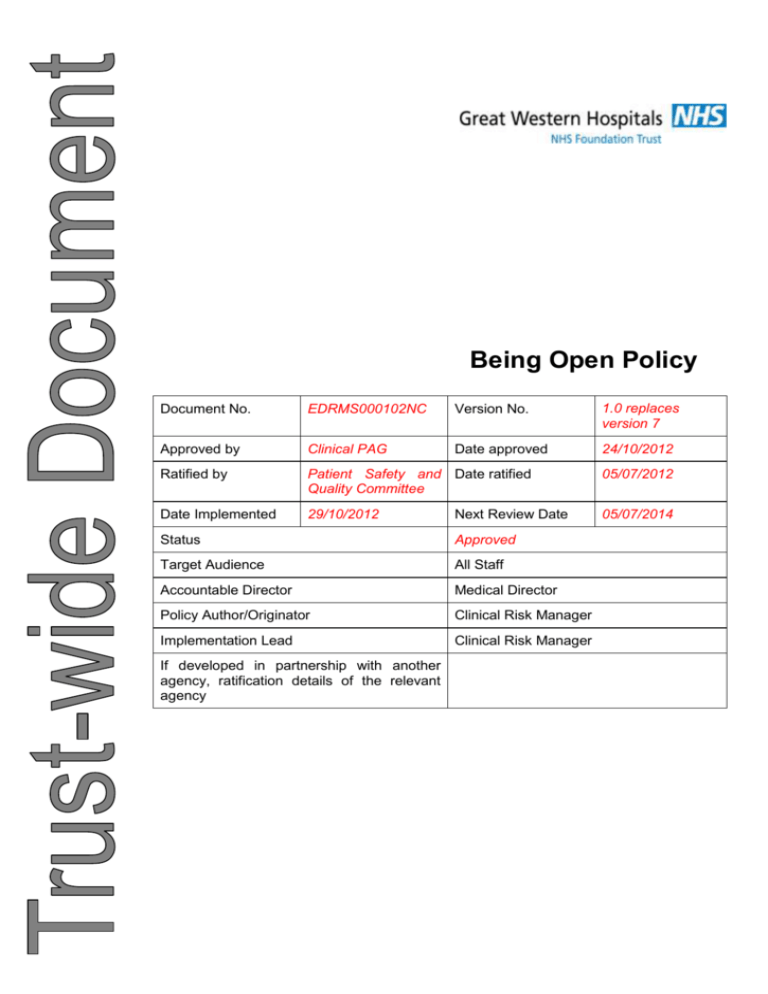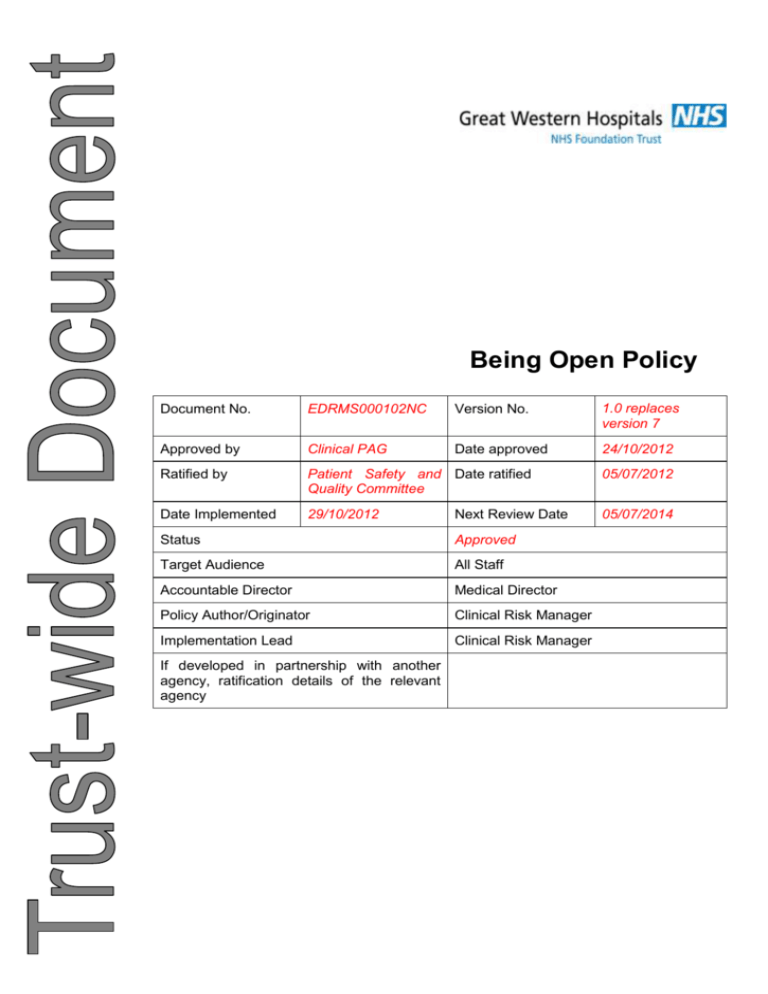
Being Open Policy
Document No.
EDRMS000102NC
Version No.
1.0 replaces
version 7
Approved by
Clinical PAG
Date approved
24/10/2012
Ratified by
Patient Safety and Date ratified
Quality Committee
05/07/2012
Date Implemented
29/10/2012
05/07/2014
Next Review Date
Status
Approved
Target Audience
All Staff
Accountable Director
Medical Director
Policy Author/Originator
Clinical Risk Manager
Implementation Lead
Clinical Risk Manager
If developed in partnership with another
agency, ratification details of the relevant
agency
Document Title: Being Open Policy
Equality Impact
Great Western Hospitals NHS Foundation Trust (‘GWH’) strives to ensure equality of opportunity for
all service users, local people and the workforce. As an employer and a provider of health care,
GWH aims to ensure that none are placed at a disadvantage as a result of its policies and
procedures. This document has therefore been equality impact assessed in line with current
legislation to ensure fairness and consistency for all those covered by it regardless of their
individuality. This means all our services are accessible, appropriate and sensitive to the needs of
the individual.
Note: This document is electronically controlled. The master copy of the latest approved version is maintained by the owner department.
If this document is downloaded from a website or printed, it becomes uncontrolled.
Version 1.0
Printed on 06/02/2016 at 5:05 PM
Page 2 of 31
Document Title: Being Open Policy
Contents
1
Document definition ....................................................................................... 5
1.1
Introduction .................................................................................................... 5
1.2
References & Further Reading ....................................................................... 5
1.3
Glossary / Definitions ..................................................................................... 6
1.4
Purpose ......................................................................................................... 8
1.5
Scope............................................................................................................. 9
1.6
Regulatory Position ........................................................................................ 9
1.7
Special Cases ................................................................................................ 9
1.8
Comments...................................................................................................... 9
2
Roles and Responsibilities ........................................................................... 10
3
Introduction .................................................................................................. 12
3.1
The principles of Being Open ....................................................................... 13
3.1.1
3.1.2
3.1.3
3.1.4
3.1.5
3.1.6
3.1.7
3.1.8
3.1.9
3.1.10
Acknowledgement ..........................................................................................13
Truthfulness, timeliness and clarity of communication. ..................................13
Apology ...........................................................................................................13
Recognising patient and carer expectations. .................................................14
Professional support. ......................................................................................14
Risk management and systems improvement. ..............................................14
Multidisciplinary responsibility. .......................................................................14
Clinical governance. .......................................................................................15
Confidentiality. ................................................................................................15
Continuity of care ............................................................................................15
4
Being Open Advisors ................................................................................... 15
5
Being Open Process .................................................................................... 16
5.1
Stage 1: Incident detection or recognition .................................................... 16
5.1.1
5.1.2
5.2
Patient Safety incidents which have occurred elsewhere ..............................17
Initial assessment to determine level of response .........................................17
Stage 2: Preliminary team discussion........................................................... 18
5.2.1
5.2.2
5.2.3
5.2.4
5.2.5
Timing .............................................................................................................18
Choosing the individual to communicate with the patients, their families and carers
........................................................................................................................18
Assistance with the initial Being Open discussion .........................................19
Responsibility of junior healthcare professionals ...........................................19
Involving the healthcare staff who made mistakes .........................................19
5.3
Stage 3: Initial Being Open discussions ....................................................... 20
5.4
Stage 4: Follow-up discussions .................................................................... 21
5.5
Stage 5: Process completion ........................................................................ 21
5.5.1
5.5.2
5.6
Communication with the patient, their family and carers ................................21
Continuity of care ............................................................................................21
Documentation ............................................................................................. 22
6
Patient issues to consider ............................................................................ 23
6.1
Communication ............................................................................................ 23
6.2
Advocacy and support .................................................................................. 24
6.3
Particular patient circumstances................................................................... 24
6.3.1
When a patient dies ........................................................................................24
Note: This document is electronically controlled. The master copy of the latest approved version is maintained by the owner department.
If this document is downloaded from a website or printed, it becomes uncontrolled.
Version 1.0
Printed on 06/02/2016 at 5:05 PM
Page 3 of 31
Document Title: Being Open Policy
6.3.2
6.3.3
6.3.4
6.3.5
6.3.6
6.3.7
6.3.8
7
Children ..........................................................................................................24
Patients with mental health issues .................................................................25
Patients with cognitive impairment .................................................................25
Patients with learning disabilities ....................................................................25
Patients with a different language or cultural considerations .........................25
Patients with different communication needs .................................................26
Patients who do not agree with the information provided ..............................26
Supporting staff ............................................................................................ 26
7.1
Training support ........................................................................................... 26
7.2
Monitoring .................................................................................................... 28
Appendix A – Quick reference guide to Being Open ....................................................................... 30
Note: This document is electronically controlled. The master copy of the latest approved version is maintained by the owner department.
If this document is downloaded from a website or printed, it becomes uncontrolled.
Version 1.0
Printed on 06/02/2016 at 5:05 PM
Page 4 of 31
Document Title: Being Open Policy
1
1.1
Document definition
Introduction
Being Open is a set of principles that healthcare staff should use when communicating with
patients, their families and carers following a patient safety incident in which a patient has been
harmed.
1.2
References & Further Reading
Ref.
No.
Document Title
Document Location
1
NPSA – Being Open – Communicating Patient http://www.nrls.npsa.nhs.uk/resources/?
Safety Incidents With Patients And Their Carers entryid45=65077
2
Confidentiality: NHS Code of Practice
www.connectingforhealth.nhs.uk/system
sandservices/infogov/codes
3
Records Management: NHS Code of Practice
www.dh.gov.uk/en/Publicationsandstatis
tics/Publications/PublicationsPolicyAnd
Guidance/DH_4131747
5
Code of Practice on Openness in the NHS
www.dh.gov.uk/en/Publicationsandstatis
tics/Publications/PublicationsPolicyAnd
Guidance/DH_4050490
6
Health Service Circular – Caldicott Guardians,
HSC 1999/012
www.dh.gov.uk/en/Publicationsandstatis
tics/Lettersandcirculars/Healthservicecir
culars/DH_4004311
7
Health Service Circular – Data Protection Act
1998: Protection and use of patient information
www.dh.gov.uk/en/Publicationsandstatis
tics/Lettersandcirculars/Healthservicecir
culars/DH_4002964
8
Use and Disclosure of Health Data (Guidance
on the application of the Data Protection Act
1998)
www.ico.gov.uk
9
Medical Defence Union. MDU encourages
doctors to say sorry if things go wrong. MDU,
May 2009
http://www.themdu.com/Search/hidden_Article.asp?art
icleID=1982&contentType=Media%20rel
ease&articleTitle=MDU+encourages+do
ctors+to+say+sorry+if+things+go+wrong
&userType=
10
NHS Litigation Authority. Apologies and
Explanations. NHSLA, London. May 2009
http://www.nhsla.com/NR/rdonlyres/00F
14BA6-0621-4A23-B885FA18326FF745/0/ApologiesandExplana
tions.pdf
11
Welsh Risk Pool. Technical Note 23: Apologies
and Explanations. WRP, July 2001.
http://howis.wales.nhs.uk/sites3/docmet
adata.cfm?orgid=287&id=71076
12
Incident Management Policy
Trust Intranet
13
Whistle Blowing Policy
Trust Intranet
14
Data Protection Policy
Trust Intranet
Note: This document is electronically controlled. The master copy of the latest approved version is maintained by the owner department.
If this document is downloaded from a website or printed, it becomes uncontrolled.
Version 1.0
Printed on 06/02/2016 at 5:05 PM
Page 5 of 31
Document Title: Being Open Policy
Ref.
No.
Document Title
Document Location
15
Code of Confidentiality for Employees in
Respect of Confidentiality, 2GEN-POL-025
Trust Intranet
16
Information Disclosure Policy
Trust Intranet
18
Information Security Incident Reporting
Procedure, 2ITD-PRD-001
Trust Intranet
19
Your Health Record – Protecting Your
Information, Avon NHS IM&T Consortium
Trust Intranet
20
Information Sharing Principles, Avon NHS IM&T Trust Intranet
Consortium
21
The Caldicott Principles, 4ITD-LFT-001
1.3
Trust Intranet
Glossary / Definitions
The following acronyms and abbreviations are used within the document:
AvMA
Action Against Medical Accidents
CHC
Community Health Councils
CNST
Clinical Negligence Scheme for Trusts
eForm
Electronic form used to submit reports to the NRLS
GMC
General Medical Council
ICAS
Independent Complaints Advocacy Services
IDT
Incident Decision Tree
MDU
Medical Defence Union
MORI
Market and Opinion Research International
MPS
Medical Protection Society
NHSLA
National Health Service Litigation Authority
NPSA
National Patient Safety Agency
NRLS
National Reporting and Learning System
PALS
Patient Advisory and Liaison Service
RCA
Root cause analysis
RPST
Risk Pooling Schemes for Trusts
SI
Serious Incident
WRP
Welsh Risk Pool
The following definitions are used within the document:
Adverse event
See ‘Patient safety incident’.
Anonymous
Information that has had patient identifiable features removed;
without making the information of no use for its purposes.
Apology
A sincere expression of regret offered for harm sustained.
Being open
Open communication of patient safety incidents that resulted in
moderate harm, severe harm or death of a patient while receiving
healthcare.
Note: This document is electronically controlled. The master copy of the latest approved version is maintained by the owner department.
If this document is downloaded from a website or printed, it becomes uncontrolled.
Version 1.0
Printed on 06/02/2016 at 5:05 PM
Page 6 of 31
Document Title: Being Open Policy
Carers
Family, friends or those who care for the patient. The patient has
consented to their being informed of their confidential information
and to their involvement in any decisions about their care.
Clinical governance
A framework through which NHS organisations are accountable for
continuously improving the quality of their services and safeguarding
high standards of care by creating an environment in which
excellence in clinical care will flourish.
Clinical risk manager
An officer within a trust assigned primary coordination responsibility
for issues of clinical risk management. See Risk management.
Harm
Injury (physical or psychological), disease, suffering, disability or
death.
Healthcare
professional
Doctor, dentist, nurse, pharmacist, optometrist, allied healthcare
professional, or registered alternative healthcare practitioner.
Healthcare
organisation
Organisations that provide a service to individuals or communities to
promote, maintain, monitor or restore health. See also ‘NHS
organisation’.
Injury
Damage to tissues caused by an agent or circumstance.
Intentional unsafe
acts
Incidents resulting from a criminal act, a purposefully unsafe act, or
an act related to alcohol/substance abuse by a care provider. These
are dealt with through performance management and local systems.
Liability
Legal responsibility for an action or event.
National Reporting
and Learning System
(NRLS)
A confidential and anonymous computer-based system developed
by the NPSA for the collection and analysis of patient safety incident
information. It receives incident reports from NHS organisations,
staff and contractor professions and, in time, patients and carers.
Near miss
See ‘Prevented patient safety incident’.
NHS-funded
healthcare
See ‘NHS organisation’
NHS organisation
Any area where NHS-funded patients are treated, i.e., NHS
establishments or services, independent establishments including
private healthcare or the patient’s home or workplace. Either all or
part of the patient’s care in these settings is funded by the NHS.
This may also be referred to as NHS-funded healthcare.
NPSA
The National Patient Safety Agency was set up in July 2001
following recommendations from the Chief Medical Officer in his
report on patient safety, An organisation with a memory. Its role is
to improve the safety of patients by promoting a culture of reporting
and learning from patient safety incidents.
Patient safety
The process by which an organisation makes patient care safer.
This should involve risk assessment, the identification and
management of patient related risks, the reporting and analysis of
incidents, and the capacity to learn from and follow up on incidents
and implement solutions to minimise the risk of them recurring. The
term ‘patient safety’ is replacing ‘clinical risk’, ‘non-clinical risk’ and
the ‘health and safety of patients’.
Note: This document is electronically controlled. The master copy of the latest approved version is maintained by the owner department.
If this document is downloaded from a website or printed, it becomes uncontrolled.
Version 1.0
Printed on 06/02/2016 at 5:05 PM
Page 7 of 31
Document Title: Being Open Policy
Patient safety
incident
Any unintended or unexpected incident that could have or did lead
to harm for one or more patients receiving NHS-funded healthcare.
The terms ‘patient safety incident’ and ‘prevented patient safety
incident’ will be used to describe ‘adverse events’ / ‘clinical errors’
and ‘near misses’ respectively.
Prevented patient
safety incident
Any unexpected or unintended incident that was prevented, resulting
in no harm to one or more patients receiving NHS-funded
healthcare.
Risk
The chance of something happening that will have an impact on
individuals and/or organisations.
It is measured in terms of
likelihood and consequences.
Risk management
Identifying, assessing, analysing, understanding and acting on risk
issues in order to reach an optimal balance of risk, benefit and cost.
Root cause analysis
(RCA)
A systematic process whereby the factors that contributed to an
incident are identified. As an investigation technique for patient
safety incidents, it looks beyond the individual concerned and seeks
to understand the underlying causes and environmental context in
which an incident happened.
Safety
A state in which risk has been reduced to an acceptable level.
Standard
Sets out agreed specifications and/or procedures designed to
ensure that a material, product, method or service is fit for the
purpose and consistently performs in the way it is intended.
Significant event
audit (SEA)
An audit process where data is collected on specific types of
incidents that are considered important to learn about and improve
patient safety.
Suffering
Experiencing anything subjectively unpleasant. This may include
pain, malaise, nausea and/or vomiting, loss, depression, agitation,
alarm, fear, grief, or humiliation.
Systems failure
A fault, breakdown or dysfunction within operational methods,
processes or infrastructure.
Systems
improvement
The changes made to improve operational methods, processes and
infrastructure to ensure better quality and safety.
Treatment
Broadly, the management and care of a patient to prevent or cure
disease or reduce suffering and disability.
1.4
Purpose
Being Open is a process rather than a one-off event. With this in mind, ten principles have been
drawn up to underpin the policy. Some of the principles listed are discussed in more detail in
subsequent sections of this policy document.
This policy provides guidance for Health Care staff on the principles of open communication with
patients and carers following patient safety incidents. This policy should be followed in conjunction
with the Incident Management Policy in the event of patient safety incidents which have resulted in
harm.
Note: This document is electronically controlled. The master copy of the latest approved version is maintained by the owner department.
If this document is downloaded from a website or printed, it becomes uncontrolled.
Version 1.0
Printed on 06/02/2016 at 5:05 PM
Page 8 of 31
Document Title: Being Open Policy
1.5
Scope
The scope of this document is Trust wide and applies to the wider organisation encompassing
Wiltshire Community Health Services
In the case of near miss or no harm incidents, patients are not usually contacted or involved in
investigations and these types of incidents are outside the scope of the Being Open policy.
1.6
Regulatory Position
1.7
Data Protection Act 1998
Human Rights Act 1998
Freedom of Information Act 2000
Care Quality Commission Outcome 4
NHSLA Risk Management Standards
Special Cases
None.
1.8
Comments
Any comments on this document should, in the first instance, be addressed to the Clinical Risk
Manager.
Note: This document is electronically controlled. The master copy of the latest approved version is maintained by the owner department.
If this document is downloaded from a website or printed, it becomes uncontrolled.
Version 1.0
Printed on 06/02/2016 at 5:05 PM
Page 9 of 31
Document Title: Being Open Policy
2
Roles and Responsibilities
Trust Board
The Trust board retains corporate responsibility for the Being Open policy.
Ensuring that a Being open policy is in place and fully implemented
throughout the organisation
Chief Executive
The Chief Executive has overall responsibility for Being Open within the
Trust, ensuring that the principles and policy are embedded in the
organisation The Chief Executive will fulfil this responsibility by leading by
example in fostering a culture of fair blame and non-punitive reporting
within the Trust.
The Chief Executive will be made aware of individual serious incidents via
the Medical Director and the Director of Workforce and Education.
Non-Executive
Director
Medical Director
Associate Director of
Quality and Patient
Safety
Investigation
Executive lead
Investigation Lead
The Chair of the Patient Safety and Quality Committee is responsible for
ensuring that the Being Open principles and policy are embedded in the
organisation.
The Medical Director will be made aware of all serious incidents. They
have executive responsibility for ensuring that these incidents are
managed, external reports made as necessary and investigations
undertaken appropriately and that the Being Open policy is implemented
and forms part of the incident management process.
The post maintains an overview of all incidents and ensures a robust
monitoring and reporting system is in place.
The post also oversees and ensures serious incident reports inform the
clinical and corporate governance committees.
An Executive lead will be identified for each Serious Incident investigation.
They are responsible for identifying the Lead Investigator in conjunction
with the Clinical Risk Team, overseeing the investigation and for ensuring
that Being Open is an integral part of the incident management process.
An Investigation Lead will be identified by the Investigation Lead Executive
for all Serious Incidents. The Lead Investigator should be a member of
staff who has undertaken incident investigation training or equivalent
experience. The Lead Investigator will usually be identified within the
directorate in which the incident occurred but outside of the immediate
speciality or department.
The Investigation Lead is responsible for ensuring the robust investigation
of an incident and for ensuring that Being Open forms an integral part of
the incident management process.
Patient Safety and
Quality Committee
(PSQC)
The Patient Safety and Quality Committee function is to improve quality
and reduce clinical risk by co-ordinating the implementation and monitoring
of cross directorate clinical governance and clinical risk management.
They will review all serious incidents on a monthly basis and make
recommendations for directorate and organisational improvements in
clinical practice.
Being Open Advisors
Provide mentoring and support to colleagues. A Being Open advisor should
only be asked to lead Being Open discussions when appropriate. Their
Note: This document is electronically controlled. The master copy of the latest approved version is maintained by the owner department.
If this document is downloaded from a website or printed, it becomes uncontrolled.
Version 1.0
Printed on 06/02/2016 at 5:05 PM
Page 10 of 31
Document Title: Being Open Policy
primary role is to provide support to their colleagues in implementing Being
Open.
Senior managers
(e.g. modern
matrons, AMDs,
general managers)
On notification of an adverse incident the senior line manager, must ensure
that all appropriate steps have been taken and that the situation has been
made safe. They must insure that the Incident Management Policy and
Being Open policies are followed within their directorate and that staff are
adequately supported to implement the polices effectively.
Responsible for ensuring that staff within the directorate are provided
opportunity to access short term and long term support following a patient
safety incident, complaint or claim.
Line managers
On notification of an adverse incident the line manager, must ensure that
the situation has been made safe and that the incident is managed in line
with the Incident Management Policy.
They are responsible for ensuring that the Being Open process described
within this policy is followed for all low and moderate harm incidents.
As a line manager they have responsibility for ensuring that all staff
reportable to them have adequate immediate and ongoing support
following a patient safety incident, complaint or claim.
All staff
The Being Open policy applies to all staff that have key roles in patient’s
care.
Clinical Risk Team
The Clinical Risk Team are responsible for advising on and ensuring
compliance with the Incident Management and Being Open policies
throughout the organisation.
The Clinical Risk Manager will champion the Being Open Policy and act as
a Being Open advisor.
Patient Advice and
Liaison Service
(PALS)
Responsible for highlighting patient safety incidents to the clinical risk,
litigation and health and safety teams which are uncovered through the
complaints procedures.
Ensuring that the principles and processes described in the Being Open
policy are considered as part of the management of complaints. See Also
Trust Complaints Policy.
The Head of Patient Experience will champion the Being Open Policy and
act as a Being Open advisor within the Trust.
Note: This document is electronically controlled. The master copy of the latest approved version is maintained by the owner department.
If this document is downloaded from a website or printed, it becomes uncontrolled.
Version 1.0
Printed on 06/02/2016 at 5:05 PM
Page 11 of 31
Document Title: Being Open Policy
3 Introduction
Being Open is a set of principles that healthcare staff should use when communicating with
patients, their families and carers following a patient safety incident in which a patient has been
harmed.
Being Open involves:
• acknowledging, apologising and explaining when things go wrong;
• conducting a thorough investigation into the incident and reassuring patients, their families and
carers that lessons learned will help prevent the incident recurring;
• providing support for those involved to cope with the physical and psychological consequences of
what happened.
In 2005, the National Patient Safety Agency (NPSA) issued a Safer Practice Notice advising the
NHS to develop a local Being Open policy and to raise awareness of this policy with all healthcare
staff.
In November 2009 the NPSA published the revised Being Open framework in order to strengthen
the Being Open throughout the NHS.
Communicating effectively with patients, their families and carers is a vital part of the process of
dealing with patient safety incidents in healthcare. Research has shown that patients are more likely
to forgive medical errors when they are discussed in a timely and thoughtful manner and that Being
Open can decrease the trauma felt by patients following a patient safety incident.
Openness also has benefits for healthcare professionals as it can: help to reduce stress through the
use of a formalised, honest, communication method; alleviate the fear of ‘being found out’; and
improve job satisfaction by:
ensuring that communication with patients, their families and carers has been handled in the
most appropriate way;
helping the healthcare professional to develop a good professional reputation for handling
difficult situation properly;
improving the healthcare professional’s understanding of incidents from the perspective of
the patient, their family and carers.
The benefits of Being Open are widely recognised and supported by policy makers, professional
bodies, and litigation and indemnity bodies, including the Department of Health, General Medical
Council (GMC), National Health Service Litigation Authority (NHSLA), Medical Defence Union
(MDU) and the Medical Protection Society (MPS).
The NHS Constitution for England embeds the principles of Being Open as a pledge to patients in
relation to complaints and redress. It states:
”The NHS also commits when mistakes happen to acknowledge them, apologise,
explain what went wrong and put things right quickly and effectively.”
The Constitution recommends that staff should view the services they provide from the standpoint of
a patient, and involve patients, their families and carers in the services they provide, working with
them, their communities and other organisations.
The work of the Welsh project ‘Putting Things Right’ and its interim guidance (September 2009)
echo these messages.
The GMC in their handbook Good Medical Practice also advises that:
Note: This document is electronically controlled. The master copy of the latest approved version is maintained by the owner department.
If this document is downloaded from a website or printed, it becomes uncontrolled.
Version 1.0
Printed on 06/02/2016 at 5:05 PM
Page 12 of 31
Document Title: Being Open Policy
“If a patient under your care has suffered serious harm, through misadventure, or for any other
reason, you should act immediately to put matters right, if that is possible. You should explain fully
to the patient what has happened and the likely long and short-term effects. When appropriate you
should offer an apology”
Fear of legal action may be preventing some healthcare professionals from being open with
patients, but the MDU, MPS, NHSLA and Welsh Risk Pool have all issued recent guidance to
reassure healthcare professionals that they are not admitting liability if they apologise when
something has gone wrong
Appendix A summarises Quick Reference Guide to Being Open When Patients Are Harmed.
3.1
The principles of Being Open
The following set of principles has been developed to help healthcare organisations create and
embed a culture of Being Open.
3.1.1
Acknowledgement
All patient safety incidents should be acknowledged and reported as soon as they are identified.
3.1.2
Truthfulness, timeliness and clarity of communication.
Information about a patient safety incident must be given to patients and/or their carers in a truthful
and open manner by an appropriate person. Patients want a step-by-step explanation of what
happened, that considers their individual needs and is delivered openly.
Communication should also be timely: patients and/or their carers should be provided with
information about what happened as soon as practicable. It is also essential that any information
given is based solely on the facts known at the time. Healthcare staff should explain that new
information may emerge as an incident investigation is undertaken, and patients and/or their carers
should be kept up-to-date with the progress of an investigation.
Patients and/or their carers should receive clear, unambiguous information and be given a single
point of contact for any questions or requests they may have. They should not receive conflicting
information from different members of staff, and using medical jargon which they may not
understand should be avoided.
3.1.3
Apology
Patients and/or their carers should receive a sincere expression of regret for the harm that has
resulted from a patient safety incident. This should be in the form of an appropriately worded and
agreed manner of apology, as early as possible. Both verbal and written apologies should be given.
Based on the circumstances, clinical teams and/or, in the case where a patient has suffered severe
harm or death, incident investigation leads should decide on the most appropriate member of staff
to issue these apologies to patients and/or their carers. The decision should consider seniority,
relationship to the patient, and experience and expertise in the type of patient safety incident that
has occurred. Verbal apologies are essential because they allow face-to-face contact between the
patient and/or their carers and the healthcare team. This should be given as soon as staff are
aware an incident has occurred. It is important not to delay for any reason, including: setting up a
more formal multi-disciplinary Being Open discussion with the patient and/or their carers; fear and
apprehension; or lack of staff availability. Delays are likely to increase the patient’s and/or their
carer’s sense of anxiety, anger or frustration.
Note: This document is electronically controlled. The master copy of the latest approved version is maintained by the owner department.
If this document is downloaded from a website or printed, it becomes uncontrolled.
Version 1.0
Printed on 06/02/2016 at 5:05 PM
Page 13 of 31
Document Title: Being Open Policy
A written apology, which clearly states the Trust is sorry for the suffering and distress resulting from
the incident, must also be given.
3.1.4
Recognising patient and carer expectations.
Patients and/or their carers can reasonably expect to be fully informed of the issues surrounding a
patient safety incident, and its consequences, in a face-to-face meeting with representatives from
the Trust. They should be treated sympathetically, with respect and consideration. Confidentiality
must be maintained at all times. Patients and/or their carers should also be provided with support in
a manner appropriate to their needs. This involves consideration of special circumstances that can
include a patient requiring additional support, such as an independent patient advocate or a
translator.
Where appropriate, information on the Patient Advisory and Liaison Service (PALS) in England, the
Community Health Councils (CHC) in Wales and other relevant support groups like Cruse
Bereavement Care (www.crusebereavementcare.org.uk/) and Action against Medical Accidents
(AvMA) should be given to the patient as soon as it is possible.
3.1.5
Professional support.
The Trust supports an environment in which all staff, whether directly employed or independent
contractors, are encouraged to report patient safety incidents. Staff should expect to feel supported
throughout the incident investigation process because they too may have been traumatised by
being involved. They should not be unfairly exposed to punitive disciplinary action, increased
medico-legal risk or any threat to their registration.
To ensure a robust and consistent approach to incident investigation, the Trust advocates the use of
the NPSA’s incident decision tree (IDT). The IDT has been developed as an aid to improve the
consistency of decision making about whether human error or systems failures contributed to an
incident. It is designed for use by anyone who has the authority to exclude a member of staff from
work following a patient safety incident (including medical and nursing directors, chief executives
and human resources staff).
More details can be found on the NPSA website:
http://www.nrls.npsa.nhs.uk/resources/type/toolkits/?q=0%c2%acroot%c2%ac&entryid45=59900
Where there is reason for the healthcare organisation to believe a member of staff has committed a
punitive or criminal act, the trust will take steps to preserve its position, and advise the member(s) of
staff at an early stage to enable them to obtain separate legal advice and/or representation.
The Trust also encourages staff to seek support from relevant professional bodies such as the
General Medical Council, Royal Colleges, the Medical Protection Society, the Medical Defence
Union and the Nursing and Midwifery Council.
3.1.6
Risk management and systems improvement.
Root cause analysis (RCA), or similar techniques should be used to uncover the underlying causes
of a patient safety incident. Investigations should focus on improving systems of care, which will
then be reviewed for their effectiveness.
3.1.7
Multidisciplinary responsibility.
Where multi-disciplinary teams are involved, communication with patients and/or their carers
following an incident that led to harm, should reflect this. This will ensure that the Being Open
process is consistent with the philosophy that incidents usually result from systems failures and
rarely from the actions of an individual.
Note: This document is electronically controlled. The master copy of the latest approved version is maintained by the owner department.
If this document is downloaded from a website or printed, it becomes uncontrolled.
Version 1.0
Printed on 06/02/2016 at 5:05 PM
Page 14 of 31
Document Title: Being Open Policy
3.1.8
Clinical governance.
Being Open requires the support of patient safety and quality improvement processes through
clinical governance frameworks, in which patient safety incidents are investigated and analysed, to
find out what can be done to prevent their recurrence.
3.1.9
Confidentiality.
The procedures for Being Open must give full consideration of, and respect for, the patient’s and/or
their carer’s and staff privacy and confidentiality. Communications with parties outside of the clinical
team should be on a strictly need-to-know basis and, where practicable, records should be
anonymous. Details of a patient safety incident should at all times be considered confidential. In
addition, it is good practice to inform the patient and/or their carers about who will be involved in the
investigation before it takes place.
3.1.10 Continuity of care
Patients are entitled to expect they will continue to receive all usual treatment and continue to be
treated with respect and compassion. If a patient expresses a preference for their healthcare needs
to be taken over by another team, the appropriate arrangements should be made for them to
receive treatment elsewhere. A key part of Being Open is considering the patient’s needs or the
needs of their carers or family in circumstances where the patient has died.
4 Being Open Advisors
The NPSA requires that Trusts identify individuals to mentor and support fellow clinicians. The
Directorate Associate Medical Directors, Director of Transition, Clinical Risk Manager, Medical
Director, Director of Nursing and Midwifery and the Head of Patient Experience can be contacted for
advice and support with the Being Open process. In the event of severe harm or death of a patient
resulting from a patient safety incident, advice should always be sought prior to any Being Open
communication.
A Being Open Advisor should only be asked to lead Being Open discussions when appropriate.
Their primary role is to provide support to their colleagues in implementing Being Open.
Being Open Advisors should:
• Support fellow healthcare professionals with Being Open by:
–– mentoring colleagues during their first Being Open discussion;
–– advising on the Being Open process;
–– being accessible to colleagues prior to initial and subsequent Being Open discussions;
–– facilitating the initial team meeting to discuss the incident when appropriate;
–– signposting the support services within the organisation for colleagues involved in Being Open
discussions;
–– facilitating debriefing meetings following Being Open discussions;
–– mentoring colleagues to become Being Open advisors
• Support fellow healthcare professionals in dealing with patient safety incidents by:
–– signposting the support services within the organisation for colleagues involved in patient safety
incident discussions;
–– advising on the reporting system for patient safety incidents.
• Practice and promote the principles of Being Open.
For further information about this role please see the supporting resources on the NRLS website at:
www.nrls.npsa.nhs.uk/beingopen
Note: This document is electronically controlled. The master copy of the latest approved version is maintained by the owner department.
If this document is downloaded from a website or printed, it becomes uncontrolled.
Version 1.0
Printed on 06/02/2016 at 5:05 PM
Page 15 of 31
Document Title: Being Open Policy
5 Being Open Process
Being Open is a process rather than a one off event. There are a number of stages in the process.
The duration depends on the incident, the needs of the patient, their family and carers, and how the
investigation into the incident progresses.
Figure 1
5.1
Stage 1: Incident detection or recognition
The Being Open process begins with the recognition that a patient has suffered harm or has died as
a result of a patient safety incident. Incidents may be identified by:
A member of staff at the time of the incident;
A member of staff retrospectively when an unexpected outcome is detected;
Outside the incident reporting process usually by way of a complaint, legal claim, Coroner’s
Officer or media interest;
A patient, their family or carers who express concern or dissatisfaction with the patient’s
healthcare either at the time of the incident or retrospectively;
Incident detection systems such as incident reporting or medical records review;
Other sources such as detection by other patients, visitors or non-clinical staff(for example,
researchers observing healthcare staff)
As soon as a patient safety incident is identified, the top priority is prompt and appropriate clinical
care. The incident should be reported in line with the Incident Management Policy.
Note: This document is electronically controlled. The master copy of the latest approved version is maintained by the owner department.
If this document is downloaded from a website or printed, it becomes uncontrolled.
Version 1.0
Printed on 06/02/2016 at 5:05 PM
Page 16 of 31
Document Title: Being Open Policy
5.1.1
Patient Safety incidents which have occurred elsewhere
A patient safety incident may have occurred in an organisation other that the one in which it is
identified. The individual who identifies the possibility of an earlier patient safety incident should
complete an electronic incident form (or paper IR1/RM1).The Clinical Risk and Health and Safety
teams will then contact their equivalent at the organisation where the incident occurred.
The Being Open process and the investigation and analysis of a patient safety incident should
normally occur in the healthcare organisation where the incident took place.
5.1.2
Initial assessment to determine level of response
All incidents should be assessed initially by the healthcare team to determine the level of response
required, the level of response to a patient safety incident depends on the nature of the incident.
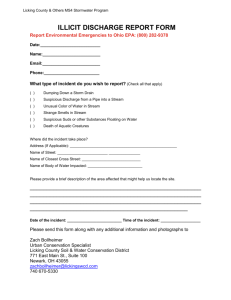
Figure 2 Grading of patient safety incidents to determine level of Being Open response
Incident
No
harm
(including
prevented
near
miss
patient safety incidents)
Low harm - short term
injury resolved in about 1
month, lacerations.
Moderate harm - semipermanent injury that
will take at least a year to
resolve,
includes
emotional, psychological
or physical harm..
Severe harm or death –
longterm or permanent
harm, such as brain
damage or disability.
Level of response
Patients are not usually contacted or involved in investigations,
these types of incidents are outside the scope of the Being
Open policy.
Unless there are specific indications or the patient requests it,
the communication, investigation and analysis, and the
implementation of changes will occur at local department level
with the participation of those directly involved in the incident.
Reporting to the Clinical Risk Manager will occur through the
incident reporting system and be analysed to detect themes.
Review will occur through local investigation as described
within the Incident Management Policy.
Communication should normally take the form of an open
discussion between the staff providing the patient’s care and
the patient, their family and carers
Apply the principles of Being Open
Summary of Being Open communication should be
documented on the corresponding incident form.
A higher level of response is required in these circumstances.
Being Open discussions will normally take the form of an open
discussion between the staff providing the patient’s care and
the patient, their family. The Trust Being Open advisors
(Directorate Associate Medical Director, Clinical Risk Manager,
Medical Director, Director of Nursing and Midwifery or the Head
of Patient Experience) can be contacted prior to any Being
Open communication taking place.
Apply the principles of Being Open
Summary of Being Open communication should be
documented on the corresponding incident form.
Patient safety incidents resulting in severe harm or death are
reported and managed as Serious Incidents in line with the
Incident Management policy. The Trust Being Open advisors
(Directorate Associate Medical Director, Clinical Risk Manager,
Medical Director, Director of Nursing and Midwifery or the Head
of Patient Experience) must be contacted prior to any Being
Open communication taking place. The Executive Lead and
Lead Investigator will be responsible for overseeing the Being
Note: This document is electronically controlled. The master copy of the latest approved version is maintained by the owner department.
If this document is downloaded from a website or printed, it becomes uncontrolled.
Version 1.0
Printed on 06/02/2016 at 5:05 PM
Page 17 of 31
Document Title: Being Open Policy
Open process.
Apply the principles of Being Open
A summary of Being Open communications will be
included within the incident investigation report.
5.2
Stage 2: Preliminary team discussion
The multidisciplinary team, including the most senior health professional involved in the patient
safety incident, should meet as soon as possible after the event to:
5.2.1
establish the basic clinical and other facts;
assess the incident to determine the level of immediate response;
identify who will be responsible for discussion with the patient, their family and carers. In the
case of severe injury or death the Executive lead and Lead investigator for the Serious
Incident will be responsible for overseeing the Being Open process and will agree who will
meet with the patient, their family and carers;
consider the appropriateness of engaging patient support at this early stage. This includes
the use of a facilitator, a patient advocate or a healthcare professional who will be
responsible for identifying the patient’s needs and communicating them back to the
healthcare team;
identify immediate support needs for the healthcare staff involved;
ensure there is a consistent approach by all team members around discussions with the
patient, their family and carers.
Timing
The initial Being Open discussion with the patient, their family and carers should occur as soon as
possible after recognition of the patient safety incident. Factors to consider when timing this
discussion include:
clinical condition of the patient;
patient preference (in terms of when and where the meeting takes place and which
healthcare professional leads the discussion);
privacy and comfort of the patient;
availability of the patient’s family and/or carers;
availability of key staff involved in the incident and in the Being open process;
availability of support staff, for example a translator or independent advocate, if required;
arranging the meeting in a sensitive location.
5.2.2
Choosing the individual to communicate with the patients, their families and carers
In the case of low and moderate harm incidents this should be the most senior person responsible
for the patient’s care and/or someone with experience and expertise in the type of incident that has
occurred. This could either be the patient’s consultant, nurse consultant, or any other healthcare
professional who has a designated caseload of patients.
In the case of severe harm or death incidents the Executive Lead and Lead investigator will be
responsible for ensuring that the most appropriate person communicates with the patient.
They should have received training in communication of patient safety incidents.
Consideration also needs to be given to the characteristics of the person nominated to lead the
Being Open process. They should:
ideally be known to, and trusted by, the patient, their family and carers;
have a good grasp of the facts relevant to the incident;
Note: This document is electronically controlled. The master copy of the latest approved version is maintained by the owner department.
If this document is downloaded from a website or printed, it becomes uncontrolled.
Version 1.0
Printed on 06/02/2016 at 5:05 PM
Page 18 of 31
Document Title: Being Open Policy
5.2.3
be senior enough or have sufficient experience and expertise in relation to the type of patient
safety incident to be credible to patients, their families and carers, and colleagues;
have excellent interpersonal skills, including being able to communicate with patients, their
families and carers in a way they can understand, and avoiding excessive use of medical
jargon;
be willing and able to offer a meaningful apology, reassurance and feedback to patients,
their families and carers;
be able to maintain a medium to long-term relationship with the patient, their family and
carers, where possible, and to provide continued support and information;
be culturally aware and informed about the specific needs of the patient, their family and
carers.
Assistance with the initial Being Open discussion
The healthcare professional communicating information about a patient safety incident should be
able to nominate a colleague to assist them with the meeting. Ideally this would be someone with
experience or training in communication and Being Open procedures.
5.2.4
Responsibility of junior healthcare professionals
Junior staff or those in training should not lead the Being Open process except when all of the
following criteria have been considered:
the incident resulted in low harm;
they have expressed a wish to be involved in the discussion with the patient, their family and
carers;
the senior healthcare professional responsible for the care is present for support;
the patient, their family and carers agree.
Where a junior healthcare professional who has been involved in a patient safety incident asks to be
involved in the Being Open discussion, it is important that they are accompanied and supported by
a senior team member. It is unacceptable for junior staff to communicate patient safety information
alone, or to be delegated the responsibility to lead a Being Open discussion unless they volunteer
and their involvement takes place in appropriate circumstances (i.e. they have received appropriate
training and mentorship for this role).
5.2.5
Involving the healthcare staff who made mistakes
Some patient safety incidents that resulted in moderate harm, severe harm or death can result from
errors made by healthcare staff while caring for the patient. In these circumstances, the member(s)
of staff involved may or may not wish to participate in the Being Open discussion with the patient,
their family and carers.
Every case where an error has occurred needs to be considered individually, balancing the needs of
the patient, their family and carers with those of the healthcare professional concerned. In cases
where the healthcare professional who has made an error wishes to attend the discussion to
apologise personally, they should feel supported by their colleagues throughout the meeting. In
cases where the patient, their family and carers express a preference for the healthcare
professional not to be present, it is advised that a personal written apology is handed to the patient,
their family and carers during the initial Being Open discussion.
Note: This document is electronically controlled. The master copy of the latest approved version is maintained by the owner department.
If this document is downloaded from a website or printed, it becomes uncontrolled.
Version 1.0
Printed on 06/02/2016 at 5:05 PM
Page 19 of 31
Document Title: Being Open Policy
5.3
Stage 3: Initial Being Open discussions
The initial Being Open discussion is the first part of an ongoing communication process. Many of the
points raised here should be expanded on in subsequent meetings with the patient, their family and
carers.
The patient, their family and carers should be advised of the identity and role of all people attending
the Being Open discussion before it takes place. This allows them the opportunity to state their own
preferences about which healthcare staff they want to be present.
If for any reason it becomes clear during the initial discussion that the patient would prefer to speak
to a different healthcare professional, the patient’s wishes should be respected. A substitute with
whom the patient is satisfied should be provided.
It should be recognised that patients, their families and carers may be anxious, angry and frustrated
even when the Being Open discussion is conducted appropriately.
The content of the initial Being Open discussion with the patient, their family and carers should
cover the following:
An expression of genuine sympathy, regret and a meaningful apology for the harm that has
occurred.
The facts that are known as agreed by the multidisciplinary team. Where there is
disagreement, communication about these events should be deferred until after the
investigation has been completed.
The patient, their family and carers are informed that an incident investigation is being
carried out and more information will become available as it progresses.
The patient’s, their family’s and carers’ understanding of what happened is taken into
consideration, as well as any questions they may have.
Consideration and formal noting of the patient’s, their family’s and carers’ views and
concerns, and demonstration that these are being heard and taken seriously.
Appropriate language and terminology are used when speaking to patients, their families
and carers. For example, using the terms ‘patient safety incident’ or ‘adverse event’ may be
meaningless or even insulting to some patients, their families and their carers. If a patient’s
first language is not English, it is also important to consider their language needs – if they
would like the Being Open discussion conducted in French or Urdu for example, this should
be arranged.
An explanation about what will happen next in terms of the short through to long-term
treatment plan and incident analysis findings.
Information on likely short and long-term effects of the incident (if known). The long term
effects may have to be presented at a subsequent meeting when more is known.
An offer of practical and emotional support for the patient, their family and carers. This may
involve getting help from third parties such as charities and voluntary organisations, as well
as offering more direct assistance. Information about the patient and the incident should not
normally be disclosed to third parties without consent.
Information on services offered by all the possible support agencies (including their contact
details) that can give emotional support, help the patient identify the issues of concern,
support them at meetings with staff and provide information about appropriate community
services.
Contact details of a staff member who will maintain an ongoing relationship with the patient,
using the most appropriate method of communication from the patient’s, their family’s and
carers’ perspective. Their role is to provide both practical and emotional support in a timely
manner.
It is essential that the following does not occur during the Being Open discussion:
Note: This document is electronically controlled. The master copy of the latest approved version is maintained by the owner department.
If this document is downloaded from a website or printed, it becomes uncontrolled.
Version 1.0
Printed on 06/02/2016 at 5:05 PM
Page 20 of 31
Document Title: Being Open Policy
5.4
speculation;
attribution of blame;
denial of responsibility;
provision of conflicting information from different individuals.
Stage 4: Follow-up discussions
Follow-up discussions with the patient, their family and carers are an important step in the Being
Open process. Depending on the incident and the timeline for the investigation there may be more
than one follow-up discussion.
The following guidelines will assist in making the communication effective:
The discussion occurs at the earliest practical opportunity.
Consideration is given to the timing of the meeting, based on both the patient’s health and
personal circumstances.
Consideration is given to the location of the meeting, for example at the patient’s home.
Feedback is given on progress to date and information provided on the investigation
process.
There should be no speculation or attribution of blame. Similarly, the healthcare professional
communicating the incident must not criticise or comment on matters outside their own
experience.
The patient, their family and carers should be offered an opportunity to discuss the situation
with another relevant professional where appropriate.
A written record of the discussion is kept and shared with the patient, their family and carers.
All queries are responded to appropriately.
If completing the process at this point, the patient, their family and carers should be asked if
they are satisfied with the investigation and a note of this made in the patient’s records.
The patient is provided with contact details so that if further issues arise later there is a
conduit back to the relevant healthcare professionals or an agreed substitute.
5.5
5.5.1
Stage 5: Process completion
Communication with the patient, their family and carers
After completion of the incident investigation, feedback should take the form most acceptable to the
patient. Whatever method is used, the communication should include:
the chronology of clinical and other relevant facts;
details of the patient’s, their family’s and carers’ concerns and complaints;
a repeated apology for the harm suffered and any shortcomings in the delivery of care that
led to the patient safety incident;
a summary of the factors that contributed to the incident;
information on what has been and will be done to avoid recurrence of the incident and how
these improvements will be monitored.
It is expected that in most cases there will be a complete discussion of the findings of the
investigation and analysis. In some cases information may be withheld or restricted, for example, in
the rare instances where communicating information will adversely affect the health of the patient;
where investigations are pending coronial processes; or where specific legal requirements preclude
disclosure for specific purposes. In these cases the patient must be informed of the reasons for the
restrictions.
5.5.2
Continuity of care
When a patient has been harmed during the course of treatment and requires further therapeutic
management or rehabilitation, they should be informed, in an accessible way, of the ongoing clinical
Note: This document is electronically controlled. The master copy of the latest approved version is maintained by the owner department.
If this document is downloaded from a website or printed, it becomes uncontrolled.
Version 1.0
Printed on 06/02/2016 at 5:05 PM
Page 21 of 31
Document Title: Being Open Policy
management plan. This may be encompassed in discharge planning policies addressed to
designated individuals, such as the referring GP, when the patient safety incident has not occurred
in primary care.
Patients, their families and carers need to be reassured that they will continue to be treated
according to their clinical needs, even in circumstances where there is a dispute between them and
the healthcare team. They should also be informed that they have the right to continue their
treatment elsewhere if they prefer.
Communication with the GP and other community care service providers for patient safety incidents
not occurring in primary care
Wherever possible, it is advisable to send a brief communication to the patient’s GP, before
discharge, describing what happened.
When the is discharged, the discharge letter should also be forwarded to the GP or appropriate
community care service. It should contain summary details of:
the nature of the patient safety incident and the continuing care and treatment;
the current condition of the patient;
key investigations that have been carried out to establish the patient’s clinical condition;
recent results;
prognosis.s
It may be valuable to include the GP in one of the follow-up discussions either at discharge or at a
later stage.
5.6
Documentation
Throughout the Being Open process it is important to record discussions with the patient, their
family and carers as well as the incident investigation.
In the case of Low and moderate harm incidents a summary of Being Open communication should
be documented on the corresponding incident form. The electronic incident reporting form includes
a mandatory Being Open section.
In the case of Serious harm incidents a summary of Being Open communication should be
documented on the corresponding incident form and in addition documentation of communications
will be included within the Root Cause Analysis investigation report.
Patient safety incident documentation should include:
incident report (electronic incident report form or paper IR1/RM1)
records of the investigation and analysis process (electronic managers form
IR1/RM1) .
or paper
Written records of the Being Open discussions may consist of:
the time, place and date, as well as the name and relationships of all attendees;
the plan for providing further information to the patient, their family and carers;
offers of assistance and the patient’s, their family’s and carers’ response;
questions raised by the family and carers, and the answers given;
plans for follow-up meetings;
progress notes relating to the clinical situation and an accurate summary of all the points
explained to the patient, their family and carers;
copies of letters sent to the patient, their family and carers, and the GP for patient safety
incidents not occurring within primary care;
copies of any statements taken in relation to the patient safety incident;
a copy of the incident report.
Note: This document is electronically controlled. The master copy of the latest approved version is maintained by the owner department.
If this document is downloaded from a website or printed, it becomes uncontrolled.
Version 1.0
Printed on 06/02/2016 at 5:05 PM
Page 22 of 31
Document Title: Being Open Policy
A summary of the Being Open discussions should be shared with the patient, their family and
carers.
6 Patient issues to consider
6.1
Communication
For open and effective communication following patient safety incidents, staff responsible for
undertaking Being Open discussions should:
Ensure early identification of, and consent for, the patient’s practical and emotional needs,
including:
the names of people who can provide assistance and support to the patient, and to
whom the patient has agreed that information about their healthcare can be given.
This person (or people) may be different to both the patient’s next of kin and from
people who the patient had previously agreed should receive information about their
care prior to the patient safety incident;
any special restrictions on openness that the patient would like the healthcare team
to respect;
identifying whether the patient does not wish to know every aspect of what went
wrong; respect their wishes and reassure them that this information will be made
available if they change their mind later on.
Provide repeated opportunities for the patient, their family and carers to obtain information
about the patient safety incident.
Provide information to patients in verbal and/ or written format.
Provide assurance that an ongoing care plan will be developed in consultation with the
patient and will be followed through.
Provide assurance that the patient will continue to be treated according to their clinical needs
and that the prospect of, or an actual dispute between, the patient, their family and carers
and the healthcare team will not affect their access to treatment.
Facilitate inclusion of the patient’s family and carers in discussions about a patient safety
incident where the patient agrees.
Provide the patient’s family and carers with access to information to assist in making
decisions if the patient is unable to participate in decision making or if the patient has died as
a result of an incident. This should be done with regard to confidentiality and in accordance
with the patient’s instructions.
Determine whether you will need to repeat this information to the patient at different times to
allow them to comprehend the situation fully.
Ensure that the patient’s family and carers are provided with known information, care and
support if a patient has died as a result of a patient safety incident. The carers should also
be referred to the coroner for more detailed information.
Ensure that discussions with the patient, their family and carers are documented and that
information is shared with them.
Ensure that the patient, their family and carers are provided with information on the
complaints procedure if they wish to have it.
Ensure that the patient, their family and carers are provided with information on the incident
reporting process.
Ensure that the patient’s account of the events leading up to the patient safety incident is fed
into the incident investigation, whenever applicable.
Ensure that the patient, their family and carers are provided with information on how
improvement plans derived from investigations will be implemented and their effects
monitored.
Note: This document is electronically controlled. The master copy of the latest approved version is maintained by the owner department.
If this document is downloaded from a website or printed, it becomes uncontrolled.
Version 1.0
Printed on 06/02/2016 at 5:05 PM
Page 23 of 31
Document Title: Being Open Policy
6.2
Advocacy and support
Patients, their families and carers may need considerable practical and emotional help and support
after experiencing a patient safety incident. The most appropriate type of support may vary among
different patients, their families and carers. It is therefore important to discuss with the patient, their
families and carers their individual needs. Support may be provided by patients’ families, social
workers, religious representatives and healthcare organisations such as PALS, Independent
Complaints Advocacy Service (ICAS) and CHCs in Wales. Where the patient needs more detailed
long-term emotional support, advice should be provided on how to gain access to appropriate
counselling and support services, for example, from Cruse Bereavement Care and AvMA.
6.3
Particular patient circumstances
The approach to Being Open may need to be modified according to the patient’s personal
circumstances. The following gives guidance on how to manage different categories of patient
circumstances.
6.3.1
When a patient dies
When a patient safety incident has resulted in a patient’s death, it is even more crucial that
communication is sensitive, empathic and open. It is important to consider the emotional state of
bereaved relatives or carers and to involve them in deciding when it is appropriate to discuss what
has happened. The patient’s family and carers will probably need information on the processes that
will be followed to identify the cause(s) of death. They will also need emotional support. Establishing
open channels of communication may also allow the family and/or carers to indicate if they need
bereavement counselling or assistance at any stage.
Usually, the Being Open discussion and any investigation occur before the coroner’s inquest. But in
certain circumstances the healthcare organisation may consider it appropriate to wait for the
coroner’s inquest before holding the Being Open discussion with the patient’s family and carers.
The coroner’s report on post-mortem findings is a key source of information that will help to
complete the picture of events leading up to the patient’s death. In any event an apology should be
issued as soon as possible after the patient’s death, together with an explanation that the coroner’s
process has been initiated and a realistic timeframe of when the family and carers will be provided
with more information.
The investigation team should request the Legal Services Manager to contact the Coroner’s Officer
allocated as liaison to the family, to discuss the most appropriate method of managing the Being
Open discussion.
6.3.2
Children
The legal age of maturity for giving consent to treatment is 16 years old. It is the age at which a
young person acquires the full rights to make decisions about their own treatment and their right to
confidentiality becomes vested in them rather than their parents or guardians. However, it is still
considered good practice to encourage competent children to involve their families in decision
making.
The courts have stated that younger children who understand fully what is involved in the proposed
procedure can also give consent. This is sometimes known as Gillick competence or the Fraser
guidelines25. Where a child is judged to have the cognitive ability and the emotional maturity to
understand the information provided, he/she should be involved directly in the Being Open process
after a patient safety incident.
Note: This document is electronically controlled. The master copy of the latest approved version is maintained by the owner department.
If this document is downloaded from a website or printed, it becomes uncontrolled.
Version 1.0
Printed on 06/02/2016 at 5:05 PM
Page 24 of 31
Document Title: Being Open Policy
The opportunity for parents to be involved should still be provided unless the child expresses a wish
for them not to be present. Where children are deemed not to have sufficient maturity or ability to
understand, consideration needs to be given to whether information is provided to the parents alone
or in the presence of the child. In these instances the parents’ views on the issue should be sought.
6.3.3
Patients with mental health issues
Being Open for patients with mental health issues should follow normal procedures, unless the
patient also has cognitive impairment (see 4.3.4 Patients with cognitive impairments’).
The only circumstances in which it is appropriate to withhold patient safety incident information from
a patient with mental health issues, is when advised to do so by a consultant psychiatrist who feels
it would cause adverse psychological harm to the patient. However, such circumstances are rare
and a second opinion (by another consultant psychiatrist) would be needed to justify withholding
information from the patient.
Apart from in exceptional circumstances, it is never appropriate to discuss patient safety incident
information with a carer or relative without the express permission of the patient.
6.3.4
Patients with cognitive impairment
Some individuals have conditions that limit their ability to understand what is happening to them.
They may have authorised a person to act on their behalf by an enduring Power of Attorney. In
these cases, steps must be taken to ensure that this extends to decision making and to the medical
care and treatment of the patient.
The Being Open discussion would be conducted with the holder of the power of attorney. Where
there is no such person, the clinicians may act in the patient’s best interest in deciding who the
appropriate person is to discuss incident information with, regarding the welfare of the patient as a
whole and not simply their medical interests. However, the patient with a cognitive impairment
should, where possible, be involved directly in communications about what has happened.
An advocate with appropriate skills should be available to the patient to assist in the communication
process. See 4.3.5 Patients with learning disabilities for details of appropriate advocates.
6.3.5
Patients with learning disabilities
Where a patient has difficulties in expressing their opinion verbally, an assessment should be made
about whether they are also cognitively impaired (see 4.3.4 Patients with cognitive impairment’).
If the patient is not cognitively impaired they should be supported in the Being Open process by
alternative communication methods (e.g. given the opportunity to write questions down). An
advocate, agreed on in consultation with the patient, should be appointed. Appropriate advocates
may include carers, family or friends of the patient. The advocate should assist the patient during
the Being Open process, focusing on ensuring that the patient’s views are considered and
discussed.
6.3.6
Patients with a different language or cultural considerations
The need for translation and advocacy services, and consideration of special cultural needs (such
as for patients from cultures that make it difficult for a woman to talk to a male about intimate
issues), must be taken into account when planning to discuss patient safety incident information. It
would be worthwhile to obtain advice from an advocate or translator before the meeting on the most
sensitive way to discuss the information. Avoid using ‘unofficial translators’ and/or the patient’s
family or friends as they may distort information by editing what is communicated.
Note: This document is electronically controlled. The master copy of the latest approved version is maintained by the owner department.
If this document is downloaded from a website or printed, it becomes uncontrolled.
Version 1.0
Printed on 06/02/2016 at 5:05 PM
Page 25 of 31
Document Title: Being Open Policy
6.3.7
Patients with different communication needs
A number of patients will have particular communication difficulties, such as a hearing impairment.
Plans for the meeting should fully consider these needs. Knowing how to enable or enhance
communications with a patient is essential to facilitating an effective Being Open process. This
involves focusing on the needs of the patient, their family and carers, and being personally
thoughtful and respectful.
6.3.8
Patients who do not agree with the information provided
Sometimes, despite the best efforts of healthcare staff or others, the relationship between the
patient, their family and carers and the healthcare professional breaks down. They may not accept
the information provided or may not wish to participate in the Being Open process. In this case, the
following strategies may assist:
deal with the issue as soon as it emerges;
where the patient agrees, ensure their family and carers are involved in discussions from the
beginning;
ensure the patient has access to support services;
where the senior health professional is not aware of the relationship difficulties, provide
mechanisms for communicating information, such as the patient expressing their concerns to
other members of the clinical team;
offer the patient, their family and carers another contact person with whom they may feel
more comfortable. This could be another member of the team or the individual with overall
responsibility for clinical risk management;
use a mutually acceptable mediator to help identify the issues between the healthcare
organisation and the patient, and to look for a mutually agreeable solution;
ensure the patient, their family and carers are fully aware of the formal complaints
procedures;
write a comprehensive list of the points that the patient, their family and carers disagree with
and reassure them you will follow up these issues.
7 Supporting staff
When a patient safety incident occurs, healthcare professionals involved in the patient’s clinical care
may also require emotional support and advice.
For further information please refer to the Trust Policy Supporting Staff Involved in Incidents
Complaints or Claims.
7.1
Training support
The Being Open advisors are required to complete the NPSA e-learning training resource. Clinical
staff have access to the Patient Safety module, available on training tracker.
Incident investigation and Being Open training resources:
An e-learning tool: ‘Being Open’. http://www.nrls.npsa.nhs.uk/resources/collections/beingopen/
An e-learning tool: ‘A guide to root cause analysis from the NPSA’,
http://www.nrls.npsa.nhs.uk/resources/?entryid45=59901;
The Incident Decision Tree is available via the Clinical Risk intranet pages;
Patient Safety training tracker module
Note: This document is electronically controlled. The master copy of the latest approved version is maintained by the owner department.
If this document is downloaded from a website or printed, it becomes uncontrolled.
Version 1.0
Printed on 06/02/2016 at 5:05 PM
Page 26 of 31
Document Title: Being Open Policy
Clinical Risk Intranet pages
Further advice and support can be accessed by contacting the Clinical Risk Manager ext 5562
(bleep 1322).
Note: This document is electronically controlled. The master copy of the latest approved version is maintained by the owner department.
If this document is downloaded from a website or printed, it becomes uncontrolled.
Version 1.0
Printed on 06/02/2016 at 5:05 PM
Page 27 of 31
7.2
Monitoring
Measurable
Objectives
Policy
Regulator
NHSLA,
1.Being Open process –
CQC
compliance
with
the
process for encouraging
open
communication
between
healthcare
organisations, healthcare
teams, staff, patients
and/or their carers
2.Compliance with the
process
for
acknowledging,
apologising
and
explaining when things
go wrong.
Monitoring/ Audit Method
Monitoring
responsibility
(individual/grou
p/ committee)
Frequency of monitoring
Compliance with Being open process is Clinical Risk Continuous
monitored by clinical risk for all reported Manager
process
serious
incidents,
Being
Open
arrangements for each SI documented
on serious incident monitoring tool.
Reporting
arrangements
(committee/group the
monitoring results is
presented)
monitoring Directorate
Governance
reports
All serious incidents are reported and PSQC
Monthly
PSQC
presented to PSQC, compliance with
Being Open process forms part of the
report.
Clinical Risk Concurrent monitoring via PSQC
Compliance with Being Open policy manager
safeguard system
audited via Safeguard system Being
Open is a mandatory section on the
electronic reporting form.
3.Compliance with the
requirements
for
truthfulness, timeliness
and clarity of information
c. Compliance with the NHSLA,
requirement
for CQC
documenting
all
communication.
Incidents resulting in low,
moderate, severe harm
or death must should
The Trust Investigation report template Clinical Risk All
serious
includes a summary of involvement and Manager
reports
support provided to patients and/or
relatives, this section must be
completed prior to sign off.
Compliance with Being Open policy Clinical
Risk
incident PSQC
PSQC, CSG
Document Title: Being Open Policy
have
a
documented
record of Being Open
communication .
audited via Safeguard system – Being Manager
Open is a mandatory section on the
electronic reporting form.
Concurrent monitoring via
safeguard system
Qualitatative audit of Being Open Clinical Risk
communication
record
to
be Department
6 monthly
undertaken, including WCHS paper
incident forms.
Note: This document is electronically controlled. The master copy of the latest approved version is maintained by the owner department.
If this document is downloaded from a website or printed, it becomes uncontrolled.
Version 1.0
Printed on 06/02/2016 at 5:05 PM
Page 29 of 31
CSG
Appendix A – Quick reference guide to Being Open
Quick reference guide to being open
The principles of Being Open are fully supported by a wide range of Royal Colleges and professional
organisations.
Apologising and explaining when patients have been harmed can be very difficult. You may have
already considered some or all of the recommendations below, but this guide will help ensure that you
follow best practice. Do also refer to your organisation’s local policy before proceeding.
Patients and/or carers should receive an apology as soon as possible after a patient safety incident
has occurred and staff should feel able to apologise on the spot. Saying sorry is not an admission of
liability and it is the right thing to do. Patients have a right to expect openness in their healthcare.
Stage 1: preliminary meeting with the patient and/or their carers
Who should attend?
• A lead staff member who is normally the most senior person responsible for the patient’s care and/or
someone with experience and expertise in the type of incident that has occurred.
• Ensure that those members of staff who do attend the meetings can continue to do so; continuity is
very important in building relationships.
• The person taking the lead should be supported by at least one other member of staff, such as risk
manager, nursing or medical director, or member of the healthcare team treating the patient.
• Ask the patient and/or their carers who they would like to be present.
• Consider each team member’s communication skills; they need to be able to communicate clearly,
sympathetically and effectively.
• Hold a pre-meeting amongst healthcare professionals so that everyone knows the facts and
understands the aims of the meeting.
When should it be held?
• As soon after the incident as possible.
• Consider the patient’s and/or their carer’s home and social circumstances.
• Check that they are happy with the timing.
• Offer them a choice of times and confirm the chosen date in writing.
• Do not cancel the meeting unless absolutely necessary.
Where should it be held?
• Use a quiet room where you will not be distracted by work or interrupted.
• Do not host the meeting near to the place where the incident occurred if this may be difficult for the
patient and/or their carers.
Stage 2: discussion
How should you approach the patient and/or their carers?
• Speak to the patient and/or their carers as you would want someone in the same situation to
communicate with a member of your own family.
• Do not use jargon or acronyms: use clear, straightforward language.
Document Title: Being Open Policy
• Consider the needs of patients with special circumstances, for example, linguistic or cultural needs,
and those with learning disabilities.
What should be discussed?
• Introduce and explain the role of everyone present to the patient and/or their carer and ask them if
they are happy with those present.
• Acknowledge what happened and apologise on behalf of the team and the organisation. Expressing
regret is not an admission of liability.
• Stick to the facts that are known at the time and assure them that if more information becomes
available, it will be shared with them.
• Do not speculate or attribute blame.
• Suggest sources of support and counselling.
• Check they have understood what you have told them and offer to answer any questions.
• Provide a named contact who they can speak to again.
Stage 3: follow-up
• Clarify in writing the information given, reiterate key points, record action points and assign
responsibilities and deadlines.
• The patient’s notes should contain a complete, accurate record of the discussion(s) including the
date and time of each entry, what the patient and/or their carers have been told, and a summary of
agreed action points.
• Maintain a dialogue by addressing any new concerns, share new information once available and
provide information on counselling, as appropriate.
For more information on the NPSA’s Being open work visit:
www.npsa.nhs.uk
© National Patient Safety Agency 2005. Copyright and other intellectual property rights in this material
belong to the NPSA and all
rights are reserved. The NPSA authorises healthcare organisations to reproduce this material for
educational and non-commercial use.
Note: This document is electronically controlled. The master copy of the latest approved version is maintained by the owner department. If
this document is downloaded from a website or printed, it becomes uncontrolled.
Version 0.2
Printed on 06/02/2016 at 5:05 PM
Page 31 of 31