Johnson, Lee and Vo - Saddleback College
advertisement

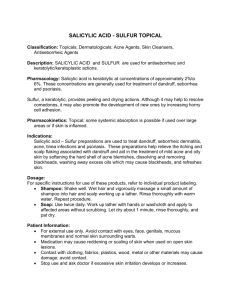
The Antibacterial Effects of Salicylic Acid Concentration on Skin Flora (Staphylococcus epidermidis) Sean Johnson, Rachel Lee and Felicia Vo Department of Biological Sciences Saddleback College Mission Viejo, CA, 92692 Acne vulgaris is a chronic inflammatory disease of the pilosebaceous unit, which is comprised of the hair follicle, hair shaft, and associated sebaceous glands. Among the many species of bacterial flora present on the facial skin, Staphylococcus epidermidis is believed to be a probable cause of its development. The most successful treatment plans will often use a combination of topical agents and oral antibiotics. The study proposed that a topical agent containing concentrated salicylic acid could exhibit antibacterial effects, even without the addition of an oral antibiotic. It was predicted that there will be a difference between the antibacterial effectiveness of salicylic acid and ampicillin against S. epidermidis. A KirbyBauer test was performed on petri dishes containing disks saturated in sterile water, ampicillin, or 1%, 2%, 5%, and 10% salicylic acid solution. Post incubation, the zone of inhibition around each disk was measured (in mm). An ANOVA was performed, resulting in a p value of less than 0.0001. While the original hypothesis was accepted, a subsequent post hoc test suggested there was no difference in the antibacterial effectiveness of the salicylic acid concentrations to each other nor to water. Introduction Acne vulgaris, more commonly known as acne, is a chronic inflammatory disease of the pilosebaceous unit (Bhate, 2012), which is comprised of the hair follicle, hair shaft and associated sebaceous glands (Singh, 2000). It is one of the most common skin diseases, affecting over forty-five million Americans, and the reason for almost twenty percent of all dermatologist visits (Bhatia, 2004). Although it is not life-threatening nor contagious, acne can persist for years. This may result in both physical and psychosocial effects, such as a decreasing a person’s self-esteem or causing permanent dermal damage in the form of scarring. While the exact etiopathogenesis for acne vulgaris is currently unknown, there are multiple common symptoms shared among all patients with this disease. These symptoms include excessive sebum production (secreted by sebaceous glands), excessive keratosis of excretory ducts and openings of sebaceous glands, development of bacterial flora and release of inflammatory mediators in the skin (Bergler-Czop, 2014). Among the many species and strains of bacterial flora present on the facial skin, Staphylococcus epidermidis is believed to be a probable cause of acne vulgaris development. The bacteria S. epidermidis is a major component of human skin flora. S. epidermidis is gram positive, coagulase-negative and believed to be a cause of acne vulgaris (Nishino, 1986). It has a short generation time of seventeen to thirty eight minutes, which is ideal to see quick growth (Gottenbos, 2000). It is also resistant to many antimicrobial and antibacterial agents due to the production of a glycocalyx “slime.” These factors make S. epidermidis an ideal bacterium for use in the study. Because acne has multifactorial causes, the most successful treatment plans target multiple symptoms. Patients will often use a combination of topical agents and oral antibiotics in order to get rid of the colonizing bacteria and inflammation within the pilosebaceous unit. This is an integral part of treating moderate to severe acne as well as acne of lesser severity (Cook, 2010). An increase in the use and duration of these antibiotic treatments, however, presents a higher risk of resistant strains of S. epidermidis developing in the future. This problem not only raises concern for the treatment of acne vulgaris, but also for the antibiotic resistance of other bacterial species as well (Toyoda, 1998). Salicylic acid is among the many topical agents available in treating acne vulgaris. Salicylic acid is keratolytic and works by dissolving the intercellular “cement” that holds epithelial cells together (Akhavan, 2003). It can be found in concentrations ranging from 0.5% to 10% in acne treatment products; however, 2% is the maximum strength allowed in any nonprescription acne product in the U.S. (Akhavan, 2003). Nonprescription acne products, especially those containing salicylic acid, are typically a part of the initial steps taken in acne treatment before consulting professional help. Salicylic acid is also the major metabolite of aspirin, and has been found to mitigate two virulence phenotypes in Staphylococcus aureus strains (Kupferwasser, 2003). The study examines the antibacterial effects of salicylic acid concentration on S. epidermidis. It is hypothesized that there is a difference between the antibacterial effectiveness of amoxicillin and salicylic acid against Staphylococcus epidermidis. Conducting this experiment will provide a greater understanding of the sole efficacy of salicylic acid on this bacterium. In turn, this may help manufacturers develop more effective acne products, as well as dermatologists to better diagnose and prescribe treatment plans for their patients. If salicylic acid is found to be ineffective against S. epidermidis on its own, it may need to be paired with another antibacterial agent in order to kill the bacteria. Materials and Methods Although S. epidermidis is a facultative anaerobe, it is able to thrive under aerobic conditions. In order to determine the antibacterial effectiveness of salicylic acid on the bacteria, a Kirby-Bauer, or disk diffusion, test was performed. The agar medium used in the petri dishes was nutrient agar, a growth medium that commonly contains approximately 0.5% peptone, 0.3% beef extract, 0.3% yeast extract, 1.5% agar, 0.5% sodium chloride and distilled water by volume. The ingredients were mixed together, the mixture was heated and poured onto sterile petri dishes. The plates were left to cool to allow the agar to solidify. An inoculated culture of S. epidermidis was obtained, and a lawn was spread onto each petri dish, using aseptic technique to prevent any outside contamination. To ensure a complete lawn, streaks were made in one direction from the top of the plate to the bottom using a sterile cotton swab. The plate was then rotated 90 degrees, and the process was repeated. Solutions of 1%, 2%, 5% and 10% concentrations of salicylic acid were chosen to simulate a fair range of concentrations commonly found in both over-the-counter and prescription acne products. Because the solubility of salicylic acid is greatly increased in hot water, the concentrations were prepared by adding a variable amount of salicylic acid to a set amount of hot water. Additionally, salicylic acid is more soluble in ethanol than hot water, so a small amount of ethanol was added to the hot water to increase the solubility of salicylic acid. The salicylic acid solutions were made by adding 0.1 g, 0.2 g, 0.5 g and 1.0 g of salicylic acid to 10 mL of hot water, and small amounts of 95% ethanol (100 microliters, 200 microliters, 500 microliters, and 1.0 milliliter respectively) were added to the boiling water. Using a micropipet, small sterile paper disks were saturated with 20 microliter diluted solutions of 1%, 2%, 5% and 10% salicylic acid, and placed in the center of the third of the agar plate allotted for each reagent. A disk containing twenty microliters of sterile water served as the negative control, to show the effects (if any) of bacterial inhibition in the sole presence of a sterile, wet paper disk. Sensi-Disc™ Antimicrobial Susceptibility Test Discs (Becton, Dickinson, and Company) containing a preset amount of ampicillin (at 10 µg) served as the positive control and allowed for a point of comparison against the salicylic acid solutions. In total, there were six reagents and disks used per “set”: a disk saturated in sterile water, a disk containing a preset amount of amoxicillin and disks with 1%, 2%, 5% and 10% concentrations of salicylic acid. There were a total of ten “sets,” for a total of twenty petri dishes used. The petri dishes were set up as indicated in Figure 1. The bacterial colonies were examined for zones of inhibition after fortyeight hours of incubation at 37 °C, and the zones of inhibition around the disks were measured with a ruler as the average diameter across in millimeters. Figure 1. A diagram depicting the arrangement of the six reagents for each “set.” The area of each petri dish were divided into thirds in case of potentially large zones of inhibition. Results The measurements for the zones of inhibition for each of the six solutions are shown in Table 1; the ampicillin had the highest average zone of inhibition, and the 10% salicylic acid had the lowest. The mean zone of inhibition for ampicillin was 22.25 mm and for sterile water was 6.85 mm. The mean zones of inhibition for 1%, 2%, 5%, and 10% salicylic acid were 7.89 mm, 6.55 mm, 6.55 mm, and 6.25 mm respectively. These values are illustrated in Figure 2. Conducting an ANOVA produced a p value less than 0.0001, which would signify a rejection of the null hypothesis that there is no difference between the antibacterial effectiveness of ampicillin and salicylic acid against Staphylococcus epidermidis. A Bonferroni correction was then conducted and suggested that our hypothesis should be accepted, that there is a difference in the efficacy of ampicillin and salicylic acid. However, the difference favored the ampicillin rather than the salicylic acid. The post hoc test suggests that there is no difference in the effectiveness of the four concentrations of salicylic acid to each other or to water. Table 1. Measured zones of inhibition (in mm) around each saturated disc per petri dish. As displayed in Figure 1, petri dishes 1-10 had the ampicillin, sterile water, and 1% salicylic acid solution, and petri dishes 11-20 had the 2%, 5%, and 10% salicylic acid solution. Plate Ampicillin (mm) Sterile water 1% (mm) salicylic acid (mm) 2% salicylic acid (mm) 5% salicylic acid (mm) 10% salicylic acid (mm) 1 23 7.5 6 2 21 7 * 3 23 7 7 4 21 6.5 8 5 24 7 11 6 11 7 7 7 26 6.5 8.5 8 24.5 7 9.5 9 25 6.5 6.5 10 24 6.5 7.5 11* 6 7 6 12 7 6.5 6 13 6.5 6.5 6 14 6 7 7 15 6 7 6.5 16 6.5 6 6.5 17 7 6 6.5 18 6 6 6 19 7.5 7 6 20 7 6.5 6 *Contamination present on petri dish. Figure 2. The mean zones of inhibition of the disks saturated in various solutions. There is a statistical difference between the zones of inhibition of ampicillin and salicylic acid (p < 0.0001, ANOVA). Performing a Bonferroni correction shows that there is no difference between water and the four concentrations of salicylic acid. Error bars are included ± SEM. Discussion The growth of Staphylococcus epidermidis was not significantly inhibited by increasing the salicylic acid concentrations in solution. The results of the analysis of variance support the original hypothesis in that there is a statistical difference between the antibacterial effects of salicylic acid and ampicillin. A subsequent Bonferroni correction supports the notion that none of the varying salicylic acid concentrations nor sterile water are statistically different from one another. It was initially predicted that ampicillin, as a prescribed oral antibiotic, would have antibiotic effects, which seems to be confirmed through the study. However, the prediction that the measured zones of inhibition would increase in size as the salicylic acid concentration increased was incorrect. One reason there may have been no difference in antibacterial activity between sterile water and the various concentrations of salicylic acid tested in this experiment was because the researchers experienced difficulties transferring the salicylic acid from the bottles to the paper disks. Salicylic acid is much more soluble in hot water than cold, so the water in the bottles was heated to boiling using a hot plate. When pipetting small 150 µL volumes onto the paper disks, it is theorized that some or most of the water boiled away, preventing the salicylic acid from making it onto the paper disk. The higher the concentration, the less water was in the pipet when transferring the solution onto the disks, and the faster that small amount of water would have evaporated; this was experimentally observed because the 5% and 10% solutions required more attempts to pipet onto the paper disks than the 1% or 2% solutions. To minimize the frequency of this happening, slightly larger volumes should be delivered with the micropipet to compensate for evaporation of some of the liquid in the pipet tip. Alternately, a solution of salicylic acid and water may be able to be purchased online, eliminating the error inherent in making the solutions from scratch. If this were the case, one need only add more water to dilute the solution to the required concentration, and there would be no need for measuring variable amounts of salicylic acid and ethanol or boiling water. Since salicylic acid is more soluble in ethanol than water, an amount of ethanol proportional to each concentration was added to help the acid dissolve. This small amount of ethanol may have slightly increased values which may otherwise have been lower because ethanol is a known antimicrobial compound. For example, instead of seeing no significant difference between 1% and 2% salicylic acid solutions, a small increase in the average zone of inhibition may have been observed. However, the amount of ethanol to water was 10% or less (0.1 mL, 0.2 mL, 0.5 mL and 1 mL were added to the 10 mL of water used to make each concentration), so the effect of ethanol on the zone of inhibition should be negligible. Other studies might examine the correlation between salicylic acid and other potential antibiotics or the effect of salicylic acid concentration on different strains of S. epidermidis. Alternately, salicylic acid may be tested on other gram-positive bacteria to see if they are equally resistant to the same concentrations tested on S. epidermidis. Salicylic acid concentrations of 1%, 2%, 5% and 10% were chosen to simulate concentrations found in acne medications, but perhaps salicylic acid may have antibacterial properties on its own at higher concentrations; it may simply not be an effective antibiotic on its own. Further studies may look at higher concentrations outside of current medication ranges. Acknowledgements The researchers would like to thank Professor Steve Teh for his advice and guidance in conducting this study as well as their colleague Faith for preparing the agar medium used for the petri plates. Literature Cited Akhavan, Arash, Bershad, Susan. 2003. Topical Acne Drugs Review of Clinical Properties, Systemic Exposure, and Safety. American Journal of Clinical Dermatology. Vol. 4 (7): 473-492. Bergler-Czop, B. 2014. The aetiopathogenesis of acne vulgaris - what’s new? International Journal of Cosmetic Science. Vol. 36 (1): 187-194. Bhate, K., Williams, H. C. 2012. Epidemiology of acne vulgaris. British Journal of Dermatology. Vol. 168 (1): 474-485. Bhatia, Ajay, Maisonneuve, Jean-Francoise and Persing, David H. 2004. The Infectious Etiology of Chronic Diseases: Defining the Relationship, Enhancing the Research, and Mitigating the Effects- Workshop Summary. Institute of Medicine of the National Academies. (1): 74-80. Cook, David, Krassas, George, and Huang, Tom. 2010. Acne - Best practice management. Australian Family Physician. Vol. 39 (9): 656-660. Gottenbos, B., van der Mei, H. C., Busscher, H. J. 2000. Initial adhesion and surface growth of Staphylococcus epidermidis and Pseudomonas aeruginosa on biomedical polymers. Journal of Biomedical Materials Research. Vol. 50 (2): 208-214. Kupferwasser, Leon Iri, Yeaman, Michael R., Nast, Cynthia C., Kupferwasser, Deborah, Xiong, Yan-Qiong, Palma, Marco, Cheung, Ambrose L. and Bayer, Arnold S. 2003. Salicylic acid attenuates virulence in endovascular infections by targeting global regulatory pathways in Staphylococcus aureus. The American Society for Clinical Investigation. Vol. 112 (2): 222–233. Nishino, Chikao, Enoki, Nobuyasu, Tawata, Shinkichi, Mori, Akihisa, Kobayashi, Koji and Fukushima, Masako. 1986. Antibacterial Activity of Flavonoids against Staphylococcus epidermidis, a Skin Bacterium. Agricultural and Biological Chemistry. Vol. 51 (1): 139-143. Singh, Paramjit, Sihorkar, V., Jaitely, Vikas, Kanaujia, P., Vyas, S. P. 2000. Pilosebaceous unit: anatomical considerations and drug delivery opportunities. Indian Journal of Pharmacology. Vol. 32 (1): 269-281. Toyoda, M. and Morohashi, M. 1998. An Overview of Topical Antibiotics for Acne Treatment. Dermatology (196): 130-134.