoid, cecum, iliac, ascending, transverse colon, descending. D. iliac, ascending, descending, sigmoid, cecum, lumbar-colon. E. * sigmoid, cecum, iliac, ascending, descending, lumbar-colon 19. Which climate is more favorable for treatment of bronchial asthma? A. warm, dry climate B. hot, dry desert climate C. * high mid mountain climate D. sea and warm climate E. forest and warm climate 20. In assessing the performance of patients with asthma which of the following should be considered: A. etiology of asthma B. weight C. respiratory function in period between attacks D. profession and working conditions E. * all of the above 21. Which factors increase the likelihood of acute bronchitis? A. young age, obesity B. cardiovascular disease, diabetes C. older age, tobacco smoking D. physical or mental exhaustion E. * tobacco smoking, alcohol abuse, infection of nasopharynx Into which forms is acute bronchitis divided according to the nature of the inflammatory process in the bronchi? 22. A. * catarrhal, purulent B. fibrinous, catarrhal C. atrophic, catarrhal D. fibrinous, purulent E. putrid, atrophic 23. Into which forms of acute bronchitis is divided according to the nature of violation of ventilation? A. * obstructive, nonobstructive B. restrictive, catarrhal C. nonobstructive, restrictive D. catarrahal, nonobstructive E. obstructive, restrictive 24. What are clinical forms of acute bronchitis? A. acute, recurrent B. * acute, protracted, recurrent C. acute, protracted, chronic D. protracted, recurrent E. chronic, relapsing 25. In obstructive form of acute bronchitis which group of antibiotics should be prescribed ? A. penicillin, aminoglycosides B. aminoglycosides, broad-spectrum penicillins C. * macrolides, tetracyclines D. nitrofurans, sulphonamides E. macrolides nifurans 26. Is glucocorticoid therapy necessary for acute bronchitis? A. Yes, in patients with recurrent disease B. * Yes, with persistent bronchial obstruction C. Yes, at a purulent inflammation of the bronchi D. No, it is never necessary E. yes, it is mandatory 27. Which way is most effective to introduce corticosteroids for acute bronchitis? A. subcutaneous injection B. * inhalation C. intravenously D. Oral E. intramuscular injection 28. What are the most characteristic complications of the course of acute bronchitis? A. pleurisy, lung abscess B. pneumonia, bronchial asthma C. * pneumonia, chronic bronchitis D. bronchial asthma, pleurisy E. pneumonia, gangrene of the lung 29. Decompensation of chronic pulmonary heart showed all the symptoms except: A. swelling of neck veins B. accent II tone in the pulmonary artery C. * low-grade temperature D. liver enlargement E. swelling of the legs 30. Which x-ray signs are not characteristic for chronic bronchitis: A. net-like pneumosclerosis in the lower parts of the lungs B. * increased bronchopulmonary lymph nodes C. increased transparency of the lung fields D. increase in right heart 31. Complication of chronic bronchitis include: A. * chronic pulmonary and heart emphysema B. pulmonary embolism C. myocardial infarction D. mediostinitis E. spontaneous pneumothorax 32. What is the most likely cause of death of patients with chronic bronchitis: A. * decompensation of cor pulmonale B. myocardial infarction C. Ischemic stroke D. pulmonary embolism E. hemorrhagic stroke 33. Which symptom is not characteristic of chronic bronchitis: A. Cough B. Hemoptysis C. * febrile temperature D. dyspnea E. cyanosis nasolabial triangle 34. If at the beginning of the disease cough is absent, chronic bronchitis is shown with: A. Weakness B. * shortness of breath C. chest pain D. hemoptysis E. fever 35. Who most often suffers from chronic bronchitis? A. young women B. * elderly men C. adolescents of both sexes D. older women E. young men 36. Chronic obstructive bronchitis is complicated by all except: A. Emphysema B. chronic pulmonary heart C. Pulmonary Hypertension D. * exudative pleurisy E. None of the above Which complex of symptoms is characteristic for exacerbation of chronic obstructive bronchitis, catarrhal 37. A. febrile temperature hemoptysis, weakness B. * cough with mucous expectoration, low-grade fever, shortness of breath C. chest pain, headaches, coughing, weakness D. purulent sputum, fever, severe weakness E. removed albuterol asthma, coughing, whistling in the chest 38. Which x-ray signs are not characteristic for emphysema: A. increased transparency of the lung fields B. wide intercostal spaces C. * high position dome of the diaphragm D. increased retrosternal space E. horizontal position rib 39. Select complaints which are typical for chronic bronchitis A. weakness, cough, hemoptysis B. * cough, shortness of breath, phlegm C. chest pain, weight loss, fever D. fever, shortness of breath, cough E. fever, cough, sputum 40. Epidemic outbreak of influenza infection (influenza A) 2-3 years arises from: A. Disappearance of specific antibodies B. * Variability of the virus within its serotype C. Recombination of viruses D. Formation of virus-mutants 41. The most intense flu virus reproduces itself : A. In the elderly B. In middle-aged persons C. * In children D. Age does not matter E. In persons of all ages equally 42. The influenza virus is circulating among the population: A. In the cold season B. Disappears in summer C. Disappears in winter D. * During the whole year E. Spring-autumn period 43. In viral-bacterial complications of influenza which preparation is the most effective: A. Antibiotics B. Sulfonamides C. Immunoglobulins normal human D. * interferon, influenza g / i globuline antibiotics E. Combined vitamin complexes 44. In the treatment of influenza steam inhalation is conducted by: A. * Acidified solution B. Alkaline solutions C. Solutions of neutral environment D. Irrelevant E. Oil solution 45. Causes of viral-bacterial complications of influenza: A. Prolonged virus B. Toxemia C. * Secondary immunodeficiency D. Serotype E. Virus mutation 46. Influenza i-globulin: A. Stimulates the synthesis of specific antibodies B. Stimulates the synthesis of interferon C. * Binds viral antigens D. Increases the body's nonspecific resistance E. - Assigned to prevent bacterial complications 47. Rimantadine for influenza A is appointed: A. * In the first 2-3 days of illness B. Within 5-6 days C. Within 4-5 days D. Not assigned E. Only in combination with antibiotics 48. Laferon during flu : A. Stimulates the synthesis of antibodies B. Stimulates the synthesis of interferon C. Prevents of bacterial complications D. Increases the body's nonspecific resistentnist E. * Has immunomodulatory and anti-viral action 49. Leukocyte alpha-interferon in influenza causes: A. type specific antiviral immunity B. Stimulates humoral immunity C. * Provides antiviral, anti-inflammatory and indirectly disintoxicating action D. Antibacterial action E. Increases the body's nonspecific resistance 50. What explains sensibilizatory and mutagenic action of influenza virus: A. * intracellular viral reproduction B. Absorption of virus on the surface of host cells C. cytologic action of the virus D. Virusemia E. Toxemia 51. Contagiousness of rhinovirus infection: A. * High for all age groups B. Only for young children C. Moderately D. High in elderly E. Not installed 52. Leading syndrome in rinoviral infection is: A. Intoxication B. Tracheobronchitis C. Fever D. * Rhinitis E. Laryngitis 53. Intoxication at rinoviral infection is: A. Pronounced B. NOT present C. * Moderate D. Prolonged E. Has a malignant course 54. The difference between parainfluenza from diphteria croup is that it: A. * Develops acutely B. Develops in stages C. Is accompanied by aphonia D. Is not clinically different E. Accompanied by loss of consciousness 55. Parainfluenza croup is caused by: A. Laryngeal edema B. Inflammation of the mucous membrane C. Accumulation of mucus D. Reflex spasm of muscles E. * All of the above 56. The leading methods of diagnosis of parainfluenza: A. Clinical B. Virologic C. Serologic D. * clinical and serological E. clinical and virologic 57. Diarrhea with adenovirusniy infection: A. Appears as a consequence of toxicity B. Is absent C. Is the primary symptom D. * can be as a variant of clinical forms E. Is due to the activation of secondary microflora 58. Driving mechanism for the transfer of adenoviral conjuctivitis: A. Airborne B. Contact-household C. Retrogradely to the nasolacrimal canal D. * Contact-household and retrogradely to the nasolacrimal canal E. Airborne and contact consumer 59. Hemogram with adenoviral infection shows: A. Leukocytosis, shift to the left of the formula B. Normocytosis, the shift to the left of the formula C. * Normocytosis or moderate leukopenia, relative lymphocytosis D. Leukocytosis, came to the right formula E. Normocytosis, thrombocytopenia 60. The mechanism of infection in various forms of adenoviral infection A. Airborne B. Fecal-oral C. Contact-household D. * All of the above E. None of the above 61. The influenza virus is stable: A. At boiling temperature B. In an acidic medium C. At room temperature D. * At low temperatures E. In neutral environment 62. Most contagious period of influenza: A. Inoculation period B. * The first week of illness C. Period of convalescence D. Period of complications E. The entire period until full recovery 63. Prevention of influenza in the epidemic period, includes provision of: A. Vaccination Stimulators of the synthesis of endogenous interferon, increased the specific resistance of the body and Vaccines B. * C. Antibiotics D. antiviral drugs E. Stimulators of the synthesis of endogenous interferon 64. The course of influenza in an immunological organism: A. * Acute B. Chronic C. Palindromic D. Protracted E. Intermittent 65. Difficulty of influenza infection is affected by: A. Cytopathogenic effect of virus B. * Toxemia and microcirculatory violations C. Tracheobronchitis D. Violation of humoral immunity E. Bronchiolitis 66. Immunity in influenza is: A. Cross B. * Type specific C. Not formed D. Not studied E. Steady 67. Viral-bacterial pneumonia with influenza develops: A. * In any period of illness B. 1 week illness C. At 2 weeks of disease D. At 3 weeks of disease E. Not found 68. Flu symptoms are predominantly seen in: A. Laringitis B. Bronchospasm C. Bronchitis D. * Intoxication and pharyngotracheobronchitis E. Obstruction 69. During severe flu what should be given in the first place A. * Influenza gamma globulin in conjunction with antiviral drugs, antibiotics and pathogenetic therapy B. Antibiotics C. Immunomodulators D. Symptomatic therapy E. Anti-inflammatory therapy 70. During bacterial complications of influenza mainly prescribed A. Nitrofurans B. * Antibiotic drugs C. Sulfanilamides D. antiviral drugs E. Antifungal drugs 71. Para influenza infection clinically is seen by: A. Acute rhinitis B. Tracheobronchitis C. Lymphadenopathy D. * Laryngitis E. Otitis 72. Tactics of the physician during a sore throat: A. Bacteriological examination of microflora, during diphtheria test regardless of antibiotic Bacteriological examination of microflora, during meningococus, microscopy for spirochets of Vincent, before prescribing antibiotics B. * C. Serological survey for diphtheria D. Bacteriological examination is conducted in the presence of plaque E. Bacteriological examination is not necessary 73. Primary prevention of diseases includes: A. Prevent further development of the disease and complications of the disease B. * Prevention of disease and risk factors C. Optimization of lifestyle D. Improving socio-economic conditions E. Health care for the acute inflammatory disease 74. Secondary prevention of diseases includes: A. Prevention of disease and risk factors B. Optimization of lifestyle C. Improving socio-economic conditions D. * Prevent further development and complications of the disease E. Health care for the acute inflammatory disease 75. The main cause of acute bronchitis A. alcoholism B. smoking C. * Acute Respiratory Infection D. overcooling E. diabetes mellitus 76. On auscultation during bronchitis A. absence of sound B. crepitus C. * dry and moist rales D. pleural friction rub E. wheezing 77. In acute bronchitis marked cough with sputum is A. pink frothy B. "Rusty" C. * mucosa -like D. glassy E. yellow-green 78. Complication of chronic bronchitis is A. lung abscess B. pleurisy C. tuberculosis D. * emphysema E. gangrene of the lungs 79. The main clinical sign of non-obstructive bronchitis: A. * Cough B. Dyspnea C. Chest pain D. Hemoptysis E. Diffuse cyanosis 80. For the differential diagnosis of acute bronchitis and pneumonia which test should be: A. * X-rays B. Monitoring of patients during the week C. Bronchoscopy D. Thorough auscultation E. Determining the number of leukocytes and ESR 81. The main clinical symptom of obstructive bronchitis is: A. * Expiratory dyspnea B. Cough C. Chest pain D. Cyanosis E. Hemoptysis 82. A feature of diphtherial bronchitis is: A. Inflammation B. Lack of increase in body temperature C. Asthma by inhalation of house dust D. Kussmaul breathing E. * Fibrinous nature of the inflammation 83. The final stage of measles bronchitis is: A. * Peribronchial sclerosis B. Lung abscess C. Gangrene of lung D. Empyema E. Central cancer 84. Recurrent bronchitis is associated with: A. * Persistent infection and a violation of reactivity B. Exposure to silica dust C. Frequent hypothermia D. Respiratory tract irritation chlorine vapor E. none of the above 85. Toxic bronchitis may be caused by: A. * Pair of nitrogen, chlorine, sulfur B. Smoking, alcohol abuse C. Tuberculous intoxication D. Helminthic infestation E. Dust, which contains silica 86. The main cause of chronic bronchitis: A. * Smoking and occupational hazards (dust, fumes) B. Acute bronchitis C. Infection D. Pathology of nasopharyngeal E. none of the above 87. The most common cause of pneumonia outside of the hospital: A. aurococcus B. * Streptococcus pneumonia C. streptococcus D. pneumococcus Friedlander E. Pseudomonas aeruginosa 88. The beginning of acute pneumonia, as a rule is: A. * Acute B. subacute C. with the presence of prodrome D. stage E. intermittent 89. Chest pain in pneumonia is associated with: A. stimulation of nerve endings of bronchi B. * involvement in the process of pleura C. damage to the pulmonary artery D. stimulation of nerve endings in bronchioles E. irritation of the nerve endings of the alveoli 90. During auscultation in lobar (lesion fraction) pneumonia the following may be heard: A. dry rales B. bubbling rales C. * crepitus D. pleural friction rub E. wheezing 91. At the beginning of the disease cough in lobar pneumonia: A. Is dry B. Sputum has mucopurulent character C. * Sputum is streaked with blood D. sputum is "mouthful" E. sputum is vitreous in nature 92. Adequate treatment in focal pneumonia is observed on X-ray in: A. 5 - 6 days B. * 8 - 10 days C. 15 - 20 days D. 20-25 days E. 30 days 93. To obtain the most reliable results of bacteriological tests, sputum needs to show no later than: A. * 1 hour after separation B. 2 hours after release C. 3 hours after release D. 4 hours after release E. 12 hours after release 94. Treatment of pneumococcal pneumonia should start with: A. Tetracycline B. Erythromycin C. * Penicillin D. Gentamicin E. Chloramphenicol 95. Antibiotics of choice for treatment of staphylococcal pneumonia are: A. Penicillins B. * Cephalosporins C. Gentamicins D. Tetracyclines E. Erythromycins 96. At the beginning of the disease the sputum of staphylococcal pneumonia has: A. mucopurulent sputum character B. sputum with streaked blood C. sputum "mouthful" D. expectoration mucus in nature E. * bloody, like raspberry jelly 97. For the treatment of legionary pneumonia is advisable to prescribe: A. Penicillin B. Streptomycin C. Tetracycline D. * Erythromycin E. Gentamicin 98. For the treatment of pneumonia mucoplazma advisable to prescribe: A. Penicillin B. Streptomycin C. * Tetracycline D. Erythromycin E. Gentamicin 99. Inhalation preparation are initially applied: A. in acute asthma B. * in remission of asthma C. in chronic bronchitis D. at Status asmaticus E. not used in asthma 100. Which groups bronchodilators are aminophylline? A. sympathomimetics B. * xanthine derivatives C. anticholinergics D. Selective b2-agonists, short-acting E. M-short-acting anticholinergics 101. Which drug is more effective for bronchospasm? A. Astmopent B. Alupent C. Ephedrine D. * Salbutamol E. Bromhexine 102. Side effect of ketotifen (Zaditena) is: A. Tachycardia B. high blood pressure C. ulcers of the gastrointestinal tract D. * drowsiness E. bradycardia 103. What disease can be attributed to complication of hormone therapy? A. Pneumonia B. Dystrophy C. lung cancer D. * osteoporosis E. myocardial infarction 104. Furthermore bronchodilatory effect of B-stimulation appears: A. * tachycardia, pain in the heart B. nausea, flatulence C. arthralgia D. dizziness E. diarrhea 105. Chronic administration of dexamethasone, causes: A. psychotic disorders B. manifestations of diabetic C. cardiovascular disorders D. * osteoporotic disorders E. myopathy 106. Key indicators for the appointment of an antihistamine will be: A. bronchial asthma B. asthmatic bronchitis C. * extrapulmonary manifestations of allergy D. rhinitis E. Bacterial conjunctivitis 107. Name the mechanism of action of glucocorticoid's in antiasthmatic effect: A. reducing the number of components of the antigen-antibody B. suppression of antibody production C. reduce the formation of free histamine D. potentiation of sympathomimetic E. * all of the above 108. 40. Eliminate the factor that is unrelated to an increase in the number of patients with asthma? A. increases in chronic nonspecific lung diseases B. allergenic population C. Air pollution D. * congested population E. GMO 109. Which of the following environmental factors form the biological defects in the body: A. pollen of trees, grasses B. viruses, bacteria C. mushrooms D. metal, cotton dust E. * all of the above 110. Exacerbation of atopic asthma arise: A. with sharp inflammation in respiratory organs B. * in contact with non-infectious allergens C. in contact with infectious allergens D. with inflammatory processes in the larynx E. with laryngitis 111. What kind of allergic syndromes often goes along with dusty asthma? A. conjuctival syndrome B. * allergic rhinitis C. urticaria D. Angioedema E. Dermatitis 112. Primary prevention of asthma consists of: A. readjustment of nasopharynx B. rational mode of life C. smoking cessation D. physical education E. * all of the above 113. In healthy individuals the highest bronchial resistance is determined in: A. * morning B. day C. evening D. night E. regardless of time of day 114. Pre-asthmatic state is characterized by: A. the first clear-cut attack or status B. * bronchitis with bronchospasm and allergic manifestations, with lack of specific attacks in patient C. vasomotor rhinitis D. allergic conjunctivitis E. manifestations of food allergy 115. What is the most common allergen of noninfectious allergens? A. * dust B. pollen C. epidermal D. food E. mushrooms 116. With which allergic syndromes Pollen asthma is associated with: A. * rhinitis, conjunctivitis B. urticaria C. migraine D. Angioedema E. Dermatitis 117. If Bronchial asthma is seasonal in nature, what kind of asthma is necessary to think first and foremost: A. Dust B. * pollen C. food D. epidermal E. caused by fungi 118. Excitation of beta 2 adrenergic receptors causes: A. * bronchodilatation B. bronchospasm C. does not affect the tone of the bronchi D. affects the tone bronchioles E. influence on the tone of the alveoli 119. The pathogenesis of status asthmaticus is: A. excitation of B-adrenoreceptor B. * B-adrenoreceptor blockade C. Hypersensitivity to sympatomimmetics bronchodilators D. reduction in pulmonary artery pressure, hypoxia E. all of the above 120. What forms of status asthmaticus are identified: A. Allergic B. Neuropsychiatric C. Medication D. hypoxic, asphiciational E. * anaphylactic, metabolic 121. Pathognomonic symptom status asthmaticus stage 2 is: A. Cyanosis B. pale skin C. presence of wheezes over the light D. * complete or nearly complete absence of rales over the lungs E. lowering blood pressure 122. What is not typical for the toxic action of sympatomimmetics: A. * bradycardia, a decrease in blood pressure B. tremor C. tachycardia, pain in the heart D. high blood pressure E. excitement 123. The first precursor, which indicates the improvement of bronchial obstruction in asthmatic status is: A. shortness of breath decrease B. decrease cyanosis C. * improves sputum D. reduces the number of wheezes over the light E. increased blood pressure 124. With an overdose of sodium bicarbonate in status asthmaticus: A. increased asthma attack B. hemoptysis C. * apnea may occur D. appears sweating E. pain in abdomen Name the most important clinical signs pointing to the effectiveness of the therapy of status asthmaticus: 125. A. decrease cyanosis B. decrease in cough C. * self-discharge of phlegm D. decrease in tachycardia E. decrease in the number of wheezes 126. Among extra-pulmonary pathology in chronic pulmonary heart more attention should be given to: A. joint damage B. phlebitis C. hypertonic disease D. vegetative-vascular dystonia E. * ulcerative processes in the gastrointestinal tract 127. What disease is accompanied by shortness of breath that occurs and increases when inhaling cold air and when the air is circulated in a warm room? A. acute pneumonia B. heart failure C. lung tumors D. tuberculosis E. * obstructive pulmonary disease In which disease appears a "warm" diffuse cyanosis, expressed at their fingertips, nose, ear lobes, which increases or passes by inhalation of oxygen? 128. A. * with pulmonary insufficiency B. heart failure C. renal failure D. with liver failure E. with cerebral insufficiency 129. Decompensation of chronic pulmonary heart shows all the symptoms except: A. swelling of neck veins B. Acceptance II tone in the pulmonary artery C. * low-grade temperature D. liver enlargement E. swelling of the legs 130. The main mechanism for development of status asthmaticus: A. * The blockade of beta 2-adrenergic receptors B. Stop the intake of glucocorticoids C. Emotional stress D. Exacerbation of chronic infection in the lungs E. Cerebral hypoxia 131. Selective stimulator of beta 2-adrenergic receptors are: A. * Salbutamol B. Bekotid C. Inderal D. Aminophylline E. Atrovent 132. When having a status asthmaticus it is recommended to take: A. Promedol B. Morphine C. Kordiamin D. Cocarboxylase E. * Glucocorticoids 133. What causes the development of pulmonary heart in Bechterew's disease? A. * Limitation of movement of chest B. Primary alveolar damage C. Hypotension in the pulmonary circulation D. All these factors E. None of these factors 134. What caused the development of pulmonary heart disease in systemic sclerosis? A. The destruction of the alveolar B. The destruction of the pulmonary vessels C. * The destruction of the alveoli and blood vessels D. Limitation of movement of the chest E. Pulmonary heart in systemic sclerosis does not develop 135. What includes the concept of "pulmonary heart"? A. * Respiratory and right ventricular failure B. Respiratory insufficiency C. Left ventricular failure D. Hypertension in the pulmonary circulation E. Bronchospasmic syndrome 136. How many variants of the pulmonary heart disease are there? A. Four B. * Three C. Two D. Five E. Variations of flow does not happen 137. How many stages there are in the development of pulmonary heart disease? A. * Three B. Two C. Four D. Five E. NO stages of development 138. The most frequent cause of acute pulmonary heart disease is: A. Pulmonary embolism B. Pneumothorax C. Asthmatic condition D. * All of the above E. None of the above 139. Causes of chronic pulmonary heart disease? A. Tuberculosis B. Chronic nonspecific lung diseases C. Bronchial asthma D. * All of the above E. None of the above What are the most typical complaints during the development of decompensated pulmonary heart disease? 140. A. * Growth of suffocation B. Increased cough C. Resistance to asphyxia of atropine D. E. Rise in temperature Fatigue 141. Cyanosis develops together with: A. * Decline in oxyhemoglobin B. Increase in level of oxyhemoglobin C. Reduced hemoglobin D. Increased melanin E. Increase in carotene 142. The mechanism of tricuspid valve insufficiency in pulmonary heart is: A. * Dilatation of the right ventricle B. The defeat of the valve C. Insufficiency of the tricuspid valve does not happen D. Accession mitral heart defect E. Accession aortic heart defects 143. What ECG changes are typical for pulmonary heart disease? A. * Signs of right heart hypertrophy B. Signs of hypertrophy of the left heart C. Signs of hypertrophy of the left atrium D. NO ECG changes E. Left bundle branch block 144. Indications for mechanical ventilation in status asthmaticus: A. Asthmatic status in stage I B. Asthmatic status of stage II C. Asthmatic status of stage III D. * "Silent lung" E. Pneumorrhagia 145. Respiratory failure diagnosis is based on the: A. Anamnesis B. Physical examination of the patient C. X-ray examination of the chest D. * The study of blood gases E. Spirographic study In secondary pulmonary emphysema, on the background of chronic obstructive bronchitis, the following are seen 146. A. Clinical signs of pulmonary heart B. Reduced lung diffusion capacity C. The increase in residual lung capacity D. Hypoxia and hypercapnia at rest E. * True all of the above 147. Hematogenous penetration of staphylococci in the lung tissue leads to development: A. Single abscess B. * Multiple abscesses C. Pulmonary gangrene D. Pneumosclerosis E. Purulent pleurisy 148. Name one of the earliest components of aspirin triad: A. Genyantritis B. Tonsillitis C. * Nasal polyp D. Bronchitis E. Pneumonia 149. Appropriateness of heparin therapy for bronchial asthma is due to: A. Improvement in gas exchange B. Antagonism to serotonin C. Mucolytic action D. Anti-inflammatory action E. * all of the above 150. Basic principles of early treatment of asthmatic attack: A. Aminophylline B. Corticosteroids C. * B2 - adrenoceptor agonists (aerosol) D. aspirin E. plasma 151. Among the components of obstruction in asthmatic patients the most important: A. Laryngism B. * Bronchospasm C. Education mucosal bunches D. Swelling of the bronchial mucosa E. Manifestations endobronchitis 152. The main risk factor for acute pneumonia: A. Abuse of carbohydrates and fats B. * Influenza, acute bronchitis, catarrh of the upper respiratory tract C. Isolation D. Physical inactivity E. Overcooling 153. To the following help to diagnose airway obstruction at the bedside: A. Relationship of meteorological conditions with acute broncho-pulmonary infection B. Character of expiratory dyspnea C. Congestion wheezing D. Hacking cough, shortness of breath, which strengthens E. * Wheezing in the lungs against expiratory dyspnea 154. The most important clinical sign of decompensated in pulmonary heart disease are: A. Swelling of the face B. Strengthening of cyanosis on the type of "cold" acrocyanosis C. Pulsation of neck veins D. Swelling of the neck veins of a permanent nature E. * Diffuse cyanosis 155. Underlying disease, which is necessary to differentiate from bronchial asthma is: A. Pleural effusion B. * Cardiac asthma C. Psychogenic breathlessness D. Periarteritis nodosa E. Spontaneous pneumothorax 156. For most atopic asthma is characterized by: A. Onset usually in childhood and young age B. Asthma attacks occur against a background of chronic nonspecific lung diseases C. * Positive family history of allergenic D. Asthma attacks occur suddenly E. Asthma attacks more often in spring 157. All of this medicaments are nitrates, except: A. izoket; B. nitrosorbit; C. nitron; D. * nifidypin E. nitroglycerin Which functional class of drugs should be given to patient with the diagnosis: CHD: postinfarction cardiosclerosis, chronic left ventricular aneurysm. CH II d., Systolic option? 158. A. I FC B. II FC C. * III FC D. IV FC E. 0 FC Which functional class of drugs should be given to patient with the diagnosis: CHD: stable angina pectoris, postinfarction cardiosclerosis. CH I d., Systolic option? 159. A. I FC B. II FC C. * III FC D. IV FC E. 0 FC Patients with peptic ulcer conducted fractional study of gastric secretion, determined by high acidity of gastric contents. Which is the leading symptom in such patients? 160. A. With the undigested food residue B. Diarrhea C. The alternation of constipation and diarrhea D. Normal E. * Constipation The patient complains of difficulty swallowing food, pain in the lower sternum, sometimes at night vomiting food he ate in the evening. Which of the methods of examination is not helpful for diagnosis? 161. A. * Ultrasound B. X-ray of the gastrointestinal tract with barium C. esophagomanometry D. Review radiography E. esophagoscopy Patient N. addressed to the doctor complaining of epigastric pain 1,5-2 hours after a meal, periodically night, hungry pain. what disease is characterized by such pain? 162. A. Esophagitis B. Gastric ulcer C. Acute gastritis D. * Peptic Duodenal ulcer E. Cholecystitis Patient S., after an examination was given the diagnosis of gastric ulcer. Which of the following symptoms are characteristic of acute gastric ulcer? 163. A. * Dysphagia B. Pain on an empty stomach C. Vomiting at the height of pain, which brings relief D. Acid regurgitation, heartburn E. Pain after 30 minutes after eating X-ray examination reveals the presence of gastric symptoms of "niche" For what is characteristic of the disease? 164. A. * ulcer B. pyloric stenosis C. not typical for any disease D. for gastric cancer E. for chronic gastritis Patient K., addressed to the doctor complaining of belching with the smell of "rotten eggs". This symptom may occur when: 165. A. by narrowing of the esophagus B. at hyperacidic state C. with gastric bleeding D. * at hypoacidic state E. intestinal bleeding Patient M., periodically disturbed epigastric pain occurring 30-40 minutes after eating. They are call ____ pain: 166. A. * Early B. later C. hungry D. night E. Seasonal The patient, who is being treated at a family doctor about stomach ulcers revealed black stools. What complications developed in a patient? 167. A. * gastric bleeding B. malignanization of a ulcer C. enterorrhagia D. penentration E. perforation Patient V., complains about the impossibility of swallowing, retrosternal discomfort during eating. This symptom is called: 168. A. anorexia B. dyspepsia C. dystonia D. * Dysphagia E. none of the above Heartburn, acid regurgitation, sour vomiting, while maintaining appetite, constipation, increased secretion and gastric acidity, this is characteristic: 169. A. * for hyperacidic state B. for anacidic state C. for atony of the stomach muscles D. for hypoacidic state E. stomach cancer X-ray examination of the stomach to the patient in an outpatient setting revealed the presence of symptoms of "filling defect" For what disease is this characteristic? 170. A. peptic ulcer B. pyloric stenosis C. not typical for a D. for chronic gastritis E. * gastric cancer The patient asked the family doctor complaining of belching with the smell of "rotten eggs", prone to diarrhea. This may occur when: 171. A. * at hypoacidic state B. at hyperacidic state C. with gastric bleeding D. at normoacidic state E. intestinal bleeding A patient at a reception at the family doctor complaining of inability to swallow, discomfort behind the breastbone during eating. This symptom is called: 172. A. * Dysphagia B. dyspepsia C. dystonia D. anorexia E. bulimia The patient is seen by a family doctor periodically complains of epigastric pain that occurs 20-30 minutes after ingestion. Such pain is called: 173. A. * Early B. late C. hungry D. night E. seasonal Patient AM on reception at the family doctor complaining of nausea, vomiting, belching, heartburn. For what syndrome are such complaints characteristic? 174. A. astenovegetative B. Dumping Syndrome C. * dyspeptic D. cholestatic syndrome E. malabsorption syndrome Patient has been vomiting undigested food, immediately after eating, without nausea. What part of the gastro - intestinal tract is affected? 175. A. * Esophagus B. Stomach C. duodenum D. small intestine E. colon After an objective examination of the patient family doctor suspected a tumor of the esophagus. What is the most significant feature of esophageal cancer? 176. A. General weakness B. Salivation C. Chest pain D. * Dysphagia E. Burping air The patient had a family doctor diagnose atrophic gastritis, with a significant decrease in gastric secretory function. What should the patient’s tongue look like? 177. A. * "Coated" (atrophy of papillae) B. Hyperplasia of the papillae C. Smooth, raspberry D. Dry as the brush E. Moist, pink, pure The patient had the following symptoms: loss of appetite, aversion to meat, belching, nausea, weight loss, feeling of heaviness, fullness in the epigastric region, and depression. These signs indicate: 178. A. Acute gastritis B. chronic gastritis C. * gastric cancer D. acute pancreatitis E. Gastric ulcer 179. Name the characteristic signs of stomach cancer A. loss of appetite (a characteristic aversion to meat) B. sharp loss of body weight, C. pain in the upper abdomen (sometimes very strong) D. "Unreasonable" diarrhea, E. * All the above . 180. What is an atypical feature of gastritis with secretory failure? A. appetite loss, B. unpleasant taste in the mouth, C. * heartburn, nausea, D. heaviness in the epigastric region, E. Diarrhea. 181. What is called the examination of the mucous membrane of the entire colon? A. gastroduodenoscopy, B. * Colonoscopy C. sigmoidoscopy, D. cystoscopy E. Laparoscopy. 182. Which is not included in the preparation of a patient in an outpatient setting for a gastroduodenoscopy? A. psychological preparation, B. before (at 18:00 ) - Dinner C. * evening (at 20:00) - a cleansing enema D. warning the patient about the procedure is carried out on an empty stomach, E. Irrigation of the throat 1-2% solution dicaine (3-5 minutes before the start of the study). X-ray examination of the stomach in an outpatient setting revealed the presence of symptoms of "niche" For what disease is this characteristic? 183. A. for gastric cancer B. for chronic gastritis C. * ulcer D. pyloric stenosis E. not typical for any X-ray examination of the stomach with the patient, aged 68, in an outpatient setting revealed the presence of symptoms of "filling defect". For what diseases is it typical? 184. A. * for gastric cancer B. for chronic gastritis C. peptic ulcer D. pyloric stenosis E. not typical for any The patient in the outpatient setting diagnosed gastric ulcer. What method of research will reveal Helicobacter pylori? 185. A. intragastral pH-metry B. CBC C. definition of uropepsinogen D. * C-breath test E. gastric probe 186. Patient in an outpatient setting conducted intragastric pH meters, pH = 7.0. What does this show? A. Normal acidity B. Slightly increased acidity C. Significantly increased the acidity D. Hypoacidity E. * Anacidy 187. The reaction of fecal occult blood test may be positive: A. at microbleeding of duodenal ulcer or intestinal B. at microbleeding of tumors of gastro - intestinal tract C. at ulcerative colitis D. increased meat intake E. * for all of the above Following the endoscopy patients with peptic ulcer a family physician appointed X-ray examination of the gastrointestinal tract to identify: 188. A. Tumor B. Polyps C. Changes in gastric and 12 duodenal ulcer D. * Changes in the motor and evacuation function of stomach E. Bleeding According to the sigmoidoscopy: the mucosal surface Procto-sigmoidal Department colon pink, shiny, smooth, with visible dilated blood vessels. What does this show? 189. A. Chronic sigmoid B. Chronic proctitis C. * Normal D. Chronic proctosigmoiditis E. chronic colitis The patient asked the family doctor complaining of a dull ache in the side and lower abdomen, feeling of incomplete emptying after a bowel movement, has been appointed ergography. What is this method? 190. A. Endoscopic examination of the colon B. Endoscopic examination of the line and the sigmoid colon C. X-ray examination of large intestine with the introduction of a mixture of barium through the mouth D. * X-ray examination of large intestine with the introduction of a mixture of barium enema E. Survey X-ray of the abdominal cavity 191. Which of the following signs are indications for the radiological examination of the gastrointestinal tract.? A. dysphagia B. unmotivated reduction in body weight C. presence of seals in the abdomen by palpation D. abdominal pain, nausea, vomiting E. * all the above X-ray examination of stomach using contrast medium in an outpatient setting revealed the presence of barium in the stomach within 24 hours after the test. What does this show? 192. A. gastric ulcer B. stomach cancer C. * pyloric stenosis D. norm E. stenosis of the cardia Patient R., 54, registered at the district physician for ulcer disease complicated with pyloric stenosis. What is the nature of vomit at the same time? 193. A. In the vomit is an admixture of bile B. In the vomit is bloody C. In the vomit is undigested food D. * In the present vomit food consumed on the evening E. In vomit mucus, pus Patient's family doctor complaining of pain in the abdomen. Chair with a tendency to constipation, feces is a form of "sheep". If any disease is a form of feces? 194. A. Chronic enteritis B. Ulcerative colitis C. * Chronic spastic colitis D. Chronic pancreatitis E. Fundic gastric 195. The patient H, 27y., when microscopic examination of feces revealed steatorrhea. In this case, we can suspect A. violation of the endocrine function of pancreas B. * violation of exocrine pancreatic function C. parenchymatous jaundice D. obstructive jaundice E. gastritis with high acid-forming function of the stomach Patients with peptic ulcer to appoint a family doctor carried out a fractional study of gastric secretion, determined by the increased acidity of gastric juice. Which is the most frequent symptom in such patients? 196. A. * Constipation B. Diarrhea C. The alternation of constipation and diarrhea D. Normal E. With the undigested food residue 197. Including the preparation of the patient in an outpatient setting in gastroduodenoscopy? A. psychological preparation, B. before (in the 18 th hour) - Dinner C. * all of the above D. warning the patient about the procedure is carried out on an empty stomach, E. irrigation of the throat 1-2% solution dicaine (3-5 minutes before the start of the study). 198. X-ray method of investigation does not allow to determine: A. * Erosion of the stomach B. Form and size of the stomach C. Gastric ulcer D. Swelling of the stomach E. The motor-evacuation function of stomach 199. Which of the diseases of the stomach accompanied by an increased ESR (erythrocyte sedimentation rate): A. * Stomach Cancer B. Uncomplicated peptic ulcer C. Chronic gastritis atrophic D. Irritable stomach E. Nervous anorexy 200. Heart burn may occur when: A. * All of the above is true B. The presence of the high rate of acidity C. Insufficiency of the lower esophageal sphincter D. The presence of bile reflux E. Dysmotility of the stomach and 12 duodenal ulcer 201. The main factors contributing to the development of gastroesophageal reflux disease include: A. * All the above is true B. Stress C. Pregnancy D. Obesity E. Smoking 202. For the treatment of patients with peptic ulcer do not prescribe: A. * Immunosuppressant / glucorticoids / B. Vitamins C. Antibiotics D. Antacids E. proton pump inhibitors 203. How does helicobacter pylori live in the acidic environment of the stomach: A. * by Forming ammonia due to hydrolysis of urea B. The presence of mucus C. by forming gastromucoproteins D. by forming gastrin E. All the above is true 204. Basic principles of diet therapy in patients with peptic ulcer A. * All the above is right B. Compliance with diet C. avoidance of mechanical stress D. avoidance of Chemical stress E. avoidance of Thermal stress 205. When a patient has an ulcer which food is recommended: A. * All of the above B. Eggs C. lean meat D. whole grain cereals E. None of the above 206. What properties are characteristic of antacids? A. * All the above is true B. Rapid elimination of pain and dyspeptic symptoms C. Absorption bile acids D. Cytoprotective effect E. Neutralization of acid-peptic factor 207. Anorexia should be differentiated: A. * With all the listed diseases B. With schizophrenia C. Cancer D. Tuberculosis E. Simondsa disease 208. For the compensated phase of chronic atrophic gastritis with secretory deficiency is characteristic: A. * All the above is true B. Marked secretory insufficiency C. B12-dependent macrocytic anemia D. The absence of clear clinical symptoms E. Lack of involvement in the process of other chronic digestive organs 209. The main complaint of patients with atrophic gastritis of sub-and decompensated stages are: A. * All the above is true B. Diarrhea C. Unstable feces D. Loss of appetite E. inability to eat certain products like sweet milk, fatty foods, juices, etc. / 210. For diagnosis of chronic gastritis least informative are: A. * X-ray Research Methods B. Intragastric pH meter C. Endoscopic method of study D. Morphological method for investigating E. Cytological method of investigation 211. Chronic gastritis primarily associated with: A. * Helicobacter pylori infection B. Genetic propensity C. Age D. Pregnancy E. All listed Which statement is false regarding dynamic observation of patients with the diagnosis: CHD: postinfarction cardiosclerosis, chronic left ventricular aneurysm. CH II d., Systole-ventricular diastolic dysfunction in type I? 212. A. The frequency of observations of cardiologist is 3 times a year; B. The frequency of observations of neurologist is 1 time a year; C. Sanatorium treatment is contraindicated; D. * Sanatorium treatment in cardiosanatorium ; E. The frequency of observations by ophthalmologist is 1 time a year 213. With IHD, stable angina pectoris FC II drugs are prescribed from all of the groups, except: A. Nitrates B. Acetylsalicylic acid C. calcium antagonists D. * Nonsteroid anti-inflammatory E. ?-blockers 214. With IHD, stable angina pectoris III FC drugs are prescribed from all of the groups, except: A. Nitrates B. Hypolipidemic C. Calcium antagonists D. * Blockers of proton pump E. ?-blockers 215. With IHD, stable angina pectoris IV FC drugs are prescribed from all of the groups, except: A. Nitrates B. hypolipidemic C. calcium antagonists D. * antacids E. ?-blockers 216. These ECG changes are the main manifestations of myocardial infarction, except? A. * Increasing the interval P-Q B. The appearance of pathological Q wave C. ST segment displacement D. Pathological changes of T wave E. Discordant ST segment shift in I and III assignments. 217. The most reliable way to determine coronary reserve are: A. * Bicycle ergometer, coronarography B. Holter monitoring C. Chest X-ray D. ECG peace blood E. Biochemical analysis of blood 218. Important features of atherosclerotic cardiosclerosis that determine the degree of heart failure are: A. * All listed B. Cardiac aneurysm C. Mitral valve insufficiency D. asynergy of left ventricular E. A significant increase in heart size 219. Which changes of cardiac conduction are the most frequent in IHD A. * All listed B. Ventricular beat C. Blink fibrillation D. Sinus syndrome E. Atrio-ventricle blockade 220. The first symptom of heart failure in atherosclerotic cardiosclerosis are: A. * Shortness of breath B. The appearance of systolic murmur including Botkin C. Dizziness D. Episodes of acute left ventricular failure E. The appearance of peripheral edema When the diagnosis of coronary disease in patients with suspected sick sinus syndrome should be given preference: 221. A. * Esophageal atrial pacemaker B. Bicycle ergometer C. Sample dosed with walking D. Tredmil-test E. Dipiridamole sample 222. The risk of IHD increases with: A. * Podagra B. Rheumatoid arthritis C. Sickness of Bekhterev D. Rheumatism E. Systemic erythematosus lupus 223. Fibrillation of IHD can be caused by: A. * All the factors listed B. Premature impulse C. Reciprical nodal tachycardia D. Ventricular tachycardia E. Sinus tachycardia 224. What is the most common cause of coronary heart disease: A. * Atherosclerosis of coronary arteries B. Inflammation in the myocardium C. Intravascular coagulation hemocyte D. Hyperlipidemia E. Dilatation of heart 225. What are the main groups of antianginal drugs you know? A. * Calcium antagonists, nitrates, beta-blockers B. Nitrates and nitrate like medicaments C. Antioxidants D. Beta-blockers E. Vasodilatators 226. Pharmacodynamic effects of which drugs are similar to those that cause beta-blocker: A. * Verapamil B. Prazozin C. Hypothiazid D. Nifedipin E. Kaptopril 227. List the main problems solved by the test with dosed physical exercises in patients with coronary heart disease A. * All listed B. Diagnosis of IHD C. Determination of exercise tolerance D. Choice of treatment and evaluation of its effectiveness E. Selection of an adequate dose of antianginal therapy What preparations have advantages in treating patients with stable angina pectoris, combined with sinus tachycardia, atrial beats or atrial fibrillation: 228. A. * Verapamil, propranolol B. Propranolol C. Nifedipin D. Isosorbide-5-mononitrate E. Trinitrolonh 229. Modern classification of stable angina pectoris include as many functional classes as: A. * Four B. Two C. Five D. Ten E. Three 230. What are the possible causes of absence of effect of antianginal drug therapy: A. * All listed options B. Wrong choice of drugs C. Incorrect determination of doses of selected drugs D. Irrational combination of drugs E. Inadequate treatment duration After 3 weeks of receiving nitrosorbid isolated in a daily dose of 80 mg there were new attacks in patients with angina pectoris with previous frequency. Your insights and tactics 231. A. * Development of tolerance to the drug, discontinuation of nitrosorbid B. The drug is ineffective, increasing the daily dose of 120 mg C. Unstable angina, hospitalization of a patient in Brit D. Improper treatment, switching to combination therapy E. None of the allegations false 232. What is the side effect most often occurs in the application of nitroglycerine? A. * Collapse, headache B. Hypertension C. Dry Mouth D. Headache E. Increased blood sugar 233. Beta-blockers are used in IHD, because they: A. * Lower myocardial oxygen demand B. Expand coronary vessels C. Cause peripheral vascular spasm D. Increase the need for myocardial oxygen E. Increase the ability of myocardial contractile 234. The positive effect of nitroglycerine is: A. * Reduced smooth muscle tone of arteries and veins B. Increase the flow of venous blood into the left ventricle C. Increased peripheral resistance and blood pressure D. Increased end-diastolic pressure E. Reduced cardiac work 235. What are the absolute contraindication to beta-blockers? A. * All listed B. Insulin diabetes C. Atrioventricular block II D. Bronchial asthma E. Sinus dysfunction 236. What is the primary mechanism of action of nifedipin as antianginal medication? A. * Reducing postload B. Reduced preload C. Increased contractility of the myocardium D. Increased heart rate E. Negative inotropic effect 237. Which of the following symptoms are pathognomonic for angina pectoralis: A. * Retrosternal pain and ST segment depression, vanishing at the same time B. Retrosternal pain during physical work C. Ventricular beat after physical work D. Retrosternal pain and ST segment depression in standard assignments E. Q wave in the third and avF assignments 238. What are the terms of secondary prevention of coronary heart disease drug? A. * For life B. 1-2 months C. In acute D. Until six months E. 1-2 years 239. Risk factor for IHD is: A. * Hypertension B. Cholelithiasis C. Alcoholism D. Azotemiya E. Hypovitaminosis C Which of the following are the risk factors for coronary heart disease: 1) the racial factor, 2) rich meaty meal, 3) hyperhamaglobulinemia 4) hyperglycemia: 240. A. * Right - 2, 4 B. Right - 1, 2, 3 C. Right - 1, 3 D. Right - 4 E. Faithful all the answers 241. Atherosclerotic cardiosclerosis has such characteristics: A. * All listed options B. Scar tissue C. Dystrophic changes of cardiac fibers D. Necrotic changes of cardiac fibers E. Compensatory hypertrophy in the intact areas of infarction 242. What diseases reinforce signs of heart failure in patients with atherosclerotic infarct? A. * All listed B. Hypertension C. Blink or atrial flutter D. Transverse heart block with bradycardia E. Ventricular beat 243. Optimal cholesterol levels in populations below 30 years: A. * <5.2 mmol / l B. 5,2-6,2 mmol / l C. <2.8 mmol / l D. 6,2-7,8 mmol / l E. 5,5-6,2 mmol / l 244. The cause of cardiac arrest in diastole can be: A. * Hyperkaliemia B. Hypercaltsiyemia C. Respiratory alkalosis D. None of the above reasons E. Hypernatriemia Which test increases myocardial oxygen demand, but does not require implementation of physical activity: 245. A. * Electrical pacing test B. Nitroglycerine test C. Dipiridamole test D. Hyperventilation test E. Ergometryne test 246. Non painful myocardial ischemia - is: A. * Episodes fading ischemic ST segment changes that are not accompanied by pain storm B. All ischemic ECG changes during exercise C. Attacks of pectoral angina that does not require termination load D. Clinical equivalents of angina pectoralis E. ECG changes during exercise that are not accompanied by clinical symptoms On the recommendation of WHO experts (1964) Sudden death - a violent death of a healthy person or patient, who was in satisfactory condition, which occurred unexpectedly within: 247. A. 1:00 B. 6:00 C. 24 hours D. 2 weeks E. 2:00 From which the drug can be expected antianginal and antiarrhythmic effect when combined angina pectorals and ventricular beats or ventricular tachycardia? 248. A. * All listed B. Propranolol C. Aymalin D. Etmozin E. Etatsyzin In a patient with an implanted artificial pacemaker in connection with A-V blockade third degree diagnosed angina pectoris III FC. How antianginal drugs you prefer in this case? 249. There no restrictions to the use of antianginal drugs related to their influence on rhythm and conduction, A. * B. Beta-blockers C. Calcium antagonists D. Only nitrate and nifedipin E. Use of antianginal drugs is contraindicated What types of employment are contraindicated for patients with IHD, regardless of state of coronary blood flow and hemodynamics? 250. A. All listed B. Working with more than 5.0 kcal of energy per minute C. Working at altitudes in extreme conditions D. Work related to the action of toxic substances, especially vascular and neurogenic poisons The work associated with maintenance of existing electrical equipment and a potential danger to others in cases of sudden cessation of work E. 251. What questions can find selective coronarography? A. * All listed B. Radiological anatomy of coronary arteries C. The presence or absence of stenosis and occlusion of coronary arteries D. Determine the type of coronary circulation E. The presence of collaterals 252. ECG criteria for termination of the dosed sample exercise: A. * All listed options B. ST segment depression greater than 1 mm, duration 0.08 sec C. ST segment elevation more than 1 mm D. Often (1:10) extrasystoles, paroxysmal tachycardia, and atrial flutter E. Violation of atrioventricular and intraventricular conduction 253. Clinical signs for stopping exercise testing: A. * All listed B. The attack of angina C. BP decrease by 25-30% on rising D. BP rising to 230/130 mmHg more E. The attack of asthma, shortness of breath expressive, cutting general weakness Which of the following is the cause of nocturnal seizures rest angina in patients with progressive coronary atherosclerosis: 254. A. * Increasing preload B. Hypertension C. Coronary artery spasm D. Increased blood volume E. Reduction of myocardial contractility 255. What are the underlying cause of the progression of coronary disease: A. * Increasing the size of atherosclerotic plaques and the appearance of new lesions B. Dilatation of heart cavities C. Myocardial infarction D. Increased blood viscosity E. Reduced diastolic myocardial relaxation 256. Which of the following states can be called angina pectoris equivalent? A. * All listed B. Heartburn at fast walking C. The attack of arrhythmia during run D. Shortness of breath when walking without signs of circulatory failure E. Go near left ventricular failure, repeating an exercise in a patient with myocardial infarct 257. What specific pharmacodynamic properties inherent beta-blockers? A. * All listed B. Internal sympatomymetyc activity C. Cardioselectivity D. Membrane action E. None of the above 258. What preparations are similar in effect to nitrates and are successfully used in the present as antianginal tools? A. * From the group sydnofarms(synonyms: korvaton, sydnofarm, molsodomin) B. Kordaron C. Nifedipin D. Propranolol E. 259. All listed The key factor that regulates coronary blood flow, is: A. * Diastolic pressure in the aorta B. Cardiac acceleration C. Myocardial hypoxia D. High pressure in the right ventricle E. None of these factors 260. Which of the following is the direct cause of angina: A. * Anaerobic metabolism of exchange B. Coronary spasm C. Latent left ventricular failure D. Local infringement reduction of left ventricle E. Increased end-diastolic pressure in the left ventricle 261. What methods should be used to evaluate the efficiency of antianginal medications? A. * All listed B. Anamnesis C. Bicycle ergometer D. Orthostatic test E. Echocardiography 262. What are the side effects encountered in the treatment with nifedipin? A. * All listed B. Swelling of the legs C. Face congestion D. Tachycardia E. Collapse There is a causal relationship with coronary heart disease: 1) arterial hypertension 2) hiperurikemia 3) thyrotoxicosis 4) hyperlipidemia: 263. A. * Right - 1, 2, 4 B. Correct - 1, 3, 4 C. True - 2, 3 D. Correct - 1, 4 E. Correct all the answers 264. Beta-blockers do not increase coronary blood, but reduces the contractile force of myocardium: A. * Both statements are correct and linked B. Both statements are correct, but not linked C. The first claim is correct, the second - false D. The first claim false, the second - correct E. Both false statement What methods of secondary prevention of coronary heart disease exist? 1) medication, 2) surgical 3) the impact of risk factors, 4) treatment of opportunistic diseases 265. A. * Right - 1, 2, 3 B. Correct - 1, 3 C. True - 2, 4 D. Correct - 1, 2 E. Correct - 3, 4 266. What drug is proven to have impact on survival of patients with coronary disease? A. * Beta-blocker B. Nitrates C. Calcium antagonists D. Combination therapy E. Verapamil 267. What disease is characterized by a sharp rise of segment ST? A. * Acute stage of myocardial infarction B. Subacute phase of myocardial infarction C. Stages of myocardial scarring D. Myocarditis E. Infectious endocarditis 268. Poisoning by cardiac glycosides occurs mainly in patients with: A. * Hypokaliemia B. Hyperthyreosis C. Chronic obstructive pulmonary diseases D. Hypermagnesiemia E. Severe illness, liver 269. In which disease is contraindicated to use large doses of nitrates of prolonged action? A. * Aortic valve stenosis B. Aortic valve insufficiency C. Mitral insufficiency D. Dilated cardiomyopathy E. Hypertrophic cardiomyopathy 270. Which of cardiac glycosides has the most pronounced cumulative properties: A. * Digitoxin B. Digoxin C. Strofantyn D. Korhlikon E. Adonizyd 271. Atrioventricular block – is a violation of electrical impulses: A. * By leading connection of atrioventricular heart B. In total ventricular and atrials C. From the atrias to ventricles D. Hold on additional ways abnormal electrical impulses from the atria to the ventricles E. On the leading system bundle branch block legs 272. What drugs are needed to prepare patients for the planned countershock? A. * Heparin B. Anticoagulants with indirect action C. Cardiac glycosides D. Diuretics E. Nitrates 273. What medications should be cancel 2-3 days before the planned cardioversion: A. * Cardiac glycosides B. Heparin C. Anticoagulant indirect action D. Diuretics E. Nitrates 274. Side effects of calcium antagonist-korinfar are: A. * Edema B. Bradycardia C. Increased blood pressure D. Proteinuria E. Hyperglycemia 275. How many degrees does synoauryculary blockade have? A. * Three B. One C. Two D. Four E. Five 276. Unstable pectoral angina include: A. * Variant angina B. Angina pectoris I functional class C. Angina functional class II D. Angina functional class III E. Angina functional class IV What are the biggest contraindications to restore sinus rhythm in patients with mitral stenosis and fibrillation? 277. A. * Left atrial thrombosis B. Restenosis C. A history of stroke D. Heart failure E. Extrasystole 278. Cardiac glycosides can not be combined with: A. * Calcium preparations B. Veroshpiron C. Potassium preparations D. Lidocaine E. Apresyn 279. Patient with predominantly diastolic left ventricular failure should be prescibed: A. * Calcium antagonists B. Cardiac glycosides C. Peripheral vessal dialatators D. Aminophyliline E. Nitrates 280. What is the main syndrome associated with the diagnosis of atherosclerosic myocardiosclerosis? A. Respiratory failure B. Pain C. * Syndrome of heart failure D. Coagulopathy E. None of the 281. What is the main syndrome associated with the diagnosis of atherosclerosic myocardiosclerosis A. Respiratory failure B. Pain C. Coagulopathy D. * Cardiac arrhythmias E. None of the 282. Which sign is not characteristic for atherosclerotic cardiosclerosis : A. Edema B. Palpitation C. Dyspnea D. * Pain in chest area E. Tachycardia 283. Dysfunction of which part of the heart happens most often at atherosclerotic cardiosclerosis? A. Left atrium B. * Left ventricle C. Right atrium D. Right ventricle E. AV-node 284. What rhythm disorders are often diagnosed at atherosclerosis cardiosclerosis? A. Ventricular beat B. Sinus tachycardia C. AV-blockade D. * Atrial fibrillation E. Paroxyzmal tachycardia 285. Heart failure at atherosclerotic cardiosclerosis is caused by: A. Myocarditis B. Violations of the coronary circulation C. Chronic anemia D. * Overload of left ventricular E. Reduction of myocardial contractility 286. In a patiet with severe heart failure what do we notice on a physical exam: Edematous, pale face Cachexia A. B. Swelling of the whole body, with no manual closed holes remain C. Fingers "clubbed" D. * Ascites 287. During chronic left ventricular failure why is apical impulse weakened, poured out: A. As a result of left ventricular hypertrophy B. As a result of hypertrophy and left ventricular tonogennic dilatation C. * As a result of biogenic dilatation of LV D. Due to increasing end-systolic left ventricular cavity volume E. Due to increasing end-diastolic left ventricular cavity volume 288. Auscultation data in atherosclerosic cardiosclerosis is: A. Amplification and tone B. * Relaxation of both heart tones C. Rhythm of "quail" D. Accent II tone on pulmonary artery E. Accent II tone at the aorta 289. Auscultation data in chronic heart failure: A. Strengthening the I tone. B. Clicking the opening of mitral valve. C. * Protodiastolic gallop . D. Rhythm of "quail" E. Accent 2 Tone at the aorta. If a patient with mitral valve insufficiency occurs chronic left ventricular failure, what happens to organic systolic noise: 290. A. It is amplified. B. * It is weakened . C. It changes from a flowing sound into a rhomboid. D. Starts to be conducted on side of the carotid art.. E. Beggings to be better auscultated in the left auxiliary fossa. 291. What are the main complaints revealed during blood stagnation in the liver: A. Decrease of appetite, nausea and vomiting. B. Disturbance of taste, thirst, dull pain in the epigastrium, which all have an enveloping character C. Paroxismal pain under the right ribs, fever after eating. Dull pain, feeling of heaviness under the right ribs, sense of full stomach, increasing shortness of breath after eating. D. * E. Constant sharp pain under the right ribs, nausea, vomiting, weight loss, refusal to eat meat. 292. What are the signs that indicates stagnation of blood in the portal vein: A. Edema of lower extremities. B. * Ascites . C. Reduction of BP. D. Reduction of central venous pressure. E. Pale skin of the lower extremities. 293. What happens with daily diuresis in patients with congestive heart failure: A. it is increased. B. * it is reduced. C. Appears nicturia. D. Hydruria combined with nicturia. E. there aren’t any diurecing disorders. If patient complains about the reduction of capacity, shortness of breath when average force exercise, with no dyspnea at rest what stage of heart failure may be present? 294. A. * Chronic heart failure stage I . B. Chronic heart failure stage IIA. C. Chronic heart failure stage IIB. D. Chronic heart failure stage III. E. Chronic respiratory failure. If patient complains of shortness of breath in normal physical stress and has a slowing of bloodflow in a small circle of blood circulation. What does the patient have?: 295. A. Chronic heart failure stage I. B. * Chronic heart failure stage IIA . C. Chronic heart failure stage IIB. D. Chronic heart failure stage III. E. Chronic respiratory failure. If patient complains of a significant stagnation in the large and small circle of circulation, shortness of breath at rest, the patient unable to work, no cachexia, what is most probable diagnosis: 296. A. Chronic heart failure stage I. B. Chronic heart failure stage IIA. C. * Chronic heart failure stage IIB . D. Chronic heart failure stage III. E. Chronic respiratory failure. If patient complaines of significant stagnation of blood circulation in both circles, shortness of breath at rest, cachexia what is most probable diagnosis: 297. A. Chronic heart failure stage I. B. Chronic heart failure stage IIA. C. Chronic heart failure stage IIB. D. * Chronic heart failure stage III . E. Chronic respiratory failure. 298. What is a typical manifestation of acute left ventricular failure: A. Loss of consciousness or collapse B. * Cardiac asthma or pulmonary edema C. Shortness of breath or a typical asthma attack D. Cyanosis, cold clammy sweat, pain in the area of heart E. Cyanosis, swelling of neck veins, their pulsation, an increase in liver size 299. What medicine is always prescribed to patients with Heart Failure? A. Digoxin B. Verapamil C. * Ramipril D. Furosemide E. Metaprolol 300. What groups of drugs are not prescribed to patient with Heart Failure? A. ACE inhibitors B. ?-blockers C. Diuretics D. * Bronchodilators E. Cardiac glycosides 301. Which method is the best at diagnosing atherosclerosic myocardiosclerosis? A. ECG B. Holter monitoring C. VEM D. * Ultrasound of the heart E. Coronarography 302. At atrial fibrillation and heart failure the drug of choice is: A. Propranolol B. Verapamil C. Hinidin D. * Cordaron E. Lidocain 303. Cardiac glycosides appointed at: A. Diastolic heart failure B. Heart failure with bradicardia C. * Heart failure with atrial fibrillation D. In gastric paroxymal tachycardia E. At a left Giss bundle blockade 304. For atherosclerotic cardiosclerosis it is typical to see a history of: A. Myocarditis B. An attack of atrial fibrillation C. Stroke D. * Myocardial infarction E. Increased bp 305. In the diagnosis of heart failure, which is test is the most efficient: A. ECG B. * 6 minute walking test C. Spirography D. Test with dipiridamol E. Holter monitoring 306. What type of heart failure is more often seen at atherosclerotic cardiosclerosis? A. * Systolic B. Diasystolic C. Mixed D. None of the above 307. What type of conduction is more often seen at atherosclerotic cardiosclerosis? A. Sinus bradicardic action B. Incomplete AV-blockade C. Complete AV-block D. * Blockade of left bundle branch block E. Blockade of right bundle 308. What should be the drug of choice at atherosclerotic cardiosclerosis: A. Essentiale B. * Neoton C. Tremetasidin D. Statins E. Aspirin 309. Definition CHF is possible only based on: A. * Echocardiographic data B. Data of clinical research C. electrocardiographic data D. biochemical studies E. X-ray examination data 310. Main criteria of variant systolic heart failure is the presence of which clinical signs of heart failure: A. * Size of left ventricular ejection fraction is less then 40% B. Size of left ventricular ejection fraction less than 50% C. Size of left ventricular ejection fraction over 50% D. Size of left ventricular ejection fraction ranging from 40% to 50% E. Size of left ventricular ejection fraction ranging from 40% to 45% 311. Main criteria of diastolic heart failure is the presence of which clinical signs of heart failure: A. Size of left ventricular ejection fraction is 40% B. Size of left ventricular ejection fraction less than 50% C. * Size of left ventricular ejection fraction over 50% D. Size of left ventricular ejection fraction ranging from 40% to 50% E. Size of left ventricular ejection fraction ranging from 40% to 45% 312. The main criteria of CHF unspecified variant is the presence of which clinical signs of heart failure: A. Size of left ventricular ejection fraction is 40% B. Size of left ventricular ejection fraction less than 50% C. Size of left ventricular ejection fraction over 50% D. * Size of left ventricular ejection fraction ranging from 40% to 50% E. Size of left ventricular ejection fraction between 50% to 55% 313. Definition of functional class of CHF at all true statements except: A. Functional Class is a dynamic characteristic B. Functional Class represents the stage of clinical evolution of heart failure C. * Functional Class patients with CHF does not change under the influence of treatment D. Functional Class CHF reflects the real status of the patient E. All the above listed What functional class of patients with the diagnosis: ischmic heart disease: postinfarction cardiosclerosis, chronic left ventricular aneurysm. CH IIA., systolic type 314. A. Fucntional class I B. Fucntional class II C. * Fucntional class III D. Fucntional class IV E. Fucntional class 0 What functional class of patients with the diagnosis: coronary heart disease: stable angina pectoris, postinfarction cardiosclerosis. CH I., systolic type 315. A. Fucntional class I B. * Fucntional class II C. Fucntional class III D. Fucntional class IV E. Fucntional class 0 What functional class of patients diagnosed with: dilatations of cardiomyopathy, a form of permanent atrial fibrillation. CH IIB., systolic type 316. A. Functional class I B. * Functional class II C. Functional class III D. Functional class IV E. Functional class What functional class of patients with the diagnosis: stage III hypertension, hypertensive heart. CH IIA., Systolic type 317. A. Functional class I B. Functional class II C. * Functional class III D. Functional class IV E. Functional class 0 What functional class of patients with the diagnosis: Hypertrophic cardiomyopathy, obstructive form. CH IIA, Diastolic type? 318. A. Functional class I B. Functional class II C. * Functional class III D. Functional class IV E. Functional class 0 319. What functional class of patients diagnosed with: Constructive perikarditis. CH III., Diastolic type? A. Functional class I B. Functional class II C. Functional class III D. * Functional class IV E. Functional class 0 What functional class of patients with the diagnosis: rheumatism, I Degree, by transmission combined with the advantage of fault failure. CH IIB? 320. A. Functional class I B. Functional class II C. Functional class III D. * Functional class IV E. Functional class 0 Which statement is FALSE regarding dynamic observation of patients with the diagnosis: rheumatism, I Degree, combined with mitral defect with the advantage of failure. CH IIB.? 321. A. The patient is seen by Rheumatologist 6-8 times per year B. * The patient is seen by Rheumatologist 2-4 times a year C. The patient is seen by otolaryngologist 2 times a year D. The patient is seen by dentist 2 times a year E. All of the above mentioned Which statement is FALSE regarding dynamic observation of patients with the diagnosis: rheumatism, inactive, combined mitral defect with the advantage of failure. CH IIA.? 322. A. * The patient is seen by Rheumatologist 6-8 times per year B. The patient is seen by Rheumatologist 2-4 times a year C. The patient is seen by otolaryngologist 2 times a year D. The patient is seen by dentist 2 times a year E. All the above listed Which statement is FALSE regarding about dynamic observation of patients with the diagnosis: hypertension stage III, hypertensive heart. CH IIB? 323. A. The patient is seen by cardiologist 3 times a year B. The patient is seen by neurologist 1 per year C. * The patient is seen by otolaryngologist 1 per year D. The patient is seen by oculist 1 per year E. The patient is seen by dentist 1 per year Which statement is FALSE regarding dynamic observation of patients with the diagnosis: CHD: postinfarction cardiosclerosis, chronic left ventricular aneurysm. CH I.Fucntional Class 324. A. The patient is seen by cardiologist 3 times a year B. The patient is seen by neurologist 1 per year C. Sanatorium treatment is contraindicated D. * Sanatorium treatment in cardio sanatorium E. The patient is seen by oculist 1 per year 325. During CHF IIA. Medicies are prescribed from all of these groups, except: A. Nitrates Group B. Diuretic Group C. ACE inhibitors Group D. * NSAID Group E. ?-blockers group 326. Which statement about treatment of CHF with cardiac glycosides is false? A. Reduce heart rate B. Often have arytmohenic action C. * Reduce myocardial oxygen demand D. Used in CHF III-IV fucntional class E. Slows AV-conduction 327. Which statement about treatment of cardiac glycosides CHF is True? A. * Reduce heart rate B. Have arythmogenic action C. Reduce myocardial oxygen demand D. Used in CHF I-II fucntional class E. Have anticoagulative action 328. The absolute indication for the prescription of cardiac glycosides in patients with CHF are: A. I-II CHF fucntional class in sinus rhythm B. * Failure of diuretics and ACE inhibitors to produce results C. Hypokaliemia D. The presence of myocardial infarction E. hypertension 329. What is seen in CHF stage I.? A. * Shortness of breath, palpitations and fatigue after physical exertion B. Severe dyspnea at rest, orthopnea, night attacks of cardiac asthma, anasarca, oliguria Signs of heart failure with little physical activity and swelling on shins and thighs, the phenomena of edema in the lungs, expressed hepatomegalia C. Swelling of feet, which reduces after night, signs of heart failure at rest expressed slight, moderate liver enlargement, wheezing only in the lower parts of lungs D. E. All the above listed 330. What is seen in CHF stage III.? A. Shortness of breath, palpitations and fatigue after physical exertion B. * Severe dyspnea at rest, orthopnea, night attacks of cardiac asthma, anasarca, oliguria Signs of heart failure with little physical activity and swelling on shins and thighs, the phenomena of edema in the lungs, expressed hepatomegaly C. Swelling of feet, which reduces after night, signs of heart failure at rest expressed slight, moderate liver enlargement, wheezing only in the lower parts of lungs D. E. All the above listed 331. What is seen in CHF stage IIA.? A. Shortness of breath, palpitations and fatigue after physical exertion B. Severe dyspnea at rest, orthopnea, night attacks of cardiac asthma, anasarca, oliguria Signs of heart failure with little physical activity and at swelling on shins and thighs, the phenomena of edema in the lungs, expressed hepatomegaly C. Swelling of feet, which reduces after night, signs of heart failure at rest expressed slight, moderate liver enlargement, wheezing only in the lower parts of lungs D. * E. All the above listed 332. What is seen in CHF stage IIB.? A. Shortness of breath, palpitations and fatigue after physical exertion B. Severe dyspnea at rest, orthopnea, night attacks of cardiac asthma, anasarca, oliguria Signs of heart failure with little physical activity and swelling on shins and thighs, the phenomena of edema in the lungs, expressed hepatomegaly C. * Swelling of feet, which reduces after night, signs of heart failure at rest expressed slight, moderate liver enlargement, wheezing only in the lower parts of lungs D. E. All the above listed Chronic heart failure stage IIB and presence of angina pectoris with fucntional class IV is the basis for determining: 333. A. I disability group; B. II disability group; C. * III of disability; D. disability group is not intended E. continuation sheet disability Chronic heart failure stage IIB and the presence of chronic respiratory failure III .. with pulmonary heart is the basis for determining: 334. A. * I disability group B. II disability group C. III of disability D. disability group is not intended E. continuation sheet disability Chronic heart failure stage IIA and the presence of chronic respiratory insufficiency II-III .. with pulmonary heart is the basis for determining: 335. A. A I disability group B. * II disability group C. III of disability D. disability group is not intended E. continuation sheet disability Chronic heart failure stage IIA and presence of angina pectoris fucntional class III after transmural myocardial infarction in patients is the basis for determining: 336. A. III of disability B.I disability group C. disability group is not intended B. C. * II disability group D. E continuation sheet disability 337. Chronic heart (for right-or left type). IIB stage failure in a patients is the basis for determining: A. I disability B. * II disability group C. III of disability D. disability group is not intended E. continuation sheet disability 338. Therapy of hypertrophic cardiomyopathy consists of A. Calcium antagonists B. ?-blockers C. antiarrhythmic drugs D. Setting an artificial pacemaker E. * All the above 339. Pharmacotherapy of dilated cardiomyopathy consists of A. ACE inhibitors B. Diuretics C. cardiac glycosides D. ?-blockers E. * All the above 340. Sanatorium treatment in cardio sanatorium is shown at: A. * CHF. STAGE I; B. CHF IIA.; C. CHF IIB.; D. III CHF .. E. 341. is absolutely contraindicated Cardiac glycosides can not be combined with: A. Spironolactone B. Preparations of potassium C. * medications with calcium D. Enalapril E. Hydralazine 342. Dangerous complication of diuretic therapy are: A. Violations of atrioventricular conduction B. Hyperkinetic syndrome C. Weakness of sinus node D. * Kaliopenia with the appearance of ventricular arrhythmias E. Occurrence of atrial flutter 343. The most common cause of right ventricular failure is: A. Pulmonary embolism B. * Mitral stenosis C. Primary pulmonary hypertension D. congenital heart disease with hypervolemia in small round of heart circulation E. Left ventricular failure 344. In congestive heart failure in the urine are all of the following changes, except: A. Albuminuria, is often repeated B. High specific gravity of urine C. * High content of sodium D. * Availability of hyaline cylinders E. Periodic appearance of red blood cells 345. Protodiastolic rhythm of gallop is most typical for: A. Acute myocardial infarction with frequent ventricular extrasystoles B. Pericarditis C. * Left ventricular failure D. Hypertension in a large circle of blood circulation E. Pulmonary artery stenosis 346. One way to treat refractory edema in heart failure: A. Increasing the dose of diuretics B. Correction of plasma protein spectrum C. Limit consumption of salt and fluid D. Accession of aldosterone antagonists E. * All mentioned methods 347. When left ventricular failure is with shortness of breath, you can expect: A. Normal life and normal lung capacity total lung capacity B. Reduction of vital capacity and normal total lung capacity of the lungs C. Normal life and reduced lung capacity total lung capacity D. * Reduction of vital capacity of the lungs and reduce the overall capacity of the lungs E. Reduction of vital capacity of the lungs and increase the overall capacity of the lungs 348. What is the best recommendation to build a diet for patients with congestive heart failure? A. Do not change the habits of sustainable food B. Reduce the content of carbohydrates in the diet C. Reduce the content of potassium and sodium content increase D. * Increase potassium and lower sodium content E. Increase the calcium content and lower potassium 349. When duodenal endoscopy is defined normal: A. * 3 portions of bile B. 2 portions of bile C. 4 portions bile D. 1 portion of bile E. 5 portions of bile 350. . In normal bile which are not found A. * Cellular elements B. White C. Urobilin D. Bile acids E. Cholesterol 351. Normal total bilirubin in biochemical blood analysis is: A. * 8,5-20,5 mmol \ l B. 1,70-17,11 mmol \ l C. 0,86-5,10 mmol \ l D. 3,5-5,6 mmol \ l E. 65-80 g / l 352. Aspartataminotransferase biochemical analysis of blood in a healthy person is: A. * 0,1-0,45 mmol \ h \ l B. 0,1-0,68 mmol \ h \ l C. 1,5-5,5 mmol \ h \ l D. 0,1-1,5 mmol \ h \ l E. 0,2-0,95 mmol \ h \ l 353. Alaninaminotransferase biochemical analysis of blood in a healthy person is: A. * 0,1-0,68 mmol \ h \ l B. 0,1-0,45 mmol \ h \ l C. 1,5-5,5 mmol \ h \ l D. 0,1-1,5 mmol \ h \ l E. 0,2-0,95 mmol \ h \ l 354. In patients with cholecystitis pathological changes found in which portion of bile during endoscopy: A. * B B. C C. A D. A and C E. C and 355. A. * In patients with liver disease at the review found "vascular stars". They look like: Elevations above the skin angioma B. Yellow patches C. Scratched skin D. Hemorrhage E. Urticaria 356. In diseases of liver and biliary tract pain can arise from all causes, except: A. Stretching glisson capsules B. Spastic reduction gallbladder C. Inflammation glisson capsules D. Inflammation and stretching the walls of the gall bladder E. * Death of hepatocytes 357. Itchy skin during liver diseases indicates: A. Presence of duodeno-gastral reflux B. * Increase of bile acids in the blood against cholestasis C. Violation protein producing function of liver D. Violation of bilirubin conjugation E. Reduction detoxification function of liver 358. In patients with liver disease at the review found xanthoma. They look like: A. Elevations above the skin angiomas B. * Yellow plaques C. Scratched skin D. Hemorrhage E. Urticaria 359. When you review the patient's family doctor revealed jaundice. Sign of "true jaundice” are: A. * Icteric sclera color B. Still white sclera C. Icteric color soft palate D. Normal oral mucosa staining E. Icteric skin coloring 360. In the patient family doctor found fluid in the abdominal cavity. How does a condition called? A. * Ascites B. Hydrothorax C. Pneumothorax D. Hydropericardia E. Extravasate 361. . In a patient with liver cancer liver palpation observed the following features: A. Enlarged liver B. Reduced liver C. * Consistency - very tight, "stony" D. Smooth surface E. Surface hilly 362. In normal liver the bottom edge palpated at: A. * At the level of costal arch B. 1-2 cm below the costal arch C. 3-4 cm below the costal arch D. 1-2 cm above the costal arch E. at the level of the navel When examining the patient's family doctor found dyskinesia of biliary ducts. What research method would be most helpful to confirm the diagnosis? 363. A. * Multiple duodenoscopy B. Retrograde pancreatography C. Ultrasound D. Liver ultrasonography E. Chromatic duodenal probing . Patient ambulatory held ultrasound hepatobiliary system: the gall bladder wall thickness is normal. Which indicators is in charge? 364. A. 0.9-1,2 mm B. 1,2-1,5 mm C. 1,5-1,9 mm D. * 2-3 mm E. 3-4,5 mm . Patient with chronic cholecystitis in acute phase family physician appointed ultrasound of the hepatobiliary system. Which is probably the gall bladder wall thickness in this case? 365. A. 0.9-1,2 mm B. 1,2-1,5 mm C. 1,5-1,9 mm D. 2-3 mm E. * 3,5-4,5 mm Patient with biliary dyskinesia family doctor appointed hepatobiliary ultrasonography. Which is probably the gall bladder wall thickness in this case? 366. A. 0.9-1,2 mm B. 1,2-1,5 mm C. 1,5-1,9 mm D. * 2-3 mm E. 3,5-4,5 mm 367. Signs of chronic inflammation in the bile ducts: A. presence of leukocytes in the first phase of the chromatic duodenal probing; B. increase in leukocytes in second phase of duodenal chromatically sensing; C. increase in leukocytes in portion A; D. increase in leukocytes in portions; E. * increasing portion of leukocytes in C 368. . Needle biopsy of liver is a diagnostic method for A. * Cirrhosis B. Anemia C. Glomerulonephritis D. Atherosclerosis E. Exudative pleurisy 369. Participation in the liver nitrous exchange is: A. * All of the above B. Synthesis of proteins C. The disintegration of proteins D. Intermediate amino acid exchange E. Formation urea creatinine 370. . Which of the following doesn’t cause chronic hepatitis: A. * Acute hepatitis A B. Chronic alcoholic intoxication C. Prolonged use of hepatotoxic drugs D. Acute hepatitis B E. Working with pesticides for a long time without complying with safety technology 371. What is the mechanism action glucocorticosteroids: A. * All of the above B. Anti-inflammatory action C. Imunosupressive action D. Increases in blood glucose level E. Arterial pressure increases 372. .Which is not a contraindication for use of glucocorticosterids during autoimune hepatitis: A. * Polyarthritis B. Ulcer of stomach and duodenum C. Diabetes mellitus D. Manifest osteoporosis E. Infections 373. . The main cause of hemolytic jaundice is: A. * The elevation of formation of bilirubin from hemoglobin B. Violation capture of bilirubin hepatocytes C. Violation Process conjugation of bilirubin D. Violation excretion of bilirubin liver cells E. Violation of transport to the intestine bilirubin 374. . The main cause obstructive jaundice are: A. To raise the formation of bilirubin from hemoglobin B. Violation capture bilirubin hepatocytes C. Violation Process conjugation of bilirubin D. Violation excretion of bilirubin liver cells E. * Violation of transport to the intestine bilirubin 375. Which of the following does not lead to cirrhosis of the liver? A. * Fatty liver disease B. Autoimune hepatitis C. Chronic hepatitis B D. Chronic hepatitis C E. Chronic alcoholic hepatitis 376. Which of the following cannot cause liver cirrhosis: A. * Acute hepatitis A B. Obstruction venous outflow from liver C. Insufficiency, alpha-I-antitrypsin D. Autoimune hepatitis E. Chronic hepatitis C 377. . Laboratory parameters of inflammatory-necrotic liver cirrhosis activity are: A. * rising of the blood serum activity of transaminase B. Anemia C. Hyperamoniemia D. Thrombocytopenia E. leukocytosis 378. . In liver cirrhosis observed: A. * All of the above B. Hepato-and splenomegalia C. Edema-ascitic syndrome D. Portal hypertension E. Hemorrhagic syndrome 379. Etiological factors of cirrhosis: A. * All of the above B. Chronic blood circulation insufficiency C. Chronic hepatitis B, C D. Autoimmune hepatitis E. Insufficiency, alpha-I-antitrypsin 380. To the clinical symptoms of liver cirrhosis stage C according to Child-Pugh does not include: A. * Hyperalbuminemia B. Palmar erythema and raspberry tongue C. Ascites D. Hepatic encephalopathy E. Jaundice 381. At the initial stage (for the Child-Pugh) Differential diagnosis of liver cirrhosis is conduct with: A. * All of the above B. Fatty liver dystrophy C. Chronic hepatitis D. Amyloidosis E. Metastatic liver cancer 382. In the presence of fever in patients with liver cirrhosis Differential diagnosis is conduct with: A. * all of the above B. Parasite and fever of infectious origin C. Malignant diseases D. Leukemia E. Collagenosis 383. To medicinal preparations, which have hepatotoxic effect, belongs: A. * All of the above B. Paracetamol C. Tetracyclin D. Aminase E. 6 mercaptopurin 384. In patients with liver cirrhosis may be caused by fever: A. * All of the above B. Ascites-peritonitis C. Pneumonia D. Acute necrosis hepatic cells E. The increased sensitivity to drugs 385. Consequences of portal hypertension of liver cirrhosis are: A. * all of the above B. Splenomegaly C. Ascites D. Hyperspleenism E. Chronic systemic derive encephalopathy 386. What should we prescribe to patients with cirrhosis of the liver with ascites A. * Albumin solutions B. Liver extracts C. Methionin D. Glucocorticoids E. Biliary preparations 387. Clinical manifestations of hypokalemia in patients with cirrhosis do not include: A. * diarrhea B. Bowel atony C. Muscle weakness D. Tachycardia E. Paralytic intestinal obstruction 388. Which of the following foods do not include high amounts of potassium: A. * Cheese B. Fruit juices C. Spinach D. Parsley E. Cauliflower 389. Development of hepatic encephalopathy in patients with liver cirrhosis contribute to: A. * all of the above B. Gastro-intestinal bleedings C. narcotic analgesics and seditive drugs D. Paracenthesis E. Excessive increase diuresis 390. What is not typical for hepato encephalopathy : A. * Hyperalbuminemia B. Excitement followed by a state of confused consciousness C. Incompliance behavior D. Liver smell E. Slowness of speech, sleep disturbance 391. To treat hepato encephalopathy apply: A. * All of the above B. Quota restriction of protein in ration C. Reducing nutrient of food D. Amino acid preparations: ornitsetil, hepatitis-Merz, Glutargin E. Acidifictual therapy (medication lactulose) 392. Viral cirrhosis may develop after: A. * Acute hepatitis A B. Chronic hepatitis B C. Chronic hepatitis C D. Acute hepatitis D E. Acute hepatitis C 393. Hepatic encephalopathy and hepatic coma may complicate liver cirrhosis in: A. * Bleeding from varicose veins of esophagus B. Aldosterone antagonists, long using C. Prolonged use of lactulose D. Sharply decrease animal proteins in ration E. Decreased amount of potassium in food 394. At initial billiary cirrhosis which drug should not be taken: A. * Per oral contraceptive drugs B. Fat soluble vitamins C. Holestiramin D. D- penitsillamin E. Ursofalk 395. Idiopathic (primary) hemochromatosis: A. * all of the above B. Related to dysfunctional iron metabolism C. This genetically conditioned violation of iron exchange D. the end stage of liver cirrhosis E. Associated with the presence of hepatoma 396. Which measures contribute to liver cirrhosis prevention : A. * all of the above B. Timely treatment of chronic hepatitis C. abstinence from alcohol D. Limitations of pharmacologic preparations E. avoiding contact with toxic substances 397. The main cause of fatty liver infiltration in alcoholism: A. * The increased synthesis of fatty acids in the liver B. Raise perspicacity of cyto-membranes C. Mesenchimal-inflammatory reaction D. Intrahepatic cholestasis E. The increased delay of hyaline 398. Necessary to differentiate fatty infiltration at alcoholic lesions of liver from fatty infiltration at: A. * With all listed conditions B. diabetes mellitus C. Adiposity D. Hyper lipoproteinemia E. Lack of protein in ration 399. Development of dyspeptic syndrome in alcoholic fat infiltration of liver etiology related with: A. * It follows from lower cholesecretory liver function B. It follows from lower stomach secretion C. It follows from the development of reflux esophagitis D. It follows from the development hemorrhagic syndrome E. It follows from splenomegalia 400. Dyspeptic syndrome with fat infiltration of liver worsens when a patient receives: A. * Fats B. B.Protein food C. Carbohydrates D. Fruit juices E. Fluid 401. Complete exclusion of alcohol in alcoholic liver fat infiltration etiology was made leads to: A. * The full normalization of liver function B. Fibrosis livers C. Only a slight improvement in temporal D. Liver steatosis E. Biliary dyskinesia 402. In the treatment of alcoholic fatty liver infiltration etiology the key treatment is: A. * Refusal from alcohol B. Lipotropic drugs C. Starvation of treatment D. Vitamin therapy E. Limitations in protein food 403. When we ask anamnesis morbi in patients of chronic liver disease is necessary to note: A. * All of the above B. The time during which the patient took in large quantities of alcohol C. Tolerance to alcohol D. if the patient engages in binge drinking E. Losing situational control 404. Chronic alcoholic hepatitis necessary to differentiate with various liver diseases except: A. * Syndrome Zollinhera-Ellisona B. Rotor syndrome C. Syndrome Zhilbera D. Fatty liver infiltration E. Wilson-Konovalov disease 405. Compensation stage of pathologic process of liver cirrhosis evaluated by a criteria-Child-Pyu: A. * All of the above B. Hypoalbuminemia C. Hypoprothrombinemia D. The presence of ascitis E. The presence encephalopathy 406. One of the main features, allowing to distinguish alcoholic liver cirrhosis from alcoholic hepatitis: A. * The presence of portal hypertension B. Severity pain syndrome C. Severity dyspeptic syndrome D. The development of jaundice E. Performance tests of functional liver 407. According to which etiology were selected following types cirrhosis: A. * All of the above B. Virus C. Toxic D. Biliary E. Cryptogenous 408. At jaundice form of hepatitis is observed: A. * yellow feces B. Eclipse of urine C. Light feces D. Total weakness E. Dyspeptic disorders 409. In staging hepatitis B virus it is important to define: A. * serological markers - HBsAg, anti-HBs, anti-HBc, HBeAg, anti-HBe B. Clinical manifestations of disease C. Dynamics of biochemical and functional tests of liver D. Hepatoscintographia E. Ultrasound investigation of liver 410. acute hepatitis is worsened by: A. * All of the above B. Physical work C. Drinking alcohol D. Pregnancy E. Excessive food 411. In patients with loss of appetite and weight in biliary disease we can suspect: A. * Gallbladder Cancer B. Acute cholecystitis C. Acute cholangitis D. All of the above E. Acute pancreatitis The presence of blunt pain in the right supracostal, fever in patients with removed gall bladder may indicate: 412. A. * Development cholangitis B. Aggravation of chronic gastritis C. Aggravation of Duodenal Ulcer D. Gilbert syndrome E. GERD 413. Electrophoresis with spasmolytics should be given to patients with: A. * Hypertension gall bladder B. Hypotension gall bladder C. Chronic pancreatitis D. All listed correctly E. Acute cholecystitis 414. For the successful dissolution of cholesterol stones most important is: A. * Concentrational property gall bladder B. High tone gall bladder C. Dimensions gall bladder D. Form gall bladder E. Gastric secretion 415. Antibiotic therapy shown in cholecystitis, with A. * All of the above B. The increased body temperature C. Leukocytosis D. Sustainable pain syndrome E. When inefficient without prior antibiotics therapy 416. When selecting antibiotics in treatment of patients with chronic cholecystitis consider: A. * All of the above B. The reason for the aggravation of cholecystitis C. Ability to concentrate antibiotics gall D. Microflora`s sensitivity to antibiotics E. Individual tolerance to drugs 417. On the synthesis of bile acids have an effect on: A. * All listed B. Genetic factor C. Sex D. Age E. Character meals 418. What features proteinogramme in blood are characteristic of chronic hepatitis? A. Normoalbuminemia B. * Hypoalbuminemia C. Hyperalbuminemia D. Hypoglobulinemia E. Normoglobulinemia 419. What are the main regulatory mediators of immuno-component cells: A. * Interleukins B. Kinins C. Serotonin D. Heparin E. Histamine 420. Which of the investigations show activity of autoimmune processes? A. seruloplasmin content B. aminotransferase activity C. CRP content D. * titer antibodies E. seromucoid content 421. What is factor is a nonspecific protector ? A. T- lymphocytes B. B- lymphocytes C. Natural killer cells D. * Neutrophilic leukocytes E. T-helpers 422. Which hormones are antioxidant and have membrane stabilizing action? A. Estrogens B. * Androgens C. Progesterone D. Mineralocorticoid hormone E. Estrogens and Progesterone 423. What symptoms are specific for arthritis? A. * Joint pain during all movements B. Swelling C. Increased skin temperature D. Hyperemia of skin E. Laboratory markers of inflammation activity 424. What symptoms are specific for arthritis? Joint pain, which increases during movements, narrowing gap in joints, osteoporosis of epiphysis, erosion of articular surfaces A. * B. Absence of joints deformation C. Full range of motion of joints D. Presence of osteofites, subchondral osteoporosis E. Local pain in the joints with normal x-ray pictures 425. What are the most frequent side effects of prolonged use of glucocorticoids ? A. Osteoporosis B. Inhibition of adrenal cortex function C. Activation of infection D. Myopathy E. * All of the signs mentioned 426. What effect do glucocorticoids have on inflammation? A. reduce permeability of capillaries B. increase the number of neutrophils in blood C. suppress the migration of leukocytes D. suppress phagocytosis of pathogens and products of inflammatory reaction E. * all of the mentioned above 427. Which group of drugs has immunomodulatory effect ? A. Nonsteroid anti-inflammatories B. Glucocorticoids C. * Thymus preparations D. Cytostatics E. Antibiotics 428. Which of the following physical immunomodulators are not used in treatment of rheumatic diseases ? A. Hemosorbtion B. Plasmapheresis C. Lymphotocytopheresis D. * Synovectomy E. Thoracic duct drainage 429. Which of the following is not part of treatment with cytostatic therapy ? A. Accuracy of diagnosis B. Detection of contraindications C. Rigorous evaluation of clinical evidence D. Poor effect of previous therapy E. * Assumption on presence of rheumatoid vasculits 430. Which disease requires ethiotropic therapy? A. * Reiter's disease B. Wegener's disease C. Systemic sclerosis D. Horton's disease E. Titce’s disease 431. What are the nonspecific protection factors of the body? A. Germicidal of skin B. Hydrolytic enzymes C. System of macrophages D. Lysozyme, properdin E. * all listed 432. What are the main functions of the immune system : A. Destruction of "debris" by hydrolytic enzymes B. Screening of cells through blood circulation C. Production of specific antibody molecules D. Production of CIC E. * All of these functions 433. Which is the true statement about joint cartilages? A. Without vascularization B. Without enervation C. Include collagen and proteoglycans D. none of above E. * all numbered 434. Ethiotropic therapy of reactive arthritis include: A. Penicillin B. * Tetracycline C. Sulfanilamides D. Fluoroquinolone E. Cephalosporines 435. Which of the chronic liver diseases require treatment of corticosteroids? A. Active viral hepatitis in the of seroconversion B. Idiopathic autoimmune hepatitis C. Cholestatic hepatitis as a pre-stage of PBTS D. Liver cirrhosis with splenomegaly E. * for all of the diseases 436. What is the nature of the joint injury during chronic active hepatitis? A. * reactive arthritis B. ankylosing spondiloarthritis C. osteoarthritis D. none of above E. all listed 437. Which signs are characteristic for skin-trombanhitis syndrome with nodular polyarthritis ? A. subcutaneous nodules B. livedo C. soft tissue necrosis D. peripheral gangrene E. * all listed Which of the following drugs are contraindicated to patients with nodular polyarthritis and presence of HveAg in serum : 438. A. Prednisolone B. plasmapheresis C. vidarabin D. * cyclophosphamide E. interferon 439. Which sign can help to differentiate rheumatoid arthritis from nodular poliarteriyitis? A. vistserytis B. Arthritis C. * fibrosing alveolitis D. fever E. pneumonitis 440. Which of the following are complications of nodular polyarthritis ? A. myocardial infarction B. retinopathy with visual violations C. chronic renal insufficiency D. stroke E. * all listed 441. What is the basic therapy for patients with nodular polyarthritis with affection to systems? A. glucocorticosteroids B. Cytostatics C. Prednisolone D. * glucocorticosteroids, cytostatics E. nonsteroidal anti-inflammatory drugs 442. Which symptoms can be found on the eye fundus in patients with nodular polyarthritis? A. retinal edema B. angiospasm C. aneurysmic vasodilatation D. hemorrhage E. * all of the listed 443. What is the most typical localization of affections of the joints in patients with rheumatoid arthritis: A. * small joints of the hands, feet B. knee joints C. elbow joints D. temperomandibular joint E. hip joints 444. What is the frequency of the joint form of rheumatoid arthritis: A. * 80 - 90% B. 70 - 80% C. 50 - 60% D. 30 - 40% E. 10% 445. Which damage of the pleura most frequently occurs in patients with rheumatoid arthritis ? A. * dry pleuritis B. interlobar pleuritis C. exudative pleuritis D. purulent pleuritis E. pleuritis does not occur 446. Which form of lung injury predominates in patients with rheumatoid arthritis ?: A. * interstitial pneumonia B. there is no affection C. membranous pneumonia D. bronchopneumonia E. abscess pneumonia Which form of liver and gastrointestinal tract injury predominates in patients with rheumatoid arthritis? 447. A. * intestinal amyloidosis B. atrophic gastritis C. erosive gastritis D. enteritis E. fatty infiltration of liver 448. What are the most characteristic signs of prodromal stage of rheumatoid arthritis? A. * Feeling stiffness in the morning B. Moderate joint pain C. Reaction to weather changes D. Decrease appetite, weight loss E. Palpitations, sweating, subfebrile temperature 449. What are the most characteristic signs of prodromal stage of rheumatoid arthritis? A. * feeling of morning stiffness B. moderate joint pain C. reaction of weather changes D. decreased appetite, weight loss E. palpitations, sweating, subfebrile temperature In which location are rheumatoid nodules most frequently localized in patients with rheumatoid arthritis ? 450. A. * In elbow joints B. posterior surface of interphalangeal joints C. external surface of the knee joint D. In heel tendons E. sternum area, shoulder blades area 451. In first stage of rheumatoid arthritis which symptoms are seen on X –ray ?: A. * Osteoporosis B. narrowing of the joint spaces, osteophites C. Osteophites and narrowing of cartilage D. Changes on cartilaginous surfaces, narrowing of the joint spaces E. ankylosis 452. Which symptoms are seen on X –ray during second stage of rheumatoid arthritis: A. osteoporosis, narrowing of the joint spaces B. * osteoporosis, narrowing of the joint spaces, osteophites enlightenment C. decrease of cartilaginous surfaces D. ankylosis E. osteophites enlightenment narrowing of cartilage 453. Which symptoms are seen on X –ray during the third stage of rheumatoid arthritis: A. * osteoporosis, osteophites enlightenment narrowing of cartilage B. osteoporosis C. osteophite enlightenment, D. narrowing of cartilage E. narrowing of the joint spaces 454. Which symptoms are seen on X –ray during IV –stage of rheumatoid arthritis: A. Osteoporosis, narrowing of cartilage, osteophites enlightenment B. narrowing of the joint spaces C. * ankylosis, double joints, cartilage narrowing D. narrowing of cartilage, double joints, osteophite enlightenment E. narrowing of cartilage 455. What is the specific characteristic for seropositive rheumatoid arthritis? A. presence of rheumatoid factor in serum B. titer of rheumatoid factor 1:32 C. titer of rheumatoid factor 1:16 D. absence of rheumatoid factor in serum E. * rheumatoid factor titer over 1:32 456. What does the rheumatoid factor show? A. * unfavorable course of disease B. possibility of relapse C. stable remission D. high activity of the process E. low activity of the process 457. When will you determine the anti-nuclear factor in patients with rheumatoid arthritis ? A. presence of vasculitis B. pseudoseptic syndrome C. severe course of disease D. * mixed syndrome E. joint form of disease 458. What does “rahocyte” in patients with rheumatoid arthritis mean? A. neutrophils with adipoid inclusions B. * neutrophils with protein inclusions C. neutrophils of rheumatoid factor D. synovial fluid lymphocytes E. synovial fluid neutrophils 459. What is the most frequent combination of rheumatoid arthritis and the other disease ? A. * RA + OA B. RA + SLE C. RA + rheumatism D. RA + SS E. RA + gout 460. What does the Felty syndrome mean ? A. rheumatoid arthritis with visceritis B. * splenomegaly, lymphoadenopathy, pancytopenia in patients with rheumatoid arthritis C. high activity of RA process D. RA with the presence of LE cells in blood E. low activity of RA process 461. What are the main laboratory markers for inactive RA? A. * Alpha-2 Globe. to 10%, CRP (-), ESR 12 mm / h B. Alpha-2 Globe. 10% C. CRP (-), ESR 12 mm / h D. ESR 12 mm / h E. ESR 20 mm / h 462. What are the main laboratory markers for first degree of activity in RA? A. * Alpha-2 Globe. to 12%, and CRP (+), ESR 20 mm / h B. Alpha-2 Globe. 10%, CRP (-) C. CRP I (+) D. CRP I (+), ESR 20 mm / h E. Alpha-2 Globe. 12% 463. What are the main laboratory markers for II degree of activity in RA ? A. * Alpha-2 Globe. 15%, CRP 2 (+) B. SRB 2 (+) C. Alpha-2 Globe. 12% D. ESR 40 mm / h E. ESR 50 mm / h, and CRP (+) 464. What are the main laboratory markers for degree of activity in RA? A. * Alpha-2 Globe. more than 15%, CRP 3 (+), ESR 40 mm / h B. ESR 60 mm / h C. CRP 4 (+) D. Alpha-2 Globe. 17% E. CRP I (+) 465. What does the index of Ritchie or joint index in patients with rheumatoid arthritis mean? A. * sum of pain scores of affected joints B. definition of pain scores during palpation of the joints C. double joint pain D. assessment of joint pain by patients themselves E. severity of the pain syndrome 466. What are the main clinical signs for inactive RA? A. * absence of morning stiffness, hyperthermia, exudation B. absence of hyperthermia C. exudative changes are not expressed D. minor joint pain E. morning stiffness for 30 minutes 467. What are the main clinical signs for first degree of activity in RA? A. * morning stiffness during 30 minutes, hyperthermia, exudation is expressed B. morning stiffness during 30 minutes, moderate pain C. exudative changes are minor D. slight hyperthermia E. morning stiffness longer than 1 hour 468. What are the main clinical signs for II degree of activity in RA? A. * morning stiffness till 12 o clock, moderate hyperthermia B. morning stiffness for 2 hours, moderate pain C. mild hyperthermia D. exudative changes are expressed E. exudative changes are moderate 469. What are the main clinical signs for III degree of activity in RA? A. * stiffness during the day, pain, hyperthermia are expressed B. stiffness during the day, the pain is expressed C. hyperthermia is expressed D. effusion of the joint E. morning stiffness till 3:00 470. Which of the following are not signs of nodulas erythema? A. dense painful subcutaneous nodules B. discoloration of the skin over the nodules C. acute beginning of fever D. * abscesses E. ESR increase 471. What is the most typical localization of disease of joints in patients with Bekhterev disease? A. * hipbone B. elbow C. shoulder D. joints of the feet E. wrist joints 472. Which factors can contribute significantly in the development of gout? A. Hereditary B. Alcohol C. abuse of fatty foods D. excessive physical activity E. * all of the factors 473. What is the most frequent clinical form of osteoarthritis? A. * knee joint osteoarthritis B. leg joint osteoarthitis C. osteoarthritis of spine D. osteoarthritis of distal interphalangeal joints of hands E. osteoarthritis of the first plyusnephalangea joint 474. What does nodulas erythema mean? A. swelling of the subcutaneous tissue B. skin swelling C. partial lysis of basal membrane of skin epithelium D. * complex allergic reaction to the development of subcutaneous nodes E. necrosis of mosaic membrane 475. What age group is most commonly affected by brachiscapula periarthritis ? A. 18-25 years B. 20-30 years C. 30-40 years D. * 40-60 years E. 60-80 years 476. Which are symptoms are characteristic for chronic ankylosing brachiscapula periarthritis? A. moderate pain in the shoulder joint during movement and resistance B. significantly reduces the allocation and rotation C. osteoporosis of shoulder D. symptom of "mechanical blockage." E. * all of the listed 477. Characteristic of expressed kyphosis in aseptic necrosis of epiphysis of the thoracic vertebrae are seen in ; A. * disease Sheyermana Mau B. chondrodystrofy C. acromegaly D. Kashina- Beck disease E. rickets 478. What is the main clinical symptoms of peryarthritis of radiopalmaris joint? A. pain in bone B. pain above the inner edge radiopalmaris joint C. limited swelling of radiopalmaris joint D. osteoporosis of shylovydny bone E. * all of the listed 479. What are the main clinical features of foot periarthritis? A. pain is associated with movement, with the participation of the affected tendon B. normal passive range of movements C. absence of inflammatory process of the joints D. radiological presence of osteoporosis and peryosthitis, osteofites E. * all of the listed 480. Give the definition of "ligamentit”: A. inflammatory affection of the joint ties B. * inflammatory laffection out joint ties C. allergic affection of the joint ties D. degenerative affection of the joint ties E. allergic affection of the joint ties and out joint ties 481. Which group is mostly affected by osteoarthritis? A. young women B. * men C. children D. adolescents E. women during menopause 482. When osteoarthritic pain is usually intensified? A. Afternoon B. in the morning C. * during walking, "starting pain." D. while standing E. at night 483. How often does lung injury happen in patients with Bekhterev disease? A. * rarely B. often C. are in 100% cases D. never E. are in 50% 484. What does juvenile rheumatoid arthritis mean? A. * RA in children B. clinical forms of RA in the elder age C. RA with viscerits D. RA with high degree of activity E. mono-, oligoarthritis 485. Which antibodies are known as rheumatoid factor? A. Immunoglobulin A B. immunoglobulin G C. * Immunoglobulin M D. immunoglobulin E E. immunoglobulin D 486. What are the characteristic signs for Bekhterev disease ? A. * absence of RF B. low titer of LDA-O C. lack of phenotype of histocompatibility D. presence of rahocytes E. thrombocytopenia 487. One of the following is not a disease modifying drug in rheumatoid arthritis - A. Auronaufin B. D-pencillamine C. Chloroquine D. * Indomethacin E. Crisanole 488. Rheumatoid arthritis pericarditis is – A. Serous B. * Fibrinous C. Serofibrinous D. Adhesives E. Exsudative 489. Which one of the following is not associated with rheumatoid arthritis - A. Pleural effusion B. Pulmonary hypertension C. Cricoarytenoid arthritis D. Fibrosing alveolitis E. * Joint errosias Which one of the following is least likely to occur in late extra articular sero-positive rheumatoid arthritis 490. A. Neutropenia B. Dry eye C. Leg ulcers D. * Hepatitis E. Pleuritis Human leukocyte antigen (HLA) DR 4 occurs in about 7% of patients with rheumatoid arthritis HLA DR4 encoded in the major histocompatibility complex (MHC) region on 491. A. * Chromosome 6 B. Chromosome 9 C. Chromosome 18 D. Choromosome22 E. Chromosome 3 492. Regarding rheumatoid arthritis, which one of the following statements is correct ? A. NSAIDs are helpful in controlling the disease process B. Corticosteroids, on long term basis, are to be given in all cases C. * DMARDs should be given early and preferably in combinations D. Every patient of rheumatoid arthritis has a positive rheumatoid factor E. 50% patients of rheumatoid arthritis has a positive rheumatoid factor 493. All of the following are seen in inflammatory polyarthritis, except - A. * New bone formation B. Spontaneous flare C. Increased ESR D. Morning stiffness more than one hour E. Decreased ESR 494. Which part of the spine is most commonly affected in Rheumatoid arthritis - A. * Cervical B. Lumbar C. Thoracic D. Sacral E. Whole spine 495. Part of spine, involved in Rheumatoid arthritis is - A. * Cervical B. Thoracic C. Lumbar D. Sacral E. Whole spine 496. Which of the following is true regarding Rheumatoid arthritis - A. Typically involves small and large joints sym metrically but spares the cervical spine B. * Causes pleural effusion with low sugar C. Pulmonary nodules are absent D. Enthesopathy prominent E. All of the above 497. The following are rheumatoid disease drugs except - A. Chloroquine B. Gold C. Penicillamine D. * BAL E. Methotrexate 498. Gold salts can be used in - A. Ankylosing spondylitis B. * Rheumatoid arthritis C. Osteoarthritis D. Behcet's syndrome E. Cancers 499. Indication of systemic steroids in rheumathoid arthritis is - A. * Mononeuritis multiplex B. Carpul tunnel syndrome C. Presence of deformities D. Articular cartilage involvement E. All of the above 500. What is the indication of using systemic steroids in a case of rheumatoid arthritis - A. Carpal tunnel syndrome B. Presence of deformities C. * Mononeuritis multiplex D. Involvement of articular cartilage E. All of the above 501. Hemophilia with rheumatoid arthritis, analgesi of choice- A. * Ibuprofen B. Aspirin C. Aetaminophen D. Phenylbutazone E. Morphine 502. What is the biological effect of vasopressin? A. Reduces blood pressure. B. * Increases muscle tone of uterus . C. Increases the tone of blood vessels. D. Affects the processes lactopoesis. E. All of the above noted. 503. . Which laboratory parameters are typical for secondary hypothyroidism? A. Low levels of corticotropine. B. High level thyroliberine. C. Low level thyroliberine. D. * Low levels of thyrotropine . E. The high level of thyrotropine. 504. What are the clinical manifestations of somatotropic diseases? A. * Low growth . B. Cachexia. C. Hypogonadism. D. The decrease of muscle mass. E. All answers are correct 505. What are the clinical manifestations of corticotropine deficiency? A. Hypertension. B. Hyperpigmentation of the skin. C. * Low blood pressure . D. Hypokalemia. E. All answers are correct 506. What are the most typical biochemical parameters of blood during Simmonds disease? A. Hyperglycemia. B. * Tendency to hypoglycemia C. Hyperkalemia. D. Hypernatremia. E. Hyponatremia. 507. What is the main test for the differential diagnosis between primary and secondary hypogonadism? A. Large dose of Dexamethasone trial B. Test with human chorionic gonadotropine C. * Determination of the level of LH, FSH . D. Determination of urinary 17 - ACS. E. Determining the level of gonadal hormones. 508. What tests should be done to investigate pituitary function? A. Dexamethasone test. B. * Test with metopirone . C. Test with thyrotropine. D. Test with tiroliberine E. Test with GnRH. 509. Which etiological factor is often the cause of hypothalamic forms of adiposity? A. Constitutional feature. B. Genetic inheritance C. * Neuroinfections . D. Nutritional factor. E. Trauma of the skull. 510. What is the direct effect of thyrotropine? A. Affects the processes of osteogenesis. B. Stimulates the development of the nervous system. C. Stimulates the growth and development of the thyroid gland. D. * Stimulates the producing of thyroid hormones E. Regulates thermogenesis. 511. Which electrolyte disorders are the most common in patients with hypopituitarism? A. Hypernatremia B. Hypokalemia. C. Hyperkalemia. D. * Hyponatremia . E. Hyperchloremia. 512. What are the most frequent symptoms of alimentary - constitutional adiposity? A. rapid increase in body weight. B. * slow increase in body weight . C. presence of autonomic disorders. D. Dysplastic distribution of adipose tissue. E. Uniform distribution of adipose tissue. 513. What are the main clinical manifestations of adipose - brilliant dystrophy? A. * Hypogonadism . B. Gynaecomastia. C. The presence of small pink stretch marks or striae D. Adiposity. E. All answers are correct. 514. Which drug affects the secretion of corticotropin during Itsenko – Cushing disease? A. Ergobromkriptine. B. * Cyproheptadine . C. Hloditan. D. Reserpine. E. Nootropil. 515. Which hormonal indices are similar in patients with adipose - genital dystrophy? A. The high level of gonadotropines. B. High levels of sex hormones. C. Increased excretion of 17 – COP D. * Low levels of sex hormones . E. All answers are correct. What is the most frequent etiological factor that causes the development of neurogenic diabetes insipidus? 516. A. * Brain tumor . B. Skull trauma. C. Tubulopathy. D. Acute and chronic infections. E. All answers are correct. 517. Which symptoms are not characteristic for Diabetes Insipidus? A. Thirst. B. Polydipsia. C. Polyuria. D. * Dysuric manifestations . E. Sleep disorders. 518. Which disease should be differentiated with diabetes insipidus? A. Diabetes. B. Hyperparathyroidism. C. Psychogenic polydipsia. D. Chronic pyelonephritis. E. * All of the above . 519. Which functional tests are used in the diagnosis of diabetes insipidus? A. With clonidine. B. With hypothiazid. C. With dexamethasone. D. * With fluid limitation E. With starvation. 520. Which drugs are used for the treatment of diabetes insipidus? A. * Analogues of arginine - vasopressin . B. Pituitrin. C. Hypothiazid. D. Miskleron. E. Clonidine. 521. .What is the possible effects of ADH analogues? A. Depression. B. Hyper-excitability. C. Loss of vision. D. Convulsive disorder. E. * Headache . 522. What clinical signs are the most common for the syndrome of inappropriate production of vasopressin? A. Thirst. B. Edema. C. * Oliguria . D. Headaches. E. Nausea, vomiting. Which disease should be differentiated with the syndrome of inappropriate overproduction of vasopressin? 523. A. Adrenal insufficiency. B. Hypothyroidism. C. Hypogonadism. D. * Congestive heart failure . E. Kidney disease. 524. Which drugs decrease the secretion of vasopressin? A. Oxytocin. B. * Glucocortu1qcoids . C. Alcohol. D. Noradrenaline. E. All of the above. 525. .Where is the primary damage in the endocrine system during Itsenko – Cushing Disease? A. Gonads. B. * Hypothalamus . C. Adrenals. D. Pituitary gland. E. Thyroid gland. 526. . What are the clinical manifestations in excess of mineralocorticoids? A. * Increased blood pressure . B. Hypernatremia. C. The decrease in cardiac output. D. Edema. E. All of the above. 527. . All these symptoms are typical for manifestations of Hyperandrogenism in women, except A. Hypertrichosis. B. Alopecia. C. * Purple - red "striae" . D. Atrophy of the testicles. E. All of the above noted. 528. Which clinical manifestations are not typical for Itsenko – Cushing disease? A. Obesity. B. Osteoporosis. C. * Leukopenia . D. Hypertension. E. All of the above noted. 529. What is the cause of the stretch marks or striae in patients with Itsenko – Cushing disease? A. Thrombosis of the capillaries of the skin. B. * Catabolic action of glucocorticoids in the proteins of the skin . C. Hemorrhage. D. All of the above. E. High blood pressure What is the difference between endocrine - exchange form of hypothalamic syndrome and Itsenko – Cushing disease? 530. A. Milder symptoms of hypercortisolism. B. The presence of osteoporosis. C. * Positive "small Dexamethasone test" . D. All of the above. E. the appearance of osteosclerosis. 531. Which drugs reduce the secretion of ACTH in patients with Itsenko – Cushing disease? A. Parlodel. B. Metopiron. C. Hloditan. D. * Cyproheptadine . E. Reserpine. 532. What disease is characterized by increased production of somatotropic hormone? A. Marfan's syndrome. B. * Acromegaly . C. Premature puberty. D. Gigantism. E. Sotos syndrome. 533. What are the early clinical manifestations which are observed in acromegaly? A. Visual impairment. B. * Disturbance of sexual function . C. Increased thyroid function. D. Reduced thyroid function. E. Improved features thyroid glands. 534. What is the method of treatments in Itsenko - Cushing's disease ? A. Unilateral adrenalectomy. B. Two-sided adrenalectomy. C. * Removal of pituitary adenoma . D. Telegammatherapy plot pituitary. E. All of the above noted. 535. What kind of lipid dysfunction in metabolism is characteristic for acromegaly? A. Decline in total lipids. B. * Increased levels of free fatty acids . C. Increased cholesterol levels. D. Cholesterol reduction. E. All of the above noted. 536. What is the characteristic change of carbohydrate metabolism during acromegaly? A. Remains unchanged. B. Reduces the tolerance to carbohydrates. C. * Increases the tolerance to carbohydrates . D. Increases gluconeogenesis. E. Reduces gluconeogenesis. 537. What changes in laboratory parameters is observed during acromegaly? A. Reduction of phosphorus levels in the blood. B. Increasing of phosphorus levels in the blood. C. Reducing the level of calcium in the blood. D. * Increasing the level of calcium in the blood . E. Reducing of residual nitrogen levels. 538. What is the reaction of peripheral endocrine glands in the initial stage of development of acromegaly? A. Hypofunction. B. Hyperfunction. C. * Hyperfunction with a transition to hypofunction . D. No change. E. Severe hypothyroidism 539. What are the etiological factors in Parchone syndrome? A. Involvement of the central nervous system. B. Lung tumors. C. Drugs. D. Pulmonary tuberculosis. E. * All of the above. 540. Which drugs can promote hyperhydropexic syndrome? A. * Oxytocin . B. Chlorpropamide. C. Clofibrate. D. Reserpine. E. All of the above noted. 541. Which disease should be differentiated with syndrome of Parhon? A. Chronic glomerulonephritis. B. * Hypothyroidism . C. Allergic edema. D. Scleroderma. E. All of the above. 542. Which symptoms characterize the syndrome of Parhon ? A. Excessive sweating. B. Decreased sweating. C. * Oliguria . D. Hypotension. E. All of the above. 543. What are the symptoms that indicate the presence of water intoxication? A. General weakness. B. Nausea, vomiting. C. Headache. D. Increased appetite. E. * Adynamia . 544. Which cases can cause increase in level of somatotropic in serum? A. In cirrhosis of the liver. B. * In neurogenic anorexia . C. In glucagonomy. D. During starvation. E. All of the above noted. What are the functional tests that are used for the investigation of somatotropin-productivity in pituitary function? 545. A. * Test with a load of insulin . B. Dexamethasone test. C. Test with klomifenom. D. Test with clonidine. E. Exercise testing. 546. Where is the location of adenoma in patients with acromegaly? A. Intracellular and supracellular B. Supracellular and intracellular C. extracellular D. * Intracellular, supracellular, intracellular E. Extracellular and intracellular 547. The normal increase in growth hormone secretion occurs during: A. After meals. B. * 1 hour after falling asleep . C. During exercise. D. When starvation. E. All of the above noted. 548. What changes are characteristic in bones in Itsenko – Cushing disease? A. * Diffuse osteoporosis . B. Deforming arthritis. C. Sudperiostalny osteoporosis. D. Osteosclerosis. E. Rheumatoid arthritis 549. Which symptoms are characteristic in Simmonds disease? A. Muscle weakness. B. Muscle pain. C. Skin pigmentation. D. * Sharp decrease in body weight . E. Hypotension. 550. Which drugs should be used in patients with hypopituitarism? A. * Cortisol . B. Thyrotropin. C. Chorionic gonadotropin. D. Thyroid hormones. E. Sex hormones. 551. Water intoxication of Parchone syndrome causes: A. General weakness. B. Weakness. C. Headaches. D. Insomnia. E. * All the above mentioned . 552. What are the complications in patients with diabetes insipidus using adiurecrine: A. Chronic rhinitis. B. Bronchospasm. C. Pulmonary fibrosis. D. Resistance to the drug. E. * All the above-mentioned . 553. Which function of the adrenal cortex is characterized by the daily excretion of 17 - ketosteroids in the urine? A. Glucocorticoid B. Mineralocorticoid C. Exchange D. Corticogenic E. * Androgenic 554. .When is the maximal secretion of corticotropin? A. Night B. * In the morning C. Day D. In the evening hours E. At dinner 555. .Daily excretion of 17 ACS is characterized by: A. Mineralocorticoid B. * Glucocorticoid C. Androgenic D. Corticogenic E. Exchange .Which drugs are the best for treatment of patients with hypocortitsizm in combination with hypertension? 556. A. Doxa B. * Prednisolone C. Furatsilin D. Insulin E. Clonidine .What needs to be done to differentiate the diagnosis between the disease and the syndrome of Itsenko - Cushing's: 557. A. The sample with the introduction of ACTH B. Small sample Deksametazon C. * Large sample Deksametazon D. The sample with the introduction of insulin E. The sample with the introduction of furosemide 558. .Small Dexamethasone test is positive for: A. Diseases Itsenko – Cushing B. Itsenko Syndrome – Cushing C. Androsteromah D. * Hypothalamic pubertal syndrome E. Diabetes .Which factors first of all can be attributed to the etiological in the development of disease Itsenko Cushing? 559. A. Neuroinfections B. * Pituitary microadenoma C. Skull injury D. Diabetes E. Obesity 560. .The Androsterome is characterized by: A. High level of urinary excretion of 17 ACS B. * High level of urinary excretion of 17 CS C. Low levels of urinary excretion of 17 COP D. Increase of cortisol in blood levels E. -Reducing the level of leptin 561. .Which type of glycemic curve is characteristic for Addison's disease? A. Diabetic B. Vezhopodibna C. * Flat D. Gothic E. Two-humped 562. .When is the highest level of corticosteroids in the blood? A. 6 - 7 am; B. 10 - 12 hours C. 16 - 18 hours D. 20 - 22 hours E. 22 - 24 hours 563. .Which test can help to identify any functional depot of the adrenal cortex? A. Dexamethasone test B. * One-day test with corticotropin C. Metapyron test D. A sample of the insulin E. Sample with treadmill .During which abnormality increased excretion in the urine 17 ACS beginning only in the second - the third day after the test Labharta? 564. A. * In secondary adrenal insufficiency B. In primary adrenal insufficiency C. In adrenal hyperplasia D. In absence of pathology of the hypothalamic - pituitary - adrenal system E. In diabetes Type III 565. .Which daily dose of dexamethasone is needed to conduct during a small sample? A. 1.5 mg B. * 2 mg C. 3 mg D. 4 mg E. 5 mg 566. Which daily dose of dexamethasone is needed to conduct during a large sample? A. 4 mg B. 6 mg C. * 8 mg D. 10 mg E. 20 mg 567. . Primary hyperaldosteronism is characterized by : A. * Reducing the level of potassium in the blood plasma B. Normal level of potassium in erythrocytes C. Reduced glucose tolerance D. Reducing the level of calcium in the blood E. Reducing the level of leptin in the blood 568. .For hypocortisone characteristic features are all, except: A. Weight Loss B. Loss of appetite C. Abdominal pain D. Dermatomelasma E. * The presence of edema All of the following statements concerning radioactive iodine treatment for Graves' disease are correct EXCEPT 569. A. it is a painless procedure B. it is indicated in patients who are low-risk candidates for surgery C. the incidence of hypothyroidism is higher than with surgical treatment D. * the incidence of hypothyroidism is decreased by giving frequent small doses E. thyroid storm is a complication An inappropriate localization study for a patient with primary hyperparathyroidism before initial neck exploration is 570. A. CT-scan B. technetium thallium scan C. * angiography D. sonography E. barium swallow During neck exploration for hyperparathyroidism, the left inferior gland is not identified. The most appropriate next step is to 571. A. * remove the thymus through the cervical incision B. perform median sternotomy and explore the mediastinum C. remove the three identified normal-appearing glands D. terminate the operation E. perform total thyroidectomy A typical battery of blood tests used for initial assessment of liver cirrhosis includes measuring all of the following except: 572. A. * urea B. Aminotransferases C. Gamma-glutamyl transferase D. autoantibodies E. Alpha 1-antitrypsin. 573. According to ERCP, what are found to have associations with chronic pancreatitis? A. * Biliary obstruction and Pancreatic duct abnormalities B. Pancreatic duct abnormalities C. Biliary obstruction D. None of mentioned E. Tumor of pancreas 574. A. * Adversely affect survival include all of the following except anemia less than 70 g/l B. age greater than 55 years, C. leukocytosis greater than 16,000/µm, D. LDH greater than 400 IU, E. AST greater than 250 IU/L. 575. All are true about pseudopancreatic cyst except A. Presents as an abdominal mass B. Serum amylase is increased C. Common after acute pancreatitis D. Common after acute cholecystitis E. * Most common site is in head of pancreas 576. All are true regarding Zollinger Ellison syndrome, except: A. severe peptic ulceration B. Hypergastrinemia C. Diarrhoea D. increased levels of the hormone gastrin E. * Decreased ratio of BAO to MAO 577. All of following may be in acute pancreatitis except: A. Hyperbilirubinemia B. Serum alkaline phosphatase is elevated C. Serum aspartate aminotransferase is elevated D. Elevated serum lactic dehydrogenase E. * 578. A. * Serum albumin is increased All of the following have been used in management of Acute Pancreatitis except Interleukin-10 B. Quamatel C. Somatostatin D. Peritoneal dialysis E. None of the listed 579. All of the following statements about Pseudopancreatic cysts are true except: A. Cystojejunostomy is treatment of choice B. Serum amylase levels are increased C. Presents as an epigastric mass D. Most common site is in body and tail of pancreas E. * Percutaneous aspiration is treatment of choice 580. All the following are causes of Acute Pancreatitis except: A. Alcohol B. Gall stones C. Hypercalcemia D. Hyperlipidemia E. * Hemochromatosis A 65-yr-old woman presents with a 1-yr history of pain in the right upper quadrant exacerbated by eating rich foods. Choose the single most likely investigation from the list of options 581. A. Upper GI endoscopy B. Barium meal C. * Ultrasound scan D. Supine abdominal X-ray E. Oesophageal manometry 582. Antimitochondrial antibody test is characteristic sign of A. * Primary biliary cirrhosis B. Sclerosing cholangitis C. Anaerobic liver abscess D. Hepatoma E. Hemochromatosis 583. At present, gall stones are considered certainly as a cause of: A. Chronic pancreatitis B. * Acute pancreatitis C. Both chronic and acute pancreatitis D. None of above E. Tumour of pancreas 584. Carcinoma of the gallbladder is a result of: A. Hepatic disease B. * Presence of cholelithiasis with chronic chole¬cystitis C. Cholecystography D. Ultrasound examination of the gallbladder E. Constipation 585. Causes of Acute Pancreatitis are all of the following except: A. Alcohol ingestion B. Biliary tract disease (gallstones) C. Postoperative state (after abdominal or nonabdominal operation) D. * Gastritis E. Trauma 586. Causes of Hyperamylasemia and Hyperamylasuria are all of the following except: A. Acute Pancreatitis B. Chronic Pancreatitis C. Pancreatic pseudocyst D. Renal insufficiency E. * Respiratory insufficiency 587. Causes of Hyperamylasemia and Hyperamylasuria are all of the following except: A. Biliary tract disease: cholecystitis, choledocholithiasis B. Perforated or penetrating peptic ulcer C. * Acute leukaemia D. Acute Pancreatitis E. Chronic Pancreatitis 588. Drug of choice in Zollinger Ellison syndrome is A. B-blocker B. Ranitidine C. Antacids D. Atropin E. * 589. A. * Omeprazole For Primary biliary cirrhosis select the circulating antibodies with which it is most closely associated: antibodies to mitochondria B. antibodies to native DNA; C. antibodies to smooth muscle cells; D. antibodies to acetylcholine receptors; E. antibodies to parietal cells. 590. Gall bladder stone formation in caused by all except: A. * Leucocytosis B. Hyperalimentation C. Primary biliary cirrhosis D. Clofibrate therapy E. None of mentioned 591. In acute pancreatitis, the pancreas: A. * is characteristically enlarged B. has scattered calcification C. has ductal decompression D. is replaced E. no changes In which one of the following situations would therapy with oral chenodeoxycholic acid be most effective in dissolving gallstone(s)? 592. A. A 27-year-old Asian woman with thalassemia B. A 49-year-old woman with two 2-cm stones C. A 60-year-old man with gallstones visible on chest x-ray D. * A 45-year-old woman with a history of gallstone pancreatitis and a residual 1-cm radiolucent gallstone A 55-year-old man with a history of biliary colic, several small gallstones seen on ultrasonography, and a poorly opacified gallbladder after oral cholecystography E. 593. Increased amylase may be seen in all of the following except: A. Pancreatic pseudocyst B. Perforated peptic ulcer C. Cancer of the pancreas D. Acute pancreatitis E. * 594. A. * Appendicitis Ingestion of arsenic causes Non cirrhotic portal fibrosis B. Hepatic adenoma C. Hepatic carcinoma D. Hepatic cirrhosis E. Pancreatic carcinoma 595. It is supposed that gall stones can result in chronic pancreatitis because they may induce: A. * Inflammation and stenosis or obstruction of ampulla of Vater B. Fever C. Abdominal pain D. None of above E. Peptic ulcer 596. likely explanation for these findings? A. Bile duct tumor B. Choledocholithiasis C. Congenital polycystic liver D. Primary biliary cirrhosis E. * 597. Primary sclerosing cholangitis Marker of Cholestatic syndrome in hepatitis is A. * Alkaline phosphatase B. All of above C. fibrinogen D. AST E. ALT 598. Markers of Cholestatic syndrome in hepatitis are all of the following except A. * ALT B. cholesterol C. Bilirubin D. Alkaline phosphatase E. GGT 599. Markers of Cholestatic syndrome in hepatitis is A. * All mentioned B. cholesterol C. Bilirubin D. Alkaline phosphatase E. GGT 600. Markers of Cholestatic syndrome in liver diseases are A. * Bilirubin, Alkaline phosphatase, GGT, cholesterol B. AST, ALT, GGT, Bilirubin C. Albumine, prothrombin, cholesterol, fibrinogen D. ESR, globulins, timol test Le, C-react. protein E. None of mentioned 601. Metabolic changes associated with excessive vomitting includes the following: A. Metabolic acidosis B. Hyperchloremia C. Decreases bicarbonates D. Hypercalciemia E. * Hypokalemia 602. Most Common Cause of death in early acute Pancreatitis is A. Renal Failure B. Cardiac failure C. * Respiratory Failure D. Uncontrolled Coagulopathy E. None of above 603. Most common complication of acute pancreatitis is: A. Phlegmon B. Pancreatic abscess C. Pleural effusion D. Appendicitis E. * 604. A. * Pseudocyst Most common site of cholangiocarcinoma is Hepatic duct bifurcation B. Intrahepatic C. Lower End of CBD (Common Bile Duct) D. Lower 1/3rd of CBD (Common Bile Duct) E. None of mentioned 605. Most lesions of pancreas on CT are characterized by all of the following except: A. * the presence of ductal decompression B. enlargement of the pancreatic outline, C. distortion of the pancreatic contoura D. a fluid filling that has a different attenuation coefficient than normal pancreas E. none of the listed 606. Nealon's classification is used for A. Acute pancreatitis B. chronic pancreatitis C. * pseudocyst pancreas D. alcoholic pancreatitis E. None of above 607. Pancreatic calcification may be seen in the following cases except: A. * primary diabetes mellitus B. severe protein-calorie malnutrition, C. hereditary pancreatitis, D. posttraumatic pancreatitis, E. hyperparathyroidism 608. Pancreatic calcification may be seen in the following cases except: A. severe protein-calorie malnutrition B. * primary diabetes mellitus C. hereditary pancreatitis D. posttraumatic pancreatitis E. hyperparathyroidism 609. Pancreatic pseudocyst in adult most often occurs after A. Trauma B. Pancreatic surgery C. Pancreatic malignancy D. Cholecystitis E. * Acute pancreatitis 610. Peptic ulcer should be differentiated with all of the following except A. Cholecystitis B. Gastritis C. Myocardial infarction D. Pancreatitis E. * Pneumonia 611. Peptic ulcer should be differentiated with all of the following except A. Stomach cancer B. Gastritis C. Myocardial infarction D. Pancreatitis E. * Pneumonia 612. Peptic ulcer should be differentiated with all of the following except A. Stomach cancer B. Gastritis C. Gastroesophageal reflux disease D. Pancreatitis E. * Bronchial asthma 613. Peptic ulcer should be differentiated with all of the following except A. Stomach cancer B. Gastritis C. Biliary colic D. Pancreatitis E. * Bronchial asthma 614. Peptic ulcer should be differentiated with all of the following except A. Stomach cancer B. Gastritis C. Referred pain (pleurisy, pericarditis) D. Pancreatitis E. * 615. A. * Bronchial asthma Peptic ulcer should not be differentiated with Ulcerative colitis B. Cholecystitis C. Gastritis D. Miocardial infarction E. Pancreatitis Pruritus, elevation of alkaline phosphatase and positive antimitochondrial antibody test are characteristic signs of 616. A. * Primary biliary cirrhosis B. Sclerosing cholangitis C. Anaerobic liver abscess D. Hepatoma E. Hemochromatosis Pruritus, elevation of alkaline phosphatase and positive antimitochondrial antibody test are characteristic signs of 617. A. * Primary biliary cirrhosis B. Sclerosing cholangitis C. Anaerobic liver abscess D. Hepatitis D E. Hemochromatosis Pruritus, elevation of alkaline phosphatase and positive antimitochondrial antibody test are characteristic signs of 618. A. * Primary biliary cirrhosis B. Sclerosing cholangitis C. Hepatitis C D. Hepatitis D E. Hemochromatosis Pruritus, elevation of alkaline phosphatase and positive antimitochondrial antibody test are characteristic signs of 619. A. * Primary biliary cirrhosis B. Hepatoma C. Hepatitis C D. Hepatitis D E. Hemochromatosis 620. Put preliminary diagnosis. A. * Chronic cholecystitis, acute phase. B. Chronic cholecystitis, subacute phase. C. Chronic cholecystitis, phase of remission. D. Dyskinezia of bile ducts. E. Rotor’s syndrome. 621. Raised serum amylase levels are used to diagnose A. Acute cholecystitis B. Degenerative diseases C. Autoimmune disease D. Appendicitis E. * Acute pancreatitis 622. The complications of chronic pancreatitis are protean A. Cobalamin (vitamin B12) malabsorption B. impaired glucose tolerance C. * vitamin C malabsorption D. vitamin A and/or zinc deficiency E. biliary cirrhosis 623. The differential diagnosis of chronic pancreatitis should include all of the following disorders except: A. * paroxysmal atrium fibrillatium B. perforated peptic ulcer; C. acute cholecystitis and biliary colic; D. acute intestinal obstruction; E. mesenteric vascular occlusion. 624. The differential diagnosis of chronic pancreatitis includes: A. * All of the listed B. myocardial infarction; C. dissecting aortic aneurysm; D. pneumonia; E. peptic ulcer. 625. The differential diagnosis of chronic pancreatitis should include all of the following disorders except: A. * Crohn’s disease B. myocardial infarction C. dissecting aortic aneurysm D. pneumonia E. diabetic ketoacidosis 626. The hallmark of Primary biliary cirrhosis is A. * antibodies to mitochondria B. antibodies to native DNA; C. antibodies to smooth muscle cells; D. antibodies to acetylcholine receptors; E. antibodies to parietal cells. 627. The Marseilles-Rome classification of 1988 includes all of the following except: A. * Chronic autoimmune pancreatitis B. Chronic calcifying pancreatitis C. Chronic obstructive pancreatitis D. Chronic inflammatory pancreatitis E. None of mentioned 628. The preparation for treatment of lamblia of gallbladder: A. Ampicillin B. Rifampicin C. Tetracilin D. Nitroxolin E. * 629. A. * Furasolidon The radiographic hallmark of chronic pancreatitis is: the presence of scattered calcification throughout the pancreas B. enlargement of pancreas C. the presence of ductal decompression D. inflammation of the pancreas E. replacement of the pancreas The Ranson criteria are used to determine prognosis in acute pancreatitis. Factors that adversely affect survival include all of the following except 630. A. * anemia less than 90 g/l B. age greater than 55 years, C. glucose greater than 200 mg/dL, D. LDH greater than 400 IU, E. AST greater than 250 IU/L. The Ranson criteria are used to determine prognosis in acute pancreatitis. Factors that adversely affect survival include all of the following except 631. A. * anemia less than 70 g/l B. age in years > 55 years C. leukocytosis greater than 16,000/µm, D. glucose greater than 200 mg/dL, E. LDH greater than 400 IU, The secretin-cholecystokinin test is useful in the evaluation of patients with suspected chronic pancreatitis. Which statement regarding this test is correct? 632. A. B. * Those with chronic pancreatitis usually have a high bicarbonate output after stimulation Secretion of pancreatic enzymes may be measured In patients with early chronic pancreatitis, enzyme output is relatively more deranged than failure to achieve an adequate bicarbonate concentration C. D. Endocrine hormone output after stimulation is an end-point of the test E. The test can distinguish between chronic pancreatitis and pancreatic carcinoma. 633. The best diagnostic test for Helicobacter pylori is: A. histology B. serology C. * urea breath test D. rapid urease test E. cytology 634. The triad originally described by Zollinger-Ellison syndrome is characterized by: A. Peptic ulceration, gastric hypersecretion, beta cell tumour B. Peptic ulceration, achlorhydria, non beta cell tumour C. Peptic ulceration, achlorhydria, beta cell tumour D. Duodenal ulceration, achlorhydria, beta cell tumour E. * Peptic ulceration, gastric hypersecretion, non beta cell tumour 635. Mechanical obstruction of the colon is most commonly caused by A. volvulus diverticulitis B. adhesions C. carcinoma D. hernia sigmoid E. * All of the above 636. Ultrasonography can provide important information in patients with all of the following except: A. acute pancreatitis B. * perforated duodenal ulcer C. chronic pancreatitis D. pancreatic calcification E. pseudocyst 637. Each of the following represents a correct mechanism of action for the laxative noted EXCEPT A. * sorbitol stimulates colonic motor activity B. psyllium increases stool bulk C. docusate salts lower the surface tension of stool D. cisapride enhances intestinal transit E. castor oil stimulates intestinal secretion Ultrasound examination of the gallbladder is a useful diagnostic examination, the incidence of its false-positive results is: 638. A. * 2% B. 51% C. 96% D. 5-10% E. 10% 639. What change can suggest severe pancreatic exocrine insufficiency? A. Steatorrhea B. marked excretion of fecal fat C. * decreased serum trypsinogen level D. elevated serum amylase E. elevated serum lipase levels 640. What imaging modality may be limited in patient with cholecystitis? A. MRCP. B. CT scan. C. * Ultrasonography. D. Esophogastroduodenoscopy (EGD). E. HIDA scan. 641. What is the best test for acute pancreatitis? A. * Lipase B. Serum amylase activity C. Urine amylase activity D. Plasma Bilirubine E. Alkaline phosphatase activity 642. What is the only major technique that provides a direct view of the pancreatic duct? A. Sonography B. CT C. Plain rradiography D. * Endoscopic retrograde cholangiopancreatography E. Laparoscopy 643. What patients with gall stones tend to induce pancreatitis? A. * B. Those patients who have common pancreatico-biliary channels in the ampullary of Vater Those patients who do not have common pancreatico-biliary channels C. Anyone who has gall stones D. None of the listed E. All of the listed 644. All the following can inhibit the secretion of gastric acid EXCEPT A. * Histamine B. Reduction of the intragastric pH below 3.0 C. Somatostatin D. Cecretin E. Presence of fat in the duodenum 645. Which answer below represents an osmotic laxative? A. * Lactulose. B. Psyllium. C. Magnesium citrate. D. Castor oil. E. Lubiprostrone. 646. The most informative indexes of secret function of the stomach is the quantity of: A. * Chloride acid B. Slime; mucus, mucilage, phlegm C. Gastric liquid D. Pepsin E. Hormones 647. Which drug is not prescribed in case of chronic cholecystitis, acute phase: A. * Pangrol B. Analgin C. No-shpa D. Amoxicillin E. Platyphyllin 648. Which drug is not prescribed in case of chronic pancreatitis: A. * Dicloberl B. Creon C. Pangrol D. Lansoprazol E. Panzinorm Under perforative gastric and/or duodenal ulcer the stomach ache usually would be described by the patient as it originates: 649. A. * Suddenly B. From time to time C. Little by little D. Attacking E. In different ways 650. Which drug is not prescribed in case of dyskinesia of bile ducts, hypertonic type: A. * Chophitol B. Platyphyllin C. No-shpa D. Duspatalin E. Meteospasmil 651. Under perforative gastric and/or duodenal ulcer the vomit usually would be described by the patient as: A. * The threat of vomiting only B. Gastric contents C. “Excrement odor” D. Blood E. Bile 652. Which drug is not prescribed in case of dyskinesia of bile ducts, hypotonic type: A. Chophitol B. Cerucal C. Motilium D. Domperidon E. * Meteospasmil 653. Which drug is not prescribed in case of dyskinesia of bile ducts: A. Chophitol B. Hepabene C. Motilium D. Domperidon E. * 654. A. * Aspirin Which drug is not prescribed in case of exocrine insufficiency of pancreas: Prednisolon B. Creon C. Pangrol D. Festal E. Panzinorm 655. Which drug is not prescribed in case of steatorrhea: A. * Corticosteroids B. Creon C. Pangrol D. Festal E. Panzinorm 656. Which drug is prescribed in case of chronic cholecystitis, acute phase: A. Pangrol B. Creon C. * No-shpa D. Festal E. Panzinorm 657. Which drug should be administrated if steatorrhea is present: A. Corticosteroids B. Vitamins A, K, D C. Azatioprine D. Riboxin E. * 658. Panzinorm The patient with the gastric and/or duodenal ulcer under fibergastroduodenal checkup would usually show: A. * Mucus defect B. Intensified peristaltic C. Extra secretion of gastric liquid D. Deadlock of gastric contents E. No substantial changes 659. Which drug should be administrated in case of dyskinesia of bile ducts, hypertonic type: A. * No-shpa B. Vitamins A, K, D C. Chophitol D. Cerucal E. Pangrol 660. Which drug should be administrated in case of dyskinesia of bile ducts, hypotonic type: A. No-shpa B. Vitamins A, K, D C. * Chophitol D. Duspatalin E. Pangrol 661. Factors stimulating gastrin secretion include: A. * gastric wall distension B. acid in the lumen of the stomach C. glucagon D. calcium E. secretin 662. Which drug should be administrated in case of endocrine insufficiency of pancreas: A. Aspirin B. Vitamins A, K, D C. Azatioprine D. * Insulin E. Pangrol 663. Which of the following foods should be avoided in celiac disease (gluten sensitive enteropathy) ? A. * all of the above B. rye cereals C. beer D. bread E. none of the listed 664. Which drug should be administrated in case of exocrine insufficiency of pancreas: A. Aspirin B. Vitamins A, K, D C. Azatioprine D. Insulin E. * Pangrol 665. Which of the following states predispose an affected person to colon carcinoma? A. * ulcerative colitis B. chronic giardiasis C. Crohn's disease D. Hirschsprung's disease E. all of the above 666. Which entity is most difficult to diagnose using MR cholangiopancreatography (MRCP)? A. Congenital anomaly B. Traumatic duct injury C. Adenocarcinoma D. * Acute pancreatitis E. Intraductal papillary mucinous neoplasm (IPMN ) 667. Which feature of pancreatic pseudocyst on CT suggests secondary infection? A. * Gas formation in the cyst. B. Calcification of the cyst wall. C. Heterogeneous attenuation of cyst contents. D. Enhancement of the cyst wall after IV contrast injection. E. Extrapancreatic extension. Which imaging technique or procedure is most specific for differentiating a mucinous cystic tumor from a microcystic adenoma? 668. A. B. * Endoscopic retrograde cholangiopancreatography (ERCP). Percutaneous cyst aspiration C. MR cholangiopancreatography D. CT E. Endoscopic sonography 669. Which is the most common cause of chronic pancreatitis? A. * Alcohol B. Autoimmune diseases C. Gall stones D. None of mentioned E. Tumor of stomach 670. Which is the most common functioning islet cell tumor? A. Glucagonoma B. Gastrinoma C. VIPoma D. Somatostatinoma E. * Insulinoma Which of the following could falsely depress the serum amylase level in a patient suspected of having acute pancreatitis? 671. A. * Hypertriglyceridemia B. Hypercholesterolemia C. Hypocalcemia D. Associated pleural effusion E. Associated intestinal infarction 672. Symptoms of acute diverticulitis include: A. * all of the above B. none of the listed C. alternating constipation and diarrhea D. severe rectal hemorrhage E. subacute intestinal obstruction Which of the following could falsely depress the serum amylase level in a patient suspected of having acute pancreatitis? 673. A. * Hypertriglyceridemia B. Hypercholesterolemia C. Hypocalcemia D. Associated pleural effusion E. None of mentioned The patient is found to have a duodenal ulcer by upper endoscopy. The likelihood of this patient having H. pylori in the gastric antrum is 674. A. * 70 % B. 5% C. 10% D. 30 to 60% E. 100% 675. Which of the following is not true for ectopic pancreas A. stomach and duodenum are the most common site B. Ectopic pancreas appears as a submucosal irregular nodule in the wall C. * D. Islet tissue is present in all the organs where ectopic pancreas is present Ulceration, bleeding and obstruction are the most common symptoms E. None of above 676. Which of the following is not true regarding blood supply of pancreas? A. * Posterio superior pancreatico-duodenal artery is a branch of Superior mesenteric artery. B. Body and tail of pancreas is supplied by Splenic artery C. It receives blood supply from coeliac trunk and superior mesenteric artery. D. All major pancreatic arteries lie posterior to pancreatic ducts. E. None of the listed 677. The best way to eradicate H. pylori in this patient is A. * Omeprazole 20 mg BID, amoxicillin 1000 mg BID, clarithromycin 500 mg BID for 14 days B. Omeprazole 20 mg PO daily for 6 weeks C. Ranitidine 300 mg PO qhs for 6 weeks D. Pepto-Bismol and metronidazole BID for 7 days E. Sulcrafate 200 mg QID for 6 weeks 678. Which of the following patients is most likely to benefit from cholecystectomy at this time? An asymptomatic 62-year-old man with gallbladder calcification seen on plain radiographs of the abdomen A. * B. An asymptomatic 34-year-old woman who has gallbladder sludge seen on abdominal ultrasonography An asymptomatic 53-year-old woman with multiple 7-to 10-mm gallstones seen on abdominal ultrasonography C. A 35-year-old woman with right upper quadrant abdominal pain who has normal gallbladder on abdominal ultrasonography D. An asymptomatic 47-year-old man with diabetes mellitus who has a single gallstone seen on abdominal ultrasonography E. 679. Which one of the following laboratory findings is most likely to result from prolonged vomiting? A. * metabolic acidosis with hyponatremia B. metabolic acidosis with hypernatremia C. metabolic alkalosis with hyperkalemia D. metabolic alkalosis with hypokalemia E. respiratory acidosis with hyponatremia 680. Which of the following patients is most likely to benefit from cholecystectomy at this time? An asymptomatic 67-year-old man with gallbladder calcification (eggshell appearance) seen on plain radiographs of the abdomen A. * An asymptomatic 37-year-old woman who is beginning a weight loss program and has gallbladder sludge seen on abdominal ultrasonography B. An asymptomatic 57-year-old woman with multiple 7-to 10-mm gallstones seen on abdominal ultrasonography C. A 35-year-old woman with right upper quadrant abdominal pain who has normal liver chemistry studies and a normal gallbladder on abdominal ultrasonography D. An asymptomatic 47-year-old man with diabetes mellitus who has a single gallstone seen on abdominal ultrasonography E. 681. Which of the following patients is most likely to benefit from cholecystectomy at this time? An asymptomatic 68-year-old man with gallbladder calcification (eggshell appearance) seen on plain radiographs of the abdomen A. * An asymptomatic 38-year-old woman who is beginning a weight loss program and has gallbladder sludge seen on abdominal ultrasonography B. An asymptomatic 59-year-old woman with multiple 7-to 10-mm gallstones seen on abdominal ultrasonography C. A 35-year-old woman with right upper quadrant abdominal pain who has normal liver chemistry studies and a normal gallbladder on abdominal ultrasonography D. An asymptomatic 45-year-old man with diabetes mellitus who has a single gallstone seen on abdominal ultrasonography E. 682. Which of the following statements concerning gastrinoma is correct? A. Most are benign B. Most are unifocal C. They are associated with multiple endocrine neoplasia (MEN) syndrome type II. D. * They usually secrete multiple hormones E. The secretin injection test reveals a reduction in gastrin levels. 683. Which of the listed organs breaks down or modifies toxic substances? A. * Liver B. Gall bladder C. Pancreas D. Spleen E. Duodenum 684. Which of the listed organs excretes digestive substances but does not produce them? A. * Gall bladder B. Pancreas C. Liver D. Spleen E. Duodenum 685. Which of the listed organs functions as endocrine gland? A. * Pancreas B. Gall bladder C. Liver D. Spleen E. Duodenum 686. Omeprazole is useful for the medical treatment of peptic ulcers because it is A. * an inhibitor of the H_/K_ ATPase pump B. a cholinergic antagonist C. an H2-receptor antagonist D. a weak base that partially neutralizes gastric acid E. an inhibitor of cyclooxygenase 687. Which organ also functions as an endocrine gland A. * Pancreas B. Gall bladder C. Liver D. Spleen E. Duodenum 688. Which one of the following is formed within the enterocytes of the small intestines? A. * high-density lipoproteins (HDLs) B. chylomicrons C. intermediate-density lipoproteins (IDLs) D. low-density lipoproteins (LDLs) E. very low-density lipoproteins (VLDLs) 689. Which organ excretes a buffer that neutralizes acid from the stomach? A. * Pancreas B. Gall bladder C. Liver D. Spleen E. Duodenum 690. Which organ functions in detoxification of the blood A. Pancreas B. Gall bladder C. * Liver D. Spleen E. Duodenum 691. Which one of the following structures is retroperitoneal? A. * Cecum B. ascending colon C. appendix D. sigmoid colon E. transverse colon 692. Which organ produces bile salts? A. * Liver B. Gall bladder C. Pancreas D. Spleen E. Duodenum 693. Which organ releases a buffer that neutralizes acid from the stomach A. * B. Pancreas Gall bladder C. Liver D. Spleen E. Duodenum 694. Which organ releases digestive substances but does not produce them A. Pancreas B. * Gall bladder C. Liver D. Spleen E. Duodenum 695. Which organ releases the digestive hormone secretin A. Pancreas B. Gall bladder C. Liver D. Spleen E. * Duodenum 696. Zollinger-Ellison syndrome is characterized by all of the following except A. increased levels of the hormone gastrin B. non-beta cell islet tumour of pancreas C. severe peptic ulceration D. gastric acid hypersecretion E. * Serum amylase is increased 697. In alcohol-related liver disease: A. * decreased tolerance to alcohol indicates progression of disease B. chronic disease is usually associated with tender palpable hepatomegaly C. patients are unlikely to be smokers D. thiamine has not been proven to prevent memory problems E. benzodiazepines are contraindicated during alcohol detoxification 698. Coeliac disease: A. * is associated with an increased risk of GI lymphoma B. is the most common cause of mal-absorption in developing countries C. patients benefit from a diet high in complex carbohydrates such as bread and pasta D. is usually diagnosed on CT abdomen E. patients are at lower risk of osteoporosis than the non-coeliac population 699. Colorectal carcinoma: A. * most commonly metastasizes to the liver B. is classified by Breslow's criteria C. is most common in those with a high fibre diet D. is more common in females than in males E. patients with disease confined to the bowel mucosa have a 40% 5 year survival rate 700. Gastric cancer: A. * when shown to be an adenocarcinoma on histology, is associated with Helicobacter pylori B. is usually a squamous cell carcinoma C. usually has a good prognosis D. most commonly presents with haematemesis E. is usually diagnosed on barium swallow A patient with newly diagnosed tropical sprue could have all the following extragastrointestinal manifestations of malabsorption EXCEPT 701. A. * pyoderma gangrenosum B. megaloblastic anemia C. night blindness D. purpura E. tetany 702. What diseases can lead to heart failure? A. Arterial hypertension B. Valvular heart disease C. Myocardial infarction D. Cardiomyopathies E. * All from above 703. What are percussion findings at the patients with RVF? A. The left border of relative heart dullness drifts left B. The right border of relative heart dullness drifts right C. The right border of relative heart dullness drifts left D. Nothing from above E. * Depend on clinical situation 704. What are the lung auscultation findings at the patients with heart failure? A. Vesicular breathing, basal rales B. Diminished vesicular breathing C. * Diminished vesicular breathing and crepitation D. Vesicular breathing and pleural friction rub E. Nothing from above 705. Acute coronary syndromes includes unstable angina and: A. Stable angina. B. * Myocardial infarction. C. Myocarditis. D. Pericarditis. E. Hypertension attack. 706. What risk factors of development of Coronary artery disease: A. High serum cholesterol and triglyceride levels. B. Sedentary lifestyle. C. Stress. D. Diabetes mellitus. E. * All of enumeration. 707. Angina pectoris may be: A. Delicate. B. Dangerous. C. Strong. D. * Unstable. E. Acute. 708. 5. What electrocardiography changes may show ischemia: A. * Change T waves. B. Change P. C. Change Q. D. Change R. E. Change S. 709. What usual cause of Coronary artery disease: A. * Atherosclerosis. B. Hepatitis. C. Tonsillitis. D. Low serum cholesterol and triglyceride levels. E. Ulcer of stomach. 710. Which diseases can be accompanied with arterial hypertension? A. Renal diseases B. Endocrine disease C. Coarctation of aorta. D. Nephropathy of pregnancy E. * all mentioned above 711. Which organs are considered target at the patients with arterial hypertension? A. Heart, liver, lungs and brain B. Liver, brain, kidney, eyes C. * Heart, brain, kidney, eyes, vessels D. Heart, liver, lungs and kidney E. Liver, brain, kidney, eyes, heart. 712. What is the commonest symptom at patients with essential hypertension? A. Sleep disorders. B. * Headache. C. Myalgia. D. Arrhythmia. E. Edemas 713. What kind of cyanosis is usually observed at patient with cardiovascular diseases? A. Central, warm B. * Peripheral, cold C. Peripheral warm D. Local (near heart region), cold E. Diffuse warm 714. What kind of posture is observed at acute left ventricular failure? A. Upright B. On the right side with high head of the bed C. * Orthopnoea D. Sitting posture bending forward E. Knee-elbow posture 715. Which of the following disorders is not likely to be associated with hemoptysis? A. Mitral stenosis B. Pulmonary embolism C. Pulmonary edema D. * Pericarditis E. None of the above 716. Bronchial asthma is a… A. Acute inflammatory disease; B. Acute infective disease; C. Chonic infective disease; D. * Chonic iinflammatory disease; E. northing from above. 717. Chronic obstructive pulmonary disease is a… A. chronic inflammatory of trachea and large bronchus B. chronic inflammatory of large and medium bronchus C. * chronic inflammatory of medium, small bronchus with involving lung parenchyma and vessels D. All from above E. Northing from above 718. Which symptoms characterize bronchial asthma? A. Mixed dyspnea, cough with purulent sputum B. * Episodic dry cough, tightness of the chest, wheezing C. Chest pain with radiation to jaw, inspiratory dyspnea D. Permanent expiratory dyspnea, cough E. Episodic hemoptysis and dyspnea due to physical effort 719. How is elasticity of the chest changed at the patient with respiratory failure? A. increasing B. decreasing C. not changed D. absence E. * depend on clinical situation 720. How percussion sound is changed at the patient with bronchial obstruction? A. * Unchanged B. dull C. small box sound D. tympanic E. depend on clinical situation 721. How percussion sound is changed at the patient with emphysema? A. unchanged B. dull C. * small box sound D. tympanic E. depend on clinical situation 722. How percussion sound is changed at the patient with respiratory failure? A. unchanged B. dull C. small box sound D. tympanic E. * depend on clinical situation 723. What is the main symptom of the respiratory failure? A. cough; B. * dyspnea; C. palpitation; D. wheezing; E. chest pain. 724. What is the main symptom of the emphysema? A. cough; B. expiratory dyspnea; C. inspiratory dyspnea; D. wheezing; E. * mixed dyspnea. 725. How is elasticity of the chest changed at the patient with emphysema? A. increasing B. * decreasing C. not changed D. absence E. depend on clinical situation 726. What symptoms characterize the bronchial obstruction syndrome? A. * Wheezing, dry cough, tightness in the chest B. Cough with sputum, chest pain, fever C. Mixed dyspnea, hemoptysis, weakness D. Dyspnea, chest pain, palpitation E. Dry cough, chest pain, edema 727. What symptoms don’t characterize the bronchial obstruction syndrome? A. Wheezing B. cough C. tightness in the chest D. dyspnea E. * purulent sputum 728. What change of vocal fremitus can be at the patient with bronchial obstruction? A. Amplifying B. Decreasing C. Absence D. Not changed E. * Change depends on clinical situation 729. What change of vocal fremitus can be at the patient with emphysema? A. Amplifying B. * Decreasing C. Absence D. Not changed E. Change depends on clinical situation 730. What change of vocal fremitus can be at the patient with respiratory failure? A. Amplifying B. Decreasing C. Absence D. Not changed E. * Change depends on clinical situation 731. Auscultation signs of massive exudative pleurisy: A. Diminished vesicular breathing and crackles B. * absent of breath sounds C. unchanged breath sound D. Pathological bronchial breathing E. Diminished vesicular breathing and wheeze 732. Which investigation is obligatory for confirming pneumonia? A. Sputum culture B. Full blood analysis C. * X-ray examination D. Bronchoscopy E. Lung function test 733. Which properties does not transudate have? A. Light yellow color B. * Protein = 40 g/l C. Negative Rivalt test D. 1-5 leucocytes and 2-6 mezoteliocytes E. All mentioned above 734. Which properties does exudate have? A. Comparative density > 1,018 B. Protein > 30 g/l C. Positive Rivalt test D. 10-25 leucocytes and 2-6 mezoteliocytes E. * All from above 735. Which investigation is the most informative for confirming lung cancer? A. Sputum culture B. Full blood analysis C. X-ray examination D. * Bronchoscopy with biopsy E. Computered tomography 736. Which syndrome can develop at the patient with central lung cancer? A. emphisema; B. pneumotorax; C. * obstructive atelectasis; D. lobar consolidation; E. northing from above. 737. 15. Which syndrome can develop at the patient with peripheral lung cancer? A. emphisema; B. pneumotorax; C. obstructive atelectasis; D. * lobar consolidation; E. northing from above. 738. Which of the following characteristics is not typical for pleuritic chest pain? A. Increases with deep breathing B. * Radiates to the jaw C. Is located laterally D. Diminishes with splinting of the affected side E. Increases with cough 739. Which of the following may cause an increase in vocal resonance? A. Emphysema B. asthma C. * pneumonia D. atelectasis E. dry pleurisy 740. Percussion sound over massive pleural effusion: A. tympanic B. clear C. resonance D. * dull E. small dull 741. Percussion sound over pneumothorax: A. * Tympanic B. clear C. small box-sound D. dull E. small dull 742. Which method of sputum examination may help to establish lung cancer? A. General macroscopic B. * Cytological C. General microscopic D. Cultural E. Northing from above 743. Which radiologic method of lung examination is routinely used? A. Computed tomography B. Magnetic resonance imaging C. Bronchography D. * X-ray E. Nothing from above Which radiologic method of lung examination has the highest level of resolution for distinguishing the smallest lung structures? 744. A. * Computed tomography B. Magnetic resonance imaging C. Bronchography D. X-ray E. Nothing from above 745. Appearance of the pleural friction rub at the patient with exudative pleurisy is sing of … A. Increasing exudate B. Obturative atelectasis in the lung collapse region C. * Decreasing exudates D. Pneumothorax E. All answers are right depending on clinical situation 746. The sonorous coarse bubbling rales can be heard at the patient with… A. Emphysema B. * Chronic abscess C. Pleural effusion D. Lobar pneumonia E. Compressive atelectasis 747. The sonorous medium bubbling rales can be heard at the patient with…? A. Emphysema B. * Bronchiectasis C. Acute bronchitis D. Pleural effusion E. Obturative atelectasis 748. When can not the weakened vesicular breath sound be heard? A. Emphysema B. Focal pneumonia C. Dry pleurisy D. * Large cavity in the lung E. Pneumosclerosis 749. When can the amphoric breath sound be heard? A. Emphysema B. lobar pneumonia C. Dry pleurisy D. * Large cavity in the lung E. Pneumosclerosis 750. What auscultation phenomenon is heard of the large pleural effusion? A. * Absent of the breath sound B. Vesicular breath sound with prorogated exhalation C. Rough vesicular breath sound D. Bronchial breath sound E. Weakened vesicular breath sound 751. What auscultation phenomenon is heard of the bronchial asthma? A. Absent of the breath sound B. * Vesicular breath sound with prorogated exhalation C. Rough vesicular breath sound D. Bronchial breath sound E. Weakened vesicular breath sound 752. What breath sound is heard of the focal pneumonia near root of lung? A. * Normal vesicular breath sound B. Vesicular breath sound with prorogated exhalation C. Rough vesicular breath sound D. Bronchial breath sound E. Weakened vesicular breath sound 753. How vesicular breath sound is changed in case of pneumotorax? A. Not change B. * Became weakened C. Became pathological bronchial D. Became amphoric E. Became rough 754. How vesicular breath sound changed is in case of acute bronchitis? A. Not change B. Became weakened C. Became pathological bronchial D. Became amphoric E. * Became rough 755. How vesicular breath sound is changed in case of the 2nd stage of the lobar pneumonia? A. Not change B. Became weakened C. * Became pathological bronchial D. Became amphoric E. Became rough 756. When may you hear hyper-resonant percussion sounds over the lung? A. Emphysema, B. * Pneumothorax, C. Above the level of pleural effusion D. Large cavity E. Everything mentioned above. 757. What pathological condition can produce dull percussion sound? A. * Pneumonia B. Emphysema C. Large cavity D. Bronchitis E. Pneumothorax. 758. What percussion sound is heard of the lobular pneumonia? A. Tympanic B. Impaired C. * Dull D. Clear lung E. Resonant. 759. What type of percussion sounds may you hear over health lung? A. Tympanic B. * Clear lung C. Dull D. Stony dull E. Resonant. 760. When may you hear dull percussion sound over lung? A. Thickened pleura. B. Collapse of lung. C. Consolidation of lung. D. Fluid in pleural cavity. E. * Everything mentioned above 761. What kind of posture is observed at the bronchial obstruction? A. Upright B. * Sitting position fixing the shoulder girdle C. Orthopnoea D. Sitting posture bending forward E. Knee-elbow posture 762. If patient skin has diffuse bluish tint, it is named: A. * Diffuse cyanosis B. Diffuse erythema C. Acrocyanosis D. Pathological pallid skin E. Northing mentioned above. 763. What mechanisms are caused by the cyanosis? A. Secondary pulmonary hypertension B. Restricted pulmonary circulation C. Artery-venous blood shunting D. Primary pulmonary hypertension E. * Everything mentioned above 764. The most widely spread theories of gastric and duodenal ulcer origination are: A. * Infectious B. Mechanic C. Peptic D. Endocrine E. Genetic origination Cell present in large numbers in the peritont fluid of Tuberculous peritonitis are765. A. Eosinophils B. Polymorphs C. * Lymphocytes D. Monocytes E. Neutrophils 766. Treatment of drug induced gastritis – A. Mesoprostol B. * H,receptorblock C. Antacids D. Famotidine E. Ranitidine 767. Which of the following cations is presents gastric juice in a larger concentration than in blood plasma- A. Na+ B. * K+ C. Mg+ D. Ca+ E. Lithium 768. Progressive dysphagia is seen in- A. * Carcinoma esophagus B. Globus hystericus C. Presbyesophagus D. Achalasia E. Gastric carcinoma 769. Carcinoma stomach is associated with blood group – A. * A B. B C. AB D. 0 E. None 770. Stress ulcers seen in burns are – A. * Curling's ulcer B. Cushing's ulcer C. Meleney's ulcer D. Rodent ulcer E. Intestinal ulcer 771. Most common cause of decrease in incidence of H.pylori in west is d/t - A. * Change in the style B. Increased use of PP1 C. Chemotherapy D. Mutation in organism E. Bad food In the Forrest classification for bleeding peptic ulcer with a visible vessel or pigmented protuberance is classified as – 772. A. * FI B. F Ila C. F lib D. F lie E. F2c 773. Treatment of H. pylori is required in all of the following expect? A. * Gastro esophageal reflex disease B. Gastric ulcers C. Duodenal ulcers D. Gastric lymphoma E. Tumor of pancreas 774. True regarding GERD is all except - A. Avoid coffee & Tea B. Transient lower esophageal relaxation C. * Lower esophageal sphincter length and its pressure is important D. Proton pump inhibitor is the treatment of choice E. Avoid meet and sugar Eradication of helicobacter pylori has been proved to be beneficial in which of the following disorders of the stomach 775. A. * Low grade malt lymphoma B. Prosive gastritis C. Carcinoma stomach D. Gastroesophageal disease E. Thyroid carcinoma 776. .H. Pylori is known to cause all of the following except- A. Gastric ulcer B. Duodenal ulcer C. Gastric lymphoma D. * Fundal gastritis E. Tumor of large intestine 777. True about mucosa associated lymphoma - A. * H. Pylori predisposes B. Chemotherapy sensitive C. Multiple lymphomas D. Stromal polyp E. Diffuse poliposis of large intestine 778. All are true regarding Helicobacter pylori except - A. * Less prevalent in developing countries B. Toxigenic strains usually causes ulcers C. Urea breath is positive D. Gram negative organism E. Gram positive organism 779. Diagnostic tests for H. Pylori include all of the following except- A. Urea-breath test B. Rapid urease test C. Gastric biopsy & Warthin-starry stain D. * SAFA test E. pHmetry 780. Epidemiological studies of H. Pylori are done by using A. Urea-breath test B. * Serological markers C. Culture D. Gastric-biopsy urease test E. SAFA test A patient with H. pylori infection is treated with drugs. The best method to detect presence of residual H. pylori infection in this person is 781. A. Rapid urease test B. * Urea breath test C. Endoscopy and biopsy D. Serum anti H. pylori titre E. Serological markers 782. Which drug is not effective against H.pylori – A. Colloidal Bismuth B. Metronidazole C. Amoxicillin D. * Erythromycin E. Clotrimazoli 783. All are used in treatment of Helicobactor pylori, EXCEPT- A. Colloid bismuth B. * Cisapride C. Clarithromycin D. Metronidazole E. Amoxicillin 784. All of the following drugs are commonly used in regimens against H. pylori except – A. * Oxytetracycline B. Amoxicillin C. Bismuth subcitrate D. Omeprazole E. Tetracyclini 785. All of the following are true regarding a patient with acid peptic disease except - A. Misoprostol is the drug of choice in patients on NSA1DS B. * DU is preventable by the use of single night time H, blockers C. Omeprazole may help ulcers refractory to H2 blockers D. Mesoprostol is DOC in pregnant patients E. All above 786. Stress ulcers seen in burns are – A. * Curling' ulcer B. Cushing's ulcer C. Meleney's ulcer D. Rodent ulcer E. Intestinal ulcer 787. Early gastric cancer generally indicates - A. Gastric adencarcinoma detected early B. Gastric adenocarcinoma confined to the mucosa C. * Gastric adenocarcinoma confined to the mucosa & submucosa D. Gastric adenocarcinoma less than 1 cm. In size E. Gastric adenocarcinoma less than 2 cm in size 788. Treatment of Heliobactor pylori are except – A. Clarithromycin B. * Cisapride C. Bismuth subsalicylate D. Metronidazole E. Tetracyclini 789. Histopathological findings in Whipple's disease include all of the following except - A. Marked increase in the number of macrophages in the mucosa. B. * Marked increased in the number of intraepethelial lymphocytes C. Dilatation of lymphatics in the mucosa D. Lipid deposition in the mucosa E. Protein deposition in the mucosa 790. Does not affect prognosis in acute pancreatitis - A. Leucocytosis> 19000 B. * Amylase > 8000IU C. Albumin < 3.2 gm/dl D. Age > 60 yrs. E. Age <70 yrs. 791. Best diagnosis of pancreatic cancer (head) is by – A. Ultrasound B. * ERCP C. CAT scan D. PTC E. Angiography 792. Ectopic ACTH syndrome is seen most common 1> with- A. Renal cell carcinoma B. Lymphoma C. * Bronchogenic carcinoma D. Pituitary adenoma E. Acute pancreatitis 793. Carcinoma pancrease attains largest size when it is sited in- A. Head B. Ampulla C. * Body & tail D. Periampullary E. Tail 794. Increased C-peptide is seen in – A. Glucagoma B. * Insulinoma C. Gastrinoma D. Hepatoma E. Carcinoma 795. Investigation of choice for pancreatic islet cell tumour is - A. CT scan B. MRI C. * Nuclear scan D. USG E. Capilaroscopy 796. Serum amylase level is raised in all except - A. Acute pancreatitis B. Perforation of stomach C. Strangulated small intestine D. * Acute appendicitis E. Acute fase of myocardial infarction 797. Pentagastrin-fast achlorhydria in patient with gastric ulcer indicates - A. Antral ulcer B. * Malignant ulcer C. Zollinger - Ellison syndrome D. Gastric lymphoma E. Intestinal ulcer 798. Surum smylase usually becomes elevated in acute pancreatitis after. A. 1/-2 hrs. B. 4-6 hrs. C. * 24-48 hrs. D. 48-72 hrs. E. 72-96 hrs. 799. Zollinger Ellison syndrome is cused by – A. * Non Beta cells B. Beta cells C. Alpha cells D. Non Alpha E. Non Beta 1 cells 800. The medical treatment of Zollinger Ellison's syndormeis- A. Cimetidine B. Ranitidine C. Famotidine D. * Omeprazole E. Pansoprasole hrs 801. Best progonosis in acute pancreatitis is seen with pancreatitis - A. * Gall stones B. Viral C. Post operative D. Alcoholic E. With dyscynesia 802. Diarrhoea in Zollinger Ellison syndrome is due to- A. Pantagastrin B. Secretin C. * Gastrin D. Enterokinin E. Holecystokinin 803. Carcinoma of pancreas attains greatest size when it is located in - A. Head B. * Body and tail C. Ampullary region D. Ampula of vater E. Head and body 804. .Which one of the following types of pancreatitis has the best prognosis - A. * Gall stone pancreatitis B. Alcoholic pancreatitis C. Idiopathic pancreatitis D. Traumatic pancreatitis E. Edeamatic pancreatitis 805. Raised serum amylase is not seen in - A. * Appendicitis B. Pancreatitis C. Blocked salivary duct D. ectopic pregnancy ruptured E. Hepatitis Which one of the following is best avoided in the treatment of acute pancreatitis 806. A. Antibiotics B. Nasogastric suction C. * Anti cholinergics D. Morphine E. Infusional therapy 807. The following can be associated with acute pancreatitis EXCEPT- A. Hyperparathyroidism B. * Hyperthyroidism C. Hypercalcemia D. Hypertriglceridemia E. Hypocalcemia The most common hormone other than gastrin, contained in the gastric - secreting islet cell tumour is 808. A. * ACTH B. Glucagon C. Melanocyte stimulating hormone D. Growth hormone releasing factor E. Insulin 809. Most common tumor of pancreas is- A. * Insulinoma B. Gastrinoma C. APUD'somas D. VIPoma E. Carcinoma 810. Complications of chronic pancreatitis include the following except A. Portal hypertension B. Obstructive jaundice C. Duodenal obstruction D. * Renal artery aneurysm E. Renal hypertension 811. Most important screening test for acute pancreatitis is- A. * Serum amylase B. Serum lipase C. CT(Abdomen) D. ERCP E. Elastase 812. Carcinoma pancrease attains largest size when it is sited in A. Head B. Ampulla C. * Body & tail D. Periampullary E. Whole gland 813. All are complications of ulcerative colitis exceptA. Haemorrhage B. Stricture C. Malignant change D. Polyposis E. * Oesophageal varices 814. Post diarrhoeal paralytic ileus occurs in – A. Hypokalemia B. * Hypomagnesemia C. Hypocalcemia D. All of the above E. None 815. Paralytic ileus is a feature of all except- A. Retroperitoneal hematoma B. Hypokalemia C. * Diabetes D. Porphyria E. Hypertension Characteristic features of ischaemic colitis at the onset of an attack include 816. A. Steatorrhoea B. Normal barium enema C. Necessity of emergency surgery D. Signs of generalized peritonitis E. * None 817. Fatal gastroenteritis is caused by A. * Typhoid B. Amoebiasis C. Anthrax D. Giardiasis E. Stafylococcus 818. The normal fecal fat excretion is – A. * Less than 5 gm/day B. 8 gm/day C. 10 gm/day D. 15 gm/day E. 20 gm/day 819. Coeliac disease is associated with HLA.... - A. A-3 B. DR-3 C. DE-8 D. DR-4 E. * None Which is not true of arthritis associated with inflammatory bowel disease 820. A. Migratory arthritis B. Knee joint most common C. * Deformities are common D. Correlates to severity of colitis E. Rheumatoid arthritis 821. Earliest pathological change is X-ray in Ulcerative Colitis- A. Loss of haustration B. Aphthous ulcerations C. * Mucosal granularity D. Skip tensions E. There no changes 822. Celiac sprue causes malabsorption syndrome due to- A. Coliform infection of small bowel B. Lactase deficiency C. * Hypersensitivity to dietary gluten D. Ischaemia of celiac artery E. Amilase defficiency 823. The schilling test is performed to determine the cause of- A. Lactose malabsorption B. Fatty acid malabsorption C. Amino acid malabsorption D. * Cobalamin malabsorption E. Gluten malabsorption 824. All are features of irritable bowel syndrome EXCEPT- A. * Vomiting B. pain abdomen C. Diarrhoea D. Constipation E. Nausea 825. Antigliadin antibodies are delectable in - A. Tropical sprue B. Whipple's disease C. * Celiac disease D. Intestinal lymphoma E. Lactase malabsorption 826. Best test for Small intestine malabsorption of carbohydrates is – A. Lund meal test B. Shilling test C. * D-Xylose test D. Follacin test E. pH metry 827. What usual cause of Coronary artery disease: A. * Atherosclerosis. B. Hepatitis. C. Tonsillitis. D. Low serum cholesterol and triglyceride levels. E. Ulcer of stomach. 828. What risk factors of development of Coronary artery disease: A. Hypertension. B. Smoking. C. Family history. D. Obesity. E. * All of them. 829. Angina pectoris may be: A. * Stable. B. Dangerous. C. Strong. D. Delicate. E. Acute. 830. Pain can be relieved by nitroglycerine during: A. 1 min. B. * 1-5 min. C. 15-20 min. D. 20-30 min. E. 30-50 min. 831. What electrocardiography changes may show ischemia: A. * Change T waves. B. Change P. C. Change Q. D. Change R. E. Change S. 832. Duration of pain at a myocardial infarction: A. 1-3 min. B. 10-20 min. C. * More then 30 min. D. Some days. E. During week. 833. Where are changes defined at a inferior infarction: A. І, ІІ, AVL. B. * ІІ, ІІІ, AVF. C. V1, V2. D. V4. E. V5, V6. 834. Duration І – acutest stage is: A. * Some first hours – 1 day. B. 2 day till 2 weeks. C. Till 2-3 months. D. Till 6 month. E. 30-60 min. 835. When is leucocytosis being increased at a myocardial infarction І – acutest stage? A. * Till 1-2 day. B. Till 12-24 hours. C. Till 2-3 day. D. Till 5-th day. E. Till 7-th day. 836. Duration ІІІ – subacute stage: A. Some first hours – 1 day. B. 2 day till 2 weeks. C. * Till 2-3 months. D. Till 6 month. E. 30-60 min. 837. What risk factors of development of Coronary artery disease: A. High serum cholesterol and triglyceride levels. B. Sedentary lifestyle. C. Stress. D. Diabetes mellitus. E. * All of enumeration. 838. Angina pectoris may be: A. Delicate. B. Dangerous. C. Strong. D. * Unstable. E. Acute. 839. What electrocardiography changes may show scar: A. Changed T waves. B. Changed P. C. * Changed Q. D. Changed R. E. Changed S. 840. Duration of pain at the angina pectoris: A. 1-3 min. B. * 5-20 min. C. More then 30 min. D. Some days. E. During week. 841. Where are changes defined at a anterior infarction: A. * І, ІІ, AVL, V1-V3. B. ІІ, ІІІ, AVF. C. V1, V2. D. V4. E. V5, V6. 842. Duration ІІ – acute stage: A. Some first hours – 1 day. B. * 2 day till 2 weeks. C. Till 2-3 months. D. Till 6 month. E. 30-60 min. 843. When leycocytosis is being decreasing at a myocardial infarction ? A. Till 1-2 day. B. Till 12-24 hours. C. Till 2-3 day. D. Till 5-th day. E. * Till 7-th day. 844. What indicator of blood is a myocardial infarction marker: A. Electrolytes. B. Glucose. C. Creatinine. D. * Troponine. E. Cholesterole. 845. Duration ІV – scarring stage: A. Some first hours – 1 day. B. 2 day till 2 weeks. C. Till 2-3 months. D. * Till 6 month. E. 30-60 min. 846. Acute coronary syndromes includes unstable angina and: A. Stable angina. B. * Myocardial infarction. C. Myocarditis. D. Pericarditis. E. Hypertension attack. 847. Heart failure is an ... A. Incompetence of the heart to provide the body’s requirements at blood circulation during rest Incompetence of the heart to provide the body’s requirements at blood circulation during rest and physical activity B. * Incompetence of the heart to provide the body’s requirements at blood circulation during physical activity C. D. Incompetence of patient to hold stable level of blood pressure and pulse rate. E. Nothing from above 848. Which symptoms characterize RVF? A. Nocturia, hepatomegaly, nocturnal cough. B. * Edema of the lower extremities, hepatomegaly. C. Edema of the lower extremities, nocturnal cough D. Dyspnea, chest pain, dry cough. E. Nothing from above. 849. What symptom does not characterize LVF? A. Dyspnea B. Orthopnea C. Cough D. Nocturia E. * Edema of the lower extremities 850. What are percussion findings at the patients with LVF? A. The left border of relative heart dullness drifts left B. The right border of relative heart dullness drifts right C. The right border of relative heart dullness drifts left D. Nothing from above E. * Depend on clinical situation 851. What are auscultation findings at the patients with heart failure? A. Weakened S1 and S2, S3 gallop B. Weakened S1 and systolic murmur C. * Depend on disease which lead to heart failure D. Accented S2 over aorta, diastolic murmur E. Weakened both sounds 852. What BP does patient with heart failure have? A. Systolic BP decreased, narrow pulse pressure B. Systolic BP increased, wide pulse pressure C. Systolic BP normal, increased diastolic BP D. * Depend on clinical situation E. Nothing from above 853. If patient has dyspnea on ordinary activity, he has… A. I functional class of HF B. * II functional class of HF C. III functional class of HF D. IV functional class of HF E. Nothing from above 854. If less than ordinary activity causes dyspnea at the patient, he has… A. I functional class of HF B. II functional class of HF C. * III functional class of HF D. IV functional class of HF E. Nothing from above 855. Ejection fraction is used to determinate… A. Cause of the LVF B. Severity of the LVF C. Cardiothoracic ratio D. * Cause of the LVF and Severity of the LVF E. Nothing from above 856. If patient has ejection fraction 44 % he has… A. No heart failure B. * Mild LVF C. Moderate LVF D. Severe LVF E. Terminal LVF 857. Which symptoms characterize LVF? A. Nocturia, hepatomegaly, nocturnal cough. B. Dyspnea, chest pain, dry cough. C. * Dyspnea, orthopnea, nocturnal cough. D. Edema of the lower extremities, hepatomegaly. E. All from above. 858. What symptom does not characterize RVF? A. Edema of the lower extremities B. Hydrotorax C. Hepatomegaly D. Ascites E. * Dry cough, dyspnea. 859. What diseases can lead to heart failure? A. Arterial hypertension B. Valvular heart disease C. Myocardial infarction D. Cardiomyopathies E. * All from above 860. What are percussion findings at the patients with RVF? A. The left border of relative heart dullness drifts left B. The right border of relative heart dullness drifts right C. The right border of relative heart dullness drifts left D. Nothing from above E. * Depend on clinical situation 861. What are the lung auscultation findings at the patients with heart failure? A. Vesicular breathing, basal rales B. Diminished vesicular breathing C. * Diminished vesicular breathing and crepitation D. Vesicular breathing and pleural friction rub E. Nothing from above 862. If patient has heart disease, but ordinary activity does not cause dyspnea, he has… A. * I functional class of HF B. II functional class of HF C. III functional class of HF D. IV functional class of HF E. Nothing from above 863. If patient has dyspnea at rest and all activity causes discomfort, he has… A. I functional class of HF B. II functional class of HF C. III functional class of HF D. * IV functional class of HF E. Nothing from above 864. Echocardiography: A. May indicate the cause of HF B. Can confirm the presence or absence of LV dysfunction C. Is the less useful than chest X – ray for recognizing HF D. * May indicate the cause of HF and Can confirm the presence or absence of LV dysfunction E. All from above 865. If patient has ejection fraction 37 % he has… A. No heart failure B. Mild LVF C. * Moderate LVF D. Severe LVF E. Terminal LVF 866. If patient has ejection fraction 23 % he has… A. No heart failure B. Mild LVF C. Moderate LVF D. * Severe LVF E. Terminal LVF 867. Which level of the blood pressure is corresponded to mild hypertension? A. 140/< 90 mm Hg. B. * 140-159/90-99 mm Hg. C. 160-179/100-109 mm Hg. D. ? 180/? 110 mm Hg. E. ?155/?100 mm Hg 868. Risk factors of essential hypertension: Family history, race (blacks), stress, obesity, a high intake of saturated fats or sodium, use of tobacco, sedentary lifestyle. A. * Family history, stress, obesity, a high intake of saturated fats or sodium, use of tobacco, hepatitis, sedentary lifestyle. B. Family history, stress, obesity, a high intake of saturated fats or sodium, cardiac arrhythmia, sedentary lifestyle. C. D. Stress, obesity, a high intake of saturated fats or sodium, use of tobacco, hepatitis, sedentary lifestyle. E. Family history, race (blacks), cardiac arrhythmia, sedentary lifestyle. 869. What arterial pressure is corresponded to moderate hypertension? A. 140/< 90 mm Hg. B. 140-159/90-99 mm Hg. C. * 160-179/100-109 mm Hg. D. ? 180/? 110 mm Hg. E. ?155/?100 mm Hg 870. What are the pulse properties at patients with arterial hypertension? A. * Hard, intense. B. Hard. C. Frequent. D. Intense, frequent. E. Arrhythmic, slow. 871. What is the commonest symptom at patients with essential hypertension? A. Sleep disorders. B. * Headache. C. Myalgia. D. Arrhythmia. E. Edemas 872. How are the heart borders displaced at patient with the 2nd stage of essential hypertension? A. Shift to the right. B. * Shift to the left. C. Shift to the left and up. D. Shift to the right, left and up. E. Not changed. 873. During auscultation of patients with prolonged arterial hypertension you can hear: A. * Diminished S1 at the apex, and accented S2 at the aorta. B. Loud S1 at the apex, and accented S2 at the aorta. C. Increased S1 at the apex, and diminished S2 at the aorta. D. Diminished S1 at the apex and S2 at the aorta. E. Normal heart sounds 874. ECG sign of the left ventricular hypertrophy: A. High R at the V3, V4. B. High R at the V1, V2. C. * High R at the V5, V6. D. Deep S at the I lead. E. High R at the III lead. 875. Which organs are considered target at the patients with arterial hypertension? A. Heart, liver, lungs and brain B. Liver, brain, kidney, eyes C. * Heart, brain, kidney, eyes, vessels D. Heart, liver, lungs and kidney E. Liver, brain, kidney, eyes, heart. 876. Criterions of the ІI stage of essential hypertension: Episodic elevation of BP with cerebral, cardiac and general symptoms without any other signs except high BP. A. B. * Permanent symptoms and signs of the target organs affecting without their failure. C. Permanent symptoms and signs of the target organs affecting with their failure (complicated stage) D. Frequent hypertonic crisis. E. Lack of effect of the medication treatment. 877. What blood pressure is corresponded to severe hypertension? A. 140/< 90 mm Hg. B. 140-159/90-99 mm Hg. C. 160-179/100-109 mm Hg. D. * ? 180/|? 110 mm Hg. E. >160/>100 mm Hg. 878. How is color of skin changed at the patient with arterial hypertension? A. * Flush of the face and sclera. B. Flush of the foot. C. Flush of the stomach. D. Flush of the back E. Flush of the hands 879. What blood pressure is corresponded to isolated systolic hypertension? A. * 140/< 90 mm Hg. B. 140-159/90-99 mm Hg. C. 160-179/100-109 mm Hg. D. ? 180/|? 110 mm Hg. E. <150/110 mm Hg. 880. How is apex bit changed at patient with prolonged arterial hypertension? A. Heaving displaced to the right, and resistant. B. Heaving, displaced to the left, and not resistant. C. * Heaving, displaced to the left, and resistant. D. Not changed, normal E. Displaced to the right and not resistant. 881. How are the heart borders displaced at patient with the 1st stage of essential hypertension? A. Shift to the right. B. Shift to the left. C. Shift to the left and up. D. Shift to the right, left and up. E. * Not changed. 882. During auscultation of patients with hypertonic crisis you can hear: A. Diminished S1 at the apex, and accented S2 at the aorta. B. * Loud S1 at the apex, and accented S2 at the aorta. C. Increased S1 at the apex, and diminished S2 at the aorta. D. Diminished S1 at the apex and S2 at the aorta. E. Normal heart sounds 883. Which investigation is the most informative for establishing arterial hypertension? A. * Daily BP monitoring. B. Daily EKG monitoring. C. Coronarography. D. Echocardiography E. Tredmill test. 884. Criterions of the ІIІ stage of essential hypertension: Episodic elevation of BP with cerebral, cardiac and general symptoms without any other signs except high BP. A. B. Permanent symptoms and signs of the target organs affecting without their failure. C. * Permanent symptoms and signs of the target organs affecting with their failure (complicated stage) D. Frequent hypertonic crisis. E. Lack of effect of the medication treatment. 885. Which diseases can be accompanied with arterial hypertension? A. Renal diseases B. Endocrine disease C. Coarctation of aorta. D. Nephropathy of pregnancy E. * all mentioned above 886. EchoCG sign of the left ventricular hypertrophy: A. Widening of the cavity of left ventricular. B. Widening of the cavity of right ventricular. C. * Widening of the posterior wall of the left ventricle. D. Widening of the left atrium cavity. E. Low ejection fraction. 887. Which functional murmur can be heard at mitral stenosis? A. Systolic hydremic B. Systolic hemodynamic C. Systolic muscular D. Kumbs’ murmur E. * Graham-Steel murmur 888. The best point for hearing the diastolic murmurs at aortic regurgitation is A. The heart apex B. * The Botkin – Erb point C. The second intercostal space, to the right from the breastbone D. The second intercostal space, to the left from the breastbone E. On the middle of the breastbone on the level of third rib 889. Anaemic murmur is heard better A. Above the lung artery B. At Bodkin’s point C. Above all valve orifices D. * On the apex of the heart E. Above the aorta 890. How is functional systolic murmur differed from organic one? A. It is not ruled by periods of breathing B. Loud, harsh, prolonged C. Do not change during exercises D. * Do not have irradiative zones E. Often supported by feeling of systolic “cat purr” 891. The pericardial friction rub usually appears at A. Uremia B. Hydropericardium C. Cardiomegaly D. Angina pectoris E. * Adhesion of pericardium and pleura 892. The pericardial friction rub differs from organic in that it is A. Become stronger during pressing the chest B. * Becomes weaker if patient bends forward C. Heard above zones, projections and places of the best auscultation of heart’s vavles D. Do not coincidance with cardiac periods E. Never gives tactile sings 893. Which organic murmur gives the filling of “cat purr” on the heart apex? A. Systolic murmur of mitral regurgitation B. * Diastolic murmur of mitral stenosis C. Systolic murmur of aortic stenosis D. Diastolic murmur of aortic regurgitation E. Systolic murmur of tricuspid regurgitation Which cardiac murmur gives tactile filling above absolute cardiac dullness that becomes stronger while bending the body forward? 894. A. Systolic murmur of mitral regurgitation B. Diastolic murmur of mitral stenosis C. Systolic murmur of aortic stenosis D. Diastolic murmur of aortic regurgitation E. * Systole-diastolic pericardial friction rub. 895. Which functional murmur can be heard at aortic regurgitation? A. Systolic hydremic B. Systolic hemodynamic C. * Flint’s murmur D. Coombs’ murmur E. Graham-Steel murmur 896. What are the reasons for Flint’s murmur in aorta valve deficiency A. Relative mitral regurgitation B. * Relative mitral stenosis C. Relative aortic stenosis D. Relative tricuspid regurgitation E. Relative pulmonary stenosis 897. Which pathological conditions can be confirmed by 2-dimenshional echocardiography? A. congenital heart disease, B. left ventricular aneurysm C. mural thrombus D. Valve heart diseases E. * All mentioned above 898. Which functional murmur can be heard at aortic regurgitation? A. Systolic hydremic B. Systolic hemodynamic C. * Flint’s murmur D. Coombs’ murmur E. Graham-Steel murmur 899. What are the reasons for Flint’s murmur in aorta valve deficiency A. Relative mitral regurgitation B. * Relative mitral stenosis C. Relative aortic stenosis D. Relative tricuspid regurgitation E. Relative pulmonary stenosis 900. Which pathological conditions can be confirmed by 2-dimenshional echocardiography? A. congenital heart disease, B. left ventricular aneurysm C. mural thrombus D. Valve heart diseases E. * All mentioned above 901. What diseases is the respiratory failure developed at? A. Lobar pneumonia B. Severe COPD C. Severe exacerbation of the bronchial asthma D. Massive pleural effusion E. * All mentioned above 902. What symptoms characterize the bronchial obstruction syndrome? A. * Wheezing, dry cough, tightness in the chest B. Cough with sputum, chest pain, fever C. Mixed dyspnea, hemoptysis, weakness D. Dyspnea, chest pain, palpitation E. Dry cough, chest pain, edema 903. What symptoms don’t characterize the bronchial obstruction syndrome? A. wheezing B. cough C. tightness in the chest D. dyspnea E. * purulent sputum 904. What change of vocal fremitus can be at the patient with bronchial obstruction? A. Amplifying B. Decreasing C. Absence D. Not changed E. * Change depends on clinical situation 905. What change of vocal fremitus can be at the patient with emphysema? A. Amplifying B. * Decreasing C. Absence D. Not changed E. Change depends on clinical situation 906. What change of vocal fremitus can be at the patient with respiratory failure? A. Amplifying B. Decreasing C. Absence D. Not changed E. * Change depends on clinical situation 907. What is the main symptom of the respiratory failure? A. cough; B. * dyspnea; C. palpitation; D. wheezing; E. chest pain. 808. What is the main symptom of the emphysema? A. cough; B. expiratory dyspnea; C. inspiratory dyspnea; D. wheezing; E. * mixed dyspnea. 909. How is elasticity of the chest changed at the patient with emphysema? A. increasing B. * decreasing C. not changed D. absence E. depend on clinical situation 910. How is elasticity of the chest changed at the patient with respiratory failure? A. increasing B. decreasing C. not changed D. absence E. * depend on clinical situation 911. How percussion sound is changed at the patient with bronchial obstruction? A. * unchanged B. dull C. small box sound D. tympanic E. depend on clinical situation 912. How percussion sound is changed at the patient with emphysema? A. unchanged B. dull C. * small box sound D. tympanic E. depend on clinical situation 913. How percussion sound is changed at the patient with respiratory failure? A. unchanged B. dull C. small box sound D. tympanic E. * depend on clinical situation 914. What are auscultation findings at the patient with bronchial obstruction? A. * Vesicular breathing with prorogated expiration, wheezing B. Diminished vesicular breathing, C. Diminished vesicular breathing and moist rales D. Diminished vesicular breathing and crepitation E. Vesicular breathing and pleural friction rub 915. What are auscultation findings at the patient with emphysema? A. Vesicular breathing with prorogated expiration, wheezing B. * Diminished vesicular breathing, C. Diminished vesicular breathing and moist rales D. Diminished vesicular breathing and crepitation E. Vesicular breathing and pleural friction rub 916. How is spirometry changed at the patient with bronchial obstruction? A. Increased FEV1, decreased FVC, FEV1/FVC> 70% B. * Normal FVC, decreased FEV1, FEV1/FVC< 70% C. Decreased FVC, decreased FEV1, FEV1/FVC <70% D. Increased FVC, increased FEV1, FEV1/FVC > 100% E. Normal FVC, normal FEV1, FEV1/FVC< 70% 917. How is spirometry changed at the patient with emphysema? A. Increased FEV1, decreased FVC, FEV1/FVC> 70% B. Normal FVC, decreased FEV1, FEV1/FVC< 70% C. * Decreased FVC, decreased FEV1, FEV1/FVC <70% D. Increased FVC, increased FEV1, FEV1/FVC > 100% E. Normal FVC, normal FEV1, FEV1/FVC< 70% 918. Which method can help to establish respiratory failure? A. bronchoscopy B. X-ray C. Computer tomography D. * pulsoxymetry E. Spirometry 919. Bronchial asthma is a… A. Acute inflammatory disease; B. Acute infective disease; C. Chonic infective disease; D. * Chonic iinflammatory disease; E. northing from above. 920. Chronic obstructive pulmonary disease is a… A. chronic inflammatory of trachea and large bronchus B. chronic inflammatory of large and medium bronchus C. * chronic inflammatory of medium, small bronchus with involving lung parenchyma and vessels D. All from above E. Northing from above 921. Which symptoms characterize bronchial asthma? A. Mixed dyspnea, cough with purulent sputum B. * Episodic dry cough, tightness of the chest, wheezing C. Chest pain with radiation to jaw, inspiratory dyspnea D. Permanent expiratory dyspnea, cough E. Episodic hemoptysis and dyspnea due to physical effort 922. Which symptoms characterize COPD? A. Mixed dyspnea, dry cough, chest pain B. Episodic dry cough, tightness of the chest, wheezing C. Chest pain with radiation to jaw, inspiratory dyspnea D. * Permanent expiratory dyspnea, cough, sputum production E. Episodic hemoptysis and dyspnea due to physical effort 923. What symptom doesn’t characterize bronchial asthma? A. wheezing B. cough C. tightness in the chest D. dyspnea E. * purulent sputum 924. What symptom doesn’t characterize COPD? A. wheezing B. cough C. * chest pain D. dyspnea E. purulent sputum 925. What change of vocal fremitus can be at the patient with COPD? A. Amplifying B. * Decreasing C. Absence D. Not changed E. Change depends on clinical situation 926. What change of vocal fremitus can be at the patient with bronchial asthma? A. Amplifying B. Decreasing C. Absence D. * Not changed E. Change depends on clinical situation 927. If patient has asthma symptoms 1-2 times in a week, 1 night awaking in a mouth, he has… A. Intermitend asthma; B. * Mild persistent asthma; C. Moderate persistent asthma; D. Severe persistent asthma; E. depends on clinical situation 928. If patient has asthma symptoms 1-2 times in a day, 1 night awaking in a week, he has… A. Intermitend asthma; B. Mild persistent asthma; C. * Moderate persistent asthma; D. Severe persistent asthma; E. depends on clinical situation 929. If patient has asthma symptoms 1-2 times in a year, night awaking is absent, he has… A. * Intermitend asthma; B. Mild persistent asthma; C. Moderate persistent asthma; D. Severe persistent asthma; E. depends on clinical situation 930. If patient has asthma symptoms 8-10 times in a day, every night awaking, he has… A. Intermitend asthma; B. Mild persistent asthma; C. Moderate persistent asthma; D. * Severe persistent asthma; E. depends on clinical situation 931. How percussion sound is changed at the patient with COPD? A. unchanged B. dull C. * small box sound D. tympanic E. depend on clinical situation 932. How mobility of the lung border is changed at the patient with COPD? A. unchanged B. * limited C. increased D. became immovable E. depend on clinical situation 933. How percussion sound is changed at the patient with mild asthma? A. * unchanged B. dull C. small box sound D. tympanic E. depend on clinical situation 934. What are auscultation findings at the patient with asthma attack? A. * Vesicular rough breathing with prorogated expiration, wheezing B. Diminished vesicular breathing, C. Diminished vesicular breathing and moist rales D. Diminished vesicular breathing and crepitation E. Vesicular breathing and pleural friction rub 935. What are auscultation findings at the patient with COPD? A. Vesicular rough breathing B. * Diminished vesicular breathing with prolongated expiration, wheezing C. Diminished vesicular breathing and moist rales D. Diminished vesicular breathing and crepitation E. Vesicular breathing and pleural friction rub 936. How is FEV1 increased after bronchial spasmolytic if patient has reversible obstruction? A. * >12% from initial B. >20% from initial C. >25% from initial D. 30% from initial E. 10% from initial If patient has permanent expiratory dyspnea during physical effort, FEV1 is 52% from predicted and FEV1/FVC 55% he has… 937. A. Mild COPD B. * Moderate COPD C. Severe COPD D. Very severe COPD E. Depend on clinical situation If patient has permanent expiratory dyspnea in a rest, FEV1 is 22% from predicted and FEV1/FVC 45% he has… 938. A. Mild COPD B. Moderate COPD C. Severe COPD D. * Very severe COPD E. Depend on clinical situation 939. What are the cardiovascular symptoms? A. Chest pain, cough, dyspnea, wheezes, haemoptysis. B. * Pain in the heart region, palpitation, intermissions, oedema C. Headache, dizziness, dysphagia, nausea, vomiting. D. Pain in the right subcostal region, bitter taste, brown urine, skin itching, jaundice. E. Back pain, dysuria, ishuria, eyes oedema, weakness. 940. What are the cardiovascular symptoms? A. Abdominal pain, nausea, vomiting B. * Dyspnea, faint (syncope), palpitation, dry cough C. Cough with rusty sputum, chest pain, dyspnea D. Swelling abdomen, constipation, melena E. Oedema, dysuria, haematuria 941. What feature does the pain at angina pectoris have? A. Be caused by physical extension B. Duration under 15 minutes C. Constricting, feeling of heaviness D. Radiate to the left hand and scapula E. * All mentioned above 942. What feature does not the pain at myocardial infarction have? A. Prolonged, continuous > 20-30 min. B. Severe, tight or burning. C. * Relief at rest D. Does not respond to nitrates. E. Radiate to both hands, jaws, neck. 943. If patient has heart failure his cough is characterized with A. * appearing at lying position B. a lot of rusty sputum C. it is permanent D. it is loud E. all mentioned above. 944. If patient has feeling of solitary beats at various intervals it is named A. * exrtasistole B. palpitation C. syncope D. dizziness E. heart dyspnea 945. If patient has feeling of accelerated and intensified heart contractions onto the chest wall it is named A. exrtasistole B. * palpitation C. syncope D. heart dyspnea E. heart pain 846. If patient has a lot of foamy pink liquid sputum it means he has A. * Pulmonary edema B. Pulmonary embolism C. Aortic aneurysm dissection D. all from above E. Northing from above 947. Which type of dyspnea is observed at the patients with cardiovascular diseases? A. Expiratory B. * Inspiratory C. Mixed D. Changing E. All mentioned above. 948. What is feature of dyspnea at patient with cardiac asthma attack? A. Appear at night B. Accompanying with dry cough C. Inspiratory D. Ortopnea position in the bed E. * all mentioned above 949. Which of the following disorders is not likely to be associated with hemoptysis? A. Mitral stenosis B. Pulmonary embolism C. Pulmonary edema D. * Pericarditis E. None of the above 950. What characteristics of edema at patient with heart failure? A. Asymmetrical on the part of body which patient lies on. B. Firstly on the face than gradually spreads to body down. C. * Firstly on the legs than gradually spreads to body up D. Hear the heart region E. Only on abdomen and hands 951. What position does a patient with cardiovascular insufficiency occupy? A. * A forced sitting position with the legs let down. B. The patient prefers to lie on the affected side. C. The patient sits upright or resting the hands on the edge of the table of chair. A lying position on the side (lateral recumbent position) with the head thrown back and the bent legs pulled up to the abdomen. D. E. A forced knee-elbow position. 952. What mechanisms are caused by the orthopnoea posture? A. Tissue oxygen demand reduce at rest, decreased myocardial ischemia B. * Re-distribution of blood into the low extremities, reducing of circulating blood volume, Decreasing blood volume, decreasing of venous pressure in the lesser circulation, improvement of gas exchange in the "alveoli-pulmonary capillaries" system, displacement of ascitis fluid C. Pericardial layers presses to one another, reduce their movement that decrease irritation of pain receptors in pericardium D. E. Improvement of diastolic cardiac function 953. What kind of posture is observed at angina pectopis? A. * Upright B. On the right side with high head of the bed C. Orthopnoea D. Sitting posture bending forward E. Knee-elbow posture 954. What kind of posture is observed at acute left ventricular failure? A. Upright B. On the right side with high head of the bed C. * Orthopnoea D. Sitting posture bending forward E. Knee-elbow posture 955. What cardiovascular disease is characterized with constant pale skin color? A. Angina pectoris B. Mitral stenosis C. * aortic valve diseases D. Essential hypertension E. All mentioned above 956. Which of the following conditions is least to produce jugular venous distention? A. * Right heart failure B. Chronic left heart failure C. Chronic hypoxemia D. Liver failure E. Circulation insufficiency 957. What kind of cyanosis is usually observed at patient with cardiovascular diseases? A. Central, warm B. * Peripheral, cold C. Peripheral warm D. Local (near heart region), cold E. Diffuse warm 958. Which method can we use for establishing edema A. Visual inspection B. Palpation C. weighing patient D. measuring leg circumstance E. * All mentioned above. 959. Loud first sound in the cardiac apex is auscultated in case of: A. Myocardiac infarction B. Myocarditis C. Myocardiac sclerosis D. * Synchronic systole of atriums and ventricles in case of full atrioventricular blockade E. Aortic stenosis 960. Weakening of the first sound in the cardiac apex is auscultated with: A. * Stenosis of mitral orifice B. Insufficiency of mitral valve C. Aortic stenosis D. Tricuspid Regurgitation E. Pulmonary hypertension 961. Weakening of both heart sounds is auscultated in case of: A. Myocardiac infarction B. Myocarditis C. Emphysema of lungs D. Myocardiosclerosis E. * All mentioned cases 962. Loud second sound in aorta is auscultated in case of: A. Insufficiency of aortic valve B. Aortic stenosis C. * Essential hypertension D. Mitral stenosis E. Mitral regurgitation 963. Loud both sounds in heart apex in case of: A. Lungs limbus shrinkage B. Posterior mediastinum tumors C. Forward inclination of body D. * All mentioned reasons E. Northing from above. 964. Loud first sound in the cardiac apex is auscultated in case of: A. Mitral stenosis B. Ciliary arrhythmia C. Full atrioventricular blockade D. * All mentioned cases E. No right answer 965. Loud second sound in pulmonary artery is auscultated in case of: A. Emphysema of lungs B. Chronic obstructive lung disease C. Pneumosclerosis D. * All mentioned reasons E. No right answer 966. ‘Quail’ rhythm is: A. Loud ‘flapping’ first sound B. * Loud ‘flapping’ first sound, second sound, opening snap of mitral valve C. Opening snap of mitral valve D. Loud first, second and third sound. E. No right answer 967. Loud ‘flapping’ first sound in heart apex is auscultated in case of: A. * Mitral stenosis B. Mitral insufficiency C. Aortic stenosis D. aortic insufficiency E. No right answer 968. Ground of the second sound accent appearance over the pulmonary artery is: A. High pressure in greater circulation B. * High pressure in the pulmonary circulation C. High pressure in cava veins D. All above mentioned E. Northing from above 969. Ground of the second sound accent above aorta is: A. * High pressure in greater circulation B. High pressure in pulmonary circulation C. High pressure in pulmonary veins D. All above mentioned E. Northing from above 970. ‘Gallop’ rhythm is auscultated in case of: A. Diffuse myocarditis B. Cardiac infarction C. Dilatational cardiomyopathy D. Cardiac insufficiency E. * All mentioned variants 971. The first sound in case of ‘gallop’ rhythm is: A. Intensified B. Reduplicated C. * Weakened D. All variants are right E. No right answer 972. Reduplication of first sound appears in case of: A. Asynchronous right and left ventricle contraction B. Block of bundle of His C. Bisystolia (systole in 2 portions) D. * All mentioned variants E. No right answer 973. Reduplication of second tone appears more often in: A. Aorta B. * Pulmonary artery C. Apex D. Xiphoid process E. All mentioned variants 974. Reduplication of second sound in pulmonary artery is connected with: A. High pressure in lesser circulation B. Asynchronous aortic and pulmonary artery valve closing C. Breathing D. * All mentioned is true E. No right answer 975. Presystolic ‘gallop’ rhythm is auscultated in case of: A. Cardiosclerosis B. * Mitral stenosis C. Chronic nephritis with hypertensive syndrome D. All above mentioned cases E. No right variant 976. Protodiastolic ‘gallop’ rhythm is auscultated in case of: A. * Myocardial infarction B. Tricuspid insufficiency C. Pneumonia D. All above mentioned cases E. No right variant 977. Embryocardia or pendulous rhythm appears in case of: A. High fever B. Paroxysmal tachycardia C. Cardiac insufficiency D. * All mentioned variants E. No right answer 978. What heart diseases listed below can you find organic systolic cardiac murmurs at? A. mitral stenosis B. * Aortic stenosis C. Aortic regurgitation D. Pulmonary regurgitation E. Tricuspid stenosis 979. The best point for hearing the systolic murmurs at aortic stenosis is A. The heart apex B. The Botkin – Erb point C. * The second intercostal space, to the right from the breastbone D. The second intercostal space, to the left from the breastbone E. On the middle of the breastbone on the level of third rib 980. Anaemic functional murmur is more often: A. * Systolic B. Diastolic C. Protodiastolic D. Presystolic E. Systola-diastolic 981. Haemodinamical functional murmurs can be auscultated at A. * Thyrotoxicosis B. Mitral stenosis C. Myocarditis D. Cardiosclerosis E. Hypertension disease 982. The pericardial friction pub is better heard A. On the heart apex B. on the Botkin-Erb point C. * Above the absolute heart’s dullness zone D. On heart’s base E. Near the xiphoid process 983. The pericardial friction rub differs from organic murmurs in that it is A. More delicate B. Heard like far away C. * Heard near the ear D. Always coincide with systole E. Well radiate to other auscultatic zones 984. The pericardial friction rub differs from organic in that it is A. Never gives any tactile fillings B. Becomes stronger if patient bends forward C. Coincidence with systole and diastole D. Loud E. * all mentioned above. Which organic murmur gives the filling of “cat purr” in the second intercostal space right from the breastbone? 985. A. Systolic murmur of mitral regurgitation B. Diastolic murmur of mitral stenosis C. * Systolic murmur of aortic stenosis D. Diastolic murmur of aortic regurgitation E. Systolic murmur of tricuspid regurgitation 986. Systolic murmur of aortic stenosis irradiates A. To the heart apex and to Botkin’s point B. To the left axillary region C. To the second left intercostal space D. To the area of xiphoid process E. * To the carotid and subclavical arteries 987. Which functional murmur can be heard at mitral stenosis? A. Systolic hydremic B. Systolic hemodynamic C. Systolic muscular D. Kumbs’ murmur E. * Graham-Steel murmur 988. The best point for hearing the diastolic murmurs at aortic regurgitation is A. The heart apex B. * The Botkin – Erb point C. The second intercostal space, to the right from the breastbone D. The second intercostal space, to the left from the breastbone E. On the middle of the breastbone on the level of third rib 989. Anaemic murmur is heard better A. Above the lung artery B. At Bodkin’s point C. Above all valve orifices D. * On the apex of the heart E. Above the aorta 990. How is functional systolic murmur differed from organic one? A. It is not ruled by periods of breathing B. Loud, harsh, prolonged C. Do not change during exercises D. * Do not have irradiative zones E. Often supported by feeling of systolic “cat purr” 991. The pericardial friction rub usually appears at A. Uremia B. Hydropericardium C. Cardiomegaly D. Angina pectoris E. * Adhesion of pericardium and pleura 992. The pericardial friction rub differs from organic in that it is A. Become stronger during pressing the chest B. * Becomes weaker if patient bends forward C. Heard above zones, projections and places of the best auscultation of heart’s vavles D. Do not coincidance with cardiac periods E. Never gives tactile sings 993. Which organic murmur gives the filling of “cat purr” on the heart apex? A. Systolic murmur of mitral regurgitation B. * Diastolic murmur of mitral stenosis C. Systolic murmur of aortic stenosis D. Diastolic murmur of aortic regurgitation E. Systolic murmur of tricuspid regurgitation Which cardiac murmur gives tactile filling above absolute cardiac dullness that becomes stronger while bending the body forward? 994. A. Systolic murmur of mitral regurgitation B. Diastolic murmur of mitral stenosis C. Systolic murmur of aortic stenosis D. Diastolic murmur of aortic regurgitation E. * Systole-diastolic pericardial friction rub. 895. Which functional murmur can be heard at aortic regurgitation? A. Systolic hydremic B. Systolic hemodynamic C. * Flint’s murmur D. Coombs’ murmur E. Graham-Steel murmur 996. What are the reasons for Flint’s murmur in aorta valve deficiency A. Relative mitral regurgitation B. * Relative mitral stenosis C. Relative aortic stenosis D. Relative tricuspid regurgitation E. Relative pulmonary stenosis 997. Which pathological conditions can be confirmed by 2-dimenshional echocardiography? A. congenital heart disease, B. left ventricular aneurysm C. mural thrombus D. Valve heart diseases E. * All mentioned above Which functional murmur can be heard at aortic regurgitation? 998. A. Systolic hydremic B. Systolic hemodynamic C. * Flint’s murmur D. Coombs’ murmur E. Graham-Steel murmur 999 What are the reasons for Flint’s murmur in aorta valve deficiency A. Relative mitral regurgitation B. * Relative mitral stenosis C. Relative aortic stenosis D. Relative tricuspid regurgitation E. Relative pulmonary stenosis 1000. Which pathological conditions can be confirmed by 2-dimenshional echocardiography? A. congenital heart disease, B. left ventricular aneurysm C. mural thrombus D. Valve heart diseases E. * All mentioned above 1001. The treatment for symptomatic sick sinus syndrome is - A. Atropine only B. Only bed rest C. * Pace maker implanation D. Propranolol only E. Cardiac massage 1002. Treatment of ventricular fibrillation is- A. * Immediate electrical cardio version B. IV sodabicarb. C. Intravenous digoxin D. IV Propranolol E. Pace maker implanation 1003. Acute symptomatic sinus bradycardia responds to - A. Adrenaline B. Dopamine C. * Atropine D. Norepinephne E. Digoxine 1004. Poor prognostic indicator in pneumococal pneumonia include - A. Leucocytosis over 20000 B. Old age C. * Systemic disease D. Type II pneumococcus E. Blood culture posituve 1005. Broncho penumonia due to measles occurs due to - A. Sinusitis B. * Immunomodulation C. Bronchial obstruction D. Aspiration E. Athelectasis 1006. Cryptogenic organising pneumonia is characterised by all of the following except - A. Migratory pulmonary opacities B. * Obstructive pattern of pulmonary function C. Arterial hypoxemia D. Good response to corticosteroids E. Arterial hypocapnia The single most useful clinical sign of severity of pneumonia in a person without underlying lung disease is 1007. A. Temp more than 38.5°C B. Heart rate more than 100/min C. Systolic BP less than 90 mm Hg D. * Respiratory rate more than 30/min E. Normal temperature 1008. Pneumonia alba is due to - A. Klebsiella B. Streptococci C. * Treponema pallidum D. Staphylococci E. Pseudomonas 1009. The most common causative organism for lobar pneumonia is- A. Staphylococcus aureus B. Streptococcus pyogenes C. * Streptococcus pheumoniae D. Haemophilus influenzae E. Streptococcus epidermalis 1010. All of the following features are seen in viral pneumonia except - A. Presence of interstitial inflammation B. * Predominance of alveolar exudates C. Bronchiolitis D. Multinucleate giant cells in the bronchiolar wall E. Acute respiratory infection 1011. Nosocomial pneumonia is most commonly caused by- A. * Gram-ve bacilli B. Gram+ ve bacilli C. Gram - ve cocci D. Mycoplasma E. Pseudomonas 1012. Complications of lobar pneumonia do not include - A. Lung abscess B. * Amyloidosis C. Suppurative arthritis D. Infective endocarditis E. Empyema of pleura 1013. Fever persisting even after treatment of pneumonia likely diagnosis is - A. * Empyema B. Fungal lesion C. Hydrothorax D. All of the above E. Amyloidosis 1014. Most common cause of empyema is- A. Bronchopleural fistula B. Tubercular pneumonia C. * Bacterial pneumonia D. Pleurisy E. Abscess of lung 1015. There is no correlation between X-ray appearance and clinical state of the patient in — pneumonia - A. * Mycoplasma B. Friedlanders C. Pneumoccal D. Staphylococcal E. Legionella 1016. Broncho penumonia due to measles occurs due to - A. Sinusitis B. * Immunomodulation C. Bronchial obstruction D. Aspiration E. Athelectasis 1017. Hypersensitivity pneumonitis is associated with - A. Hillarlymphodenopathy B. Raised IgE C. * Raised serum precipitins D. Increased eosionophilis E. Leucocytosis 1018. Red 'current jelly' sputum is characteristc of- A. Mycoplasma pneumonia B. * Klebsiella pneumonia C. Amebic lung abscess D. Bronchiectasis E. Legionella Devi, a 28 year female, has diarohea, confusion, high grade fever with bilateral pneumonitis.The diagnosis is 1019. A. * Legionella B. Neisseria meningitidis C. Streptoccocos pneumoniae D. H. Influenzae E. Staphylococcus aureus 1020. True about Legionella penumonia include- A. Occurs in epidemics B. Treated with penicillin C. Associated with splenomegaly D. * Diagnosed from sputum E. More common in children 1021. Which is not true about legionaire pneumonia - A. Seen mainly in immunocompromised person B. * Erythromycin is drug of choice C. Common in children and adult D. Smoking and alcohol are risk factor. E. Alcohol is a risk factor 1022. Characteristic histopathological feature of penumocystis carini pneumonia A. Interstitial pneumonitis B. Increased eosinophills C. * Foamy vacuolated exudates D. Mononuclear cell in bronchoalveolar lavage E. Neutrophil infiltration 1023. Pneumocystis carini pneumonia is diagnosed by - A. * Interstitial penumonia B. Eosinophils in septa C. Alveolar type I cell damaged with eosinophils D. All of the above E. Rentgenography 1024. All the following are used in the treatment of Pneumocystis carinii except - A. Pentamidine B. Dapsone C. Cotrimoxazole D. * Fluoroquinolones E. Peniciline 1025. Pneumocystis carini pneumonia prophylaxis is given in - A. * IfCD4 count < 200ml B. Tuberculosis C. If the viral load is 25,000 copies/ml D. Oral candidiasis E. Honorrhea 1026. Treatment of choice in Chlamydia pneumoniae is – A. Streptomycin B. * Erythromycin C. Cephalosporins D. Cotrimoxazole E. Penicillin 1027. Treatment of chlamydia pneumonia is A. * Erythromycin B. Ceftriaxone C. Penicillin D. Sulphonamide E. Tetracycline 1028. In mycoplasma pneumonia, following are seen except- A. Diffuse infiltration of lungs B. Cannot be cultured routinely C. * Best treatment by cefotaxime D. Serology is useful in diagnosis E. All antibiotics can be used 1029. Drug of choice for Mycoplasma pneumoniae is – A. Penicillin B. * Tetracycline C. Amphotericin B D. Cotrimoxazole E. Cephalosporine 1030. Bronchiectasis is most lobe- A. Right upper lobe B. Right middle lobe C. Left upper lobe D. * Left lower lobe E. Whole lung 1031. Which of the following is NOT a complication of bronchiectasis – A. Lung abscess B. * Lung cancer C. Amyloidosis D. Empyema E. Pneumonia 1032. Complication of bronchiectasis include all except A. Amyloidosis' B. Lung abscess C. Cerebral abscess D. * Bronchiogenic carcinoma E. Pneumonia 1033. True about kartagener's syndrome - A. * Dextrocardia B. Infertility C. Mental retardation D. Bronchiectas E. Tetrade of Fallot 1034. Features seen in Bronchiolitis obliterans with organizing Pneumonia include - A. Polypoid plugs in bronchioles B. Ulceration and exudation of epithelium into the C. * Exudation of proteinaceous material in airways D. Bronchoconstriction E. Response to steroids 1035. All the following are features of Tropical Pulmonary Eosinophilia except - A. Eosinophilia > 3000/mm3 B. * Microfilaria in blood C. Paroxysmal cough and wheezing D. Bilateral chest mottling and increased bronchovascular markings E. High leucocytosis 1036. Commonest sign of aspiration pneumonitis is A. Cyanosis B. * Tachypnoea C. Crepitations D. Rhonchi E. Dyspnoe 1037. Hemolysis is caused in which pneumonia - A. Haemophilous B. Klebsiella C. Pseudomonas D. * Streptococcus E. Legionella 1038. Earliest manifestation of pulmonary embolism is - A. Cyanosis B. Hemophysis C. * Dyspnoea D. Chest pain E. Cough 1039. Pulmonary embolism causes - A. Bradycardia B. Decreased cardiac output C. * Arterial hypoxemia D. Acute right ventricular strain E. Tachycardia 1040. Pulmonary embolism is seen in all except - A. * Fanconi's anemia B. Paroxysmalnocturnal hemoglobinuria C. Oral contraception D. Old age E. Children 1041. Commonest symptoms of pulmonary embolism - A. Chest pain B. * Dyspnoea C. Haemoptysis D. Cough E. Chest pain 1042. Most reliable investigation in the diagnosis of pulmonary embolism is - A. Lung scan B. * Angiography C. Differential gas tension D. ECG E. CT 1043. Treatment of recurrent pulmonary embolism in adults includs - A. Mobin Udin Umbrella B. * Kimray greenfield filter C. Plication of IVC D. Femoral thromboembolectomy E. Medicamentations 1044. Investigation of choice in pulmonary embolism is – A. Chest X-ray B. Ultrasound C. * CT scan D. Ventillation - Perfusion scan E. Holter monitoring 1045. Most diagnostic investigation in pulmonary embolism is - A. Angiography B. X-ray chest C. * Ventilation - perfusion scan D. CT scan E. USG 1046. Which of the following are featrues of pulmonary embolism - A. * Respiratory alkalosis B. Right axis deviation C. Normal A-a Gradient D. Ventricular strain E. Methabolic acydosis 1047. Pulmonary embolism is most commonly produced by which of the following - A. Trauma B. Atherosclerosis C. * Thrombosis of pelvic vessels D. None E. Operation 1048. Most reliable investigation in the diagnosis of pulmonary embolism is - A. Lung scan B. * Angiography C. Differential gas tension D. ECG E. Holter monitoring 1049. What is the definitive method of diagnosing pulmonary embolism ? A. Ventilation perfusion imaging B. Positron Emission Tomography C. High Resolution CT D. * Pulmonary angiography E. Rentgenjgraphy 1050. The recent terminlogy for status asthmaticus is - A. Episodic asthma B. Chronic asthma C. Acute asthma D. * Severe actute asthma E. Atopic asthma 1051. Which of the following drugs are used in bronchial asthma – A. Isoprenaline B. Salbutamol C. Aminophylline D. * All of the above E. Becotidi 1052. Curschmann's spirals in sputum is seen in - A. Tuberculosis cavity B. * Asthma C. Bronchitis D. Bronchiectasis E. Pneumonia 1053. All of the following are useful for treating acute bronchial asthma in children except - A. 100% Oxygen B. Hydrocortisone infusion C. IV aminophylline D. Sodium chromoglycate inhalation E. * Inhalation of Carbogen 1054. Following are true of Acute bronchial Asthma except- A. Intercostal muscle retraction B. * Monosyllabilic sound C. Cyanosis D. Decreased respiratory rate E. Dyspnoea 1055. Bronchial Asthma is associated with raised levels of- A. * Leukotrienes B. PGI2 C. PGI 1 D. Thrombo xane E. All above 1056. Drug of choice in asthma with heart disease is- A. Rimiterol B. Terbutaline C. * Ipratropium D. Cromolyn sodium E. Steroids 1057. One of the following is not an indicator of the severity of asthma - A. Use of accessory muscles B. Pulsus paradoxus C. Cyanosis D. * Systolic hypertension E. Increase of heart rate 1058. In bronchial asthma there is constriction of - A. Large airway B. Medium airway C. Terminal bronchiole D. * Respiratory bronchiole E. Low airway 1059. Aspirin sensitive asthma associated with - A. Extrinsic asthma B. Usually associated with urticaria C. Associated with nasal polyp D. * Obesity E. Atopic asthma 1060. Asthma is associated with all except – A. Hyper recactive airways B. Persistent cough C. Episodic wheezing D. * Normal Spirometry E. Picfluometry 1061. Use of disodium cromoglycate as a preventive measure has been found to be of value in - A. Intrinsic asthma B. * Excercise induced asthma C. Chronic bronchitis D. Famers lung E. Aspirin asthma 1062. Bronchial asthma is characterized - A. * Inflammatory disease of airway B. Allergic disease of air way C. Hypo responsive ness of airway D. Hyper responsiveness of airway E. Treatment is mostly inhaled steroid 1063. True about Asthma except- A. Inflammatory disease B. * Hyper responsive C. Necrosis of airway D. Mucous plug formation E. Airway edema 1064. True about morphology of Asthma - A. Charcot- leyden crystal B. Irreversible C. Involve larger airways D. * Intermittent asthma is better responsive to bronchodilator therapy E. Hypersensitive lung. 1065. True about asthma - A. * Increasing incidence day by day B. Allergic asthma common in older patints C. Increase in IgE in idiosyncratic asthma D. Bronchoconstriction E. Atopic asthma in children 1066. Not a feature of acute severe asthma - A. Tachycardia B. Respiration C. Pulsus paradoxus D. * None E. Dyspnoea 1067. Bronchial asthma can be diagnosed by- A. * Wheeze B. Dyspnea C. Normal FEV, D. Cough E. Reversible obstruction 1068. Universal finding is asthma is - A. * Hypoxia B. Hypercarbia C. Hypoxemia D. Respiratory acidosis E. Metabolic acidosis 1069. Anti-inflammatory action of airways- A. Fluticasone B. Ipratropium bromide C. * Budesonide D. Theophylline E. Terbutaline 1070. What are exacerbations of bronchial occur with little or no warning, called A. * Brittle asthma B. Acute severe asthma C. Poorly controlled asthma D. Nocturnl asthma E. Aspirin asthma 1071. All are used in bronchial asthma, except – A. Salbutamol B. * Morphine C. Aminophylline D. Steroid E. Bocotidi 1072. The features of addisons disease is/are – A. Weight loss B. Skin pigmentation C. Hyponatremia D. Hyperkalemia E. * All 1073. In addisons diesease, the follwoing features are seen - A. Hypokalaemia B. High blood pressure C. Weight loss D. Hyperpigmentation E. * Hyponatremia 1074. Diagnostic test for pheochromocytoma is - A. Ultra sound B. * Estimation of urinaiy metanephrines C. Estimation of urinary 5-HIAA D. Phenotolamine test E. Adrenaline test 1075. In addisons disease the following is seen- A. Hypernatremia B. Hypokalemia C. Hypertension D. * Hypotension E. Hyperkalemia 1076. Conn's syndrome is characterised by all except – A. Polyuria B. Polydipsia C. Weakness D. * Anasarca E. Hypertension 1077. Which of the following are causes of Hyperkalemia – A. Crush syndrome B. Conn's syndrome C. * Addisons disease D. Acute renal failure E. Coushing syndrome 1078. Which is fals e about Conns Syndrome- A. * Generalised edema B. Hypotension C. Hyponatremia D. Hyperkalemia E. Weight loss 1079. Congenital 17-hydroxylse deficiency leads to - A. * Hypertension B. Virilism C. Hermaphroditism D. Hyperkalemia E. Hypotension 1080. Adrenal reserve is best tested by means of infusion with A. Glucocorticoids B. * ACTH C. Hypothyrodism D. Metyrapone E. Glucose 1081. Hyperaldosteronism causes - A. Hyperkalemia B. Hyponatremia C. Decreased water reabsorption D. * Hypokalemia E. Hypertenson 1082. Activation of the renin stimulates - A. Water excretion B. Potassium retention C. * Sodium retention D. Magnesiumexcretion E. Protein methabolism 1083. Primary hyperaldosteronism does not have – A. * Ankle oedema B. Polyuria C. Hypertension D. Hypokalemia E. Hypotension 1084. Metyrapone inhibits – A. * 11-B-hydroxylase B. 21-B-hydroxylase C. Both D. None E. There is no right answer A 25 year old male presnents with weakness, occasional vomiting hypotension, skin and mucous membrane pigmentgation. The diagnosis can be best established by 1085. A. Metyrapone test B. Basal plasma Cortisol levle C. 24- hour urinary 17-Ketosteroid D. * ACTH stimulation test E. Adrenaline test A 25 year old male patient presents with hypertension, investigatin - Na 145 meq/1 k-1.3 meq/I serum creatinine most probable diagnosis is 1086. A. Pheochromocytoma B. * Conn's syndrome C. Cushing's syndrome D. Renal paranchymal disease E. Diabetes mellitus 1087. Werner's syndrome (multiple endocrine neoplasia type I) is characterised by all of the following except A. Tumours of anterior pituitary B. Tumours of parathyroids C. Pancreatic adenomas D. * Phaeochromocytoma E. Cancer of thyroid 1088. Pheochromocytoma is associated with A. Vitiligo B. * Cafe-au-lait spots C. Ash leaf amelanotic macules D. Acanthosis Nigricans E. Demodecosis 1089. Characteristic feature of primary aldosteronism is - A. Low serum sodium B. High plasma renin C. * Low serum potassium D. High serum creatinine E. High blood potassium 1090. Adrenal aldosteronoma is best diagnosed by- A. * HRCT B. MRI C. IVP D. KUB E. CT Sushila, 25 year old young lady presented with complaint of acute hirsuitism and hoarseness of voice. Which of the following should be the best investigation to be done for the diagnosis 1091. A. Blood pregnenolone levels B. * Blood DHEA levels C. 17-ketosteroids level D. LH and FSH levels E. Glucose level 1092. In the adrenal gland, androgens are produced by the cells in the – A. Zona glomerulosa B. * Zona reticularis C. Zona fasciculata D. Medulla E. Whole gland 1093. Hypertonic contraction of fluid volume is caused by - A. Addisons disease B. Cushings disease C. Salt losing hephropathy D. * Diabetes insipidus E. Pancreatic carcinoma 1094. Which is true about addison's disease except - A. * Hypoglycemia B. Hypokalemia C. Hypernatremia D. Increased protein catabolism E. Hypercalemia 1095. Cushings syndrome is most commonly seen in - A. * Bronchogenic carcinoma B. Renal cell carcinoma C. Pancreatic carcinoma D. Lymphoma E. Addisons disease 1096. The levels of 17- ketosteroids in urine is increased in- A. Adrenal tumour only B. * Adrenal and testicular tumour C. Liver secondaries D. Bronchogenic carcinoma E. Pancreatic carcinoma 1097. Excretion of which of the following is increased in pheochromocytoma – A. Plasma HMA B. Serum bradykinin C. * Urinary VMA D. All of the above E. Adrenaline 1098. Secretion of cortisone is highest in – A. * 6a.m.-8a.m. B. 8a.m.-10a.m. C. 10a.m.-12a.m. D. 6p.m.- 10p.m. E. 8 p.m.-9 p.m. 1099. Addisonian like syndrome is a charactersitic side effect of- A. Chlopromazine B. Demeclocycline C. * Busulfan D. Practolol E. Prednisolone 1100. Which of the following drug is contra-indicated in pheochromocytoma- A. * Guenethidine B. Phenoxybenzamine C. Labetalol D. Propranolol E. Practolol Hypertension with androgenisation of a female child is a feature of congenital adrenal hyperplasia due to deficiency of1101. A. C-21 hydroxylase B. * C-ll hydroxylase C. C-17 hydroxylase D. Desmolase E. Both 1102. Congenital adrenal hyperplasia is associated most commonly with deficiency of – A. * 21 - hydroxylase B. 11 - hydroxylase C. 3-beta-ol dehydrogenase D. 17 – hydroxylase E. Both 1103. To differentiate malignant pheochromocytoma from benign, biochemically in the former, there is - A. Norepinephrine is increased B. * Dopamine metabolism is increased C. VMA over 10mg/24 hrs D. Epiinephrine is increased E. Adrenaline is increased 1104. Most common cause of adrenal insufficiency is - A. Sepsis B. Pneumococcal sepsis C. Waterhouse Friderickson Syndrome D. * Disuse atrophy due to steroid adminstration E. Pneumonia 1105. Ectopic ACTH secretion by carcinoma brounchus is differentiated from cushing's desease by - A. Purple stria B. Glucose intolerance C. Centripetal obesity D. * Hypokalemia and alkalosis E. Cough 1106. Drug used for medical adrenal medullectomy is - A. * Aminoglutethemide B. Ortho - para methyl benzoic acid C. Alloxan D. Methiodobenzo guanidine tagged 1131 E. Chlopromasine 1107. Regarding Addisonian pigmentation, all are true except- A. Involves moles and scars B. Involves palmer creases C. * Does not involve oral mucosa D. Decreased fibrosis E. Incresed fibrosis 1108. Medical adrenalectomy is seen with – A. Vincristine B. Vinblastine C. * Mitotane D. Methotrexate E. Cyclosporine 1109. True about cushing's syndrome is - A. Adrenomedullary hyperplasia in association with MEN syndrome is common cause B. * Bronchial & Mediastinal carcinoid causes cushing syndrome C. It is diagnosed by hypokalemia in association with increased adrenal secretion D. It is often fatal due to its coronary and cerebrovascular accidents E. All written above is true 1110. Conn's syndrome is characterised by all except – A. Polyuria. B. Polydipsia C. Weakness D. * Anasarca E. Cyrosis 1111. .Hypokalemia may be a feature of all following diseases, except - A. * Addison's disease B. Cushing's syndrome C. Barter's syndrome D. Gitelman's syndrome E. Adams Stocks syndrome 1112. Conn's syndrome is characterized by – A. Hyperinsulinism B. Hyperthyroidism C. Hypoadrenalism D. * Hyperaldosteronism E. Increased level of glucose 1113. Cushing's syndrome is not a feature of - A. Adrenal carcinoma B. Oat cell carcinoma of lung C. * Medulloblastoma D. Pituitary adenoma E. Thyroid adenoma 1114. The most common cause of Cushing's syndrome is – A. Pituitary adenoma B. Adrenal adenoma C. Ectopic ACTH D. * Iatrogenic steroids E. Adenoma of pancreas 1115. Intake of exogenous steroid causes – A. Addison's disease B. * Cushing's syndrome C. Pheochromocytoma D. Conn's syndrome E. Pituitary adenoma 1116. A common cause of Cushing syndrome is - A. Cancer producing ectopic ACTH B. * Pituitary adenoma C. Adrenal tuberculosis D. None of the above E. All of above 1117. Cushing syndrome is characterized by all except – A. DM B. HT C. Proximal myopathy D. Centripetal obesity E. * None 1118. Cushing syndrome is characterized by all except – A. Acne B. Hypertension C. Proximal myopathy D. Centripetal obesity E. * Hypoglycemia 1119. Features not seen in Cushing's Syndrome is A. * Hypoglycemia B. Hypertension C. Frank psychosis D. Hypokalemia E. Hypernatriemia 1120. All are features of cushings disease except - A. Central obesity B. * Episodic hypertension C. Easy bruising D. Glucose intolerance E. Hypotension 1121. About cushing syndrome, true is - A. Low dose dexamethasone suppress cortisone secretion B. CA of adrenal is more common than adenoma C. Pituitary adenoma size > 2 cm (usually) D. * TACTH secretion is the commonest cause E. High dose prednisolone supress cortisone secretion A patient with cushinoid features presents hemoptysis: he shows no response to dexamethasoc supression test; most likely diagnosis here is 1122. A. Adrenal hyperplasia B. Adrenal adenoma C. * Ca lung with ectopic ACTH production D. Pituitary microadenoma E. Diabetes mellitus 1123. Which of the following is the earliest manifestatkn of Cushing's syndrome - A. * Loss of diurnal variation B. Increased ACTH C. Increased plasma Cortisol D. Increased urinary metabolites of Cortisol E. Decreased ACTH 1124. Cushing's disease presents with - A. * Increased ACTH and increased Cortisol B. Decreased ACTH and decreased Cortisol C. Increased ACTH and decreased Cortisol D. Increased catecholamines E. Decreased catecholamines 1125. Most common cause of Conn's syndrome is - A. Adrenal hyperplasia B. Adrenal carcinoma C. * Adrenal adenoma D. Pituitary ACTH hypersecretion E. Adrenal hypoplasia 1126. NOT a feature of primary hyperaldosteronism is – A. * Pedal edema B. Diastolic hypertension C. Polyuria D. Hypokalemia E. Hypernatriemia 1127. Which is NOT a feature of primar hyperaldosteronism - A. Hypokalemia B. Hypertension C. Hypernatremia D. Increased renin level E. * Hypotension 1128. The following are features of primaf hyperaldosteronism except - A. Polyuria B. Hypertension C. Hypokalemia D. * Hyperkalemia E. Hypotension 1129. True about conn's syndrome – A. increase K+ B. decreaseK+ C. * Proximal myopathy D. increased plasma renin activity E. Edema 1130. All of the following are features of priman hyperaldosteronism except - A. * Pedal edema B. Polyurea C. Hypokalemia D. Hypertension E. Hypotension 1131. Conn's syndrome is associated with aiL except - A. Hypertension B. Muscle weakness C. Hypokalemia D. * Edema E. Weight loss 1132. True about primary aldosteronism – A. Pedal oedema B. Increased renin C. * Increased Na+ D. Decreased K+ E. Hypertension 1133. In primary adrenal hyperplasia, incorrect is- A. Hypokalemia B. * Hyponatremia C. Hypernatremia D. Water retention E. Hyperkaliemia 1134. Addison's disease is characterized by all except – A. * Hyperglycemia B. Hypotension C. Hyperkalemia D. hyponatremia E. Hypertension 135. Chronic adrenal insufficiency is characterized by all of the following except - A. Excess pigmentation B. Asthenia C. * Weight gain D. Hypoglycemic episodes E. Weigth loss 1136. Addison's disease is characterized by following except – A. Hyperkalemia B. Hypotension C. Hyponatremia D. * Hypocalcemia E. Hypotension 1137. Which is NOT a clinical feature of Addison's disease – A. Hypoglycemia B. Hyponatremia C. * Hypocalcemia D. Hyperkalemia E. Hypercalcemia 1138. Regarding Addisonian pigmentation, all are true except - A. Involves moles and scars B. Involves palmer creases C. * Does not involve oral mucosa D. Decreased fibrosis E. Involve oral mucosa 1139. Addisons's disease is associated with all except - A. Cardiac atrophy B. Decreased diastolic B.P. C. Serum Cortisol < 8 D. * Low renin levels E. High renin levels 1140. What points, concerning myxedema coma are correct ? A. * Hypothermia is common B. Feeling warm may provoke myxedema coma C. Cause is – increased sensitivity to T 3 and T4 receptors. D. Hyperfunction of adrenal glands E. Thyroid cancer 1141. Developing of gigantism is conditioned by: A. * Overwhelming secretion of GH in adolescence B. Overwhelming secretion of GH in old age C. Overwhelming secretion of GH in adults D. Overwhelming secretion of somatostatin in adolescence E. Inborn sensitivity lack in tissues to GH 1142. Choose factors, which can cause Addison’s disease A. * Tuberculosis B. Tumor acting on adrenal hormone C. Autoimmune destruction of thyroid gland D. Diabetes Mellitus E. Brain tumor 1143. To remove onset of tetany you will order A. * Calcium chloride B. Benzylpenicillin C. Prednisolone D. Potassium citrate E. Magnesium sulphate 1144. Macroangiopathy, as a symptom of diabetes mellitus, most often destroy vessels of: A. * Brain B. Lung C. Kidneys D. Retina E. Intestine 1145. The treatment of Grave’s disease usually include A. * Antithyroid drugs B. Antidepressants C. Narcotic analgesics D. Diuretics E. Sulfonylureas 1146. Choose factors, which can cause Addison’s disease A. * Tuberculosis B. Tumor acting on adrenal hormone C. Autoimmune destruction of thyroid gland D. Diabetes Mellitus E. Brain tumor 1147. Fundus picture of stage 2 of keith Wegener classification includes- A. * Copper wire AV nipping and focal spasm B. Silver wire increased reflex C. Exudate and hemorrhagic spots D. Papilledema E. Vitiligo 1148. Quick reduction of blood pressure is done in - A. Cerebral infarct B. * Hypertensive encephalopathy C. Myocardial infarction D. Any patient with hypertension E. Renal failure 1149. Hypertension can be caused by- A. * Renin B. Antigiotensin I C. Angiotension II D. PG E. Adrenalin 1150. Hypertension with increased renin levels is seen in- A. Segmental infarction B. Fibromuscular hyperplasia of renal artery C. * Aortic stenosis D. Hyperaldosteronism E. Mitral stenosis 1151. Renin dependent hypertension includes - A. Primary hyperaldosteronism B. Essential hypertension C. Renovascular hypertension D. * Pheochromocytoma hypertension E. Secondary hyperaldosteronism 1152. Which does not cause hypertension - A. Dobutamine B. * Ritodrine C. Dopamine D. Methoxamine E. Prednisolone 1153. Malignant hypertension is diagnosed when - A. Associated malignancy is present B. Diastolic B.P. 120 mg Hg C. * Papilledema associated with elevated B.P. D. All of the above E. Nothing of the above 1154. Treatment of hypertensive emergency is- A. * Hydralazine B. Glucokinase C. Propranolol D. Furosemide E. Ritodrine 1155. Calcium blocking agents of use in treatment of hypertension include - A. Prazosin B. Verapamil C. Captopril D. * Nifedipine E. Lidoflazine 1156. Severity of B.P. is graded mainly by- A. * Systolic B.P. B. Pulse pressure C. Diastolic pressure D. Response to treatment E. Clinic features 1157. Renin plays important role in - A. * Renovascular hypertension B. Malignant hypertension C. Coronary artery disease D. Essential hypertension E. Adrenal hypertension 1158. Ideal imaging modality for Renal arterial A. aj IVP B. USG C. * Angiography D. Renin assay E. MRI hypertension - Which one of the following is of most serious prognostic significance in a patient of essential hypertension 1159. A. Diastolic blood pressure greater than 130 mmHg B. Transient ischaemic attacks C. Left ventricular hypertrophy D. * Papilledema and progressive renal failure E. Right ventricular hypertrophy 1160. In benign hypertension commonest vascular pathology is. A. Atherosclerosis B. Fatty infilitraion of intima C. Fibrnoid necrosis D. * Hyaline arteriosclerosis E. Molecular necrosis 1161. All of the following are feature of malignant hypertension EXCEPT - A. Grade IV hypertensive retinopathy B. Haemolytic blood picture C. Renal failure D. * Respiratory failure E. Hepatic failure 1162. Drug of choice for hypertensive crisis associated with acute nephritis is - A. * Sodium nitroprusside B. Hydralazine C. Reserpine D. Calcium channel blockers E. Propranolol 1163. In essential hypertension the drug prescribed with least cardiovascular effect- A. Clonidine B. Alpha blocker C. Beta blocker D. * ACE inhibitor E. Diuretic 1164. Most common cause of renal artery stenosis in young adults in India is- A. Atherosclerosis B. * Non specific aorto-aortitis C. Fibro muscular dysplasia D. None of the above E. All of the above 1165. Renal artery stenosis may occur in all of the following except - A. Atherosclerosis B. Fibromuscular dysplasia C. Takayasu's arteritis D. * Polyarteritis nodosa E. Hyaline atherosclerosis Angiographically, the typical "beaded" or "pile of plates" appearance involving the internal carotid artery is seen in 1166. A. Takayasu's Disease B. Non-specific aorto-arteritis C. * Fibromuscular dysplasia D. Rendu-Osler-Weber Disease E. Aortoarthreitis 1167. Commonest cause of sustained severe hypertension in children- A. Endocrine causes B. Coarctation of aorta C. * Renal parenlchyma disease D. Pheochromocytoma E. Tumor of pancreas 1168. In essential hypertention changes seen in the heart are- A. Cardiac cell hyperplasia B. * Cardiac cell hypertrophy C. Increse in the mitochondrial number D. Increase in size of mitochondria E. Decrease in size of mitochondria Which of the following is most specific and sensitive screening test in a case of renovascular hypertensive 1169. A. * HRCT B. CT guided angiography C. Captopril induced radionuclide scan D. MRI E. Capilaroscopy 1170. Quick Reduction of blood pressure is done in - A. Cerebral infarct B. * Hypertensive encephalopathy C. Myocardial infarction D. Any patient with hypertension E. Renal failure 1171. All of the following drugs can be used in hypertens emergency A. Trimethaphan B. * I.V. hydralazine C. Indapamide D. Sublingual nifedipine E. Clofeline 1172. All of the following are useful intravenous there for hypertensive emergencies except A. Fenodolpam B. Uradipil C. Enalapril D. * Nifedipine E. Furosemide 1173. A hypertensive, diabetic is having proteinuria antihypertensive of choice is A. Propanolol B. Clonidine C. * Enalapril D. Alpha methyldopa E. Furosemide 1174. A young patient presented with blood pressure I 190/120 mm of Hg without any clinical symptw and fundus examination is normal, treatment of choice A. Oral Nitroglycerine B. IV Nitroglycerin I C. * Oral Enalapril D. IV Enalapril E. Sublingual short acting Nifedipine 1175. In Accelerated HTN what is metabolic defect - A. Normal non-ionic metabolic acidosis B. Ionic gap met acidosis C. Hypomagnesemia D. * Metabolic alkalosis E. Metabolic acidosis 1176. An elderly patient with hypertension with proteinuria without renal failure, drug choice is - A. Furosemide B. Methyldopa C. * Enalapril D. Propranolol E. Clofeline 177. In primary pulmonary hypertension basic abnormality in gene lies in A. * Bone morphogenetic protein receptor II B. Endothelin C. Homeoboxgene D. PAX-11 E. Thrombine 11178. Not seen in pre capillary pulm. hypertension A. T pressure in pulm circulation B. T capillary pressure C. Rt-vent. hypertrophy D. * T Pulm. wedge pressure E. Lung pressure 1179. Pulmonary hypertension is caused by - A. * Interstitial lung disease B. Myocardialinfarction C. Systemichypertension D. Thromboembolism E. Chronic pulmonal heart 1180. All are causes of pulmonary hypertension except A. * Hyperventilation B. Morbid obesity C. High altitude D. Fenfluramine E. Low altitude 1181. PuImonary hypertension in COPD is due to- A. Constriction of pulm vessels B. * Hypoxia C. Interstitial fibrosis D. Bronchoconstriction E. Hypercapnia 1182. PuImonary hypertension may occur in all of the following conditions except A. Toxic oi1 syndrome B. Progressive systemic sclerosis C. Sicke cell anemia D. * Argemone mexicana poisoning E. Atherosclerosis 1183. Which is a feature of high altitude pulmonary edema- A. Associated with low cardiac output B. * Associated with pulmonary hypertension C. Occcurs only in unacclamatized persons D. Exercise has no effect E. Associated with high cardiac output 1184. All are used for treating Pulmonary hypertension except A. Endothelin receptor antagonists B. Phosphodiesterase inhibitors C. Calcium Channel Blockers D. * Beta blockers E. Diuretics 1185. Most specific test for renovascular hypertension - A. CT Angiography B. MRI C. * Captopril induced radionuclide scan D. HRCT E. Capilaroscopy 1186. A 70% old male presented with B.P. 220/140.Which drugs should be included in his management plan A. Enalaprilat B. Losartan C. Amplodipine D. * Furosemide E. Chlorthalidone A person has headache & profuse sweating. On examinatio his B.P is 200/120 mm Hg. Which of the following shoud not not used 1187. A. * Nifedipine B. Sodium nitroprusside C. Phenaxybeszamine D. Methyldopa E. Labetalol A 20 year female has b/I bruit on flank. Her B.P is 160/110. Which of the following statement is correct. 1188. A. Enalaprildeteriotes renal function B. * Most definitive diagnostic procedure is contrast enhanced arteriography C. Always b/I D. Surgical intervention may be used E. Fibromuscular dysplasia is a common cause in this patient 1189. Calcium blocking agents of use in the treatment of hypertension include A. Prazosin B. Lidoflazine C. Captopril D. * Nifedipine E. Furosemide Which of the following drugs should not be used in a setting of severe hypertension in elderly on empirical basis ? 1190. A. Enalapril B. Amlodipine C. Chlorthiazide D. * Prazosin E. Clofeline 1191. In MI, which enzyme is raised in 4 to 6 hrs. & decreases in 3 to 4 days A. SGOT B. LDH C. * CPK D. SGPT E. CK-MB 1192. In stable angina- A. CK-MB is elevated B. Troponin I is elevated C. Myoglobin is elevated D. * The levels of cardiac markers remain unchanged E. Myoglobin is decreased 1193. What is diagnostic of fresh myocardial infarction inECG- A. QT interval prolongation B. P mitrale C. * ST segment elevation D. ST segment depression E. P pulmonale 1194. ST depression & T wave invesion in VI to V6 and a VL leads indicate- A. * Anterolateral wall AMI B. Posterior wall AMI C. Inferior AMI D. Lateral wall AMI E. None 1195. ALL of the following statement regarding the ECG in acute pericarditis are true except A. * T wave inversions develop before ST elevation retur to baseline B. Global ST segment elevation is seen in early pericarditis C. Sinus tachycardia is a common finding. D. PR segment depression is present in majority of E. patients F. T wave inversions develobp after St elevation retur tu baseline 1196. All of the following are risk factors for atherosclerosis except - A. Increased waist-hip ratio B. Hyperhomocysteinemia C. * Decreased fibrinogen levels D. Decreased HDL levels E. Increased HDL levels 1197. Risk factors for coronary artery disease (CAD) - A. High HDL B. Increased homocysteine levels C. * High LDL D. Decreased fibrinogen levels E. Increased lipoproeins In an old patient, the best indicator of probability of developing cardiovascular disease can be calculated by1198. A. * LDL/HDL ratio B. Triglycerides C. Total cholesterol D. Serum LDL E. Lipids A patient presents 12 hours following a Myocardial infarction. Which of the following enzymes will be elevated at this period 1199. A. Lactate dehydrogenase B. Serum glutamate oxaloacetate Transferase C. * Creatinine phosphokinase D. Myoglobin E. T I Troponins Troponin-T is preferable to CPK-MB in the diagnosis of acute myocardial infarction (MI) in all of the following situations except 1200. A. Bedside diagnosis of MI B. Postoperatively (after CABG) C. * Reinfarction after 4 days D. Small infarcts E. Transmural infarcts 1201. In Aortic dissection drug used are- A. * Propanolol B. Diazoxide C. Na nitroprusside D. Hydralazine E. Labetelol A patient complains of intermittent claudication, dizziness and headache, Which one of the following is the likely diagnosis ? 1202. A. * Coarctation of aorta B. Patent ductus arteriosus C. Tetralogy of Fallot D. Atrial septal defect E. Pentage of Fallot 1203. True about bicuspid aortic valve - A. * Aortic root dilation is present B. More in female C. Associated with NOTCH 1 mutation D. Most commonly associated with coarctation of aorta E. Most common complication is calcification of valve A 21-year old male presents with exertional dyspnea, raised JVP and loud P2. ECG shows right axis deviation. All of the following conditions are possible except: 1204. A. Atrial septal defect B. Mitral stenosis C. * Ostium primum D. Pulmonary thromboembolism E. Mitral insufficiency 1205. Changes in mean electrical axis of may be caused by - A. * Muscular necrosis B. Bundle branch block C. Change in body position D. Hypertrophy of one ventricle E. All of the above 1206. Most common cause of orthostatic hypotension – A. * Peripheral neuropathy B. Carcinoid Syndrome C. Pheochromocytoma D. Hypothyroidism E. All of the above The presence of one of the following clinical feature indicates very poor prognosis in a case of endotoxin shock 1207. A. Generalised weakness B. * Low volume pulse C. Tachycardia D. Oliguria E. Restlessness 1208. Endotoxic shock is due to - A. Gram positive bacteria B. * Gram negative enterobacteriae C. Viruses D. Gas gangrene E. Staphyloccocus 1209. Treatment of choice in cardiogenic shock with pump failure is- A. * Dopamine B. Intra cardiac adrenaline C. Digoxin D. Intra aortic balloon pumping E. Bisoprolol 1210. Hypovolemic shock is seen in all except A. Hemorrhage B. * Starvation C. Vomiting D. Diarrhoea E. Weight loss 1211. 40 % Loss of blood volume in a patient is managed by- A. Vasopressor agents B. Cardiac stimulants C. * Saline infusion D. Intracardiac adrenaline E. Diuretics 1212. In shock all happens except - A. Constriction of capacitance vessels B. Dilation of arterioles C. Decrease in cardiac output D. * Heart rate decreases E. Constriction of venules 1213. Which is not an early manifestation of septicemia- A. Hyperventilation B. * Respiratiory alkalosis C. Confused mentation D. Hypotension E. Hepertension 1214. Dopamine in doses of 5-10 micro gm/kg/min acts on- A. * Beta-1 receptors B. Alpha-1 receptors C. Beta- 2 receptors D. Alpha- 2 receptors E. All receptors 1215. Sepsis syndrome is characterised by all except A. * Normal Pulse B. RR>20 C. Hypotension D. Evidence of clinical infection E. Tachycardia 216. The following are used in septic shock except- A. Adrenaline B. * Nalaxone C. Steriods D. Dopamine E. Noradrenaline 1217. Hypovolemic shock manifests when the percentage of blood loss exceeds A. 10% B. 15% C. 25% D. 30% E. * 40% 1218. Most important step in cardiac resuscitation is - A. Bicarbonate administration B. * Cardiac massage C. Ventilation D. Intracardiac adenaline E. Using the medicamentation 1219. The primary factor in resuscitation of a patient of cardiac arrestis – A. * Cardiac compression B. I.V. fluids C. Adequate airway D. Digitalis E. None of the abvove Acute physiology and Chronic Health Evaluation (APACHE) scoring system is used as a scoring system to 1220. A. To predict postoperative cardiac risk B. To predict postoperative pulmonary complications C. * To evaluate prognosis in the critical care settings D. To evaluate prognosis after acute myocardial infarction E. All of the above 1221. In gram negative septicemia, early findings setting before shock of florid is - A. ^Cardiac output, ^ Total peripheral resistance B. * ^ Cardiac output v Total peripheral resistance C. v Cardiac output, ^ Total peripheral resistance D. vCardiac output, v Total peripheral resistance E. Hypertension and tachycardia 1222. Early sepsis is characterized by a/e – A. Confusion & restlessness B. Bradycardia C. Hypotension D. * Sweating E. Cold extremities 1223. True statements about sepsis and septic shock- A. * It is commonest cause of death in surgical patients. B. Main treatment is - infection site C. Leads to organ dysfunction D. Antibiotic had no role E. Best fluid isNS or RL A 70 year old man develops pneumonia and septicemia. Patient goes into renal failure and has a BP of 70/50 mm of Hg. Drug that should be used to maintain BP is1224. A. Adrenaline B. Ephedrine C. Phenylephrine D. * Norepinephrine E. Noradrenaline 1225. True statements about shock A. * During dehydration both ICF and EC-volume decreases B. 10-20% of fluid loss is compatible to 1ife C. Early change in shock is increased release of noradrenaline D. Risk of death is high when fluid loss is 20-40% E. Hemorrhage cause intravascular fluid loss 1226. In cardiac shock - A. * SBP < 90 mm of Hg B. DBP <80mm of Hg C. Urine output < 20 ml/hr D. Cardiac index <3.5 E. Stroke volume 70 ml 1227. Feature of septic shock is A. * Acute tubular necrosis B. Acute cortical necrosis C. Acute glomerulonephritis D. Acute papillary damage E. Total necrosis A patient in ICU has normal pulmonary A pressure low systemic peripheral resistance; lot cardiac index; arterial P02 = 93; diagnostic possibilities are1228. A. Cardiogenic shock B. Septic shod; C. Hypovolemic shock D. * Cardiac tamponade E. ATN 1229. A patient presented with shock and suspecting it due to hypoglycemia. The treatment should be based on A. * IV glucose after clinical assessment B. Urine sugar C. Blood sugar D. IV access E. All of the above 1230. Which test is not useful in a patient with history of syncopal attack A. Electrophyciological test B. Table tilt test C. * PET scan D. d)Holter monitoring E. Echography 1231. Neurocardiagenic syncope, the least useful investigation is - A. Tilt table B. Carotid sinus massage C. * Carotid duplex scan D. Orthostatic blood pressure recording E. Holter monitoring 1232. A 42 year old presenting with dizziness on standing with systolic reduction of BP of 50 of mm Hg A. * Graded compression stockings B. SIL isoprenaline C. Fludrocortisone D. Oral indomethacine E. Salmeterol A 40 year old presenting with dizziness on standing with systolic reduction of BP of 50 of mm Hg appropriate treatment 1233. A. * Graded compression stockings B. Salbutamol C. Fludrocortisone D. B-blockers E. Diuretics A 42 year old presenting with dizziness on standing with systolic reduction of BP of 50 of mm Hg and HR is 52/man likely cause is 1234. A. B. * C. D. CHF Inferior wall MI Pheochromocytoma Theophylline toxicity E. Sick sinus syndrome, 1235. A patient with DM of 4 yrs duration presents with dizziness and HR 52/min, probable cause is - A. Hypoglycaemia B. Inferior wall MI C. * Sick sinus syndrome D. automatic dysfunction E. Miocardial infarction 1236. Sudden cardiac death may occur in all of the following except A. Dilated cardiomyopathy B. Hypertrophic cardiomyopathy C. Eisenmenger's syndrom D. * Ventricular septal defect E. Restrictive cardiomyopathy 1237. Which of the following is used in resuscitation – A. * Epinephrine B. Oxygen C. Lignocaine D. Magnesium E. Nor-epihephrine 1238. True regarding cardio pulmonary resuscitation is A. Most common presentation in ECG is asystole B. Compression to ventilation ratio is 5:1 C. * Adrenaline is given if cardioversion fails. D. Calcium gluconate is given immediately. E. Glucose is given immediately 1239. In basic life support (BLS), support is given to which of the following organ A. Lung B. * Heart C. Kidney D. Skeletal muscle E. Brain 1240. In cardio pulmonary resuscitation, calcium can be given in all except A. Hypocalcemia B. * Hypokalemia C. Hyperkalemia D. Calcium channel blocker E. Hypercalcemia What would be the first line of treatment is a patient develops ventricular fibrillation after intravenous injection of potassium chloride 1241. A. Cardiac massage B. I. V. Adrenaline C. * Defibrillation D. IPPV E. Intra cardiac adrenaline During cardiopulmonary resuscitation, intravenous calcium gluconate is indicated under all of the following circumstances except1242. A. * After 1 minute of arrest routinely B. Hypocalcemia C. Calcium channel blockers toxicity D. Electromechanical dissociation E. Arrhytmia 1243. Immediate treatment of peripheral circulatory failure in Dengue Shock Syndrome (DSS) is- A. * IV Dextrose Saline B. IV high dose of Dexamethasone C. IV crystalloid infusion D. IV Dopamine + Dobutamine E. IV Adrenaline 1244. Features of shock- A. * DecreasedGFR B. Increasedrenin C. Decreasedrenin D. Decreasedcortisole E. Increase lactate 1245. Serious complication of bacterimic shock ? A. * Causes shock lung B. Decrease peripheral resistance C. Increase cardiac output D. Decrease cardiac output E. Increase peripheral resistence 246. Systemic inflammatory response syndrome (SIRS) includes all of the following, Except – A. Leucocytosis B. Hyperthermia C. Hypothermia D. * Thrombocytopenia E. Leucopenia 1247. Which of the following of drugs is not recommended in septic shock ? A. Normal saline B. ActivatedproteinC C. * Steroids D. Rituximab E. Adrenal hormons 1248. Dengue shock syndrome occurs due to: A. )Super-imposed Bacterial infection B. * Capillary Leak C. Addison's Crisis D. Myocarditis E. Pneumonia 1249. Systemic inflammatory response syndrome is characterised by : A. * Temperature either above 38°C or below 36°C B. Heart rate less than 80/min C. Tachypnoea > 20/min D. Leucocyte count > 4 x 109/L 1250. The most common cause of tricuspid regurgitation A. Rheumatoid heart disease B. * Dilatation of right ventricle C. Coronary artery disease D. Endocarditis due to intravenenous drug abuse E. Dilatation of left ventricle 1251. All can cause recurrent pulmonary infection except- A. VSD B. Recurrent LVF C. * TOF D. ASD E. None 1252. Paessure difference of 5 mm Hg between the two upper limbs occurs in which congenital heart disease- A. TOF B. TGA C. HOCM D. * Supra-valvular aortic stenosis E. Mitral stenosis 1253. All of the following Findings would be expected in a person with coarctation of the aorta except- A systolic murmur across the anterior chest and back and a high-pitched diastolic murmur along the left sternal border A. B. A higher blood pressure in the right arm than in the left arm C. * Inability to augment cardiac output with exercise D. Persistent hypertension despite complete surgical repair E. None A patient presents with headache, intermittent claudication and dizziness. Which of the following may be the underlying cause 1254. A. Tetrology of Fallot B. * Coarctation of aorta C. Patent ductus arteriosus D. Atrial septal defect E. Mitral stenosis 1255. Coarctation of aorta is associated with all, except_ A. Turner's syndrome B. Bicuspid aortic valve C. * Pulmonary stenosis D. Atresia of aortic arch E. Pentade of Fallot 1256. Coarctation of aorta is most commonly associated with A. VSD B. PDA C. * Bicuspid aortic valve D. ASD E. Tetrade of Fallot 1257. Co-arctation of aorta may be associated with all of the following except - A. Bicuspid aortic value B. Turner synd C. * Renal artery stenosis D. PDA E. VSD 1258. All are associated with coarctation of aorta except A. Patent ductus arteriosus B. * Renal artery stenosis C. Bicuspid aortic valve D. Turner's syndrome E. VSD 1259. Rib notching is seen in all except A. Coarctation of aorta B. Classical blalock tausing operation C. * IVC obstruction D. Neurofibromatosis E. Atherosclerosis 1260. MC cause of death in adult with PDA is A. * CCF B. Infective endocardia C. Rupture D. Embolism E. MI 1261. Causes of cynosis A. VSD B. PDA C. * Tricuspid atresia D. Eisenmengers complex E. TGA 1262. Pulmonary flow is decreased in - A. * Fallot's tetralogy B. Ebstein's anomally C. Common atria D. TGV with intact septum E. Mitral stenosis 1263. Treatment of cardiac arrest in systole - A. Cardiac massage B. Intracardiac adrenaline C. IV soda bicorbonate D. * All of the above E. None 1264. Desynchronised defibrillation is used in- A. Atrial fibrillation B. Atrial flutter C. SVT D. * Ventricular fibrillation E. All of the above 1265. The treatment of Grave’s disease usually include A. * Antagonists of thyroid hormones B. Antidepressants C. Narcotic analgesics D. Diuretics E. Sulfonylureas 1266. Minor criteria for infective endocarditis are all of the following EXCEPT: A. Fever >38°C B. Embolic/vascular phenomena C. Immunological phenomena D. * Migratory arthritis E. Blood cultures compatible but not typical for endocarditis 1267. Acute Aortic regurgitation is seen in all the following except: A. * Acute myocardial infarction B. Marfan's syndrome C. Bacterial endocarditis D. Ankylosing spondylitis E. Posttraumatic Aortic aneurism 1268. Acute myocarditis is caused most commonly by: A. * viruses B. bacteria C. fungi D. protozoa E. metazoa 1269. Aggravation of symptoms of angina in a patient when given nitrates is seen in: A. Aortic regurgitation B. Mitral regurgitation C. Single left coronary artery stenosis D. * Idiopathic hypertrophic subaortic stenosis E. Tricuspid regurgitation 1270. All are the true regarding hypertrophic obstructive cardiomyopathy, except: A. * Digitalis is useful B. Left ventricular outflow obstruction C. Asymmetrical septal thickness D. Double apical impulse E. Syncopal episodes 1271. All next are correct about hypertrophic cardiomyopathy, except: A. * Systolic dysfunction B. Concentric hypertrophy C. Left ventricular outflow obstruction D. Double apical impulse E. Murmur is decreased in Valsalva maneuver 1272. All are true about Hypertrophic Obstructive cardiomyopathy, except: A. * agonist are useful B. Asymmetrical hypertrophy of septum C. Dynamic L.V. outflow obstruction D. Condition improves on passive leg raising E. Systolic murmur 1273. All of the following heart sounds occur shortly after S2 except: A. * Ejection click B. Opening snap C. Pericardial knock D. MR E. LVF 1274. All of the following may cause ST segment elevation on ECG, except: A. Early repolarization variant. B. * Constrictive pericarditis. C. Ventricular aneurysm. D. Prizmetal angina. E. Acute myocardial infarction 1275. All of the following murmurs may be heard in patients with aortic regurgitation except: A. * Pansystolic murmur B. Austin flint murmur C. High-pitched decrescendo diastolic murmur. D. Soft, low pitched mid distolic rumbling murmur E. Mid-systolic ejection flow murmur 1276. All patients with acute rheumatic fever should be treated by: A. * intramuscular benzathine penicillin G B. diltiazem C. ergotamine D. heparin E. streptokinase 1277. An early systolic murmur may be caused by all of the following except: A. * Aortic stenosis B. Small ventricular septal defect C. Papillary muscle dysfunction D. Tricuspid regurgitation E. Mitral regurgitation 1278. Angina pectoris and Syncope are most likely to be associated with: A. * Aortic stenosis B. Mitral stenosis C. Mitral regurgitation D. Tricuspid stenosis E. Aortic regurgitation 1279. Aortic regurgitation does NOT occur in : A. * Acute MI B. Marfan' s syndrome C. Rheumatic heart disease D. Infective endocarditis E. Syphilitic aortitis 1280. Auscultative picture of pericardial effusion is: A. * B. Heart sounds tend to become faint Systolic murmur C. Diastolic murmur D. Pericardial friction rub E. Third sound 1281. Austin Flint murmurs is usually mistaken for the murmur of A. * mitral stenosis B. mitral regurgitation C. tricuspid stenosis D. pulmonary regurgitation E. pulmonary stenosis 1282. Cardiac apex double in character. Choose the single most likely diagnosis from the list of options below. A. Mitral stenosis B. Coarctation of aorta C. Aortic stenosis D. * HOCM E. Mitral regurgitation 1283. Cardinal manifestations of many forms of acute pericarditis may be all of the following except: A. pain B. pericardial friction rub C. * migratory polyarthritis D. pericardial effusion with cardiac tamponade E. paradoxic pulse. 1284. Cases of Infectious pericarditis may be all of the following EXCEPT: A. Viral B. Pyogenic C. Tuberculous D. Fungal E. * 1285. Lyme disease Cases of myocarditis may be all of the following EXCEPT: A. Systemic lupus erythematosus B. Viral myocarditis C. Bacterial myocarditis D. Fungal myocarditis E. * 1286. A. * Eosinophilic myocarditis Causative organism in subacute bacterial endocarditis is streptococcus viridians B. staphylococcus aureus C. pneumococcus D. streptococcal pyogenes E. group A streptococcus 1287. Causative organism in acute bacterial endocarditis is A. * staphylococcus aureus B. streptococcus viridians C. pneumococcus D. streptococcal pyogenes E. group A streptococcus 1288. Causes of Chronic Pericardial Effusion are all of the following EXCEPT: A. Myxedema B. SLE C. Rheumatoid arthritis D. Radiation therapy E. * 1289. Viral Chest radiograph findings: egg in cup. Choose the single most likely diagnosis from the list of options below. A. B. * C. Mitral stenosis Constrictive pericarditis Aortic stenosis D. HOCM E. Pericardial effusion Chest radiograph findings: pear-shaped or water bottle appearance. Choose the single most likely diagnosis from the list of options below. 1290. A. Mitral stenosis B. Constrictive pericarditis C. Aortic stenosis D. HOCM E. * Pericardial effusion 1291. Clinical findings in constrictive pericarditis may be all of the following EXCEPT: A. Pulse pressure is normal or reduced B. Edema C. * Acute pulmonary edema D. Distended cervical veins E. Increased abdominal girth 1292. Clues that should lead to the consideration of acute myocarditis include all of these disorders except: A. tachycardia out of proportion to the body temperature in any acute infectious illness B. dyspnea, palpitation, gallop rhythms, or evidence of heart failure during or following an acute viral illness C. D. * new electrocardiograhic or echocardiographic abnormalities following an acute illness electrocardiograhic or echocardiographic abnormalities without any inflammatory process patients with myocardial involvement give a history of a preceding upper respiratory febrile illness or a flulike syndrome, and viral nasopharyngitis isolation of virus from the stool, pharyngeal washings, or other body fluids in patients with myocardial involvement E. 1293. A. * Continuous murmur is seen in all the following except: Peripheral pulmonary stenosis B. Aortic sinus of valsalva rupture C. Coarctation of Aorta D. AV malformations E. PDA 1294. Differential diagnosis of Left atrial myxoma with A. * Mitral stenosis B. Aortic stenosis C. Aortico pulmonary window D. Atrial septal defect E. Mitral regurgitation 1295. Differential diagnosis of mitral stenosis and A. * Left atrial myxoma B. Ebstein anomaly C. Aortico pulmonary window D. Atrial septal defect E. Ventricle septal defect Differential diagnosis of the constrictive pericarditis we should do with all of the following diseases EXCEPT: 1296. A. Tricuspid stenosis B. Cor pulmonale C. * Pericardial effusion D. Cirrhosis of the liver E. Restrictive cardiomyopathy 1297. Dilated cardiomyopathy often producing symptom of: A. * congestive heart failure B. bradycardia C. angina pectoris D. paradoxic pulse E. elevated serum levels of myocardial enzyme. ECG shows prolonged QT, all ST segments elevated and show characteristic saddle shape. Choose the single most likely diagnosis from the list of options below. 1298. A. Pneumonia B. Acute myocarditis C. * Acute pericarditis D. HOCM E. Congestive cardiomyopathy 1299. Echocardiographic findings for infective endocarditis are all of the following EXCEPT: A. * New valvar stenosis B. Mobile echo dense masses attached to valve leaflets or endocardium C. Periannular abscesses D. New dehiscence of a prosthetic valve E. New valvar regurgitation Echocardiography can be used successfully to aid in the diagnosis or management of all the following situations EXCEPT 1300. A. determining left ventricular function after a myocardial infarction B. estimating the mitral valve area in a patient with mitral valve stenosis C. establishing the presence of an atrial septal defect D. * E. excluding the presence of pericarditis assisting with pericardiocentesis Elevated JVP, displaced apex, PSM at the apex and 3rd heart sound. Choose the single most likely diagnosis from the list of options below. 1301. A. * Mitral regurgitation B. Mitral stenosis C. ASD D. Tetralogy of Fallot E. Aortic stenosis Examination of the carotid pulse reveals two impulses or peaks during ventricular systole. Which of the following physical findings probably would be associated with this finding? 1302. A. Diastolic murmur beginning after an opening snap B. Decrease in systolic arterial pressure during inspiration C. * Systolic murmur increasing during the Valsalva maneuver D. Right-sided third heart sound E. Left-sided third sound Examination of the carotid pulse reveals two impulses or peaks during ventricular systole. Choose the single most likely diagnosis from the list of options. 1303. A. Angina pectoris B. Aortic stenosis C. * HOCM D. MI E. Acute pericarditis 1304. Exercise testing is absolutely contraindicated in which one of the following: A. * Aortic stenosis B. One week following myocardial infarction C. Stable angina D. Peripheral vascular disease E. Constrictive pericarditis 1305. Feature that distinguish myocarditis from: rheumatic fever A. * migratory arthritis B. ST-T-wave abnormalities C. Arrhythmias D. heart failure E. tachycardia. 1306. Feature that distinguish rheumatic fever from myocarditis: A. * migratory arthritis B. ST-T-wave abnormalities C. Arrhythmias D. heart failure E. tachycardia. 1307. Feature that distinguishes rheumatic heart diseases from infective endocarditis is: A. * vegetations B. A. Doppler echocardiographic restriction of mitral valve leaflets, their calcification C. pulmonary hypertension D. cardiomegaly E. syncope. 1308. First heart sound is soft in all, except: A. * Short PR interval B. Ventricular septal defect C. Mitral regurgitation D. Calcified valve E. Dilatation of left ventricle 1309. Following is true regarding opening snap: A. * It is a high-pitched diastolic sound. B. It is due to opening of stenosed aortic valve. C. It indicates pulmonary arterial hypertension D. D. It preceedes the aortic component of second heart sound. E. Heard in systola 1310. Graham Steel murmur occurs in: A. * pulmonary regurgitation B. aortic stenosis C. aortic regurgitation D. mitral regurgitation E. tricuspid regurgitation 1311. Haemopericarditis occurs in all of the following conditions except: A. Transmural myocardial infarction. B. Dissecting aneurysm of aorta. C. Metastatic disease of pericardium. D. * Constrictive pericarditis. E. Posttraumatic 1312. Hemoptysis is seen mainly in: A. * mitral stenosis B. aortic stenosis C. pulmonary stenosis D. tricuspid stenosis E. aortic regurgitation 1313. Hoarseness of voice may occur in A. * mitral stenosis B. aortic stenosis C. pulmonary stenosis D. pulmonary regurgitation E. aortic regurgitation 1314. Holosystolic murmur conducted from apex to axilla occurs in A. * mitral regurgitation B. tricuspid regurgitation C. ventricular septal defect D. mitral valve prolapse E. aortic regurgitation 315. Immunological phenomena in infective endocarditis are all of the following EXCEPT: A. glomerular nephritis B. rheumatoid factor C. Osler's nodes D. Roth spots E. * 1316. A. * Erythema marginatum In adults the mitral valve orifice is: 4 to 6 cm2; B. 4 to 5 cm2; C. 2 to 6 cm2; D. 2 to 4 cm2; E. 3 to 5 cm2. 1317. A. * In aortic regurgitation the left ventricle is: dilated B. hypertrophic C. small D. atrophic E. normal 1318. In chronic constrictive pericarditis EchoCG changes are all of the following EXCEPT: A. The ventricular end-diastolic and stroke volumes are reduced B. The end-diastolic pressures in both ventricles are elevated C. The mean pressure in the atria is elevated, D. The mean pressures in pulmonic veins is elevated E. * 1319. A. * The left ventricle chamber is dilated In rheumatic heart disease, embolism is commonly caused by tight mitral stenosis with atrial fibrillation B. aortic stenosis with sinus tachycardia C. tricuspid regurgitation D. atrial septal defect E. aortic regurgitation 1320. In severe aortic stenosis true finding is: A. * ST segment changes in ECG B. Loud S2 C. Loud S1 D. Late systolic ejection clicks E. Heaving with outward apex Interventions that may all cause an increase in the gradient and the murmur in patients with hypertrophic cardiomyopathy are following except: 1321. A. * diltiazem B. Exercise C. tachycardia D. digitalis glycosides E. sudden standing. Jerky carotid pulse, dominant 'a' wave in the JVP, double apical impulse ejections systolic murmur at the left sternal border. Choose the single most likely diagnosis from the list of options below. 1322. A. Mitral stenosis B. ASD C. Aortic stenosis HOCM D. * E. Mitral regurgitation 1323. Kussmaul's sign is seen rare in A. Restrictive cardiomyopathy B. Constrictive pericarditis Cardiac tamponade C. * D. RV infarct E. A and B Low serum complement levels would be seen in patients with hematuria, proteinuria, and hypertension resulting from all of the following EXCEPT 1324. Henoch-Schonlein purpura A. * B. diffuse proliferative lupus nephritis C. hepatitis C-associated membranoproliferative glomerulonephritis D. streptococcal infective endocarditis glomerulonephritis E. rheumatism F. . 1325. LV dilatation is commonly seen with : A. * Pure mitral stenosis B. ASD with fossa-ovalis C. Aortic incompetance D. Carcinoid syndrome E. Pulmonary stenosis 1326. Main syndrome in acute pericarditis is: A. Heart failure, B. * Chest pain, C. Arrythmias D. Inflammation E. Hemoptysis 1327. Main syndrome in cardiomyopathy is: A. Heart failure, B. * Syncope, C. Arrythmias D. Inflammation E. Hemoptysis 1328. Main syndrome in dilated cardiomyopathy is: A. * Heart failure, B. Chest pain, C. Arrythmias D. Inflammation E. Hemoptysis 1329. Main syndrome in dilated cardiomyopathy is: A. Heart failure, B. * Angina, C. Arrythmias D. Inflammation E. Hemoptysis 1330. Major criteria of rheumatic fever are the following EXCEPT: A. * Recent group A streptococcal infection B. Carditis C. Migratory polyarthritis D. Sydenham's chorea E. Erythema marginatum 1331. Migrating polyarthritis is characteristically seen in A. * rhematic arthritis B. syphilitic arthritis C. rheumatoid arthritis D. psoriatic arthritis E. gouty arthritis 1332. Migratory polyarthritis in rheumatic fever most often affecting following joints except: A. * small joints of hands B. the ankles C. wrists D. knees E. elbows 1333. Minor criteria for infective endocarditis are all of the following EXCEPT: A. * Migratory arthritis B. Fever >38°C C. Embolic/vascular phenomena D. Immunological phenomena E. Blood cultures compatible but not typical for endocarditis 1334. Minor Criterion of rheumatic fever is: A. * Prolonged P-Q interval B. sinus tachycardia C. sinus bradycardia D. inversion of T waves E. ectopic beats 1335. Mitral stenosis is associated with: A. * B. Left ventricular hypertrophy Right ventricular hypertrophy C. Left axis deviation D. Changed QRS complex E. Left ventricular dilatation 1336. Noncardiac Manifestations of infective endocarditis are the following except: A. * a rash on the trunk and proximal extremities B. splenomegaly C. petechiae D. arterial emboli E. Osler's nodes On auscultation a patient is noted to have a rumbling diastolic murmur at the apex. The murmur is accentuated during exercise. Choose the single most likely diagnosis from the list of options below. 1337. A. * Mitral Stenosis B. Aortic stenosis C. Tricuspid Regurgitation D. Mitral Regurgitation E. Aortic Regurgitation 1338. Opening of the aortic valve is initiated by A. * when ventricular pressure is more than aortic pressure B. contraction of atria C. contraction of ventricles D. none of the above E. all of them 1339. Pain is often absent in all of the following pericarditis EXCEPT: A. slowly developing tuberculous pericarditis B. postirradiation pericarditis C. neoplastic pericarditis D. uremic pericarditis E. * acute pericarditis 1340. A. * Paradoxical splitting of S2 is seen in: all of the above B. aortic stenosis C. severe hypertension D. coarctation of aorta E. left bundle branch block Patints with acute rheumatic fever in initial attack have evidence of carditis, which may be characterized by all are the following EXCEPT: 1341. A. * the first heart sound is accentuated B. sinus tachycardia C. the murmur of mitral regurgitation D. an S3 gallop E. cardiomegaly Patients with acute rheumatic fever in initial attack have evidence of carditis, which may be characterized by all are the following except: 1342. A. * the first heart sound is generally accentuated B. sinus tachycardia C. the murmur of mitral regurgitation D. an S3 gallop E. cardiomegaly Patients with acute rheumatic fever in initial attack have evidence of carditis, which may be characterized by all are the following EXCEPT: 1343. A. sinus tachycardia B. the murmur of mitral regurgitation C. an S3 gallop D. * the first heart sound is accentuated E. cardiomegaly 1344. Propranolol should be given very cautiously to managed the patients with myocarditis associated with: A. palpitation B. tachycardia C. * congestive heart failure D. arrythmias E. chest pain 1345. Rheumatic fever caused by: A. * beta-hemolytic streptococci. B. Staphylococcus lugdunensis C. Enterococci D. The HACEK group E. H. influenza 1346. S4 is not seen in : A. * Ventricular aneurysm B. Acute Mitral regurgitation C. Hypertrophic cardiomyopathy D. Hypertension E. Aortic stenosis 347. Select the proper symptom of consequence of the rheumatic fever from the following: A. * Mitral stenosis B. Isolated lesion of the aortic valve. C. Frequent affections of the liver. D. Splenomegaly. E. Haemorrhagic diathesis. 1348. Severity of mitral stenosis is assessed by: A. * Length of murmur B. Loud opening snap C. Loud S1 D. Splitting S2 E. Accentuated P2 Slow rising pulse and undisplaced apex, which is heaving in character. There ESM heard best at the right intercostal space that does not radiate. Choose the single most likely diagnosis from the list of options 1349. below. A. * Aortic stenosis B. Aortic regurgitation C. Mitral valve prolapse D. Mitral Stenosis E. Mitral Regurgitation Slow rising pulse, prominent left ventricular impulse, ejection systolic murmur and fourth heart sound. Choose the single most likely diagnosis from the list of options below. 1350. A. * Aortic stenosis B. Tricuspid stenosis C. Aortic regurgitation D. Mitral stenosis E. Tricuspid regurgitation 1351. Soft, single second heart sound (S2) is heard in A. * Aortic regurgitation B. Mitral stenosis C. Mitral regurgitation D. Tricuspid regurgitation E. Tricuspid stenosis 1352. ST elevation is seen in all of the following conditions except: A. Acute myocardial infarction B. Coronary artery spasm C. * Constrictive pericarditis D. Ventricular aneurysm E. Acute pericarditis 1353. Typical therapy of dilated cardiomyopathy with severe heart failure includes all of the following except: A. salt restriction B. angiotensin-converting enzyme (ACE) inhibitors C. * calcium antagonists D. diuretics E. digitalis. 1354. Standard therapy of heart failure in dilated myocardiopathy includes all of the following EXCEPT: A. Salt restriction B. Angiotensin-converting enzyme (ACE) inhibitors C. * Calcium channel blockers D. Diuretics E. Digitalis 1355. Sudden death may be seen in A. * aortic stenosis B. mitral stenosis C. mitral regurgitation D. aortic regurgitation E. tricuspid regurgitation 1356. Supporting evidence of a recent group A streptococcal infection may be all of the following except: A. * recent malar rash B. A. elevated or increasing streptococcal antibody test - antistreptolysin- O (ASO) C. positive throat culture D. recent scarlatine E. all mentioned above 357. Systolic blood pressure that is 20 mm Hg higher in the leg than in the arm (Hill’s sign) A. * Aortic regurgitation B. Aortic stenosis C. Mitral stenosis D. Mitral regurgitation E. Tricuspid regurgitation The 19-year-old patient presents with tachypnea and syncopal episode. Echocardiography of the heart showed normal cardiac morphology with asymmetric septal hypertrophy. Which of the following you will give to treat this patient: 1358. A. Digoxin B. Frusemide C. * Propranolol D. Isoptin E. Molsidomin 1359. The diagnosis of constrictive pericarditis is supported by which of the following findings? A. * Neck vein distension that increases during inspiration B. Exaggerated first and second heart sound (S1 and S2) C. Unequal diastolic pressure in the four chambers of the heart D. A predominance of the lef-sided signs and symptoms over right-sided findings E. Inspiratory chest pain 1360. The diagnosis of constrictive pericarditis is supported by which of the following findings? the signs and symptoms of heart failure are out of proportion to the degree of systolic dysfunction or valvular heart disease A. * B. Exaggerated first and/or second heart sound (S1 and S2) C. Unequal diastolic pressure in the four chambers of the heart D. A predominance of the lef-sided signs and symptoms over right-sided findings E. Inspiratory chest pain 1361. The first heart sound (S1) is generally accentuated and snapping in: A. * mitral stenosis B. mitral regurgitation; C. aortic regurgitation; D. aortic stenosis E. coarctation of the aorta. 1362. The most frequent type of arrhythmia in patient with mitral stenosis: A. * atrial fibrillation B. extrasystole supraventricular C. extrasystole ventricular D. WPW-syndrome E. CLC-syndrome 1363. The most important ECG sign of acute pericarditis is: A. * Widespread elevation of the ST segments B. Significant changes in QRS complexes C. Arrhythmias D. AV heart blocks E. Loss of R-wave amplitude 1364. The most important physical sign of acute pericarditis is: A. * Pericardial friction rub B. Thachycardia C. Hypotension D. Cardiomegaly E. Systolic murmur 1365. The most sensitive method to confirm valve diseases is A. * Echo B. ESG C. X-Ray D. auscultation E. laboratorian tests 1366. The murmur of hypertrophic obstructive cardiomyopathy is decreased in which of the following: A. * Supine position B. Standing position C. Valsalva maneuver D. Amylnitrate inhalation E. Exercise The pathophysiology of mitral valve stenosis involves which of the following hemodynamic abnormalities? 1367. A. * Increased left atrial pressure B. Increased left ventricular filling C. Increased forward cardiac output D. Decreased right ventricular pressure E. Pulsus alternans The pulse is regular and jerky in character. The cardiac impulse is hyperdynamic and not displaced. There is a midsystolic murmur with no ejection click loudest at the left sternal edge. Choose the single most likely diagnosis from the list of options below. 1368. A. Myocardial ischaemia B. Left ventricular aneurysm C. Aortic stenosis D. * HOCM E. Aortic sclerosis 1369. The S1 is soft, or buried in the systolic murmur in: A. * mitral regurgitation; B. A. increased influence of sympatic nervous system; C. mitral stenosis D. aortic regurgitation; E. aortic stenosis 1370. The severity of mitral regurgitation is decided by: A. * all of the above B. Presence of mid- diastolic murmur across mitral valve. C. Wide split second heart sound. D. Presence of left ventricular S3 gallop. E. Grade III/VI intensity systolic murmur across mitral valve The systolic ejection murmur in hypertrophic obstructive cardiomyopathy is diminished when a patient does which of the following? 1371. A. B. * Perform the Valsava maneuver Lies down C. Inhales amyl nitrite D. Stands up E. -adrenergic agonists There is soft late systolic murmur at the apex radiating to the axilla. Choose the single most likely diagnosis from the list of options below. 1372. A. * Mitral valve prolapse B. Aortic regurgitation C. Tricuspid Regurgitation D. Aortic stenosis E. Mitral Regurgitation 1373. Third heart sound (S3, or ventricular gallop) is auscultated in A. * Mitral regurgitation B. Mitral stenosis C. Tricuspid regurgitation D. Aortic stenosis E. Aortic regurgitation 1374. Third heart sound is seen in all except: A. * Mitral stenosis B. Athletes C. Constrictive pericarditis D. LVF E. MR 1375. True statements regarding the effect of alcohol on the heart include which of the following? A. Chronic ingestion of alcohol will lead to a restrictive cardiomyopathy Once heart failure develops, discontinuing the consumption of alcohol will not appreciably affect the natural history of the disease B. C. D. * If thiamine deficiency is present in an alcoholic, high output failure is noted If a patient with heart failure caused by ethanol continues to drink, he or she is unlikely to be alive in 3 years E. The most common arrhythmia associated with a drinking binge is ventricular tachycardia 1376. Vegetations on undersurface of A.V. valves are found in: A. * Limban Sack's endocarditis B. Acute Rheumatic corditis C. Non thrombotic bacterial endocarditis D. Chronic rheumatic carditis E. MVP Which group of drugs has a significant role in the treatment of the patients with severe carditis accompanied by congestive heart failure: 1377. A. * steroids B. salicylates C. cefazolin D. erythromycin E. heparin 1378. Which investigation can detect vegetations in approximately 90% of patients with proven endocarditis: A. * Transoesophageal echocardiogram B. Echocardiogram C. ECG D. CT E. Chest X-ray 1379. What investigation can detect vegetations in approximately 90% of patients with proven endocarditis: A. * Transoesophageal echocardiogram B. Echocardiogram C. ECG D. CT E. Chest X-ray 1380. What is duration of the antibiotic treatment of the patients with acute rheumatic fever? A. * not less then two weeks B. not less then 20 days C. not less then a week D. not less then 5 days E. not less then a month 1381. When pericardial friction rub can be elicited? when firm pressure with the diaphragm of the stethoscope is applied to the chest wall with a patient sitting up A. when firm pressure with the diaphragm of the stethoscope is applied to the chest wall with a patient leaning forward B. * when firm pressure with the diaphragm of the stethoscope is applied to the chest wall with a patient lying supine C. when firm pressure with the diaphragm of the stethoscope is applied to the chest wall at the left lower sternal border. D. when firm pressure with the diaphragm of the stethoscope is applied to the chest wall with a patient lying on the right side. E. 1382. A. * Which cardiac valve is most frequently affected as a result of rheumatic fever? Mitral B. Aortic C. Tricuspid D. Pulmonic E. Mitral and Pulmonic 1383. Which chamber of the heart suffers firstly in mitral regurgitation? A. * left atrium B. left ventricle C. right ventricle D. right atrium E. left and right atria 1384. Which investigation can detect vegetations in approximately 90% of patients with proven endocarditis: A. * Transoesophageal echocardiogram B. Echocardiogram C. ECG D. CT E. Chest X-ray 1385. Which of following electrocardiogram changes acute pericarditis often produces? A. * widespread elevation of the ST segments with reciprocal depressions only in aVR B. Q waves C. loss of R-wave amplitude D. elevation of the ST segments with reciprocal depression of ST segments E. changes in QRS complexes 1386. Which of the following are immune complex lesions in SBE A. * Osler’s nodes B. mycotic aneurysms C. anemia D. vegetations E. meningitis 1387. Which of the following patients with severe chronic MR is not a surgical candidate? A. * NYHA functional class I, EF 70%, LV end systolic diameter 35 mm B. NYHA functional class III, EF 40% C. NYHA functional class II, EF 50% D. NYHA functional class II, EF 70%, LV end systolic diameter 42 mm E. NYHA functional class III, EF 40% and NYHA functional class II, EF 1388. Which of the following are accepted indications for surgery in patients with severe chronic AR? A. * NYHA class III or greater B. LVEF C. LV end-diastolic diameter > 65 mm D. LV end-systolic diameter > 45 mm E. Bicuspid aortic valve with ascending aortic diameter of 40 mm 1389. Which of the following EchoCG changes is found in restrictive cardiomyopathy? A. Left ventricular dilatation B. Left ventricular diastolic dysfunction C. * D. Increased left ventricular wall thickness Asymmetric septal hypertrophy E. Systolic anterior motion (SAM) of the mitral valve 1390. Which of the following EchoCG changes is found in hypertrophic cardiomyopathy? A. Left ventricular dilatation B. Left ventricular diastolic dysfunction C. Increased left ventricular wall thickness D. Symmetric septal hypertrophy E. * 1391. A. * Systolic anterior motion (SAM) of the mitral valve Which of the following findings noted during physical examination is a sign of severe aortic stenosis? A delayed carotid upstroke B. A harsh, late-peaking holosystolic murmur C. A loud aortic component (A2) of the second heart sound (S2) D. A diastolic rumble E. An opening snap 1392. Which of the following haemodynamic indices is decisive in the diagnosis of mitral stenosis: A. * Gradient between pressure in the left atrium and diastolic pressure in the left ventricle. B. Pressure in the pulmonary artery. C. Pressure in the left atrium. D. E. Gradient between pressure in the left ventricle and pressure in the aorta. Pressure in the right_atrium. Which of the following investigation can’t help to distinguish constrictive pericarditis and cirrhosis of the liver? 1393. A. Distended neck veins B. Chest roentgenography C. chest CT D. * EchoCG E. ChestMRI 1394. Which of the following is the most common late manifestation of acute rheumatic fever? A. * B. Chorea Pharyngitis C. Erythema marginatum D. Iritis E. Enthesopathy 1395. Which of the following is not one of the major Jones criteria for the diagnosis of rheumatic fever? A. * Urethritis B. Carditis C. Arthritis D. Chorea E. Erythema marginatum 1396. Which of the following physical signs is seen in a patient with severe aortic stenosis: A. * Delayed peak of systolic murmur B. Opening snap C. Diastolic rumble D. Holosystolic murmur E. Loud S2 1397. Which of the following sings is more prominent in constrictive pericarditis? A. Edema B. * Ascites C. Pulmonary edema D. Hypertension E. Thromboembolism 1398. Which of the following statements best characterized tricuspid regurgitation? A. * Infective endocarditis is a common cause B. The murmur heard in tricuspid regurgitation decreases with inspiration C. Large a waves in jugular venous pulse are characteristic D. Correction of coexistent left ventricular failure rarely improves the condition E. Cardiac catheterization is required for the diagnosis 1399. Which of the following statements best characterizes the physical signs noted in aortic regurgitation? A. * The presence of an Austin Flint murmur indicates moderate-to-severe insufficiency A large increase in stroke volume occurs when the condition is acute, producing many of the physical signs present in this disease B. C. Concentric left atrium hypertrophy is the major compensatory mechanism D. A low-pitched, diastolic blowing murmur is heard best when the patient is lying down E. Corrigan’s pulse is elicited best in the femoral artery 1400. Which of the following usually causes irreversible dilated cardiomyopathy? A. Endocrinopathies (e. g., thyrotoxicosis) B. Metabolic disorders (e.g. hypophosphatemia) C. Prolonged ethanol abuse D. * High-dose doxorubicin therapy E. Aspirin overdose 1401. Which of the following would be most likely in a patient with chronic severe MR? A. * Third heart sound B. Normal LV cavity size C. Dyspnea D. EF>65% E. RV lift 1402. Which one of the following is the most common cause for 'Restrictive cardiomyopathy'? A. Alcohol B. Hemochromatosis C. * Amyloidosis D. Sarcoidosis E. IHD One worker in the surgical center is found to be culture-positive for streptococcal microorganisms in his nasal mucosa but has no symptoms of infection. What is this patient's status in the chain of infection? 1403. A. * Reservoir B. Portal of entry C. Portal of exit D. Susceptible host E. Non of above 1404. 1nvestigaion of choice to distinguish between COPD with emphysema and bronchial asthma is : A. * Allergy test to pollens B. Methacholine provocatin test C. Chest X-ray D. Arterial blood gas analysis E. All of the above 1405. A criterion for the diagnosis of asthma is: A. * 15 %reversibility in spirography B. 5% reversibility in spirography C. 10% reversibility in spirography D. X-ray changes E. Sputum changes A middle-aged smoker presents with chronic cough and phlegm. His sputum is tenacious but not yellow or blood stained. His chest is hyperinflated. His arterial carbon dioxide is high and is arterial oxygen is low. What changes may be founded on spyrogram? 1406. A. * FEV1, FVC, Typhno index are low B. FEV1, FVC, Typhno index are high C. FEV1, FVC, Typhno index are normal D. FEV1, FVC are high, Typhno index is low E. FEV1, FVC are low, Typhno index is high A middle-aged smoker presents with chronic cough and phlegm. His sputum is tenacious but not yellow or blood stained. His chest is hyperinflated. His arterial carbon dioxide is high and is arterial oxygen is low. What is the previous diagnosis? 1407. A. * Emphysema B. Bronchitis C. Bronchogenic carcinoma D. Pneumonia E. Respiratory failure A patient who is 2 days postoperative from a bowel resection tells her physician that she is having a hard time “catching her breath,” feels nauseated, and has chest pains when she inhales. The physician suspects that she is having a pulmonary embolism. What intervention should the physician perform before notifying the physician? 1408. A. B. * Increase the IV flow rate. Apply oxygen by mask or nasal cannula at 5 L/min. C. Assess the chest and axillary area for the presence of petechiae. D. Place the patient in shock position, with her head and neck flat and her legs elevated. E. Non of above A young woman complains of wheeze, dyspnoea and cough. She cannot sleep at night because of a chronic cough. She and her mother love animals and together they have 14 cats. Her PEFR is normal but her CXR suggests hyperinflation. What is the previous diagnosis? 1409. A. * Bronchial asthma B. Bronchogenic carcinoma C. Emphysema D. Respiratory failure E. Bronchitis According recommendations of WHO daily dose of inhaled glucocortisteroids in the case of mild persistant bronchial asthma is: 1410. A. * 200-500 mkg B. 150-300 mkg C. 800-2000 mkg D. More than 2000 mkg E. Glucocorticosteroids are not recommended After emotional exertion patient of 24 received condition with dyspnea and prolonged expiration, distantional wheezes, frequent night symptoms. All that limited his physical activity. PEV and FEV1 < 60 %, daily variability -30 %. What diagnosis is possible? 1411. A. * Severe persistent bronchial asthma B. Mild persistent bronchial asthma C. Persistent bronchial asthma of moderate severity D. Intermittent bronchial asthma E. Bronchospastic syndrome of allergic origin 1412. A. * All are decreased in infiltrative lung disease, except: Alveolar arterial difference in PaO2 B. Vital capacity C. Total lung capacity D. Lung compliance E. Nothing of the above 1413. All are true in definition of chronic bronchitis except: A. * Haemoptysis B. Cough for 2 months C. Productive cough D. More than 2 consecutive months E. All of the above 1414. All are used in bronchial asthma, except: A. * Morphine B. Salbutamol C. Aminophylline D. Steroid E. All of the above 1415. All of the following are useful for treating acute bronchial asthma in children except : A. * Sodium chromoglycate inhalation B. 100% Oxygen C. Hydrocortisone infusion D. IV aminophylline E. All of the above 1416. All of the following drugs useful in the treatment of a patient with acute bronchial asthma except A. * Montelukast B. Ipratropium C. Salbutamol D. Hydrocortisone E. All of the above 1417. All of the following features are seen in the viral pneumonia except: A. Presence of interstitial inflammation. B. * Predominance of alveolar exudates. C. Bronchiolitis. D. Multinucleate giant cells in the bronchiolar wall. E. All features are present All of the following statements about Leukotriene modifiers in the management of bronchial asthma are true except. 1418. A. * May be used for acute asthma B. May be used for exercise induced asthma C. Zileuton is Leukotriene modifier D. May uncover Churg strauss syndrome E. All of the above 1419. All show wide alveolar-arterial O2 gradient except A. * Central hypoventilation B. Bronchiectasis C. ARDS (acute respiratory distress syndrome ) D. Interstitial fibrosis E. Nothing of the above 1420. All the following are causes of hemorrhagic pleural effusion except : A. * Pancreatitis B. Pulmonary embolism C. Rheumatoid arthritis D. TB E. Nothing of the above 1421. All the following are true about Chronic Obstructive lung disease except: A. * Decreased diffusion capacity B. Decreased FeV1 C. Decreased MEFR D. Increased RV E. Nothing of the above 1422. All the following lung volumes can be measured by a simple spirometer except : A. * Residual volume B. Vital capacity C. Tidal volume D. Forced vital capacity E. Nothing of the above 1423. Alveolar -arterial tension gradient increases in all except : A. * Hypoventilation B. Diffusion defects C. R-L shunt D. Ventilation perfusion abnormality E. All of the above 1424. Alveolar -arterial tension gradient increases in all except : A. * Hypoventilation B. Diffusion defects C. R-L shunt D. Ventilation perfusion abnormality E. Nothing of the above 1425. Aspirin sensitive asthma is associated with : A. * Nasal polyps B. Extrinsic asthma C. Urticaria D. Obesity E. All of the above 1426. A. * Aspirin-sensitive asthma is associated with: Nasal polyp B. Obesity C. Urticaria D. Extrinsic asthma E. Nothing of the above 1427. Asthma is precipitated by all except: A. * Gold B. Aspirin C. Alcohol D. Suxamethonium E. Nothing of the above 1428. Attack of bronchial asthma differs from heart asthma by such sign A. * By expiration dyspnea B. By sudden development of attack C. By orthostatic position of the patient D. By duration of the attack E. By inspiration dyspnea 1429. Best position to reveal small pleural effusions on chest X-ray is A. * Lateral decubitus view B. AP view C. PA view D. Lateral view E. All of the above 1430. Bilateral clubbing may be seen in all except : A. * Chronic bronchitis B. Bronchiectasis C. PBS D. Fibrosing alveolitis E. All of the above 1431. Bilateral malignant pleural effusion is most often seen in : A. * CA -lung B. Ca breast C. Mesothelioma D. Lymphoma E. Nothing of the above 1432. Bilateral pleural effusion is seen in : A. * All of the above B. Nephritic syndrome C. Constrictive pericarditis D. Congestive cardiac failure E. Nothing of the above 1433. Blocking these can worsen the asthma A. * Beta 2 receptors B. Alpha receptors C. Mast cells D. Neutrophils E. Eosinophils 1434. Bronchial Asthma is associated with raised levels of A. * Leukotrienes B. Thromboxane C. PGI 2 D. PGI 1 E. All of the above 1435. Bronchial asthma patient on artificial ventilation requires : A. * B. An IE ratio 1: 2.5 A low inspiratory flow C. An equal IE ratio of 1:1 D. An inverese ratio ventilation E. Nothing of the above 1436. Bronchial asthma, is associated with raised levels of : A. * Leukotriens B. PGI2 C. PGlj D. Thromboxane E. All of the above 1437. Bronchiectasis is most common in which lobe : A. * Left lower lobe B. Right upper lobe C. Right middle lobe D. Left upper lobe E. All of the above 1438. Bronchodylation activity is specific for A. * Berotec B. Anuzol C. Inderal D. Paracetamol E. Azafen 1439. Carbon monoxide diffusion capacity decreases in all, except: A. * Alveolar haemorrhage B. Emphysema C. Primary pulmonary hypertension D. Infiltrative lung disease E. Nothing of the above 1440. Causes of haemorrhagic pleural effusion are all except: A. * Bronchial adenoma B. Pulmonary infarction C. Mesothelioma D. Tuberculosis E. Nothing of the above 1441. Choice of drug by inhalation in acute asthma not responding to salbutamol is : A. * Inpratropium bromide B. Atropine sulfate C. Isopropamide D. Hyoscine methyl bromide E. All of the above 1442. Complication of bronchiectasis are all except : A. * Bronchiogenic carcinoma B. Cerebral abscess C. Lung abscess D. Amyloidosis E. All of the above Consider the following statement : Early onset extrinsic episodic asthma is characterized by: 1. Family history of eczema or rhinitis 2. Development of an early and late asthmatic reaction mediated by mast cells 3. T lymphocytes that release cytokine like interleukin-4 Which of these statements are correct ? 1443. A. * 1,2 and 3 B. 1 and 2 C. 2 and 3 D. 1 and 3 E. Nothing of the above Consider the following statements : Life threatening features of acute - severe asthma in children include : (1) Altered sensorium (2) Pulsus paradoxus (3) Audible wheeze in both inspiration and expiration (4) Oxygen saturation 92-95% Which of these statements is/are correct ? 1444. A. * B. 1 and 2 1 only C. 2 and 4 D. 1, 2, 3 and 4 E. Nothing of the above 1445. Contraindication for glucocorticosteroid therapy of bronchial asthma is A. * Bleeding from gastric ulcer B. Chronic persistant hepatitis C. Exacerbation of respiratory-heart failure D. Emphysema of lungs E. Respiratory failure 1446. Curschmann's crystals are seen in A. * Bronchial asthma B. Bronchiectasis C. Chronic bronchitis D. Wegners Granulomatosis E. All of the above 1447. Curschmann's spirals in sputum is seen in A. * Bronchial asthma B. Bronchiectasis C. Chronic bronchitis D. Wegners Granulomatosis E. All of the above 1448. Curshmann's spirals in sputum is seen in : A. * Asthma B. Tuberculosis cavity C. Bronchitis D. Bronchiectasis E. All of the above 1449. Cyanosis is seen if : A. * All of the above B. Meth HB 1.5 gm % C. SulfHB0.5gm% D. Reduced HB 5 gm % E. Nothing of the above 1450. Decreased maximum mid-expiratory flow rate indicates obstruction in: A. * Small airways B. Trachea C. Large airways D. Trachea & Bronchi both E. Nothing of the above 1451. Drug of choice in asthma with heart disease is A. * Ipratropium B. Rimiterol C. Terbutaline D. Cromolyn sodium E. All of the above 1452. Exercise induced asthma is not precipitated by : A. * Swimming in hot water B. High altitude climb and exercises C. Cycling in cold weather D. Swimming in cold water E. All of the above 1453. False about COPD is : A. * Decreased diffusion capacity B. Decreased FEV1 C. Decreased midexpiratory peaks flow rate D. Increased residual capacity E. Nothing of the above 1454. A. * Features of restrictive lung disease is: FEVj/FVC increases and compliance decreases B. FEV1/FVC decreases and compliance decreases C. FEV1/FVC increases and compliance increases D. FEV 1/FVC decreases and compliance increases E. Nothing of the above 1455. FEV,/FVC is reduced in case of: A. * Asthma B. Pleural effusion C. Lung fibrosis D. All of the above E. Nothing of the above 1456. FEV,/FVC is reduced in case of: A. * COPD B. Pleural effusion C. Lung fibrosis D. All of the above E. Nothing of the above 1457. FEV1 ratio is decreased in all except : A. * Interstitial lung disease B. Bronchiectasis C. Emphysema D. Chronic bronchitis E. Nothing of the above 1458. Following are ture of acute bronchial asthma except A. * Inpratropium bromide B. Atropine sulfate C. Isopropamide D. Hyoscine methyl bromide E. All of the above 1459. For diagnosis of obstructive airway disease which of the following measurement is usual A. * Timed vital capacity B. Vital capacity C. Tidal volume D. Blood gas analysis E. All of the above For the patient who has sustained tracheobronchial trauma, which assessment finding alerts the physician to the possibility of tracheal lacerations? 1460. A. B. * Hypertympanic sound on affected side Subcutaneous emphysema over the trachea C. Hypotension and decreased capillary refill D. Deviation of the trachea to the affected side E. Non of above 1461. Found more commonly in spirography of patients with bronchial asthma A. * FEV1, FVC, Typhno index are low B. FEV1, FVC, Typhno index are high C. FEV1, FVC, Typhno index are normal D. FEV1, FVC are high, Typhno index is low E. FEV1, FVC are low, Typhno index is high 1462. Found more commonly in sputum of patients with asthma A. * Eosinophils B. T cells C. Mast cells D. Neutrophils E. IgM General medical contraindications to admittance on the work related to the dangerous harmful substances and harmful industrial factors, are the following, except: 1463. A. B. * Chronic diseases of lungs with the evident pulmonary-cardiac insufficiency. essential hypertension of II stage C. Bronchial asthma of severe form with the evident disturbance of breathing and circulation of blood. D. Active forms of tuberculosis of any localization. E. Stomach and duodenal ulcer with chronic recurrent course and susceptibility to complications. 1464. Hemoptysis is an important symptoms in all except: A. * Alpha Antitrypsin deficiency B. Idiopathic hemosiderosis C. Bronchial Adenoma D. Pulmonary T.B. E. All of the above 1465. High oxygen tension in alveoli is due to : A. * Ventilation perfusion mismatch B. Right to left shunt C. Inappropriate gas exchange D. Bronchial asthma E. All of the above 1466. How does antibiotic therapy increase the risk for infection? Most intravenous antibiotics contain high concentrations of glucose, providing an ideal medium for bacterial proliferation. A. B. C. * The associated diarrhea causes ulcerations to form in the intestinal tract, creating a new portal of entry. Antibiotic therapy also kills off normal flora, which provide a means of protection from infection. D. The resulting dead bacteria provide a rich culture medium for viruses. E. Non of above 1467. How does prostacyclin therapy reduce the pathologic problems of primary pulmonary hypertension? A. * Increasing lung blood flow by dilating pulmonary blood vessels B. Improving ventilation by increasing the contractility of the diaphragm C. Increasing gas exchange by changing the elasticity of the alveolar D. Protecting the heart from development of cor pulmonale by increasing cardiac muscle strength E. Non of above 1468. How does the drug oseltamivir (Tamiflu) prevent influenza or shorten the duration of illness? A. * Preventing the virus from entering respiratory cells B. Boosting the patient’s immune system C. Inhibiting the virus from multiplying D. Directly killing the virus E. Non of above 1469. How long is the usual course of drug treatment for a patient with active tuberculosis (TB)? A. 7 to 10 days B. 6 weeks C. * 6 months D. 2 years E. Non of above 1470. How many stages of severity of bronchial asthma do you know? A. * 4 B. 1 C. 2 D. 3 E. There are no stages of severity 1471. Hypercapnea at rest is most indicative of A. * Hypoventilation B. Right to left shunt C. Impaired diffusion D. CO poisoning E. All of the above 1472. If.FEV, is 1.3 lit. FVC is 3.1 lit. in an adult man the pattern is suggestive of A. * B. Obstructive lung disease Normal lung function C. Restrictive lung disease D. None of the above E. All of the above 1473. In bronchial asthma glucocorticoids A. * Reduce airway inflammation B. Act as potent bronchodilators C. Inhibit degranulation of mast cells D. Block the action of humoral mediators E. Nothing of the above 1474. In chronic obstructive disease following pulmonary function abnormalities are present except: A. * Decreased diffusing capacity B. Decreased FEV1 C. Decreased maximum expiratory flow rate D. Increased residual volume E. Nothing of the above 1475. In chronic obstructive pulmonary disease all are seen EXCEPT A. * Increased FEV/VC ratio B. LowFEV C. Smoking strongly associated D. Partially reversible by bronchodilator therapy E. Nothing of the above 1476. In COPD following pulmonary function abnormalities are present except : A. * Diffusing capacity decreased B. FEV1 decreased C. maximum expiratory flow rates decreased D. Residual volume increased E. All of the above In patient K. 21 years old was diagnosed persistent bronchial asthma. Prophylaxis of attacks of dyspnea can be provided with: 1477. A. * Beclomethasoni B. Theophillin C. Nedokromili sodium D. Antihystaminic medicines E. Atrovent 1478. In restrictive lung disease : A. * FEV/FVC is high B. FVC is high C. FEV1 is high D. All of the above E. Nothing of the above 1479. In severe bronchial asthma, true is : A. * Hyperresonant chest with prolonged expiration B. Infrequent rhonchi and absent breath sounds C. Increased fremitus and D. Decreased fremitus and crackles E. All of the above 1480. In the time of attack of bronchial asthma in lungs are heard A. * Dry soundings wheezes B. Moist soundings wheezes C. Moist soundless wheezes D. Voice of pleural friction E. Dry and moist wheezes 1481. In what specific way does the respiratory system function contribute to acid-base balance? A. Prevents excessive loss of hydrogen ions by evaporation B. Increases the potassium ion content in bronchial secretions C. * D. Removes carbon dioxide generated as a result of metabolism Maintains body water levels through mucous membrane function E. Non of above 1482. In which patient with chronic airflow limitation would you expect to find dependent edema? A. 25-year-old with cold-induced asthma B. 65-year-old with exercise-induced asthma C. * 55- year-old with chronic bronchitis D. 45-year-old with moderate emphysema E. Non of above 1483. It is necessary to diagnose bronchial asthma A. * To notice the asthmatic attack of dyspnea B. To find allergic antibodies C. To find the presence of expiration dyspnea D. To find the presence of signs of obstructive respiratory failure E. To find the presence of eosinophylia in blood 1484. Lung involvement in chronic bronchitis is : A. * Bilateral B. Segmental C. Lobar D. Unilateral E. All of the above Moderate decreasing of FVC and FEV1/FVC, significant – of FEV1 is the sign of such type of respiratory failure: 1485. A. * Obstructive B. Restrictive C. Mixed D. Diffuse E. Indexes are normal 1486. Normal mean Reid index is : A. * 0.44 B. 0.22 C. 0.35 D. 0.6 E. All of the above 1487. Obstructive type of insufficiency of pulmonary ventilation is caused by: A. * Narrowing of bronchi B. Decreasing of diaphragm mobility C. Arrising of pleuritis D. Decreasing of breathing muscles strength E. Violences of ptrfusion 1488. Ominous sign in bronchial asthma is : A. * B. C. * Accessory muscles functioning Tachypnea Increased wheezing and and crepts D. Feeble breath sounds and absent wheezing E. All of the above 1489. One of the following condition is not associated with clubbing. A. * Chronic bronchitis B. Primary biliary cirrhosis C. Cryptogenic fibrosing alveolitis D. Central bronchiectasis E. Nothing of the above 1490. One of the following is not an indicator of the severity of asthma : A. * Systolic hypertension B. Use of accessory muscles C. Pulsus paradoxus D. Cyanosis E. All of the above 1491. One of the patient's coexisting medical problems? A. Asthma Alveoli B. Hypotension Larynx C. Kidney stones Pharynx D. * Urinary retention Airways E. Non of above 1492. Patient with bronchiectasis may give a past history of: A. * Whooping cough B. Chickenpox C. Mumps D. Typhoid E. Nothing of the above 1493. Patient with mild persistent bronchial asthma received exacerbation. Your recommendations? A. * B. To increase dose of inhaled glucocorticosteroid, ? -2-agonist of short action To increase dose of ? -2-agonist of short action, do not change dose of inhaled glucocorticosteroid To provide test with dronchodylator, and then to increase dose of inhaled glucocorticosteroid and ? -2-agonist C. To provide provocational test with hystamin, and then to increase the dose of inhaled glucocorticosteroid and ? -2-agonist D. To increase dose of inhaled glucocorticosteroid, ? -2-agonist, and then to provide provocational test with hystamin E. Patient`s diagnosis is “bronchial asthma, persistant of moderate severity”. What medicine would you give advantage for the planned treatment of disease? 1494. A. * Budesonid-forte B. Intal C. Euphyllini orally D. Salbutamol E. Berotec 1495. Poor prognostic indicators in acute severe asthma include all of the following EXCEPT A. * B. PEFR less than 20% of previous value Pulsus paradoxus C. Hypocarbia D. Use of accessory muscles of respiration E. Nothing of the above 1496. Pulmonary surfactant is secreted by: A. Type I pneumocytes. B. * Type II pneumocytes. C. Clara cells. D. Bronchial epithelial cells. E. Tracheal epithelial cells. 1497. Restrictive lung disease is associated with : A. * Interstitial lung disease B. High residual lung volume C. High PCO2 D. FEV1 below 50 % E. Nothing of the above 1498. Silent chest is seen in A. * Very severe asthma B. Chronic bronchitis C. Emphysema D. Bronchiectasis E. All of the above 1499. Silicatosis is: A. * Asbestosis B. Siderosis C. Aluminosis D. Bisinosis E. All of the above 1500. Spirals of Kurshman in patients with bronchial asthma may be founded during laboratory research of: A. * Sputum B. Urine C. Biopsy of pulmonary tissue D. Gastric juice E. Pleural exudates 501. Steroid inhalation side effect include: A. * Oropharyngeal candidiasis B. Cushing's syndrome C. Sedation D. None of the above E. Nothing of the above 1502. Steroid inhalation side effect include: A. * Oropharyngeal candidiasis B. Cushing's syndrome C. Sedation D. None of the above E. All of the above Study the results of the pulmonary functions tests shown below : Parameters Actual Predicted FEV,(L) 1.2 3.5-4.3 FVC (L) 4.1 4.6-5.4 FEV,FVC(%) 29 72-80 PEF (L/min) 80 440-540 These result are consistent with the disease of : 1503. A. * Chronic bronchitis B. Interstitial lung disease C. Pneumonia D. Pneumothorax E. Nothing of the above 1504. Swan - Ganz catheter is used to measure : A. * Pulmonary capillary pressure B. Right atrial flow C. Central venous pressure D. Right ventricular pressure E. Nothing of the above 1505. The complication least likely to occur in a case of chronic bronchitis is : A. * Amyloidosis B. Pulmonary hypertension C. Pneumothorax D. Emphysema E. All of the above 1506. The FEV1 is the volume of: A. * air forcefully expired during the first second after a full breath and normally comprises > 75% of the VC B. B) air normally expired during the first second after a full breath and normally comprises > 75% of the VC. C. C) air forcefully expired during the first minute after a full breath and normally comprises > 75% of the VC D. D) air normally expired during the first minute after a full breath and normally comprises > 75% of the VC. E) air forcefully expired during the second minute after a full breath and normally comprises > 75% of the VC. E. 1507. A. * The following are acceptable as normal result : PO2 100 mm Hg B. V/Q ratio : 1.0 C. Resting tidal ventilation 10 L/mm D. FEV, : 60% of vital capacity E. Nothing of the above 1508. The hall mark of generalised obstructive lung disease is A. * Reduced timed vital capacity B. Reduced tidal volume C. Reduced residual volume D. Reduced vital capacity E. All of the above 1509. A. * The major sign of hypoventilation is Сyanosis B. Hypoxia C. Hypercapnia D. Dyspnea E. All of the above 1510. The most common cause of lowering of lower lungs borders is: A. * Pulmonary emphysema B. Bronchial asthma C. Chronic pulmonary artery hypertension D. Pneumothorax E. Enteroptosis 1511. The most frequent cause of peripheral cyanosis is: A. * Slowed circulation through the skin B. Interatrial septal defect C. Methaemoglobinaemia D. Interstitial pulmonary fibrosis E. Nothing of the above The most predictive and dangerous side effect of propranolol that makes it to be avoided in known patient of COPD is induction of : 1512. A. * Acute asthmatic attack B. Respiratory failure C. Glaucoma D. Pleural effusion E. All of the above 1513. The severity of COPD and the potential for response to bronchodilator can be adequately assessed by: A. * B. simple spirometry (± flow-volume loop) before and after inhalation of bronchodilator, X-ray examination C. bronchscopy D. simple spirometry (± flow-volume loop) after inhalation of bronchodilator, E. nothing mentioned. 1514. The substance released by the mast cell activation and causes bronchospasm. A. * Histamine B. Leukotrienes C. IgM D. IgG E. IgE 1515. True about chronic obstructive lung disease are all except : A. * Decreases total lung capacity B. Decrease vital capacity C. FEV,/FVC D. Increased residual volume E. Nothing of the above 1516. Tubular breathing is seen in : A. * Consolidation B. Pleural effusion C. Pleurisy D. Tuberculous cavity E. All of the above 1517. Use of disodium cromoglycate as a preventive measure has been found to be of value in : A. * Exercise induced asthma B. Pneumonia C. Chronic bronchitis D. Fanner's lung E. Nothing of the above 1518. Ventilation/perfusion ratio is highest in : A. * Apex of lung B. Mid zone C. Lower zone D. Hilum E. Nothing of the above 1519. Volume of air taken into the lungs in normal respiration is known as : A. * Tidal volume B. Vital capacity C. Timed vital capacity D. Inspiratory reserve volume E. All of the above 1520. WBC 11,500; Hct 57%; Hgb 22 g/dL; serum sodium 139 mEq/L A. Dehydration is present as a result of rapid, shallow breathing. B. * Polycythemia is present as a result of compensation for hypoxemia. C. Septicemia is present as a result of bronchitis and possible pneumonia. D. Cor pulmonale is present as a result of increased pulmonary vascular resistance. E. Non of above What is necessary to make during periodic medical examination to all workers, who contact with occupational dust? 1521. A. Common blood analyses B. Biochemical analyses C. ECG D. Ultrasound examination E. * 1522. A. * Roentgenography of chest organs What is not specific for severe persistant bronchial asthma? Severe vomiting B. Long duration of attacks C. Development of status asthmaticus D. Development of acute heart failure E. Necessarity of usage of glucocorticosteroids 1523. What is the main purpose of a negative-pressure ventilator? A. Healing diseased lung tissue B. Relieving hypoxemia by opening obstructed airways C. * Assisting ventilation to healthy lungs by mimicking normal chest pressures D. Delivering an individualized preset tidal volume to the lower respiratory tract E. Non of above 1524. What is the major difference in pathophysiology between asthma and COPD? A. Asthma is a restrictive disorder and COPD is an obstructive disorder. COPD results in permanent airflow obstruction and asthma is a condition of reversible airflow obstruction. B. * COPD is caused by chronic exposure to inhalation irritants and the major cause of asthma is cigarette smoking. C. Asthma is the result of an inflammatory process and COPD is a result of inflammatory, infectious, and hyperresponsiveness processes. D. E. Non of above 1525. What is the mechanism of reduced gas exchange in a patient who has atelectasis? A. Airway obstruction B. * Reduced alveolar surface area C. Failure of pulmonary circulation to fully perfuse lung tissue D. Increased bronchial secretions filling the alveoli with fluid rather than with air E. Non of above 1526. What is the most important intervention for the patient with acute respiratory distress syndrome? A. Antibiotic therapy B. Bronchodilators C. * Oxygen therapy D. Diuretic therapy E. Non of above 1527. What is the physiologic consequences of CO2 narcosis? A. Excessive sleepiness in the patient with hypercarbia B. * Failure of rising blood levels of CO2 to trigger more rapid and deeper respirations C. A change in the ventilation-perfusion ratio, in which ventilation exceeds perfusion D. Increase in the percentage of oxygen delivered to the patient does not result in an increasedPaO2 E. Non of above 1528. What is the primary cause for the increased incidence in lung cancer among women during the past 20 years? A. B. * C. Women now have a longer life expectancy than men. Cigarette smoking among women increased dramatically 50 years ago. More women now work in the industrial setting than in previous decades. Increased use of oral contraceptives combined with air pollution has driven the incidence of lung cancer up in women. D. E. Non of above 529. What is the role of surfactant in pulmonary function? A. * Reduces alveolar surface tension, improving gas exchange B. Increases alveolar surface tension, improving gas exchange C. Dilates pulmonary blood vessels, decreasing pulmonary vascular resistance D. Relaxes bronchial smooth muscle, decreasing pulmonary vascular resistance E. Non of above 1530. What medicine does have bronchodilatory activity? A. * Berotec B. Panzinorm C. Inderal D. Atropin E. Paracetamol 1531. What part of the pulmonary system is most affected by asthma? A. Alveoli B. Larynx C. Pharynx D. * Airways E. Non of above Which assessment finding in a patient who has been medicated during an asthma attack indicates to you that the therapy should be modified? 1532. A. Peak expiratory rate flow 10% below expected value B. Presence of bilateral tactile fremitus C. * Suprasternal retraction on inhalation D. Trachea at the midline E. Non of above Which assessment finding in a patient with severe dyspnea indicates to you that the respiratory problem is chronic? 1533. A. Wheezing on exhalation B. Productive cough C. * Clubbed fingers D. Cyanosis E. Non of above 534. Which assessment finding should you expect in the patient with COPD? A. * Decreased vocal fremitus B. Grossly bloody sputum C. Loss of the gag reflex D. Tracheal deviation E. Non of above 1535. Which beta 2 agonist is not given for acute bronchial asthma ? A. * Salmeterol B. Salbutamol C. Terbutaline D. Methyl xanthine E. All of the above 1536. Which blood gas value indicates that the patient is experiencing hypercarbia? A. pH = 7.33 B. C. * Bicarbonate = 20 mEq/L PaCO2 = 60 mm Hg D. PaO2 = 80 mm Hg E. Non of above 1537. Which clinical change indicates the patient's COPD is becoming worse? A. Pulse pressure has increased from 35 mm HG to 40 mm Hg,Alveoli B. * The patient has had an unplanned weight loss of 15 pounds. C. The patient's average respiratory rate has decreased from 34 to 33. D. The patient's PaCO2 is 58 mm Hg this month compared with 64 mm Hg last month. E. Non of above Which clinical manifestation alerts you to the presence of hypoventilation when you are monitoring a patient with chronic lung disease and hypercarbia who is receiving oxygen therapy? 1538. A. B. * Coarse crackles and wheezes on auscultation Slow, shallow respirations C. Pulse oximetry of 90% D. Clubbing of the fingers E. Non of above Which clinical manifestation in a patient with chronic bronchitis indicates to you a worsening of the patient's respiratory condition? 1539. A. Fatigue B. Cachexia C. * Confusion D. Slow capillary refill E. Non of above Which clinical manifestation in a patient with long-standing COPD alerts you to the possibility of cor pulmonale? 540. A. Pursed-lip breathing occurs when the patient is at rest. B. The patient's neck muscles are enlarged and prominent. C. The patient's ECG shows tall, peaked T waves and an absent U wave. D. * Jugular venous distention is present when the patient is in a sitting position. E. Non of above Which clinical manifestation in an older patient with pneumonia indicates that the disease is responding to the therapeutic regimen? 1541. A. The patient does not have a cough. B. Urine output is 900 mL for the day. C. * Pulse oximetry shows an oxygen saturation of 90%. D. Tactile fremitus is increased over the affected lung fields. E. Non of above 1542. Which complication is most frequent in patients with silicosis? A. Tromboembolia of pulmonary artery. B. Bronchial asthma. C. Pneumonia. D. Cancer of lungs. E. * Tuberculosis. 1543. Which diagnostic indicator confirms the presence of active tuberculosis? A. Positive PPD test B. The presence of calcified lesions on chest x-ray C. * The presence of M. tuberculosis in a sputum culture The combined clinical manifestations of weight loss, night sweats, fever, and cough productive of mucopurulent bloody sputum D. E. Non of above 1544. Which disorder is an example of a "restrictive" pulmonary disease? A. Asthma B. Bronchitis C. Lung cancer D. * Pulmonary fibrosis E. Non of above 1545. Which drug is more commonly used as therapy for COPD than as therapy for asthma? A. Theophylline (Theo-Dur) B. C. * Montelukast (Singulair) Guaifenesin (Organidin) D. Salmeterol (Serevent) E. Non of above 1546. Which laboratory value indicates to you that the patient may have allergic asthma? A. * Eosinophil count of 1200 cells/mm3 (13%) B. Total white blood cell count of 9080 cells/mm3 (100%) C. Total absence of macrophages in the differential white blood cell count D. Band neutrophil count of 2880 cells/mm3 (32%) and a segmented neutrophil count of 1980 cells/mm3 (22%) E. Non of above Which manifestations in a patient receiving oxygen therapy at 60% for more than 24 hours alerts you to the possibility of oxygen toxicity? 1547. A. * Increased dyspnea B. Decreased rate and depth of respiration C. Wheezing on inhalation and exhalation D. Increased excretion of thick, white, frothy sputum E. Non of above 1548. Which of the following patients could be expected to require mechanical ventilation longterm? A. 27-year-old with status asthmaticus B. 45-year-old with morphine overdose C. * 24-year-old with muscular dystrophy D. 65-year-old with bilateral bacterial pneumonia E. Non of above 1549. Which patient is a greatest risk for contracting SARS? A. * The 30-year-old physician providing direct care to patients with SARS B. The 50-year-old farmer working directly with cows and pigs C. The 60-year-old patient with type 2 diabetes mellitus and renal insufficiency D. The 70-year-old patient residing in an assisted living environment E. Non of above 11550. Which patient is a greatest risk for developing nosocomial pneumonia? A. * The 60-year-old patient receiving mechanical ventilation B. The 40-year-old patient receiving antibiotics for a surgical wound infection C. The 60-year-old patient in traction for a fractured femur who also has a cold D. The 40-year-old patient with type 2 diabetes who has a 50 pack-year smoking history E. Non of above 1551. Which patient is at greatest risk for acute respiratory distress syndrome? A. The 62-year-old with COPD who has pneumonia B. * The 22-year-old who received 10 units of blood after a motor vehicle crash C. The 78-year-old with chronic congestive heart failure and pulmonary edema D. The 24-year-old with asthma who has not taken any of her asthma medications for 2 weeks E. Non of above 1552. Which patient is at greatest risk for developing a “community-acquired” pneumonia? A. The 40-year-old first-grade teacher B. * The 60-year-old smoker who is also an alcoholic C. The 75-year-old with exercise-induced wheezing D. The 35-year-old aerobics instructor who skips meals and eats only vegetables E. Non of above Which patient should the physician caution to avoid taking over-the-counter decongestants for manifestations of a cold or flu? 1553. A. B. * 25-year-old man with a latex allergy 45-year-old woman with hypertension C. 32-year-old woman who is taking oral contraceptives D. 65-year-old man who has had type 1 diabetes mellitus for 20 years E. Non of above 1554. Which set of arterial blood gas values indicates early pneumonia as the respiratory problem? A. * B. pH 7.35, HCO3– 22 mEq/L, PCO2 45 mm Hg, PO2 86 mm Hg pH 7.30, HCO3– 22 mEq/L, PCO2 60 mm Hg, PO2 92 mm Hg C. pH 7.32, HCO3– 17 mEq/L, PCO2 25 mm Hg, PO2 98 mm Hg D. pH 7.30, HCO3– 28 mEq/L, PCO2 65 mm Hg, PO2 75 mm Hg E. Non of above Which set of arterial blood gases would the physician expect to find in a patient who developed a pulmonary embolism 15 minutes ago? 1555. A. pH 7.30, HCO3– 22 mEq/L, PCO2 60 mm Hg, PO2 66 mm Hg B. pH 7.38, HCO3– 22 mEq/L, PCO2 45 mm Hg, PO2 96 mm Hg C. * pH 7.47, HCO3– 23 mEq/L, PCO2 25 mm Hg, PO2 82 mm Hg D. pH 7.30, HCO3– 28 mEq/L, PCO2 65 mm Hg, PO2 75 mm Hg E. Non of above Which set of arterial blood gases would the physician expect to find in a patient who developed a pulmonary embolism 6 hours ago? 1556. A. * pH 7.30, HCO3– 22 mEq/L, PCO2 60 mm Hg, PO2 66 mm Hg B. pH 7.38, HCO3– 22 mEq/L, PCO2 45 mm Hg, PO2 96 mm Hg C. pH 7.47, HCO3– 23 mEq/L, PCO2 25 mm Hg, PO2 82 mm Hg D. pH 7.30, HCO3– 28 mEq/L, PCO2 65 mm Hg, PO2 75 mm Hg E. Non of above 1557. Which type of acid-base imbalance is most common among patients with COPD? A. * Respiratory acidosis B. Respiratory alkalosis C. Metabolic acidosis D. Metabolic alkalosis E. Non of above 1558. With which of the following theophylline has an antagonistic interaction? A. Histamine receptors. B. Bradykinin receptors. C. * Adenosine receptors. D. Imidazoline receptors. E. Beta-adrenoreceptors Your patient with asthma is receiving aminophylline intravenously. Which manifestation alerts you to the possibility of aminophylline toxicity? 1559. A. B. * Pulse oximetry of 93% Increased restlessness C. Hourly urine output of 45 mL D. Heart rate increase from 72 to 84 beats per minute E. Non of above 1560. ?1- Antitrypsin deficiency is associated with : A. * Panaciner-emphysema B. Centriaciner emphysema C. Irregular emphysema D. Paraseptal-emphysema E. All of the above A typical list of blood tests used for the initial assessment of liver cirrhosis includes measuring all of the following except of: 1561. A. * Urea. B. Aminotransferases. C. Gamma-glutamyl transferase. D. Autoantibodies. E. Alpha 1-antitrypsin. 1562. All of the following diagnostic tests is useful to be performed in patient with jaundice except of: A. * Creatinin. B. Blood serum bilirubin. C. Complete blood analysis. D. Liver biopsy. E. Liver function tests and cholesterol. 1563. All of the following diagnostic tests is useful to be performed in patient with jaundice except of: A. * Blood serum bilirubin. B. Complete blood analysis. C. Prothrombin time. D. Ultrasound of the abdomen. E. Urine and fecal urobilinogen. 1564. All of the following functions of the liver are carried out by the hepatocytes except of: A. Amino acid synthesis. B. Gluconeogenesis. C. Glycogenolysis. D. Glycogenesis. E. * Production of rennin. 1565. All of the following functions of the liver are carried out by the hepatocytes except of: A. * Production of renin. B. Protein metabolism. C. Cholesterol synthesis. D. Production of triglycerides. E. Production of coagulation factors. 1566. Antimitochondrial antibody test is characteristic feature of: A. * Primary biliary cirrhosis. B. Sclerosing cholangitis. C. Anaerobic liver abscess. D. Hepatoma. E. Hepatitis C. 1567. Autoimmune hepatitis is characterized by: A. * Increased IgG level, a positive anti-smooth-muscle antibodies - 60%. B. It is most aggressive when it is presented in the first and second decades. C. It is more common in men than in women. D. All mentioned. E. No one mentioned. 1568. Causes of cirrhosis and/or chronic liver disease are in all of the following cases except of: A. * Viral hepatitis A. B. Autoimmune. C. Viral hepatitis C. D. Viral Hepatitis B. E. Viral Hepatitis B with hepatitis D. 1569. Causes of cirrhosis and/or chronic liver disease are in all of the following cases except of: A. * Viral hepatitis E. B. Autoimmune. C. Viral hepatitis C. D. Viral Hepatitis B. E. Viral Hepatitis B with hepatitis D. 1570. Causes of liver cirrhosis are in all of the following cases except of: A. * Viral hepatitis A. B. Autoimmune. C. Viral hepatitis C. D. Viral Hepatitis B. E. Alcoholic liver disease. 1571. Causes of liver cirrhosis are in all of the following cases except of: A. * Viral hepatitis A. B. Primary biliary cirrhosis. C. Viral hepatitis C. D. Non-alcoholic steatohepatitis. E. Alcoholic liver disease. Chronic active hepatitis is most definetly distinguished from chronic persistent hepatitis by the presence of: 1572. A. * Characteristic liver histology. B. Hepatitis B surface antigen in the serum. C. Antibody to hepatitis B core antigen in the serum. D. A significant titer of anti-smooth-muscle antibody. E. Extrahepatic manifestations. 1573. Chronic hepatitis is characterized by following clinical syndrome: A. Cholestatic. B. Hepatomegaly. C. Dyspeptic. D. * All mentioned. E. No one mentioned. 1574. Chronic hepatitis is generally defined as disease that lasts for: A. * 6 months or longer. B. 1 months. C. 2 months. D. 2,5 months. E. 3 months. 1575. Chronic hepatitis is not characterized by following clinical syndrome: A. * Portal hypertension. B. Cholestatic. C. Hepatomegaly. D. Dyspeptic. E. Hypochondriac pain. 1576. Complications of liver cirrhosis are are in all of the following cases except of: A. * Hyperuricemia. B. Bruising and bleeding. C. Jaundice due to decreased processing of bilirubin. D. Itching (pruritus). E. Hepatic encephalopathy. 1577. Complications of liver cirrhosis are in all of the following cases except of: A. * Hyperuricemia. B. Bruising and bleeding. C. Jaundice due to decreased processing of bilirubin. D. Itching (pruritus). E. Esophageal varices. 1578. Drug-induced chronic hepatitis can not be caused by: A. * Silymarin. B. Paracetamol. C. Isoniazid. D. Oestrogens. E. Antibiotics. 1579. Drug-induced chronic hepatitis can be caused by: A. Paracetamol. B. Isoniazid. C. Oestrogens. D. Antibiotics. E. * All mentioned. 1580. Primary biliary cirrhosis is the most closely associated with such circulating antibodies: A. * Antibodies to mitochondrium. B. Anantibodies to phospholipidis. C. Antibodies to native DNA. D. Antibodies to smooth muscle cells. E. Antibodies to parietal cells. 1581. Gall bladder stone formation in caused by all factors except of: A. * Leucocytosis. B. Hyperalimentation. C. Primary biliary cirrhosis. D. Clofibrate therapy. E. None of mentioned. 1582. Hemochromatosis is characterized by all of the following clinical manifestations except of: A. * Gout. B. Liver cirrhosis. C. Diabetes mellitus. D. Gonadotropin deficiency. E. Cardiomyopathology. 1583. Hemochromatosis is characterized by: A. * Excessive deposition of iron in the liver. B. Excessive deposition of copper in liver. C. Transforms into cirrhosis and emphysema. D. No one mentioned. E. All mentioned. 1584. Hepatic jaundice causes all of the following diseases except of: A. * Ductal carcinoma. B. Acute hepatitis. C. Hepatotoxicity. D. Alcoholic liver disease. E. Primary biliary cirrhosis. 1585. Hepatic encephalopathy may be aggravated by all of the following factors except of: A. * Hyperkalemia. B. Barbiturates. C. Alkalosis. D. Hypoxia. E. Hyponatraemia. 1586. In patients with acute liver failure the most important prognostic indicator is: A. * Factor V estimation. B. Serum alpha fetoprotein. C. Serum bilirubin. D. Serum albumin. E. Level of GGT. 1587. In which cases in patient with fatty liver steatosis the microvesicular fat is seen due to biopsy? A. * Acute fatty liver steatosis of pregnancy. B. Hemochromatosis. C. Total parenteral nutrition. D. Prolonged intravenous hyperalimentation. E. Carbon tetrachloride poisoning. 1588. In which of the following cases jaundice isn’t of hepatic origin: A. * Ductal carcinoma. B. Acute hepatitis. C. Hepatotoxicity. D. Alcoholic liver disease. E. Primary biliary cirrhosis. 1589. Absorbtion in digestive system of arsenic metal causes: A. * Non cirrhotic portal fibrosis. B. Hepatic adenoma. C. Hepatic carcinoma. D. Hepatic cirrhosis. E. No one mentioned. 1590. Jaundice, alkaline phosphatase elevation, pale stool are signs of: A. * Pancreatic carcinoma. B. Hemolysis secondary to G6PD deficiency. C. Acute viral hepatitis. D. Crigler-Najjar syndrome. E. Gilbert syndrome. Liver biopsy shows an inflammatory, obliterative process in intrahepatic and extrahepatic bilious ducts. What is the most probable disease? 1591. A. * Sclerosing cholangitis. B. Primary biliary cirrhosis. C. Anaerobic liver abscess. D. Hepatoma. E. Hepatitis C. Liver biopsy shows Mallory's hyaline and collagen deposition. Choose the most probable diagnosis from the list of the options: 1592. A. * Alcoholic hepatitis. B. Leptospirosis. C. Primary biliary cirrhosis. D. Gallstones. E. Hepatitis B associated with the primary hepatocellular carcinoma. 1593. Liver cirrhosis is characterized by following clinical syndrome: A. Cholestatic. B. Hepatomegaly. C. Hemorrhagic syndrome. D. Dyspeptic. E. * All mentioned. 1594. Liver is involved in development of such following systemic diseases except of: A. * Ischemic hepatitis. B. Sarcoidosis. C. Amyloidosis. D. Celiac disease. E. Tuberculosis. 1595. Many patients with Budd-Chiari syndrome often have such complication: A. * Paroxysmal night hemoglobinuria. B. Hepatocellular carcinoma. C. Right ventricular failure. D. Renal cell carcinoma. E. Pneumonia. 1596. Many patients with Budd-Chiari syndrome often have such complication: A. * Polycythemia vera. B. Hepatocellular carcinoma. C. Right ventricular failure. D. Renal cell carcinoma. E. Pneumonia. 1597. Marker of cholestatic syndrome in patient with hepatitis is: A. * Increased alkaline phosphatase. B. Decreased fibrinogen. C. Increased AST. D. Increased ALT. E. All of above. 1598. Marker of cholestatic syndrome in patient with hepatitis is: A. * Increased ALT. B. Increased alkaline phosphatase. C. Increased cholesterol. D. Decreased fibrinogen. E. All of mentioned. 1599. Marker of liver cellular insufficiency syndrome in patient with hepatitis is: A. * Decreased albumine. B. Increased ALT. C. Increased GGT. D. Increased bilirubin. E. Increased AST. 1600. Markers of cholestatic syndrome in patient with hepatitis are all of the following except of: A. * Increased ALT. B. Increased cholesterol. C. Increased bilirubin. D. Increased alkaline phosphatase. E. Increased GGT . 1601. Markers of cholestatic syndrome in patient with hepatitis are all of the following except of: A. Increased cholesterol. B. Increased bilirubin. C. Increased alkaline phosphatase. D. Increased GGT. E. * All mentioned. 1602. Markers of cholestatic syndrome in patient with liver disease are: A. * Increased bilirubin, increased alkaline phosphatase, increased GGT, increased cholesterol. B. Increased AST, increased ALT, increased GGT, increased bilirubin. C. Decreased albumine, decreased prothrombin, decreased cholesterol, decreased fibrinogen. D. Increased ESR, increased Y-globulins, increased timol test, increased Le, increased C-react. protein. E. None of mentioned. 1603. Markers of cytolitic syndrome in patient with hepatitis are: A. Increased ALT . B. Increased GGT . C. Increased bilirubin. D. Increased AST . E. * All mentioned. 1604. Markers of cytolitic syndrome in patient with hepatitis are all except of: A. * Increased alkaline phosphatase. B. Increased ALT. C. Increased GGT. D. Increased bilirubin. E. Increased AST. 1605. Markers of cytolitic syndrome in patient with liver disease are: A. * Increased AST, increased ALT, increased GGT, increased bilirubin. B. Increased .ilirubin, increased alkaline phosphatase, increased GGT, increased cholesterol. C. Decreased albumine, decreased prothrombin, decreased cholesterol, decreased fibrinogen. D. Increased ESR, increased Y-globulins, increased timol test increased Le, increased C-react. protein. E. No one mentioned. 606. Markers of hypersplenism syndrome in patient with liver cirrhosis are all of the following except of: A. * Leukocytosis, increased ESR. B. Thrombocytopenia. C. Anemia+ thrombocytopenia. D. Anemia+ thrombocytopenia +leukocytopenia. E. Anemia+ increased ESR. 1607. Markers of hypersplenism syndrome in a patient with liver cirrhosis are: A. * Anemia, thrombocytopenia, leukocytopenia. B. Increased AST, increased ALT, increased GGT, increased bilirubin. C. Increased bilirubin, increased alkaline phosphatase, increased GGT, increased cholesterol. D. Decreased albumine, decreased prothrombin, decreased cholesterol, decreased fibrinogen. E. No one mentioned. 1608. Markers of hypersplenism syndrome in a patient with liver cirrhosis are: A. Anemia. B. Thrombocytopenia. C. Leukocytopenia. D. No one mentioned. E. * All mentioned. 1609. Markers of liver cellular insufficiency syndrome in patient with liver cirrhosis are: A. * Decreased albumine, decreased prothrombin, decreased cholesterol, decreased fibrinogen. B. Increased AST, increased ALT, increased GGT, increased bilirubin. C. Increased bilirubin, increased alkaline phosphatase, increased GGT, increased cholesterol. D. Increased ESR, increased Y-globulins, increased timol test increased Le, increased C-react. protein. E. No one mentioned. 1610. Markers of liver cellular insufficiency syndrome in patient with hepatitis are: A. Decreased albumine. B. Decreased cholesterol. C. Decreased prothrombin. D. Decreased fibrinogen. E. * All mentioned. 1611. Markers of mesenchyme-inflammatory syndrome in patient with liver cirrhosis are: A. * Increased ESR, increased Y-globulins, increased timol test increased Le, increased C-react. protein. B. Increased AST, increased ALT, increased GGT, increased bilirubin. C. Increased bilirubin, increased alkaline phosphatase, increased GGT, increased cholesterol. D. Decreased albumine, decreased prothrombin, decreased cholesterol, decreased fibrinogen. E. No one mentioned. 1612. Findings of Mallory hyaline characterizes such pathology as: A. * Alcoholic hepatitis. B. Autoimmune hepatitis. C. Cryptogenic hepatitis. D. Chronic viral hepatitis B. E. Chronic viral hepatitis C. 1613. Peptic ulcer should be differentiated with: A. Cholecystitis. B. Gastritis. C. Miocardial infarction. D. Pancreatitis. E. * All mentioned Pruritus, elevation of alkaline phosphatase and positive antimitochondrial antibody test are characteristic signs of: 1614. A. * Primary biliary cirrhosis. B. Sclerosing cholangitis. C. Anaerobic liver abscess. D. Hepatoma. E. Hemochromatosis. 1615. Risk factor of Budd-Chiari syndrome is: A. * Hormonal contraception. B. Hepatocellular carcinoma. C. Right ventricular failure. D. Renal cell carcinoma. E. Pneumonia. 1616. Signs of liver cirrhosis are all of the following except of: A. * Erythema nodosum. B. Spider angiomata. C. Palmar erythema. D. Nail changes. E. Hypertrophic osteoarthropathy. 1617. The stage of chronic hepatitis is determined due to all following features except of: A. * No fibrosis. B. Fibrosis and necrosis. C. Necrosis. D. Moderate fibrosis. E. Acute fibrosis including bridging fibrosis. 1618. There following diagnostic tests for establishing diagnosis of chronic hepatitis B are except of: A. * HDV RNA. B. IgG anti-HBc. C. HbeAg. D. HBV DNA. E. HbsAg. What disease may be in patient with a long history of ulcerative colitis and with recently developed jaundice, pruritus and pain in the right upper part of abdomen? 1619. A. * Primary biliary cirrhosis. B. Sclerosing cholangitis. C. Anaerobic liver abscess. D. Hepatitis C. E. Hemochromatosis. What disease may be in patient with a long history of ulcerative colitis and with recently developed jaundice, pruritus and pain in the right upper part of abdomen? 1620. A. * Sclerosing cholangitis. B. Primary biliary cirrhosis. C. Hepatitis C. D. Hepatitis D. E. Hemochromatosis. What disease may be in patient with a long history of ulcerative colitis and with recently developed jaundice, pruritus and pain in the right upper part of abdomen? 1621. A. * Sclerosing cholangitis. B. Hepatoma. C. Hepatitis C. D. Hepatitis D. E. Hemochromatosis. F. Hepatitis D. What disease may be in patient with a long history of ulcerative colitis and with recently developed jaundice, pruritus and pain in the right upper part of abdomen? 1622. A. * Sclerosing cholangitis. B. Primary biliary cirrhosis. C. Hepatoma. D. Hepatitis C. E. Hemochromatosis. 1623. What is not true about autoimmune hepatitis: A. * It is more common in men than in women. B. It can be associated with other autoimmune diseases. C. There is a rise of IgG, a positive anti-smooth-muscle antibody is present in 60% of patients. D. Antinuclear antibody and liver-kidney microsomal antibody (LKM-1) may be present. E. Response on corticosteroids therapy consists 70-90%. What is the most probable diagnosis in patient whith decreased serum albumin and ascitic fluid albumin - 1.4 g/dL? 1624. A. * Portal hypertension. B. Pancreatitis. C. Tuberculous peritonitis. D. Hepatoma. E. Ascitis. 1625. What is true about a1-antiirypsin defficiency: A. * It results in cirrhosis and emphysema. B. Characterized by excessive deposition of iron in liver. C. Characterized by excessive deposition of copper in liver. D. No one mentioned. E. All mentioned. 1626. What is true about autoimmune hepatitis: A. It is four times more common in women than in men B. There is a rise of IgG, a positive anti-smooth-muscle antibody is present in 60% of patients. C. Antinuclear antibody and liver-kidney microsomal antibody (LKM-1) may be present. D. Response on corticosteroids therapy consists 70-90%. E. * All mentioned. 1627. What is true about cryptogenic hepatitis: A. * Unknown cause. B. It is four times more common in women than in men. C. There is a rise of IgG level, a positive anti-smooth-muscle antibody is present in 60% of patients. D. Antinuclear antibody and liver-kidney microsomal antibody (LKM-1) may be present. E. Response on corticosteroids therapy consists 70-90%. 1628. What is cause of an osmotic laxative? A. * Lactulose. B. Psyllium. C. Magnesium citrate. D. Castor oil. E. Lubiprostrone. 629. What is not a paraneoplastic syndrome for hepatocellular carcinoma? A. * Hyperglycemia. B. Hypoglycemia. C. Erythrocytosis. D. Hypercalcemia. E. None of mentioned. 1630. Which of the following statements is true according to the a-fetoprotein- L3? A. * High level is seen in casr of hepatic carcinoma. B. Pre-operative high level means worse prognosis. C. High level is seen in case of stomach carcinoma. D. Level may be increased in case of hepatitis. E. No one mentioned. 1631. Which of the following statements according tothe cryptogenic hepatitis is true? A. * No specific test. B. HbsAg. C. IgG anti-HBc. D. HbeAg. E. Anti-HBs. 1632. Which of the following statements according to the delta hepatitis virus (HDV) is correct? A. * HDV can infect only persons who are infected by hepatitis B virus (HBV). B. HDV is a defective DNA virus. C. The HDV genome is partially homologous to the HBV DNA. D. HDV infection has been found only in limited areas of the world. Simultaneous infection with HDV and HBV results in an increased risk of the development of chronic hepatitis. E. 633. Which of the following statements according to the liver cirrhosis isn’t true? A. * Caused by viral hepatitis A B. Caused by alcohol C. Treatment focuses on preventing progression and complications’ development. D. Caused by fatty liver disease. E. Is generally irreversible condition. 1634. Which of the following statements according to the liver cirrhosis isn’t true? A. * Caused by viral hepatitis E. B. Is generally irreversible condition. C. Treatment focuses on preventing progression and complications’ development. D. Caused by alcohol. E. Caused by hepatitis B and C. 635. Which one of the following pathology cause the non cirrhotic portal fibrosis? A. Intrahepatic phlebosclerosis and fibrosis. B. Portal and splenic vein sclerosis. C. Portal and splenic vein thrombosis. D. Schistosomiasis. E. * All of mentioned. 1636. Which one of the following statements about hepatitis B antigen (HBeAg) is the least correct? A. * The absence of HBeAg in the serum determine a chronic infection caused by the hepatitis B virus. B. The presence of HBeAg in the serum is correlated with infectiousness. C. HBeAg can be detected transiently in the serum of patients with acute hepatitis B infection. D. HBeAg is distingished immunologically from HBsAg but is genetically related with HBcAg. The disappearance of HBeAg from the serum can be a sign of patient’s recovering with acute hepatitis B infection. E. 1637. Wilson’s disease is characterized by: A. * Excessive deposition of copper in liver. B. Excessive deposition of iron in liver. C. Transfers into cirrhosis and emphysema. D. No one mentioned. E. All mentioned. 1638. Gastric Ulcer is caused due to - A. Bile acid reflux B. Recurrent herb C. Hyperacidity D. * Decreased mucosal resistance E. Decreased local imunity 1639. Which cells are present in large number in the peritonel fluid of Tuberculous peritonitis? A. Eosinophils B. Polymorphs C. * Lymphocytes D. Monocytes E. Leukocytes 1640. Treatment of drug-induced gastritis: A. Mesoprostol B. * H2 receptor blockers C. Antacids D. Aspirin E. Broad-spectrum antibiotics Which of the following cations is presents in gastric juice in a larger concentration than in blood 1641. plasmaA. Na+ B. * K+ C. Mg+ D. Ca+ E. Lithium 1642. Which of the following diagnostic method of confirming tuberculousis peritonitis is the best ? A. Culture peritoneal fluid B. Mantoux C. * Peritoneal biopsy D. Upper GL contrast films E. Laparoscopy 1643. PH of the gastric acid is - A. * 1.5 to 2.0 B. 0.5 to 2.5 C. 2.5 to 3.0 D. 3.0 to 3.5 E. 3.5 to 4.0 1644. Differential diagnosis of chylous ascites includes all the following syndroms except A. Lymphoma B. * Nephrotic Syndrome C. Tuberculosis D. Amyloidosis E. Leukemia 1645. Tietz's syndrome usually develops at the” ... ” costal cartilage- A. * Second B. Sixth C. Eigth D. Fourth E. First 1646. Level of gastrin is raised because of- A. Zolinger Ellison syndrome B. Pernicious anaemia C. Gastric ulcer D. * AH E. Gastritis 1647. The treatment of peptic ulcer includes: A. Antacids B. Ranitidine C. Sucralfate D. * All E. Vitamins 1648. Bernstein test is useful in the diagnosis of cause of- A. * Pyrosis B. Odynophagia C. Dysphagia D. Dyspepsia E. Polyphagia 1649. The best method to estimate secretion of gastric acid is- A. F.T.M B. Night secretion C. * Pentagastrin test D. A.H.T E. Daily Ulcer in lesser curvature in 65 year old man after biopsy is negative for malignancy but is not healing after treatment of H2 blockers during 6 weeks.Next treatment is1650. A. Repeat biopsy B. Total gastrectomy C. Partial gastrectomy D. * Hydrogen blockers for another 6 weeks E. Antacids 1651. What is wrong regarding Menetrier's disease - A. Associated with protein loss B. A premalignant condition C. Hypertrophy of mucosal folds in stomach is seen D. * All is correct E. All is wrong 1652. Sites of Cushing's ulcer are,except of- A. Oesophagus B. Stomach C. Proximal duodenum D. * Distal duodenum E. Distal part of oesophagus Endoscopy of a patient having peptic ulcer disease shows features of chronic antral gastritis. Which of the following dyes you will use for stain a specimen taken from the stomach 1653. A. PAS B. Gram stain C. * Warthin starry stain D. Zwihl Nielson stain E. Romanovskiy-Hymsa stain 1654. Least irritant fluid to peritoneum - A. * Blood B. Urine C. Bile D. Pancreatic fluid E. Gastric juice 1655. Progressive dysphagia is seen in connection with - A. * Carcinoma esophagus B. Globus hystericus C. Presbyesophagus D. Achalasia E. Chalasia 1656. Carcinoma stomach is associated with blood group – A. * A B. B C. AB D. O E. Is not associated with any blood group 1657. Stress ulcers seen in burns are – A. * Curling's ulcer B. Cushing's ulcer C. Meleney's ulcer D. Rodent ulcer E. All 1658. Early gastric cancer generally indicates- A. Gastric adencarcinoma detected early B. Gastric adenocarcinoma confined to the mucosa C. * Gastric adenocarcinoma confined to the mucosa and submucosa D. Gastric adenocarcinoma is less than 1 cm in size E. Gastric adenocarcinoma is less than 0,5 cm in size 1659. Most common causes of decrease in incidence of H.pylori inwestisd/t- A. * Change in the style B. Increased use of PPI C. Chemotherapy D. Mutation in organism E. Radiotherapy 1660. True about mucosa associated lymphoma - A. * H. Pylori predispose B. Chemotherapy unsensitive C. Multiple lymphomas D. Stromal polyp E. Radiotherapy unsensitive In the Forrest classification for bleeding peptic ulcer with a visible vessel or pigmented protuberance is classified as – 1661. A. * FI B. FIIa C. FIIb D. FIIc E. FIII 1662. Treatment of H. pylori is required in all of the following diseases,expect ? A. * Gastro esophageal reflex disease B. Gastric ulcers C. Duodenal ulcers D. Gastric lymphoma E. Duodenal lymphoma 1663. All about regarding GERD is true except - A. Avoid coffee & Tea B. Transient lower esophageal relaxation C. * Length and pressure of lower esophageal sphincter is important D. E. Proton pump inhibitor is the treatment of choice Avoid smoking and Tea In which of the following disorders of the stomach eradication of helicobacter pylori has been proved to be beneficial? 1664. A. * Low grade malt lymphoma B. Prosive gastritis C. Stomach cancer D. Gastroesophageal disease E. Gastric ulcers 1665. Small intestinal lesions in children with pathognomonic biopsy-finding is - A. Giardiasis B. Tropical sprue C. * A-beta-lipoproteinemia D. All E. Polyposis 1666. AH are complications of ulcerative colitis except - A. Haemorrhage B. Stricture C. Malignant change D. Polyposis E. * Oesophageal varices 1667. Diarrhea and paralytic ileus occurs in – A. * Hypokalaemia B. Hypermagnesemia C. Hypocalcemia D. All of the above E. Hypercalcemia 1668. Paralytic ileus is a feature in all diseases except - A. Retroperitoneal hematoma B. Hypokalemia C. * Diabetes D. Porphyria E. Peritonitis 1669. All of the following methods have been used to treat uncomplicated regional ilietis, except - A. * Radiation therpapy B. Prokinetics C. Steroids D. Nonabsorbable sulfonamides E. Hormonetherapy 1670. Characteristic features of ischaemic colitis at the onset of an attack include - A. Steatorrhoea B. * None C. Necessity of emergency surgery D. Signs of generalized peritonitis E. Family history of the disease 1671. Meconium ileus is a manifestation of- A. Hirschprungs disease B. Achalasia cardia C. * Fibrocystic disease of pancrease D. Coeliac disease 1672. Fatal gastroenteritis is caused by A. * Typhoid B. Amebiasis C. Anthraxis D. Giardiasis E. Esheryhiozis 1673. The normal fecal fat excretion is - A. * Less than 5 gm/day B. 8 gm/day C. 10 gm/day D. 15 gm/day E. 17 gm/day 1674. Lactase deficiency of jejunal leads to diarrhea from eating A. * Milk B. Gluten C. Meat D. Rice E. Potato 1675. Gluten induced enterpopathy has the following signs - A. D-xylose absent in stools B. * Fecal fat is high C. Schilling test 18% in 48 hours D. Acanthosis E. Fecal fat is low The urinary excretion of Radioactive vitamin B12 after oral administration in vitamin B12 malabsorptionis1676. A. More than 50% B. 30 to 40% C. 20 to 30% D. * less than 10% E. More than 60% 1677. There is a deficiency In Coeliac sprue of all items except- A. Vitamin A B. * Vitamin B|2 C. Folicacid D. Iron E. Vitamin B|1 1678. Non tropical sprue is characterized by - A. Elongation of intestinal villi B. Current jelly stools C. Hypertriglyceridaemia D. * Poor absorption of lipids E. Rich absorption of lipids 1679. Xylose absorption tests is good screening test for A. Fat absorption B. Pernicious anaemia C. * Carbohydrate absorption D. Amino acid absorption E. Protein absorption 680. Abnormal schilling test which persists after intrinsic factor is given suggests A. * Blind loop syndrome B. Pernicious anaemia C. Defective marrow D. Total gastrectomy E. Sectoral gastrectomy 1681. Specific test for malabsorption - A. * D-xylose test B. Schilling test C. Fecal fatestimation D. Hydrogen breath test E. X-xylose test 1682. Whipples disease is associated with - A. Cerebellar ataxia B. * All C. Dementia D. Supranuclear ophthalmoplegia E. It is not associated with anything Patient with congenital lactose deficiency will experience distension, flatulence and diarhoea after ingestion of1683. A. Glucose B. Sucrose C. * Milk D. Eggs E. Cheese 1684. Diarrhoea, flatulence and abdominal cramps aftersucrose ingestion is probably due to- A. * Disacaharidase deficiency B. Insulinoma C. Diabetes mellitus D. Glucose-6 phosphate dehydrogenase deficiency E. Violation of glucose tolerance 1685. Rare complication of ulcerative colitis – A. Pseudopolypi B. * Carcinoma C. Toxic dilatation D. Massive hemorrhage E. Perforation 1686. Perecentages of small intestine which can be removed without causing much digestive disabilities- A. 10% B. * 0% C. 70% D. 90% E. 55% 1687. Coeliac disease is associated with HLA.... - A. A-3 B. DR-3 C. D&8 D. DR-4 E. * None 1688. Extra intestinal complication which is more common in Ulcerative Colitis than Crohns disease - A. Uveitis B. * Pyoderma gangrenosum C. Cirrhosis D. Cholangiocarcinoma E. Pyoderma simplex 1689. Which is not true about arthritis, which is associated with inflammatory bowel disease - A. Migratory arthritis B. Knee joint most common C. * Deformations are common D. Correlates to severity of colitis E. Deformations are local 1690. Fibrosis around Brunner's glands is characteristic of - A. Intestinal lymphoma B. Radiation eneritis C. Amyloidosis D. * Scleroderma E. Gastroineritis 1691. Treatment for psuedomembranous enterocolitis including all methods,except - A. Retention enema of saline with faecal suspension B. Azulfidine C. ACTH D. Sodium colistimethate E. * All 1692. All is true about short bowel syndrome except - A. * Intestinal transmit time is increased B. Nutritional deficiency present C. Site atorrhea present D. None E. Decreased 1693. Punctuated yellow exudate in colon, which was found during endoscopic examiantion are indicative ofA. Balantidium coli B. Ulcerative colitis C. * Antibiotic colitis D. Gluten induced enteropathy E. Hemocolitis 1694. After extensive small bowel resection, increased incidence of renal stones is due to - A. Increased absorption of Vit. D B. Increased CA absorption from rectum C. Increased acid loss duodenum D. * Increased oxalate absorption E. Decreased oxalate absorption 1695. Loss of 90% of ileum & jejunum leads to all of following sings,except - A. Anemia B. Osteomalacia C. Fluid loss D. * All E. General weakness 1696. Jejunal biopsy is diagnostic in A. Celiac Sprue B. Tropical Sprue C. * Whipple's disease D. Radiation enteritis E. In all cases 1697. Regarding incidence of Ca during ulcerative colitis which is true for- A. Arise from pseudopolyps B. * Increased incidence if age of ulcerative colitis is early C. Always D. decreased incidence with increase in age E. Decreased incidence if age of ulcerative colitis is early 1698. What are the respiratory symptoms? A. * Chest pain, cough, dyspnea, wheezes, haemoptysis. associated with exraintestinal manifestation B. Pain in the heart region, palpitation, intermissions, oedema C. Headache, dizziness, dysphagia, nausea, vomiting. D. Pain in the right subcostal region, bitter taste, brown urine, skin itching, jaundice. E. Back pain, dysuria, ishuria, eyes oedema, weakness. 1699. What are the respiratory symptoms? A. Abdominal pain, nausea, vomiting B. Heartburning, faint (syncope), palpitation C. * Cough with rusty sputum, chest pain, dyspnea D. Swelling abdomen, constipation, melena E. Oedema, dysuria, haematuria 1700. What feature does pleural pain have? A. Be caused by physical extension B. Radiate to the right hand C. * Appears and increases due to cough and deep breathing D. Radiate to the left hand and scapula E. Duration under 15 minutes. 1701. What are the cough causes? A. Irritation of the larynx receptors B. Irritation of the trachea and bronchus receptors C. Irritation of the pleural receptors D. * All mentioned above E. Northing from above 1702. If patient has laryngitis his cough is characterized with A. harsh and hoarse sound B. absent of sputum C. it is permanent D. it is loud E. * all mentioned above 1703. If patient has clear, thick sputum it is named A. * Mucoid B. Purulent C. Copious D. Fetid E. Hemoptysis 1704. Chronic expectorating copious sputum is observed at patient with A. Acute bronchitis B. Asthma C. Atelectasis D. Emphysema E. * Bronchiectasis 1705. What is an objective dyspnea? A. Disorders of the respiratory rate B. Disorders of the respiratory depth C. Disorders of the respiratory rhythm D. * Disorders of the respiratory rate, depth, rhythm E. Northing from above 1706. Which type of dyspnea is observed at the patients with obstructive syndrome? A. * Expiratory B. Inspiratory C. Mixed D. Changing E. All mentioned above. 1707. Which types of dyspnea do you know? A. Mixed B. Expiratory C. Inspiratory D. * All mentioned above E. Northing from above 1708. Sputum production that contains pus is described by what term? A. * Purulent B. Fetid C. Copious D. Colored E. None of the above 1709. Which of the following characteristics is not typical of pleuritic chest pain? A. Increases with deep breathing B. Increases with coughing C. * Radiates to the jaw D. Is located laterally E. Diminishes with splinting of the affected side 1710. Which type of pulmonary problem usually causes a breathing pattern with a prolonged expiratory time? A. * Chronic obstructive pulmonary disease B. Atelectasis C. Pulmonary edema D. Pneumonia E. Pleural effusion. 1711. Inspiratory dyspnea is – A. Difficult breathing during exhalation B. * Difficult breathing during inhalation C. Difficult breathing during exhalation and inhalation D. Difficult breathing during hyperventilation E. Northing from above 1712. Expiratory dyspnea is – A. * Difficult breathing during exhalation B. Difficult breathing during inhalation C. Difficult breathing during exhalation and inhalation D. Difficult breathing during hyperventilation E. Northing from above 1713. Mixed dyspnea is – A. Difficult breathing during exhalation B. Difficult breathing during inhalation C. * Difficult breathing during exhalation and inhalation D. Difficult breathing during hyperventilation E. Northing from above 1714. Whistle and noise breathing with feeling breathlessness is named … A. Dyspnea B. Respiratory noise C. Musical breathing D. * Wheezing E. All mentioned above 1715. What quantity of the blood is characterized hemoptysis? A. * 20-50 ml B. 60 – 70 ml C. 140 - 250 ml D. All mentioned above E. Northing from above Lung bleeding is a pathological condition when the blood expectorates from airways. What quantity of the blood is characterized lung bleeding? 1716. A. 15 - 20 ml B. 30–40 ml C. * 240 - 250 ml D. All mentioned above E. Northing from above Amount of cigarettes that patient smokes in a day multiply to number of smoking years and divide to 20 (pack/years) use for calculating … 1717. A. * Smoking history B. Smoking C. Smoking habit D. Smoking abuse E. All mentioned above. 1718. If patient’s respiratory rate is 32 per minute he has… A. * Tachypnea B. Bradypnea C. Apnea D. Polypnea E. Dyspnea 1719. What types of breathing does healthy man have in a rest? A. * Abdominal breathing B. Thoracic breathing C. Mixed breathing D. All mentioned above E. Northing from above 1720. If patient doesn’t have respiratory moving his condition is named: A. Tachypnea B. Bradypnea C. * Apnea D. Polypnea E. Dyspnea 1721. Kussmaul ‘s breathing is… A. * Disorder of breathing depth B. Disorder of the respiratory rate C. Disorder of the respiratory rhythm consumption D. Disorder of the respiratory types E. Hyperventilation syndrome 1722. Cheyne-Stokes breathing is … A. Disorder of breathing depth B. Disorder of the respiratory rate C. * Disorder of the respiratory rhythm D. Disorder of the respiratory types E. Hyperventilation syndrome 1723. What is the normal respiratory rite in a rest? A. 12-14 per 1 minute B. * 16-20 per 1 minute C. 10-12 per 1 minute D. 20-24 per 1 minute E. 24-28 per 1 minute 1724. What types of breathing does healthy woman have in a rest? A. Abdominal breathing B. * Thoracic breathing C. Mixed breathing D. All mentioned above E. Northing from above 1725. If patient’s respiratory rate is 10 per minute he has…: A. Tachypnea B. * Bradypnea C. Apnea D. Polypnea E. Dyspnea 1726. What types of breathing do you know? A. Abdominal breathing B. Thoracic breathing C. Mixed breathing D. * All mentioned above E. Northing from above 1727. Which of the following conditions is associated with increased vocal fremitus? A. * Pneuomonia B. Emphysema C. Pneumothorax D. Pleural effusion E. Bronchial asthma 1728. Which of the following condition is associated with asymmetrical diminished vocal fremitus? A. Pneumonia B. Emphysema C. Bronchial asthma D. Chronic bronchitis E. * Pleural effusion 1729. Which of the following condition is associated with painfulness of the pleural points? A. * Lobar pneumonia B. Bronchial asthma C. Pleural effusion D. Emphysema E. Chronic bronchitis 1730. Which of the following condition is associated with increased chest resistance? A. acute bronchitis B. focal pneumonia C. * COPD D. mild bronchial asthma E. all mentioned above. 1731. What does the general inspection start with? A. Skin B. Position in bed. C. * General condition D. Edemas E. Joints 1732. What kind of posture is observed at the bronchial obstruction? A. Upright B. * Sitting position fixing the shoulder girdle C. Orthopnoea D. Sitting posture bending forward E. Knee-elbow posture 1733. If patient skin has diffuse bluish tint, it is named: A. * Diffuse cyanosis B. Diffuse erythema C. Acrocyanosis D. Pathological pallid skin E. Northing mentioned above. 11734. What mechanisms are caused by the cyanosis? A. Secondary pulmonary hypertension B. Restricted pulmonary circulation C. Artery-venous blood shunting D. Primary pulmonary hypertension E. * Everything mentioned above 1735. What kind of posture is observed at the left dry pleurisy? A. Upright B. Sitting position fixing the shoulder girdle C. Orthopnoea D. * On the left side E. Sitting posture bending forward 1736. What kind of posture is observed at the right pleural effusion? A. Orthopnea B. * On the right side C. Sitting position fixing the shoulder girdle D. On the left side E. Sitting posture bending forward 1737. What shape of the chest can be observed at the patient with chronic tuberculosis? A. Normosthenic B. Asthenic C. Barrel D. * Paralytic E. "Funnel breast" 1738. What shape of the chest can be observed at the patient with emphysema? A. Normosthenic B. Asthenic C. * Barrel D. Paralytic E. "Funnel breast" 1739. How is chest shape changed at the left side pneumothorax? A. * Enlarged left part of the chest B. Reduced left part of the chest C. Enlarged right part of the chest D. Reduced right part of the chest E. Not changed 1740. Where is bronchial breath sound formed? A. * in larynx B. in trachea C. in bronchus D. in alveoli E. in pleural cavity 1741. Where is vesicular breath sound formed? A. in the larynx B. in the trachea C. in the bronchus D. * in the alveoli E. in the pleural cavity 1742. Which of the following properties is not appropriate to bronchial breath sound? A. Heard over trachea and major bronchi B. Loud and rough C. * Heard only during inspiration D. Sound like “h” heard during inspiration and expiration E. Formed in the larynx 1743. Which of the following properties is not appropriate to vesicular breath sound? A. * Heard over trachea and major bronchi B. Soft sound C. Heard during inspiration and one third of expiration D. Sound like “f” heard during inspiration and expiration E. Formed in the alveoli 1744. When can the weakened vesicular breath sound be heard? A. 2nd stage of lobar pneumonia B. Acute bronchitis C. Large cavity in the lung D. * Emphysema E. Complete atelectasis 1745. When can not the weakened vesicular breath sound be heard? A. Emphysema B. Focal pneumonia C. Dry pleurisy D. * Large cavity in the lung E. Pneumosclerosis 1746. When can the amphoric breath sound be heard? A. Emphysema B. lobar pneumonia C. Dry pleurisy D. * Large cavity in the lung E. Pneumosclerosis 1747. What auscultation phenomenon is heard of the large pleural effusion? A. * Absent of the breath sound B. Vesicular breath sound with prorogated exhalation C. Rough vesicular breath sound D. Bronchial breath sound E. Weakened vesicular breath sound 1748. What auscultation phenomenon is heard of the bronchial asthma? A. Absent of the breath sound B. * Vesicular breath sound with prorogated exhalation C. Rough vesicular breath sound D. Bronchial breath sound E. Weakened vesicular breath sound 1749. What breath sound is heard of the focal pneumonia near root of lung? A. * Normal vesicular breath sound B. Vesicular breath sound with prorogated exhalation C. Rough vesicular breath sound D. Bronchial breath sound E. Weakened vesicular breath sound 1750. How vesicular breath sound is changed in case of pneumotorax? A. Not change B. * Became weakened C. Became pathological bronchial D. Became amphoric E. Became rough 1751. How vesicular breath sound changed is in case of acute bronchitis? A. Not change B. Became weakened C. Became pathological bronchial D. Became amphoric E. * Became rough 1752. How vesicular breath sound is changed in case of the 2nd stage of the lobar pneumonia? A. Not change B. Became weakened C. * Became pathological bronchial D. Became amphoric E. Became rough 1753. When can the stridor be heard? A. Emphysema B. Atelectasis C. Pleural effusion D. * Obstruction of the trachea and major bronchi E. Pneumosclerosis 1754. How vesicular breath sound is changed in case of COPD exacerbation? A. Not change B. Became weakened C. Became pathological bronchial D. Became amphoric E. * Became rough with prorogated exhalation 1755. How vesicular breath sound is changed in case of the 1nd and 3rd stage of the lobar pneumonia? A. Not change B. * Became weakened C. Became pathological bronchial D. Became amphoric E. Became rough 1756. How vesicular breath sound is changed in case of the dry pleurisy? A. Not change B. * Became weakened C. Became pathological bronchial D. Became amphoric E. Became rough 1757. When can bronchophony be heard? A. pulmonary emphysema B. * lobar infiltration of the lungs C. fluid in the pleural cavity D. pleural obliteration E. Everything mentioned above. 1758. What auscultation phenomenon is heard of the complete atelectasis of the lower right lung lobe? A. * Absent of the breath sound B. Vesicular breath sound with prorogated exhalation C. Rough vesicular breath sound D. Bronchial breath sound E. Weakened vesicular breath sound 1759. Syndrome of the focal consolidation of the lung tissue can be if patient has: A. focal pneumonia; B. focal pneumofibrosis; C. focal tuberculosis; D. lung cancer; E. * all mentioned above. 1760. Syndrome of the lobar consolidation of the lung does not reveal at patient with… A. Lobar pneumonia B. Infiltrative tuberculosis C. Pulmonary embolism with infarction-pneumonia D. * COPD E. Lung cancer 1761. At the patient with lobar consolidation at palpation of the chest can be obtained A. * Amplifying vocal fremitus on the affected side B. Weakened vocal fremitus on the affected side C. Vocal fremitus does not change D. Vocal fremitus is absent E. Amplifying vocal fremitus on the health side 1762. At the patient with focal consolidation near the root of lung at palpation of the chest can be obtained A. Amplifying vocal fremitus on the affected side B. Weakened vocal fremitus on the affected side C. * Vocal fremitus does not change D. Vocal fremitus is absent E. Amplifying vocal fremitus on the health side 1763. Pathological bronchial breathing is heard at patients with: A. focal consolidation B. * lobar consolidation C. pleural effusion D. emphysema E. acute bronchitis 1764. Percussion sound of the lobar consolidation of lung tissue is: A. tympanic B. clear C. resonance D. * dull E. small dull 1765. Auscultation signs of the focal consolidation is: A. Vesicular breathing with prorogated exhalation and wheeze B. Absent of the any breath sound C. * Diminished vesicular breathing and sonorous bubbling (moist) rales D. Unchanged vesicular breathing E. Pathological bronchial breathing 1766. Auscultation signs of the lobar consolidation is: A. Vesicular breathing with prorogated exhalation and wheeze B. Absent of the any breath sound C. Diminished vesicular breathing and sonorous bubbling (moist) rales D. Unchanged vesicular breathing E. * Pathological bronchial breathing 1767. Obstructive atelectasis can be if patient has: A. Lung cancer; B. Metastasis into pulmonary lymphonodes; C. Foreign body of bronchus; D. Tuberculosis of the pulmonary lymphonodes; E. * all mentioned above 1768. Compressive atelectasis can be if patient has: A. Pleural tumor (mesotelioma); B. Massive pleural effesion; C. Pneumothorax; D. Deformation of the chest; E. * all mentioned above. 1769. Percussion sound over massive pleural effusion: A. tympanic B. clear C. resonance D. * dull E. small dull 1770. Percussion sound over pneumothorax: A. * tympanic B. clear C. small box-sound D. dull E. small dull 1771. Auscultation signs of pneumothorax: A. Diminished vesicular breathing and wheeze B. Diminished vesicular breathing and crackles C. * absent of breath sounds D. unchanged breath sound E. Pathological bronchial breathing 1772. Auscultation signs of massive pleural effusion: A. Diminished vesicular breathing and wheeze B. Diminished vesicular breathing and crackles C. * absent of breath sounds D. unchanged breath sound E. Pathological bronchial breathing 1773. If patient has massive pleural effusion vocal fremitus is: A. * Absent on the affected side B. Increased on the affected side C. Diminished on the affected side D. Normal E. Increased on the health side 1774. Percussion sound over small pleural effusion: A. tympanic B. clear C. resonance D. dull E. * small dull 1775. If patient has small pleural effusion vocal fremitus is: A. Absent on the affected side B. Increased on the affected side C. * Diminished on the affected side D. Normal E. Increased on the health side 1776. Which properties does transudate have? A. Light yellow color B. Protein < 30 g/l C. Negative Rivalt test D. 1-5 leucocytes and 2-6 mezoteliocytes E. * All mentioned above 1777. Which properties does not exudate have? A. * Comparative density < 1,018 B. Protein > 30 g/l C. Positive Rivalt test D. 10-25 leucocytes and 2-6 mezoteliocytes E. Yellow color 1778. Percussion sound of the focal consolidation of lung tissue is: A. tympanic B. clear C. resonance D. dull E. * small dull 1779. What disease does patient have only dry cough and never sputum at? A. Acute bronchitis; B. * Dry pleurisy; C. Bronchoectasis; D. Cavernous tuberculosis; E. Pneumonia 1780. Test of Rivalt needs for: A. % contents of lymphocytes B. Determination of fibrin in pleural fluid C. * Differentiation transudates from exudates D. Determination of hemorrhagic character of exudates E. Determination of neutrophiles in pleural fluid 1781. Auscultation data of lobar pneumonia at resolution is: A. Bronchial breath sounds B. Vesicular breath sounds C. Amphoric breath sounds D. Saccadic breath sounds E. * Crackles 1782. Auscultation signs of the focal pneumonia near root of lung is: A. Wheeze B. Bronchial breath sounds C. sonorous bubbling (moist) rales D. diminished vesicular breath sounds E. * Vesicular breath sounds 1783. Percussion data of high point of lobar pneumonia is: A. small dullness B. * dullness C. clear D. resonance E. small dullness with tympanic tinge. 1784. Pneumonia is an inflammatory process that affects: A. bronchi and never alveoli or pleura B. only alveoli and never bronchi C. only pleura and bronchi D. * alveoli and pleura, can spread from bronchi E. only interstitial tissue and pleura 1785. Which of the following characteristics is not typical for pleuritic chest pain? A. Increases with deep breathing B. * Radiates to the jaw C. Is located laterally D. Diminishes with splinting of the affected side E. Increases with cough 1786. Which of the following may cause an increase in vocal resonance? A. emphysema B. asthma C. * pneumonia D. atelectasis E. dry pleurisy 1787. Percussion sound over fluid at the patient with massive exudative pleurisy is: A. * Dull B. Tympanic C. Resonant D. Small dull E. Clear 1788. Auscultation data at patient with dry pleurisy: A. Diminished vesicular breathing and crackles B. Diminished vesicular breathing and moist rales C. Bronchial breathing D. Rough vesicular breathing and dry rales E. * Diminished vesicular breathing and pleural friction rub 1789. Auscultation data at patient with high point stage of the lobar CAP is: A. breathing is absent B. normal vesicular breathing C. * bronchial breathing D. diminished vesicular breathing E. rough vesicular breathing 790. What types of pneumonias do you know? A. Community-acquired pneumonia B. Hospital pneumonia C. Aspiration pneumonia D. Pneumonia at immunocompromised patients E. * All mentioned above 1791. At the patient with focal pneumonia near the root of lung at palpation of the chest can be obtained A. Amplifying vocal fremitus on the affected side B. Weakened vocal fremitus on the affected side C. * Vocal fremitus does not change D. Vocal fremitus is absent E. Amplifying vocal fremitus on the health side 1792. Which syndrome can develop at the patient with central lung cancer? A. emphisema; B. pneumotorax; C. * obstructive atelectasis; D. lobar consolidation; E. northing from above. 1793. Which syndrome can develop at the patient with peripheral lung cancer? A. emphisema; B. pneumotorax; C. obstructive atelectasis; D. * lobar consolidation; E. northing from above. 1794. Auscultation signs of massive exudative pleurisy: A. Diminished vesicular breathing and crackles B. * absent of breath sounds C. unchanged breath sound D. Pathological bronchial breathing E. Diminished vesicular breathing and wheeze 1795. Which investigation is obligatory for confirming pneumonia? A. Sputum culture B. Full blood analysis C. * X-ray examination D. Bronchoscopy E. Lung function test 1796. Which properties does not transudate have? A. Light yellow color B. * Protein = 40 g/l C. Negative Rivalt test D. 1-5 leucocytes and 2-6 mezoteliocytes E. All mentioned above 1797. Which properties does exudate have? A. Comparative density > 1,018 B. Protein > 30 g/l C. Positive Rivalt test D. 10-25 leucocytes and 2-6 mezoteliocytes E. * All from above 1798. Which investigation is the most informative for confirming lung cancer? A. Sputum culture B. Full blood analysis C. X-ray examination D. * Bronchoscopy with biopsy E. Computered tomography 1799. What diseases is the bronchial obstruction syndrome developed at? A. Bronchial asthma; B. COPD; C. Acute obstructive bronchitis; D. * all mentioned above; E. northing from above. 1800. What diseases is the syndrome of increased lung airiness developed at? A. Lobar pneumonia B. * Emphysema C. Lung cancer D. Acute bronchitis E. Dry pleurisy 1801. What diseases is the respiratory failure developed at? A. Lobar pneumonia B. Severe COPD C. Severe exacerbation of the bronchial asthma D. Massive pleural effusion E. * All mentioned above 1802. What symptoms characterize the bronchial obstruction syndrome? A. * Wheezing, dry cough, tightness in the chest B. Cough with sputum, chest pain, fever C. Mixed dyspnea, hemoptysis, weakness D. Dyspnea, chest pain, palpitation E. Dry cough, chest pain, edema 1803. What symptoms don’t characterize the bronchial obstruction syndrome? A. wheezing B. cough C. tightness in the chest D. dyspnea E. * purulent sputum 1804. What change of vocal fremitus can be at the patient with bronchial obstruction? A. Amplifying B. Decreasing C. Absence D. Not changed E. * Change depends on clinical situation 1805. What change of vocal fremitus can be at the patient with emphysema? A. Amplifying B. * Decreasing C. Absence D. Not changed E. Change depends on clinical situation 1806. What change of vocal fremitus can be at the patient with respiratory failure? A. Amplifying B. Decreasing C. Absence D. Not changed E. * Change depends on clinical situation 1807. What is the main symptom of the respiratory failure? A. cough; B. * dyspnea; C. palpitation; D. wheezing; E. chest pain. 1808. What is the main symptom of the emphysema? A. cough; B. expiratory dyspnea; C. inspiratory dyspnea; D. wheezing; E. * mixed dyspnea. 1809. How is elasticity of the chest changed at the patient with emphysema? A. increasing B. * decreasing C. not changed D. absence E. depend on clinical situation 1810. How is elasticity of the chest changed at the patient with respiratory failure? A. increasing B. decreasing C. not changed D. absence E. * depend on clinical situation 1811. How percussion sound is changed at the patient with bronchial obstruction? A. * unchanged B. dull C. small box sound D. tympanic E. depend on clinical situation 1812. How percussion sound is changed at the patient with emphysema? A. unchanged B. dull C. * small box sound D. tympanic E. depend on clinical situation 1813. How percussion sound is changed at the patient with respiratory failure? A. unchanged B. dull C. small box sound D. tympanic E. * depend on clinical situation 1814. What are auscultation findings at the patient with bronchial obstruction? A. * Vesicular breathing with prorogated expiration, wheezing B. Diminished vesicular breathing, C. Diminished vesicular breathing and moist rales D. Diminished vesicular breathing and crepitation E. Vesicular breathing and pleural friction rub 1815. What are auscultation findings at the patient with emphysema? A. Vesicular breathing with prorogated expiration, wheezing B. * Diminished vesicular breathing, C. Diminished vesicular breathing and moist rales D. Diminished vesicular breathing and crepitation E. Vesicular breathing and pleural friction rub 1816. How is spirometry changed at the patient with bronchial obstruction? A. Increased FEV1, decreased FVC, FEV1/FVC> 70% B. * Normal FVC, decreased FEV1, FEV1/FVC< 70% C. Decreased FVC, decreased FEV1, FEV1/FVC <70% D. Increased FVC, increased FEV1, FEV1/FVC > 100% E. Normal FVC, normal FEV1, FEV1/FVC< 70% 1817. How is spirometry changed at the patient with emphysema? A. Increased FEV1, decreased FVC, FEV1/FVC> 70% B. Normal FVC, decreased FEV1, FEV1/FVC< 70% C. * Decreased FVC, decreased FEV1, FEV1/FVC <70% D. Increased FVC, increased FEV1, FEV1/FVC > 100% E. Normal FVC, normal FEV1, FEV1/FVC< 70% 1818. Which method can help to establish respiratory failure? A. bronchoscopy B. X-ray C. Computer tomography D. * pulsoxymetry E. Spirometry 1819. Bronchial asthma is a… A. Acute inflammatory disease; B. Acute infective disease; C. Chonic infective disease; D. * Chonic iinflammatory disease; E. northing from above. 1820. Chronic obstructive pulmonary disease is a… A. chronic inflammatory of trachea and large bronchus B. chronic inflammatory of large and medium bronchus C. * chronic inflammatory of medium, small bronchus with involving lung parenchyma and vessels D. All from above E. Northing from above 1821. Which symptoms characterize bronchial asthma? A. Mixed dyspnea, cough with purulent sputum B. * Episodic dry cough, tightness of the chest, wheezing C. Chest pain with radiation to jaw, inspiratory dyspnea D. Permanent expiratory dyspnea, cough E. Episodic hemoptysis and dyspnea due to physical effort 1822. Which symptoms characterize COPD? A. Mixed dyspnea, dry cough, chest pain B. Episodic dry cough, tightness of the chest, wheezing C. Chest pain with radiation to jaw, inspiratory dyspnea D. * Permanent expiratory dyspnea, cough, sputum production E. Episodic hemoptysis and dyspnea due to physical effort 1823. What symptom doesn’t characterize bronchial asthma? A. wheezing B. cough C. tightness in the chest D. dyspnea E. * purulent sputum 1824. What symptom doesn’t characterize COPD? A. wheezing B. cough C. * chest pain D. dyspnea E. purulent sputum 1825. What change of vocal fremitus can be at the patient with COPD? A. Amplifying B. * Decreasing C. Absence D. Not changed E. Change depends on clinical situation 1826. What change of vocal fremitus can be at the patient with bronchial asthma? A. Amplifying B. Decreasing C. Absence D. * Not changed E. Change depends on clinical situation 1827. If patient has asthma symptoms 1-2 times in a week, 1 night awaking in a mouth, he has… A. Intermitend asthma; B. * Mild persistent asthma; C. Moderate persistent asthma; D. Severe persistent asthma; E. depends on clinical situation 1828. If patient has asthma symptoms 1-2 times in a day, 1 night awaking in a week, he has… A. Intermitend asthma; B. Mild persistent asthma; C. * Moderate persistent asthma; D. Severe persistent asthma; E. depends on clinical situation 1829. If patient has asthma symptoms 1-2 times in a year, night awaking is absent, he has… A. * Intermitend asthma; B. Mild persistent asthma; C. Moderate persistent asthma; D. Severe persistent asthma; E. depends on clinical situation 1830. If patient has asthma symptoms 8-10 times in a day, every night awaking, he has… A. Intermitend asthma; B. Mild persistent asthma; C. Moderate persistent asthma; D. * Severe persistent asthma; E. depends on clinical situation 1831. How percussion sound is changed at the patient with COPD? A. unchanged B. dull C. * small box sound D. tympanic E. depend on clinical situation 1832. How mobility of the lung border is changed at the patient with COPD? A. unchanged B. * limited C. increased D. became immovable E. depend on clinical situation 1833. How percussion sound is changed at the patient with mild asthma? A. * unchanged B. dull C. small box sound D. tympanic E. depend on clinical situation 1834. What are auscultation findings at the patient with asthma attack? A. * Vesicular rough breathing with prorogated expiration, wheezing B. Diminished vesicular breathing, C. Diminished vesicular breathing and moist rales D. Diminished vesicular breathing and crepitation E. Vesicular breathing and pleural friction rub 1835. What are auscultation findings at the patient with COPD? A. Vesicular rough breathing B. * Diminished vesicular breathing with prolongated expiration, wheezing C. Diminished vesicular breathing and moist rales D. Diminished vesicular breathing and crepitation E. Vesicular breathing and pleural friction rub 1836. How is FEV1 increased after bronchial spasmolytic if patient has reversible obstruction? A. * >12% from initial B. >20% from initial C. >25% from initial D. 30% from initial E. 10% from initial If patient has permanent expiratory dyspnea during physical effort, FEV1 is 52% from predicted and FEV1/FVC 55% he has… 1837. A. Mild COPD B. * Moderate COPD C. Severe COPD D. Very severe COPD E. Depend on clinical situation If patient has permanent expiratory dyspnea in a rest, FEV1 is 22% from predicted and FEV1/FVC 45% he has… 1838. A. Mild COPD B. Moderate COPD C. Severe COPD D. * Very severe COPD E. Depend on clinical situation 1839. What are the cardiovascular symptoms? A. Chest pain, cough, dyspnea, wheezes, haemoptysis. B. * Pain in the heart region, palpitation, intermissions, oedema C. Headache, dizziness, dysphagia, nausea, vomiting. D. Pain in the right subcostal region, bitter taste, brown urine, skin itching, jaundice. E. Back pain, dysuria, ishuria, eyes oedema, weakness. 1840. What are the cardiovascular symptoms? A. Abdominal pain, nausea, vomiting B. * Dyspnea, faint (syncope), palpitation, dry cough C. Cough with rusty sputum, chest pain, dyspnea D. Swelling abdomen, constipation, melena E. Oedema, dysuria, haematuria 1841. What feature does the pain at angina pectoris have? A. Be caused by physical extension B. Duration under 15 minutes C. Constricting, feeling of heaviness D. Radiate to the left hand and scapula E. * All mentioned above 1842. What feature does not the pain at myocardial infarction have? A. Prolonged, continuous > 20-30 min. B. Severe, tight or burning. C. * Relief at rest D. Does not respond to nitrates. E. Radiate to both hands, jaws, neck. 1843. If patient has heart failure his cough is characterized with A. * appearing at lying position B. a lot of rusty sputum C. it is permanent D. it is loud E. all mentioned above. 1844. If patient has feeling of solitary beats at various intervals it is named A. * exrtasistole B. palpitation C. syncope D. dizziness E. heart dyspnea 1845. If patient has feeling of accelerated and intensified heart contractions onto the chest wall it is named A. exrtasistole B. * palpitation C. syncope D. heart dyspnea E. heart pain 1846. If patient has a lot of foamy pink liquid sputum it means he has A. * Pulmonary edema B. Pulmonary embolism C. Aortic aneurysm dissection D. all from above E. Northing from above 1847. Which type of dyspnea is observed at the patients with cardiovascular diseases? A. Expiratory B. * Inspiratory C. Mixed D. Changing E. All mentioned above. 1848. What is feature of dyspnea at patient with cardiac asthma attack? A. Appear at night B. Accompanying with dry cough C. Inspiratory D. Ortopnea position in the bed E. * all mentioned above 1849. Which of the following disorders is not likely to be associated with hemoptysis? A. Mitral stenosis B. Pulmonary embolism C. Pulmonary edema D. * Pericarditis E. None of the above 1850. What characteristics of edema at patient with heart failure? A. Asymmetrical on the part of body which patient lies on. B. Firstly on the face than gradually spreads to body down. C. * Firstly on the legs than gradually spreads to body up D. Hear the heart region E. Only on abdomen and hands 1851. What position does a patient with cardiovascular insufficiency occupy? A. * A forced sitting position with the legs let down. B. The patient prefers to lie on the affected side. C. The patient sits upright or resting the hands on the edge of the table of chair. A lying position on the side (lateral recumbent position) with the head thrown back and the bent legs pulled up to the abdomen. D. E. A forced knee-elbow position. 1852. What mechanisms are caused by the orthopnoea posture? A. Tissue oxygen demand reduce at rest, decreased myocardial ischemia B. * Re-distribution of blood into the low extremities, reducing of circulating blood volume, Decreasing blood volume, decreasing of venous pressure in the lesser circulation, improvement of gas exchange in the "alveoli-pulmonary capillaries" system, displacement of ascitis fluid C. D. Pericardial layers presses to one another, reduce their movement that decrease irritation of pain receptors in pericardium E. Improvement of diastolic cardiac function 1853. What kind of posture is observed at angina pectopis? A. * Upright B. On the right side with high head of the bed C. Orthopnoea D. Sitting posture bending forward E. Knee-elbow posture 1854. What kind of posture is observed at acute left ventricular failure? A. Upright B. On the right side with high head of the bed C. * Orthopnoea D. Sitting posture bending forward E. Knee-elbow posture 1855. What cardiovascular disease is characterized with constant pale skin color? A. Angina pectoris B. Mitral stenosis C. * aortic valve diseases D. Essential hypertension E. All mentioned above 856. Which of the following conditions is least to produce jugular venous distention? A. * Right heart failure B. Chronic left heart failure C. Chronic hypoxemia D. Liver failure E. Circulation insufficiency 1857. What kind of cyanosis is usually observed at patient with cardiovascular diseases? A. Central, warm B. * Peripheral, cold C. Peripheral warm D. Local (near heart region), cold E. Diffuse warm 1858. Which method can we use for establishing edema A. Visual inspection B. Palpation C. weighing patient D. measuring leg circumstance E. * All mentioned above. 1859. Loud first sound in the cardiac apex is auscultated in case of: A. Myocardiac infarction B. Myocarditis C. Myocardiac sclerosis D. * Synchronic systole of atriums and ventricles in case of full atrioventricular blockade E. Aortic stenosis 1860. Weakening of the first sound in the cardiac apex is auscultated with: A. * Stenosis of mitral orifice B. Insufficiency of mitral valve C. Aortic stenosis D. Tricuspid Regurgitation E. Pulmonary hypertension 1861. Weakening of both heart sounds is auscultated in case of: A. Myocardiac infarction B. Myocarditis C. Emphysema of lungs D. Myocardiosclerosis E. * All mentioned cases 1862. Loud second sound in aorta is auscultated in case of: A. Insufficiency of aortic valve B. Aortic stenosis C. * Essential hypertension D. Mitral stenosis E. Mitral regurgitation 1863. Loud both sounds in heart apex in case of: A. Lungs limbus shrinkage B. Posterior mediastinum tumors C. Forward inclination of body D. * All mentioned reasons E. Northing from above. 1864. Loud first sound in the cardiac apex is auscultated in case of: A. Mitral stenosis B. Ciliary arrhythmia C. Full atrioventricular blockade D. * All mentioned cases E. No right answer 1865. Loud second sound in pulmonary artery is auscultated in case of: A. Emphysema of lungs B. Chronic obstructive lung disease C. Pneumosclerosis D. * All mentioned reasons E. No right answer 1866. ‘Quail’ rhythm is: A. Loud ‘flapping’ first sound B. * Loud ‘flapping’ first sound, second sound, opening snap of mitral valve C. Opening snap of mitral valve D. Loud first, second and third sound. E. No right answer 1867. Loud ‘flapping’ first sound in heart apex is auscultated in case of: A. * Mitral stenosis B. Mitral insufficiency C. Aortic stenosis D. aortic insufficiency E. No right answer 1868. Ground of the second sound accent appearance over the pulmonary artery is: A. High pressure in greater circulation B. * High pressure in the pulmonary circulation C. High pressure in cava veins D. All above mentioned E. Northing from above 1869. Ground of the second sound accent above aorta is: A. * High pressure in greater circulation B. High pressure in pulmonary circulation C. High pressure in pulmonary veins D. All above mentioned E. Northing from above 1870. ‘Gallop’ rhythm is auscultated in case of: A. Diffuse myocarditis B. Cardiac infarction C. Dilatational cardiomyopathy D. Cardiac insufficiency E. * All mentioned variants 1871. The first sound in case of ‘gallop’ rhythm is: A. Intensified B. Reduplicated C. * Weakened D. All variants are right E. No right answer 1872. Reduplication of first sound appears in case of: A. Asynchronous right and left ventricle contraction B. Block of bundle of His C. Bisystolia (systole in 2 portions) D. * All mentioned variants E. No right answer 1873. Reduplication of second tone appears more often in: A. Aorta B. * Pulmonary artery C. Apex D. Xiphoid process E. All mentioned variants 1874. Reduplication of second sound in pulmonary artery is connected with: A. High pressure in lesser circulation B. Asynchronous aortic and pulmonary artery valve closing C. Breathing D. * All mentioned is true E. No right answer 1875. Presystolic ‘gallop’ rhythm is auscultated in case of: A. Cardiosclerosis B. * Mitral stenosis C. Chronic nephritis with hypertensive syndrome D. All above mentioned cases E. No right variant 1876. Protodiastolic ‘gallop’ rhythm is auscultated in case of: A. * Myocardial infarction B. Tricuspid insufficiency C. Pneumonia D. All above mentioned cases E. No right variant 1877. Embryocardia or pendulous rhythm appears in case of: A. High fever B. Paroxysmal tachycardia C. Cardiac insufficiency D. * All mentioned variants E. No right answer 1878. What heart diseases listed below can you find organic systolic cardiac murmurs at? A. mitral stenosis B. * Aortic stenosis C. Aortic regurgitation D. Pulmonary regurgitation E. Tricuspid stenosis 1879. The best point for hearing the systolic murmurs at aortic stenosis is A. The heart apex B. The Botkin – Erb point C. * The second intercostal space, to the right from the breastbone D. The second intercostal space, to the left from the breastbone E. On the middle of the breastbone on the level of third rib 1880. Anaemic functional murmur is more often: A. * Systolic B. Diastolic C. Protodiastolic D. Presystolic E. Systola-diastolic 1881. Haemodinamical functional murmurs can be auscultated at A. * Thyrotoxicosis B. Mitral stenosis C. Myocarditis D. Cardiosclerosis E. Hypertension disease 1882. The pericardial friction pub is better heard A. On the heart apex B. on the Botkin-Erb point C. * Above the absolute heart’s dullness zone D. On heart’s base E. Near the xiphoid process 1883. The pericardial friction rub differs from organic murmurs in that it is A. More delicate B. Heard like far away C. * Heard near the ear D. Always coincide with systole E. Well radiate to other auscultatic zones 1884. The pericardial friction rub differs from organic in that it is A. Never gives any tactile fillings B. Becomes stronger if patient bends forward C. Coincidence with systole and diastole D. Loud E. * all mentioned above. Which organic murmur gives the filling of “cat purr” in the second intercostal space right from the breastbone? 1885. A. Systolic murmur of mitral regurgitation B. Diastolic murmur of mitral stenosis C. * Systolic murmur of aortic stenosis D. Diastolic murmur of aortic regurgitation E. Systolic murmur of tricuspid regurgitation 1886. Systolic murmur of aortic stenosis irradiates A. To the heart apex and to Botkin’s point B. To the left axillary region C. To the second left intercostal space D. To the area of xiphoid process E. * To the carotid and subclavical arteries 1887. Which functional murmur can be heard at mitral stenosis? A. Systolic hydremic B. Systolic hemodynamic C. Systolic muscular D. Kumbs’ murmur E. * Graham-Steel murmur 1888. The best point for hearing the diastolic murmurs at aortic regurgitation is A. The heart apex B. * The Botkin – Erb point C. The second intercostal space, to the right from the breastbone D. The second intercostal space, to the left from the breastbone E. On the middle of the breastbone on the level of third rib 1889. Anaemic murmur is heard better A. Above the lung artery B. At Bodkin’s point C. Above all valve orifices D. * On the apex of the heart E. Above the aorta 1890. How is functional systolic murmur differed from organic one? A. It is not ruled by periods of breathing B. Loud, harsh, prolonged C. Do not change during exercises D. * Do not have irradiative zones E. Often supported by feeling of systolic “cat purr” 1891. The pericardial friction rub usually appears at A. Uremia B. Hydropericardium C. Cardiomegaly D. Angina pectoris E. * Adhesion of pericardium and pleura 1892. The pericardial friction rub differs from organic in that it is A. Become stronger during pressing the chest B. * Becomes weaker if patient bends forward C. Heard above zones, projections and places of the best auscultation of heart’s vavles D. Do not coincidance with cardiac periods E. Never gives tactile sings 1893. Which organic murmur gives the filling of “cat purr” on the heart apex? A. Systolic murmur of mitral regurgitation B. * Diastolic murmur of mitral stenosis C. Systolic murmur of aortic stenosis D. Diastolic murmur of aortic regurgitation E. Systolic murmur of tricuspid regurgitation Which cardiac murmur gives tactile filling above absolute cardiac dullness that becomes stronger while bending the body forward? 1894. A. Systolic murmur of mitral regurgitation B. Diastolic murmur of mitral stenosis C. Systolic murmur of aortic stenosis D. Diastolic murmur of aortic regurgitation E. * Systole-diastolic pericardial friction rub. 1895. Which functional murmur can be heard at aortic regurgitation? A. Systolic hydremic B. Systolic hemodynamic C. * Flint’s murmur D. Coombs’ murmur E. Graham-Steel murmur 1896. What are the reasons for Flint’s murmur in aorta valve deficiency A. Relative mitral regurgitation B. * Relative mitral stenosis C. Relative aortic stenosis D. Relative tricuspid regurgitation E. Relative pulmonary stenosis 1897. Which pathological conditions can be confirmed by 2-dimenshional echocardiography? A. congenital heart disease, B. left ventricular aneurysm C. mural thrombus D. E. * Valve heart diseases All mentioned above