Rare causes of lower GI bleeding - Dis Lair
advertisement

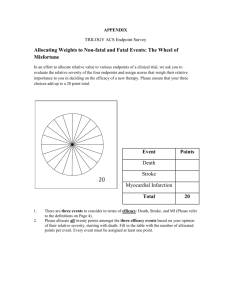
Lower Gastrointestinal Bleeding, Surgical Treatment Introduction Acute lower gastrointestinal (GI) hemorrhage accounts for approximately 20% of all cases of GI hemorrhage. The annual incidence is about 20-27 cases per 100,000 population in westernized countries. Lower GI hemorrhage continues to be a frequent cause of hospital admission and is a factor in hospital morbidity and mortality. Mortality rates are reportedly 10-20% and are dependent on age (>60 y), multiorgan system disease, transfusion requirements in excess of 5 units, need for operation, and recent stress (eg, surgery, trauma, sepsis). Localization of hemorrhage relative to the Treitz ligamentum directs the initial evaluation and resuscitation. The passage of maroon stools or bright red blood from the rectum is usually indicative of massive lower GI hemorrhage. Lower GI hemorrhage can be due to numerous conditions, including diverticulosis, anorectal diseases, carcinomas, inflammatory bowel disease (IBD), and angiodysplasias. For types of GI bleeding and an algorithm for massive bleeding, see the images below. History of the Procedure Understanding of the pathogenesis, diagnosis, and treatment of lower GI bleeding has drastically changed during the last 50 years. In the first half of the 20th century, large intestinal neoplasms were believed to be the most common cause of lower GI bleeding. In the 1950s, lower GI hemorrhage was commonly attributed to diverticulosis. In this period, surgical treatment consisted of blind segmental bowel resections, with disappointing results. Patients who underwent blind segmental bowel resection suffered from a prohibitively high rebleeding rate (up to 75%), morbidity (up to 83%), and mortality (up to 60%). In the last 4 decades, diagnostic methods for locating the precise bleeding point greatly improved. In 1965, Baum et al described selective mesenteric angiography, which permitted the identification of vascular abnormalities and the precise bleeding point.1 Experience with mesenteric angiography in the late 1960s and 1970s suggested that angiodysplasias and diverticulosis were the most common reasons for lower GI bleeding. Since its discovery, mesenteric angiography remains the criterion standard in precise localization of the bleeding. Rösch et al described superselective visceral arteriography for infusion of vasoconstrictors in 1971 and superselective embolization of the mesenteric vessels as an alternative technique to treat massive lower GI bleeding in 1972.2 The most feared complication of embolization of the mesenteric vessels is ischemic colitis, which has limited its use for GI bleeding. The initial experience with vasopressin infusion was reported in 1973-1974. Vasopressin causes vasoconstriction and arrests the bleeding in 36-100% of patients. The recurrence rate following completion of vasopressin infusion can be as high as 71%; therefore, vasopressin is used to temporize the acute event and to stabilize patients before surgery. The flexible endoscope was developed in 1954. The fulllength colonoscope was developed in 1965 in Japan. The first anal colonoscopy was performed in 1969. Endoscopic control of bleeding with thermal modalities or sclerosing agents has been in use since the 1980s. One of the advantages of upper (or lower) endoscopic evaluation is that it provides a means to administer therapy in patients with GI bleeding. Nuclear scintigraphy has been used since the early 1980s as a very sensitive diagnostic tool to evaluate bleeding from GI tract. Nuclear scintigraphy can detect hemorrhage at rates as low as 0.1 mL/min. The average age of patients with lower GI bleeding is 60 years in most series. Etiology varies according to the age of the patient. Segmental bowel resection following precise localization of the bleeding point is a well-accepted surgical practice today. Despite improvement in diagnostic imaging and procedures, 10-20% of patients with lower GI bleeding have no demonstrable bleeding source. Subtotal colectomy is the procedure of choice in patients who are actively bleeding from an unknown source. Problem Lower GI hemorrhage is defined as an abnormal intraluminal blood loss from a source distal to the Treitz ligamentum. Lower GI bleeding is classified under 3 groups according to the amount of bleeding. These groups are shown in the image below. Massive hemorrhage is a life-threatening condition and requires transfusion of at least 5 units of blood. Patients with massive hemorrhage present with a systolic blood pressure of less than 90 mm Hg and a hemoglobin level of 6 g/dL or less. These patients are usually aged 65 years and older, have multiple medical problems, and are at risk of death from acute hemorrhage or its complications. Therefore, the overall mortality rate for massive lower GI hemorrhage ranges from 0-21%. Occult bleeding manifests as microcytic hypochromic anemia and intermittent guaiac reaction. Definition of massive lower GI bleeding 1. Passage of a large volume of red or maroon blood through the rectum 2. Hemodynamic instability and shock 3. Initial decrease in hematocrit (Hct) level of 6 g/dL or less 4. Transfusion of at least 2 units of packed RBCs 5. Bleeding that continues for 3 days 6. Significant rebleeding in 1 week Frequency The total incidence of lower GI bleeding in the United States is not known; although lower GI bleeding is common, most patients do not require hospitalization. Vernava et al reviewed Department of Veterans Affairs' (VA) databases for a 4-year period to study the incidence and etiology of lower GI bleeding. They found that less than 1% of 5.1 million hospital admissions were for lower GI hemorrhage. Another study, in which the Kaiser Permanente database was reviewed, estimated an annual incidence rate of 20.5 patients per 100,000 (24.2 in males vs 17.2 in females). The rate of lower GI bleeding increased more than 200-fold from the third to the ninth decades of life. Etiology Bleeding from diverticular disease has been reported as the most common reason for massive lower GI bleeding in most of the single-institution publications. However, the reported frequency of various other etiologies of lower GI bleeding is not consistent in these manuscripts because of the small number of cases and the highly selective referral pattern and patient populations. Comprehensive knowledge of the etiology of lower GI bleeding is essential for patient management and, ultimately, for patient outcome. In a retrospective review of medical records from approximately 1100 patients with acute lower GI bleeding, all of whom were admitted to the surgical service of a single urban emergency hospital, Gayer et al determined that the most common etiologies for bleeding in these patients were diverticulosis (33.5%), hemorrhoids (22.5%), and carcinoma (12.7%).3 The investigators also found that most patients in the study (55.5%) presented with hematochezia, with the next most frequent presentations being maroon stools (16.7%) and melena (11%). Vernava and colleagues' review found that patients with lower GI bleeding made up only 0.7% of all hospital admissions (17,941 patients). The average age of these patients was 64 years. Only 24% of these patients (4410) had a diagnostic workup, including colonoscopy, barium enema, and/or mesenteric angiography. Among the patients who underwent a diagnostic workup, the most common causes of bleeding were diverticular disease (60%), IBD (13%), and anorectal diseases (11%) (see Table 1), the figures differing somewhat from the above-mentioned study by Gayer et al. Although some publications have reported arteriovenous malformations as a common cause of lower GI bleeding, the true incidence of arteriovenous malformations is insignificant (3%), as stated by Vernava et al. Table 1: Common Causes of Lower GI Bleeding in Adults* LOWER GI HEMORRHAGE IN ADULTS % OF PATIENTS Diverticular disease 60% -Diverticulosis/diverticulitis of small intestine -Diverticulosis/diverticulitis of colon IBD 13% -Crohn's disease of small bowel, colon, or both -Ulcerative colitis -Noninfectious gastroenteritis and colitis Benign anorectal diseases 11% -Hemorrhoids -Anal fissure -Fistula-in-ano Neoplasia 9% -Malignant neoplasia of small intestine -Malignant neoplasia of colon, rectum, and anus Coagulopathy 4% Arteriovenous malformations (AVM) 3% TOTAL 100% *From Vernava and colleagues' survey of 4410 patients Longstreth reviewed the discharge summary and colonoscopy data from a large health maintenance organization with members in the San Diego, Calif, area. In all, 235 hospital admissions for 219 patients were reviewed. The estimated hospital admission rate for lower GI bleeding was found to be 20 patients per 100,000 admissions. Bleeding from diverticular disease was the most common reason for lower GI bleeding (42%), followed by colorectal malignancies (9%) and ischemic colitis (8.7%). The incidence of lower GI bleeding due to colonic angiodysplasias was 6%. These findings were consistent with those of the VA database study, although that study was limited to males. The common causes of lower GI bleeding in infants, children, and adolescents differ from those found in adults. Meckel diverticulum, intussusception, polyposis syndromes, and IBD are the common causes of GI bleeding in children and adolescents (see Table 2).4 Table 2: Common Causes of Lower GI Hemorrhage in Children and Adolescents LOWER GI HEMORRHAGE IN CHILDREN & ADOLESCENTS Intussusception Polyps and polyposis syndromes -Juvenile polyps and polyposis -Peutz-Jeghers syndrome -Familial adenomatous polyposis (FAP) IBD -Crohn's disease -Ulcerative colitis -Indeterminate colitis Meckel diverticulum Many other causes of lower GI bleeding have been documented, including hemorrhage from small bowel diverticulosis, Dieulafoy lesions of the colon or small bowel, portal colopathy with colonic and rectal varices, endometriosis, solitary rectal ulcer syndrome, and vasculitides with small bowel or colonic ulcerations (see Rare causes of lower GI bleeding). Pathophysiology Diverticulosis is a common acquired condition in Western societies. Approximately 50% of adults older than 60 years have radiologic evidence of diverticulosis. Diverticula are most commonly located in the sigmoid and descending colon. Diverticular bleeding originates from vasa rectae located in submucosa, which can rupture at the dome or the neck of the diverticulum. Up to 20% of patients with diverticular disease experience bleeding. In 5% of patients, bleeding from diverticular disease can be massive. Hemorrhage from diverticular disease stops spontaneously in 80% of patients. Although diverticulosis is a left colonic condition, approximately 50% of diverticular bleeding originates from a diverticulum located proximal to the splenic flexure. Diverticula located on the right side may expose the larger portions of vasa rectae to injury because they have wider necks and larger domes compared to the typical left-sided colonic diverticulum. Colonic angiodysplasias are arteriovenous malformations located in the cecum and ascending colon. Colonic angiodysplasias are an acquired lesion affecting elderly persons older than 60 years. These lesions are composed of clusters of dilated vessels, mostly veins, in the colonic mucosa and submucosa. Colonic angiodysplasias are believed to occur as a result of chronic, intermittent, low-grade obstruction of submucosal veins as they penetrate the muscular layer of the colon. The characteristic angiographic findings are clusters of small arteries during the arterial phase of the study, accumulation of contrast media in vascular tufts, early opacification, and persistent opacification due to the late emptying of the draining veins. If mesenteric angiography is performed at the time of active bleeding, extravasation of contrast media is visualized. Unlike diverticular bleeding, angiodysplasia tends to cause slow but repeated episodes of bleeding. Therefore, patients with angiodysplasia present with anemia and syncopal episodes. Infrequently, angiodysplasias can cause an abrupt loss of large quantities of blood. Angiodysplasias can be easily recognized by colonoscopy as 1.5- to 2-mm red patches in the mucosa. Actively bleeding lesions can be treated with colonoscopic electrocoagulation. Incidentally discovered lesions should be left alone. Massive hemorrhage due to IBD is rare. Ulcerative colitis causes bloody diarrhea in most cases. In up to 50% of patients with ulcerative colitis, mild-to-moderate lower GI bleeding occurs, and approximately 4% of patients with ulcerative colitis have massive hemorrhage. Lower GI bleeding in patients with Crohn’s disease is not as common as in patients with ulcerative colitis; 1-2% of patients with Crohn’s disease may experience massive bleeding. The frequency of bleeding in patients with Crohn’s disease is significantly more common with colonic involvement than with small bowel involvement alone. Ischemic colitis, the most common form of ischemic injury to the digestive system, frequently involves the watershed areas, including the splenic flexure and the rectosigmoid junction. In most cases, the precipitating event cannot be identified. Colonic ischemia is a disease of the elderly population and is commonly observed after patients' sixth decade of life. Ischemia causes mucosal and partial-thickness colonic wall sloughing, edema, and bleeding. Ischemic colitis is not associated with significant blood loss or hematochezia, although abdominal pain and bloody diarrhea are the main clinical manifestations. Colorectal adenocarcinoma is the third most common cancer in the United States. Colorectal carcinoma causes occult bleeding, and patients usually present with anemia and syncopal episode. The incidence of massive bleeding due to colorectal carcinoma varies from 5-20% in different series. Postpolypectomy hemorrhage is reported to occur up to 1 month following colonoscopic resection. The reported incidence is between 0.2-3%. Postpolypectomy hemorrhage can be managed by electrocoagulation of the polypectomy site/bleeding with either snare or hot biopsy forceps or by epinephrine injection. Benign anorectal disease (eg, hemorrhoids, anal fissures, anorectal fistulas) can cause intermittent rectal bleeding. Massive rectal bleeding due to benign anorectal disease has also been reported. The VA database review revealed that 11% of patients with lower GI bleeding had hemorrhage from anorectal disease. Patients who have rectal varices with portal hypertension may develop painless massive lower GI bleeding; therefore, examining the anorectum early in the workup is important. If active bleeding is identified, treat it aggressively. Note that the discovery of benign anorectal disease does not exclude the possibility of more proximal bleeding from the lower GI tract. Presentation Massive lower GI bleeding is a life-threatening condition. Although massive lower GI bleeding manifests as maroon stools or bright red blood from the rectum, patients with massive upper GI bleeding may also present with similar findings. Regardless of the level of the bleeding, one of the most important elements of the management of patients with massive upper or lower GI bleeding is the initial resuscitation. These patients should receive 2 large-bore intravenous catheters and isotonic crystalloid infusions. Meanwhile, rapid assessment of vital signs, including heart rate, systolic blood pressure, pulse pressure, and urine output, should be performed. Orthostatic hypotension (ie, a blood pressure fall of >10 mm Hg) is usually indicative of blood loss of more than 1000 mL. History and physical examination are essential parts of an initial evaluation. Document prior episodes of GI bleeding as well as significant medical history and prior medications, including peptic ulcer disease, liver disease, cirrhosis, coagulopathy, IBDs, and use of nonsteroidal antiinflammatory drugs (NSAIDs) and/or warfarin. Symptoms are also important in identifying the source of bleeding. The symptoms of young patients with abdominal pain, rectal bleeding, diarrhea, and mucous discharge may be associated with IBD. On the other hand, symptoms of elderly patients with abdominal pain, rectal bleeding, and diarrhea can be associated with ischemic colitis. Stools streaked with blood, perianal pain, and blood drops on the toilet paper or in the toilet bowl may be associated with perianal pathology, such as anal fissure or hemorrhoidal bleeding. The physical examination must include careful inspection and examination of the oropharynx, nasopharynx, abdomen, perineum, and anal canal. Nasogastric aspirates usually correlate well with upper gastric hemorrhage proximal to the Treitz ligamentum; therefore, insert a nasogastric tube to confirm the presence or absence of blood in the stomach. If necessary, perform gastric lavage with warm isotonic fluids to obtain bilious discharge from the nasogastric tube to exclude any upper GI bleeding beyond the pylorus. Nasogastric tube aspirates can provide false-negative results in approximately 50% of cases if the aspirate contains no bile or if the bleeding is intermittent. These patients eventually need esophagogastroduodenoscopy (EGD) to obtain a more specific evaluation of the upper GI tract. Place a Foley catheter to monitor urine output. Careful digital rectal examination, anoscopy, and rigid proctosigmoidoscopy should exclude an anorectal source of bleeding. Indications Surgical treatment is indicated if the patient continues to bleed and if nonoperative management is unsuccessful or unavailable. Segmental colectomy is indicated if the bleeding point is localized by preoperative diagnostic studies. Subtotal colectomy is the procedure of choice if the bleeding point cannot be localized with preoperative or intraoperative diagnostic studies. Subtotal colectomy is associated with negligibly higher perioperative morbidity and mortality compared to segmental colonic resection. In addition, postoperative diarrhea can be a significant problem in elderly patients who undergo subtotal colectomy and ileorectal anastomosis. Relevant Anatomy The average length of the large intestine is 135-150 cm. Ascending and descending segments of the colon are fixed to the retroperitoneum. On the other hand, the transverse and sigmoid colon are supported by a mesentery in the abdomen. A comprehensive understanding of small bowel and colonic vascular anatomy is essential for any surgeon performing primary lower GI surgery for hemorrhage or other diseases. The ileocolic, right colic, and middle colic branches of the superior mesenteric artery supply blood to the cecum, ascending, and proximal transverse colon, respectively. The superior mesenteric vein drains the right side of the colon, joining the splenic vein to form the portal vein. The inferior mesenteric artery supplies blood to the distal transverse, descending, and sigmoid colon. The inferior mesenteric vein carries blood from the left side of the colon to the splenic vein. A rich network of vessels from the superior, middle, and inferior hemorrhoidal vessels supplies the rectosigmoid junction and rectum. Contraindications No contraindications exist with regard to surgery in hemodynamically unstable patients with active bleeding. Surgery is warranted even in the absence of accurate preoperative localization for patients who require transfusion of 5 units or more blood in the first 24 hours. Surgery is also necessary in patients with recurrent bleeding during the same hospitalization. Workup Laboratory Studies Appropriate blood tests include CBC; serum electrolytes (sequential multiple analysis 7 [SMA7]); and coagulation profile, including activated partial thromboplastin time (aPTT), prothrombin time (PT), manual platelet count, and bleeding time. Imaging Studies 1. The role of nuclear scintigraphic imaging in the diagnosis and treatment of patients who present with lower GI bleeding remains controversial. Nuclear scintigraphy is a sensitive diagnostic tool (86%) and can detect hemorrhage at rates as low as 0.1 mL/min. Nuclear scintigraphy is reportedly 10 times more sensitive than mesenteric angiography in detecting ongoing bleeding. The scintigraphic imaging suffers from a low specificity (50%) due to its limited resolution; this has led many investigators to recommend that scintigraphic imaging be used primarily as a screening examination to select patients for mesenteric angiography. See the algorithm for GI bleeding in the image below. 2. No preparation is required for99m sulfur colloid. This agent has a very short half-life (2.5-3.5 min) because it is rapidly cleared by the reticuloendothelial system. Because it enhances the liver and spleen, bleeding from both the hepatic flexures and the splenic flexures may be obscured.99m Tc-labeled RBC scintigraphy is the preferred technique because its half-life is longer. Images delayed up to 24 hours can be taken with labeled RBC scanning. 3. The sensitivity of the99m Tc-labeled RBC scintigraphy is reportedly 20-95%. The bleeding site can be identified accurately when intraluminal accumulation of 99m Tclabeled RBCs is observed during the dynamic phase of scanning. Although nuclear scintigraphy is sensitive enough to diagnose ongoing bleeding at a rate as low as 0.1 mL/min, it is not highly accurate in locating the bleeding point. The bleeding point is accurately localized in 52-90% of positive cases, with an average of 86% and incorrect localization of 14%, as reported in 24 publications. Because of the high false localization rate (10-60%) for the bleeding site, performing segmental resections based solely on scintigraphy results is not recommended. 4. Ng and colleagues reviewed 86 patients with positive99m Tc-labeled RBC scintigraphy findings.5 Patients with an immediate blush (within 2 min of the study) revealed a positive predictive value of 75% for angiography. Patients with a delayed blush (after 2 min of the study) had a negative predictive value of 93% for angiography. Thus, patients with delayed blush should proceed with colonoscopic evaluation instead of mesenteric angiography. Use99m Tc-labeled RBC scintigraphy as a prescreening test for selective mesenteric angiography. 5. 6. In 1992, Ryan et al published their experience with 99m Tclabeled RBC scintigraphy. In this study, 29 patients with lower GI bleeding were identified. Scintigraphy identified the site of bleeding accurately in 9 patients with massive lower GI bleeding. In 6 of 9 patients, the scintigraphy finding was positive in the first 5 minutes of the study. In 3 patients, the scintigraphy finding was positive at 14-45 minutes. Another study was performed to evaluate the efficacy of RBC scintigraphy in confirming the location of the lower GI bleeding. Twenty-one patients with positive scintigraphy results were included in the study. Of these, the bleeding site was confirmed in 16 patients by various methods. RBC scintigraphy findings were positive within the continuous phase of the study in 10 of the confirmed studies and in none of the incorrectly localized studies. Therefore, in carefully selected cases, patients can undergo segmental resections only if scintigraphy findings are strongly positive in the very initial part of the test. Cinematic99m Tc-labeled RBC scintigraphy (real-time scanning) has been described as a noninvasive alternative to mesenteric angiography. Continuous dynamic imaging using sequential computer acquisition provides more accurate localization of the bleeding point because it enables cinematic playback. More studies are necessary to identify the success of real-time scintigraphic evaluations. Recurrent lower GI bleeding occurs after negative99m Tclabeled RBC scintigraphy. Hammond et al conducted retrospective evaluations of 84 patients with negative99m Tc-labeled RBC scintigraphy. The overall rebleeding rate was found to be 27% (n=23 patients). Hammond et al concluded that age, gender, bleeding source, use of anticoagulant/antiplatelet agents, length of hospital stay, admission Hct, Hct nadir, and transfusion requirements are not predictive of the patients who will rebleed. The use of111 indium–labeled RBC scintigraphy to detect intermittent bleeding has been described in the medical literature in a handful of publications. Ferrant and colleagues initially used111 indium–labeled RBC scintigraphy in patients with lower GI bleeding in 1980; however, it remains underutilized because of a prolonged half-life of 67 hours. This scintigraphy is more expensive and also is a more labor-intensive technology than99m Tc labeling. The image quality and localization of bleeding can be less than desirable because of the prolonged half-life and intestinal motility. However, the longer half-life of111 indium–labeled RBC scintigraphy can be useful in locating intermittent bleeding points, particularly when conventional methods have failed. Schmidt et al published a report on 6 patients in whom99m Tc scanning was initially 7. 8. 9. unrewarding.6Subsequent scintigraphy with111 indium– labeled RBCs located the site of bleeding in all patients. Mole et al detected synchronous, small and large intestinal adenocarcinomas with111 indium–labeled RBC scintigraphy in a 70-year-old patient with intermittent GI bleeding and profound blood loss anemia.7 In 1965, Baum et al described selective mesenteric angiography in the diagnosis of GI bleeding. 1 Since then, the value of mesenteric angiography in the diagnosis and management of lower GI bleeding has been well established. The extravasation of contrast material indicates a positive study finding. Selective mesenteric angiography can detect bleeding at a rate of more than 0.5 mL/min. In a patient with active GI bleeding, the radiologist concentrates on the major mesenteric vessel most likely to be responsible (eg, the inferior mesenteric artery in bright red rectal bleeding). If no bleeding is identified, the other major mesenteric vessels, including the superior mesenteric artery and celiac axis, are studied. In some cases, aberrant vascular anatomy can contribute to colonic or small bowel circulation; in other cases, patients with upper GI bleeding may present in an uncommon clinical fashion. Helical CT scan of the abdomen and pelvis can also be used when routine workup fails to determine the cause of active GI bleeding. Multiple criteria, including vascular extravasation of the contrast medium, contrast enhancement of the bowel wall, thickening of the bowel wall, spontaneous hyperdensity of the peribowel fat, and vascular dilatations, are used to establish the bleeding site with helical CT. The presence of diverticula alone was not enough to define the bleeding site. Three-phase helical CT should be performed using intravenous contrast. Water can be used as an oral contrast in the workup of patients who are actively bleeding. Therefore, helical CT could be a good diagnostic tool in acute lower GI bleeding to help the physician identify the bleeding site. A pilot study was done in Sydney, Australia, to evaluate CT as a diagnostic tool for acute lower GI bleeding. Helical CT was compared to selective mesenteric angiography and colonoscopy in the diagnosis and detection of a bleeding site. Seven patients with acute lower GI bleeding were included. All patients underwent mesenteric angiography following CT. Colonoscopies were also performed on 5 patients investigated with both CT and mesenteric angiography. Both modalities had concordant findings of 2 active bleeding sites, 1 nonbleeding rectal tumor, and 1 negative result. In 3 patients, the source of bleeding was found on CT, whereas the mesenteric angiography finding was negative. Colonoscopies performed in these 3 patients confirmed blood in the colon/ileum. 10. 11. 12. 13. Sabharwal et al concluded that helical CT is a safe, convenient, and accurate diagnostic tool for acute lower GI hemorrhage.8 The authors proposed a new management algorithm for acute lower GI hemorrhage using CT as the preselective mesenteric angiography screening tool. Frattaroli et al examined the sensitivity of multi-detector row CT (MDCT) scanning in identifying the site and etiology of acute upper (11 patients) and lower (18 patients) GI bleeding.9 Comparing this modality with endoscopy, the investigators reported that, in terms of identifying the anatomic location and etiology of upper GI bleeding, MDCT had a sensitivity of 100% and 90.9%, respectively, while endoscopy had a sensitivity of 72.7% and 54.5%. For lower GI bleeding, MDCT had a sensitivity for site and etiology identification of 100% and 88.2%, respectively, while endoscopy had a sensitivity of 52.9% for both identifications. Once the bleeding point is identified, angiography offers potential treatment options, such as selective vasopressin drip and embolization. Thirteen publications reported experiences with selective mesenteric angiography. When 657 patients underwent mesenteric angiography, the percentage of positive study findings fluctuated between 27-86%, with an average of 45%. Because of the intermittent nature of lower GI bleeding, the number of positive study findings is significantly less with this invasive diagnostic modality. Emergency angiography as an initial study is indicated in a highly selected group of patients with massive ongoing lower GI bleeding. Browder et al used 2 criteria to triage patients for emergency angiography.10 The criteria were at least 4 units of blood transfusion in the first 2 hours following hospital admission and systolic blood pressure of less than 100 mm Hg with aggressive resuscitation. Fifty patients underwent emergency angiography, and bleeding was localized in 72% of patients. Vasopressin infusion was successful in 91%; however, half experienced bleeding following cessation of the vasopressin infusion. Thus, patients with ongoing hemorrhage, emergency angiography, and vasopressin infusion have improved operative morbidity, mortality, and outcome. Five to 10% of patients may present with recurrent episodes of massive lower GI bleeding without any diagnosis of the bleeding site. These patients experience multiple hospital admissions; they also undergo recurrent blood transfusions and several invasive studies repeatedly. Ryan et al performed 17 elective provocative bleeding studies for occult lower GI bleeding in 16 patients.11 Although an abnormality was identified in 50% of patients, bleeding was provoked in 6 (37.5%) patients. Most of the positively provoked patients (ie, 5 patients) had a previously positive tagged red cell scintigraphy.11 Of the 6 patients with provoked bleeding, 3 were treated with superselective embolization at the time of provoked bleeding, 2 were treated with estrogen therapy, and 1 was treated with palliative therapy. 11 Ten patients did not bleed during the provoked study.11 14. Widlus and Salis reported 9 patients who underwent provocative angiography with Reteplase, a new fibrinolytic agent.12 An initial diagnostic visceral arteriogram was performed and failed to identify the source of bleeding in each patient.12 Reteplase was administered, and provocative arteriography was repeated. Bleeding was identified in 8 (89%) patients, and these patients were treated with microembolization, segmental resection, or conservatively.12 It was concluded that the use of Reteplase is safe and effective as a provocative agent, stimulating bleeding to allow localization, in patients with occult, recurrent, massive lower GI bleeding.12 Other Tests 1. Double-contrast barium enema examinations can be justified only for elective evaluation of unexplained lower GI bleeding. Do not use barium enema examination in the acute hemorrhage phase because it makes subsequent diagnostic evaluations, including angiography and colonoscopy, impossible. 2. Elective contrast radiography of the small bowel and/or enteroclysis is often valuable in investigation of longterm, unexplained lower GI bleeding. Diagnostic Procedures Colonoscopy has an important role in the diagnosis and treatment of lower GI bleeding. Rapid colonic lavage with GoLYTELY clears the intraluminal blood, clot, and stool, providing an adequate environment for visualization of the lower GI mucosa and lesions. GoLYTELY can be administered orally or by nasogastric tube. The best candidates for colonoscopic evaluation are patients who are bleeding slowly or who have already stopped bleeding. Histologic Findings Most colonic diverticula are false pulsion diverticula and are composed only of mucosa and submucosa herniated through the colonic wall musculature. Hemorrhage associated with diverticula comes from perforated vasa rectae located at the neck or the apex of the diverticula. Colonic angiodysplasias are vascular ectasias commonly located on the right side of the colon. Microscopically, vascular ectasia consists of dilated thin-walled venules and capillaries localized in the submucosa of the colonic wall. Treatment Medical Therapy Vasoconstrictive agents Initially, vasoconstrictive agents, such as vasopressin (Pitressin), can be used. An experimental study of treatment of lower GI bleeding by selective arterial infusion of vasoconstrictors, such as epinephrine with propranolol and vasopressin, was reported. Although epinephrine and propranolol drastically reduced mesenteric blood flow, they also caused a rebound increase in blood flow and recurrent bleeding. Vasopressin is a pituitary hormone that causes severe vasoconstriction in the splanchnic bed. Vasoconstriction reduces the blood flow and facilitates hemostatic plug formation in the bleeding vessel. The results are less than satisfactory in patients with severe atherosclerosis and coagulopathy. Following positive angiogram findings, the angiographic catheter is left in place and vasopressin infusion is started at a rate of 0.2 unit/min. A repeat angiogram is obtained every half hour, and the rate of infusion is increased up to 0.4 unit/min if bleeding continues. Vasopressin doses above 0.4 unit/min are not recommended because of the high rate of potential complications. If hemorrhage remains controlled, the dose of vasopressin is reduced to half every 6-12 hours. The angiographic catheter, following an additional 6-12 hours of saline infusion, is removed. If vasopressin infusion fails to control the hemorrhage, patients should undergo a segmental resection. The initial experience with vasopressin infusion was reported in 1973-1974. Twenty-four patients were included in this study. In 22 of the patients, bleeding was controlled. Of these, 12 received no further therapy and were discharged. Three patients (25%) developed recurrent bleeding within 212 months of discharge. Selective vasopressin infusion was used as the sole treatment and arrested the bleeding in 36100% of the cases. Because the rebleeding rates fluctuated between 27-71%, vasopressin infusion was used in the acute event to stabilize patients prior to surgery. During vasopressin infusion, monitor patients for recurrent hemorrhage, myocardial ischemia, arrhythmias, hypertension, and volume overload with hyponatremia. Nitroglycerine paste or drip can be used to overcome cardiac complications. Selective mesenteric infusion induces bowel wall contraction and spasms, which should not be confused with bowel wall ischemia. Do not administer vasopressin into systemic circulation intravenously because this causes coronary vasoconstriction, diminished cardiac output, and tachyphylaxis. Superselective embolization Superselective embolization of the mesenteric vessels is an alternative technique for treating massive lower GI bleeding. Rösch and colleagues first described this technique in 1972. Autologous clot, Gelfoam, polyvinyl alcohol, microcoils, ethanolamine, and oxidized cellulose can be used as embolic agents. Embolization involves superselective catheterization of the bleeding vessel to minimize necrosis, the most feared complication of ischemic colitis. Rosenkrantz et al reported 3 cases of colonic infarction. 14 One patient died following segmental colectomy, and the other patients revealed full-thickness bowel wall injury in the resected specimen. Intestinal ischemia and infarction have also been reported. To prevent this complication, perform embolization beyond the marginal artery as close as possible to the bleeding point in the terminal mural arteries. A total of 139 cases have been collected from the medical literature since 1972. Overall bleeding was controlled in 115 patients (83%), with a rebleeding rate of 11% (15 patients). Complications were observed in 20%, and bowel injury and perforation were observed in 12% (16 patients). The overall mortality rate was 11% (15 patients); thus, careful patient selection is necessary for this procedure. Use embolization in high-risk patients whose conditions are refractory to conservative management. If terminal mural branches of the bleeding vessel cannot be catheterized, abort the procedure and immediately perform surgery. Kuo et al evaluated the safety and effectiveness of superselective microcoil embolization for the treatment of lower GI bleeding in 2003.15 Twenty-two patients with angiographic evidence of lower GI bleeding underwent superselective microcoil embolization during a 10-year period. Complete clinical success was achieved in 86% of patients with a rebleeding rate of 14%. Minor and major ischemic complication rates were reported as 4.5% and 0%, respectively. The authors also reviewed the data from 122 cases of lower GI superselective microcoil embolization in the literature. The meta-analysis was performed in 144 patients. This combined analysis revealed a minor ischemic complication rate of 9% and a major ischemic complication rate of 0%. It was concluded that superselective microcoil embolization is a safe and effective treatment of acute lower GI hemorrhage. Colonoscopy Colonoscopy has become the first choice of diagnostic modality following rapid purge with volume cathartics, such as GoLYTELY. Jensen and Machicado have evaluated the role of urgent colonoscopy after purge prospectively in 80 consecutive patients with severe hematochezia. 16 Urgent colonoscopies were performed in the intensive care unit. Seventy-four percent of patients had colonic lesions, 11% had upper GI lesions, and 9% had presumed small bowel lesions; in 6%, no bleeding site was identified. Although Jensen and Machicado recommended that EGD be performed prior to colonoscopy, upper and lower endoscopies can be performed simultaneously. In another study, colonoscopy yielded a diagnosis in 90% of the patients, which provided opportunity for therapy at the same time. The patients who underwent colonoscopic evaluation had a significantly shorter hospital stay. Perform the urgent colonoscopy in the operating room or endoscopy suite on hemodynamically stable patients. If patients become unstable or colonoscopy reveals an active fulminant inflammation, abort the procedure. Endoscopic coagulation The treatment options for angiodysplasias are numerous, including segmental bowel resection and selective mesenteric embolization. Endoscopic coagulation of angiodysplasias is becoming a treatment of choice using either heated probe or lasers, such as Nd:YAG and argon. Argon laser treatment is recommended for mucosal or superficial lesions because the energy penetrates only 1 mm. Nd:YAG lasers are more useful for deeper lesions because they penetrate 3-4 mm. Hunter et al evaluated 222 GI endoscopic laser procedures in 122 patients. Hemorrhage was arrested in 84% of the patients with GI bleeding. No perforations were reported in this series. One death occurred and was attributed to laser therapy in a patient with duodenal ulcer and gastroduodenal artery bleeding. Forty patients with GI arteriovenous malformations underwent 72 photocoagulation sessions with mostly argon laser. Of those 40 patients, 15 had significant hemorrhage from colonic arteriovenous malformations. No deaths occurred in ablation of GI arteriovenous malformations in 15 patients with colonic lesion. One of the advantages of upper or lower endoscopic evaluation is that it provides access to therapy in patients with GI bleeding. Endoscopic control of bleeding can be achieved using thermal modalities or sclerosing agents. Absolute alcohol, morrhuate sodium, and sodium tetradecyl sulfate can be used for sclerotherapy of upper and lower GI lesions. Endoscopic thermal modalities (eg, laser photocoagulation, electrocoagulation, heater probe) can also be used to arrest hemorrhage. Endoscopic control of hemorrhage is suitable for GI polyps and cancers, arteriovenous malformations, mucosal lesions, postpolypectomy hemorrhage, endometriosis, and colonic and rectal varices. The medical literature has also been reviewed for endoscopic treatment of significant lower GI bleeding. A total of 286 patients were identified in 8 publications. Hemorrhage was successfully arrested in 70% of patients, with a rebleeding rate of 15%. Endoscopic therapy for lower GI bleeding is a minimally invasive and viable option in carefully selected patients. Surgical Therapy An emergency operation is required in approximately 10% of patients with lower GI bleeding. When the bleeding point is localized, perform a limited segmental resection of the small or large bowel. The crude outcome analysis was applied to 483 cumulative cases of limited segmental resection derived from 23 publications since 1974. The rebleeding rate was 7% (0-21%), and the mortality rate was 10% (0-15%). A morbidity rate of 0-33% was reported in only a very few publications; thus, limited segmental resection is preferred because it can be performed with low morbidity, mortality, and rebleeding rates. If the patient is hemodynamically unstable because ongoing hemorrhage, perform an emergency operation before any diagnostic study. In these cases, make every attempt to diagnose the bleeding point intraoperatively. Intraoperative EGD, surgeon-guided enteroscopy, and colonoscopy may be helpful in diagnosing undiagnosed massive GI bleeding. Depending on the availability of local resources and the patient's condition, it may sometimes be better to perform subtotal colectomy with distal ileal inspection than to try to achieve these other tests, particularly if the surgeon is not privileged or comfortable with endoscopy. If the bleeding point cannot be diagnosed following a thorough intraoperative endoscopy and examination and if evidence points to colonic bleeding, perform a subtotal colectomy with ileorectal anastomosis. Subtotal colectomy is a rational option because it is associated with a very low rebleeding rate (3%) and with acceptable average morbidity (32%) and mortality (19%) rates. Practitioners must understand that blind segmental resection should not be performed because of a prohibitively high rebleeding rate of up to 75%, a morbidity rate up to 83%, and a mortality rate up to 60%. Once the bleeding point is identified, a limited segmental resection should be performed. Patients who have experienced multiple episodes of lower GI bleeding without a known source or diagnosis should undergo elective mesenteric angiography, upper and lower endoscopy, Meckel scan, upper GI with small bowel series, and enteroclysis. Elective evaluation of the entire GI tract may identify uncommon lesions and undiagnosed arteriovenous malformations. Rare causes of lower GI bleeding 1. Chronic radiation enteritis/proctitis 2. Ischemic colitis/mesenteric vascular insufficiency 3. Small bowel diverticulosis 4. Meckel diverticulum 5. Colonic/rectal varices 6. Portal colopathy 7. Solitary rectal ulcer syndrome 8. Diversion colitis 9. Dieulafoy lesion of colon 10. Dieulafoy lesion of small bowel 11. Vasculitides 12. Small bowel ulceration 13. Intussusception 14. Endometriosis 15. GI bleeding in runners If the bleeding point is diagnosed by mesenteric angiography, vasopressin infusion can be temporarily used to control the hemorrhage to stabilize the patient in anticipation of semiurgent segmental bowel resection. Use selective mesenteric embolization in high-risk patients for whom the operative management is associated with prohibitive risk of morbidity and mortality. If mesenteric embolization is used, these patients must be carefully monitored for bowel ischemia and perforation. Any evidence of ongoing bowel ischemia and/or unexplained sepsis following mesenteric embolization requires exploratory laparotomy to resect the affected bowel segment. Perform subtotal colectomy with ileoproctostomy in patients with multiple episodes of nonlocalized lower GI bleeding or bilateral sources of colonic hemorrhage. Preoperative Details Acute lower GI hemorrhage is a common clinical entity and is associated with significant morbidity and mortality. Mortality rates associated with lower GI hemorrhage are reported to be 10-20% and are dependent on age (>60 y), multiorgan system disease, transfusion requirements (>5 units), need for operation, and recent stress (eg, surgery, trauma, sepsis). Three major aspects are involved in managing lower GI hemorrhage. The initial priority is to treat the shock. Second, localization of the source of bleeding is required to perform the third task—formulating an interventional plan. Insert a nasogastric tube in all patients. A clear bile-stained aspirate generally excludes bleeding proximal to the Treitz ligamentum. After initial resuscitation, undertake a search for the cause of the bleeding to precisely locate the bleeding point. Following accurate localization by angiogram, bleeding can be temporarily controlled with either angiographic embolization or vasopressin infusion. Segmental bowel resection is performed in the next 24-48 hours following correction of the patient's physiologic parameters, which include hypotension, hypothermia, acute hemorrhagic anemia, and deficient coagulation factors. Intraoperative Details Surgical intervention is required in only a small percentage of patients with lower GI hemorrhage. The surgical option depends on whether the bleeding source has been accurately identified preoperatively; if so, it is then possible to perform segmental intestinal resection. If the bleeding source is unknown, an upper GI endoscopy should be performed prior to any surgical exploration. At celiotomy, identifying the bleeding point is often impossible, as blood refluxes into the proximal and distal bowel. The abdominal cavity is explored through a midline vertical incision. The assistance of a gastroenterologist is required for intraoperative endoscopic evaluation. The colonoscope is introduced, and the surgeon assists its passage. On-table colonic lavage and colonoscopy may identify the colonic source of bleeding. Surgeon-guided intraoperative small bowel enteroscopy is also performed when no colonic source of bleeding is identified. Again, the colonoscope can be used for this procedure. Unlike colonoscopy, enteroscopy is performed during the advancement of the scope. Colonoscopic manipulation of the small bowel may cause iatrogenic mucosal tears and hematomas, which may be mistakenly identified as a source of bleeding. Another intraoperative strategy is to clamp segments of the bowel with noncrushing intestinal clamps to identify the segment that fills with blood. If the bleeding point cannot be diagnosed through intraoperative panintestinal endoscopy and examination and if evidence points to a colonic bleeding, perform a subtotal colectomy with end ileostomy. Postoperative Details Hypotension and shock are the eventual consequences of blood loss, but this depends on the rate of bleeding and the patient's response. Clinical development of shock may precipitate myocardial infarction, cerebrovascular accident, and renal or hepatic failure. Azotemia occurs in patients with GI blood loss. Follow-up Postoperative office visits every 2 weeks are essential to ensure proper wound healing. Upon discharge, a general diet abundant in fruits and vegetables is recommended. Patients are instructed to drink 6-8 glasses of fluid per day. Psyllium seed preparations should also be started. Complications Patients who have had surgery of the lower GI tract are prone to the development of complications. The most common early postoperative complications are intraabdominal or anastomotic bleeding, ileus, mechanical small bowel obstruction (SBO), intra-abdominal sepsis, localized or generalized peritonitis, wound infection and/or dehiscence, Clostridium difficilecolitis, pneumonia, urinary retention, urinary tract infection (UTI), deep venous thrombosis (DVT), and pulmonary embolus (PE). Intra-abdominal sepsis following colorectal surgery is a lifethreatening complication and requires aggressive resuscitation. Systemic conditions (eg, severe blood loss and shock, poor bowel preparation, irradiation, diabetes, malnutrition, hypoalbuminemia) may adversely affect anastomotic healing. Changes in anatomy and physiology of the large bowel, high bacterial content, improper operative technique, tension, and ischemia can cause anastomotic leak associated with abscess and intra-abdominal sepsis. This condition requires either laparotomy (if the sepsis is generalized) or percutaneous drainage (if the sepsis is localized). Delayed complications usually occur more than a week after surgery. The most common delayed complications are anastomotic stricture, incisional hernia, and incontinence. Outcome and Prognosis Identification of the bleeding point is the most important initial step in treatment. Once the bleeding point is localized, the treatment options are straightforward and curative. Although diagnostic methods for precisely locating the bleeding point have greatly improved over the last 3 decades, 10-20% of patients with lower GI bleeding have no demonstrable bleeding source. Therefore, this complex problem requires systematic and orderly evaluation to reduce the percentage of undiagnosed and untreated cases of lower GI bleeding. Future and Controversies The evolution of more sophisticated diagnostic imaging (eg, angiography, bleeding scan, flexible fiberoptic colonoscope) offers the promise of precise localization of the bleeding site. These advances also provide nonoperative and less invasive control of bleeding using angiographic techniques or colonoscope. Pharmacologic discoveries are also improving patient care and outcome. Therefore, the therapeutic armamentaria have expanded greatly in the last 50 years.Precise localization of the bleeding point is essential for treatment of lower GI bleeding. Despite the improvement in diagnostic imaging and procedures, up to 10-20% of the patients with lower GI bleeding have no demonstrable bleeding source; therefore, noninvasive diagnostic images and techniques should be developed to improve patient outcome.