prehospital pharmacology cheat sheet
advertisement

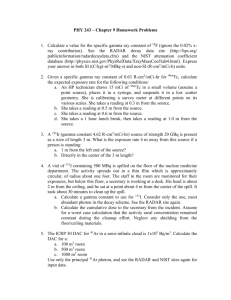
PREHOSPITAL PHARMACOLOGY CHEAT SHEET Amy Gutman MD ~ February 2014 This information is provided as a summary of basic information needed to treat patients and study for Board Reviews. Dosages reflect national standards and may be slightly different that OEMS 2% LIDOCAINE GEL Class: Acetamide local anesthetic Actions: Stabilizes nerve membrane by inhibiting initiation /conduction of pain impulses Indications: Procedural anesthetic lubricant, gastritis (GI cocktail) C/I: Allergy, familial malignant hyperthermia Side Effects: Anxiety, seizures, AMS, blurred vision, respiratory depression, bradycardia, hypotension Critical Info: Few systemic effects Dose: Apply small amount of gel to external ETT surface for lubrication ACTIVATED CHARCOAL Class: Adsorbent Actions: Adsorbs toxic substances from GI tract Indications: Oral poisonings / medication overdoses C/I: Depressed gag reflex, after ingestion of corrosives, caustics or petroleum distillates Side Effects: N/V, black stool (not GI bleeding); bonds /inactivates most medications in GI tract Critical Info: Does not adsorb cyanide, lithium, iron, lead or arsenic Dose: Adult/ Pediatric: 1-2 gm/kg mixed with 6-8 oz water PO/NGT ADENOSINE / ADENOCARD Class: Class V antiarrhythmic, naturally occurring nucleoside Actions: Slows AV node conduction, interrupts AV reentry pathways (SVT) Indications: PSVT refractory to vagal maneuvers C/I: 2nd/3rd degree HB, sick sinus syndrome; theophylline decreases effectiveness Side Effects: Facial flushing, headache, SOB, dizziness, nausea Critical Info: Transient arrhythmias / asystole at time of cardioversion; caution in COPD, ½ life 5 secs Dose: Adult: 6mg rapid IVP; may repeat at 12mg x 2 ALBUTEROL / PROAIR Class: Sympathetic Agonist Actions: Sympathomimetic selective for beta-2 adrenergic receptors causing bronchodilation Indications: Asthma, bronchospasm associated with COPD C/I: Cautious in the elderly, known cardiovascular disease, HTN Side Effects: Anxiety, dizziness, HA, tremor, HTN, arrhythmias, CP, N/V Critical Info: Worsens tachycardia; beta blockers may blunt the effects of Albuterol. Dose: 2.5 mg in 3mL NS via nebulizer, repeat as needed. AMIODARONE Class: Class III antiarrhythmic (non-competitive sodium channel blocker) Actions: Lengthens cardiac action potential. Negative chronotropic effect on nodal tissue. Blocks potassium channels prolonging conduction refractoriness. Vasodilatation decreases myocardial oxygen consumption Indications: Ventricular arrhythmias unresponsive to other antiarrythmics C/I: Breast-feeding, bradycardia, 2nd/3rd degree HB. Side Effects: Hypotension, bradycardia, arrythmogenic via prolongation of PR/QRS /QT intervals Critical Info: Caution in CHF, causes pulmonary toxicity, warfarin toxicity Dose: Unstable: 300mg IV/IO; 150mg in conscious / stable Prehospital Pharmacology Cheat Sheet Page 1 ASPIRIN Class: Actions: Indications: C/I: Side Effects: Critical Info: Dose: ATROPINE Class: Actions: Indications: C/I: Side Effects: Critical Info: Dose: Platelet aggregator inhibitor, NSAID Anti-inflammatory, inhibitor of platelet function. Blocks formation of thromboxane A2, causing platelet aggregation and arterial constriction Chest pain Relatively contraindicated if active ulcer disease, NSAID allergies or asthma Heartburn, GI bleeding, nausea, vomiting, wheezing, and prolonged bleeding. Can be given PR if patient vomiting 324-325mg (4 81mg chewable tablets) Anticholinergic, parasympatholytic Respiratory emergencies (bronchodilator, dries respiratory secretions). Organophosphate poisoning antidote. Bradycardia: reduces vagal tone, increases SA node automaticity, increases AV conduction. Positive chronotrope, little inotropic effect. Bradycardia, asystole, COPD, bronchospasm, organophosphate overdose No significant prehospital contraindications Blurred vision/ mydriasis, dry mouth, tachycardia, drowsiness, confusion, arrhythmia, anxiety, dizziness, HA, rash, N/V May worsen bradycardia if 2nd/3rd degree AV blocks (consider pacing); no response in post-cardiac transplant patients (no vagus nerve) Bradycardia 0.5-1mg IV/IO, may repeat in 5 min up to 1mg. Asystole: 1mg IV/IO, may repeat every 3 mins to max 0.04 mg/kg Organophosphate Toxicity: 2-5mg IV/IM/IO every 10-15 mins Pediatrics: 0.05 mg/kg IV/IM/IO every 10- 15 minutes to max 3mg CALCIUM CHLORIDE 10% Class: Calcium supplement Actions: Increases myocardial contractile force and ventricular automaticity Indications: Magnesium / calcium channel blocker OD; treatment for hyperkalemia, hypocalcemia C/I: May precipitate digitalis toxicity Side Effects: Bradycardia, arrhythmias, syncope, N/V, cardiac arrest Dose: Adult: 4mg/kg IVP, 25-50mg IM Pediatrics: 0.5mg/kg IM; 1mg/kg PR CETACAINE / BENZOCAINE / TETRACAINE Class: Cholinesterase (ester) anesthetic Actions: Local anesthetic, blocks initiation & conduction of pain impulses. Reversible nerve conduction blockade by decreasing sodium nerve membrane permeability. Decreases rate of membrane depolarization, increasing electrical excitability threshold. Indications: Anesthesia of all mucous membranes except eyes; limits gagging for NTI C/Is: Application to large open wounds, cholinesterase deficiencies, methemoglobinemia Side Effects: Contact dermatitis, erythema, pruritus, vesiculation, urticaria, edema, anaphylaxis Dizziness, lethargy, sweating; arrhythmia, tremor, N/V, dyspnea, anxiety, eye irritation Critical Info: Only use the formulation specifically for eyes (tetracaine) in eyes; may enhance effects of CNS depressants, hypotension if used with vasodilators Dose: 14%, 2% Gel/Liquid/Spray, apply for 1-2 secs; 1-2 drops in eye; may repeat in 5 mins Prehospital Pharmacology Cheat Sheet Page 2 CYANOKIT / HYDROXYCOBALAMIN Class: Vitamin B Actions: Cyanide causes rapid death via cytochrome oxidase inhibition (stops cellular respiration). Cyanide binds with mitochromial cytochrome a3, prevents cell from using oxygen, forcing anaerobic metabolism, lactate production, cellular hypoxia and metabolic acidosis. Hydroxycobalamin binds cyanide ions forming cyanocobalamin, which is excreted in urine rapidly increasing BP/HR, due to improving cellular respiration Indications: Suspected hydrogen cyanide exposure / toxicity C/Is: None Side Effects: Transient photosensitivity, red skin & urine coloration Critical Info: Cyanide poisoning must be recognized and treated quickly. Antidote must be used in conjunction with aggressive airway and cardiopulmonary resuscitation Dose: 5g IV over 15 minutes; 2nd dose of 5g over 15mins-2 hrs if clinically indicated DEXTROSE Class: Actions: Indications: C/I: Side Effects: Critical Info: Dose: Carbohydrate, hypertonic solution Rapidly increases serum glucose levels with short-term osmotic diuresis Hypoglycemia, AMS, coma of unknown etiology, seizure of unknown etiology ICH, head injury. Interacts with sodium bicarbonate, warfarin Warmth, pain, burning, thrombophlebitis, tissue necrosis, rhabdomyolysis Thiamine prior to D50 in alcoholics. Do not give if suspected CVA with normal glucose Adult: 50% 25g D5W (50mL) IV Pediatric: 25% 0.5-1 gm/kg/dose slow IV; may be repeated as necessary DIAZEPAM / VALIUM Class: Benzodiazepine, GABA inhibitory neurotransmitter Actions: Hypnotic, sedative, anxiolytic, amnesic, anticonvulsant, muscle relaxant. GABA inhibitor (major CNS inhibitory neurotransmitter) Indications: Anxiety / agitation, alcohol withdrawal, muscle relaxant, seizures, procedural analgesia C/I: Glaucoma, coma, shock, substance abuse, head injury. Pregnancy category D Side Effects: Respiratory depression, hypotension, somnolence, ataxia, reflex tachycardia, phlebitis Critical Info: Multiple drug incompatibilities. Flumazenil (benzo antagonist) causes acute withdrawal if chronic benzodiazepine usage, resulting in intractable seizures. Pregnancy category C Dose: Adult: 5-10mg IV/IM to max 30mg Sedation for cardioversion: 5- 15 mg IV over 5 mins Pediatric: 0.2-0.3 mg/kg (0.5-2mg) slow IV; PR 0.5mg/kg every 15-30 mins to max 10mg DILTIAZEM / CARDIAZEM Class: Class IV antiarrythmics, calcium channel blocker Actions: Slows AV nodal conduction time, prolongs AV refractoriness. Blocks influx of calcium ions into cardiac muscle, prevents spasm of coronary arteries, arterial and venous vasodilator to reduce preload, afterload and myocardial oxygen demand. Indications: Control of rapid ventricular rates due to AF / Aflutter, SVT, angina C/I: Hypotension, sick sinus syndrome, 2nd/3rd degree HB, cardiogenic shock, wide-complex tachycardias, pregnancy category C Side Effects: Bradycardia, 2nd/3rd degree AV blocks, CP, CHF, syncope, VF/VT, N/V, dizziness, SOB, HA Critical Info: Caution in patients using medications that affect cardiac contractility (i.e. beta blockers) Dose: 0.25mg/kg (1st dose), 0.35mg/kg (2nd dose); infusion 5-15 mg / hr Prehospital Pharmacology Cheat Sheet Page 3 DIPHENHYDRAMINE / BENADRYL Class: Antihistamine, anticholinergic, sedative Actions: Blocks histamine1 receptor stimulation (bronchoconstriction, visceral contractions) and histamine2 receptor stimulation (peripheral vasodilation, gastric acid secretion) Indications: Anaphylaxis, allergic reactions, dystonic reactions accompanying phenothiazines C/I: Asthma, breastfeeding Side Effects: Sedation, dries bronchial secretions, blurred vision, HA, palpitations, tachycardia Critical Info: Effects potentiated with other CNS depressants Dose: Adult: 25-50mg IV/IM/PO Pediatric: 1-2 mg/kg IV/IO/IM. PO: 5 mg/kg/24hrs DOPAMINE / INTROPIN Class: Sympathetic agonist, naturally occurring catecholamine Actions: Dose-dependent effect on alpha-adrenergic receptors (peripheral vasoconstriction). Inotropic effect on myocardium (increased cardiac output, peripheral vasoconstriction and pulmonary occlusive pressure).Positive inotropic effect on beta-1 receptors. Dopaminergic effect maintains renal and mesenteric blood flow via increasing systolic and pulse pressures (less effect on diastolic pressure) Indications: Significant hypotension not resulting from hypovolemia, cardiogenic shock C/Is: Pheochromocytoma. Not used as sole agent in management of hypovolemic shock Side Effects: Deactivated by alkaline solutions. Anxiety, HA, arrhythmias, CP, SOB, N/V Critical Info: Induce or worsen SVT and ventricular arrhythmias. Hypotension when used concomitantly with phenytoin (dilantin) Dose: 400mg in 250cc (1600mcg/cc concentration; 2-20mcg/kg/min titrated to effect EPINEPHRINE Class: Sympathetic agonist, naturally occurring catecholamine Actions: Direct effects on alpha and beta-adrenergic receptors increases HR, cardiac contractile force, myocardial electrical activity, systemic vascular resistance, BP, and automaticity. Bronchodilator. Effects within 90 secs of administration, effect for 3-5 mins Indications: Asystole, PEA, cardiac arrest, bronchospasm (asthma, COPD, anaphylaxis) C/Is: Bronchospasm: Underlying cardiovascular disease, HTN Side Effects: Arrhythmia, anxiety, tremor, HA dizziness, N/V, cardiac ischemia and increased myocardial oxygen demand Critical Info: Protect from light. Deactivated by alkaline solutions. Dose: Adult Arrest: 1mg 1:10,000 IV/IO every 3-5 min Pediatric Arrest: 0.01mg/kg 1:10,000 IV/IO (~1mg in 10cc); Subsequent 0.1mg/kg IV/IO Adult Allergic: 0.3-0.5 1:1,000 SQ every 5 min (~3mg); 0.5-1mg 1:10,000 IV Pediatric Allergic: 0.01mg/kg 1:1,000 SQ every 5 min; 0.01mg/kg 1:10,000 IV FENTANYL / SUBLIMAZE Actions: Narcotic Analgesic Indications: Analgesia for trauma, chest pain, procedural premedication C/Is: Respiratory depression, hypotension; pregnancy category C Side Effects: Respiratory depression/ arrest, apnea, chest rigidity, bradycardia, hypotension, paradoxical HTN, cardiac arrest, N/V, dizziness, blurred vision, laryngospasm, Critical Info: 100mcg analgesic equivalent to 10mg morphine or 75mg meperidine Dose: Adult: 1 mcg/kg to max 150mcg. slow IV/IM/IN Prehospital Pharmacology Cheat Sheet Page 4 FUROSEMIDE / LASIX Class: Loop diuretic Actions: Inhibits NaCl reabsorption in proximal and distal renal tubules and loop of Henle. Direct vasodilator (onset in 5-10 mins, onset of diuresis in 20-30 mins) Indications: CHF, pulmonary edema, HTN emergency C/I: Pregnancy, sulfa allergy Side Effects: HA, dizziness, hypotension, volume depletion, potassium depletion, arrhythmias, N/V Critical Info: Protected from light Dose: Adult: 40-120 mg slow IV Pediatric: 1 mg/kg slow IV GLUCAGON Class: Actions: Indications: C/I: Side Effects: Critical Info: Dose: GLUCOSE Class: Actions: Indications: C/Is: Side Effects: Critical Info: Dose: Hormone, antihypoglycemic Breakdown of stored glycogen to glucose, inhibits synthesis of glycogen from glucose. Positive cardiac inotrope, decreases renal vascular resistance Hypoglycemia, beta-blocker and calcium channel overdoses Caution if history of cardiovascular or renal disease. Hypotension, dizziness, headache, N/V Slow return to consciousness following administration (5-20 mins) Treats beta blocker OD (bypasses beta adrenergic signaling system). High levels from pancreatic tumors (insulin-resistant hyperglycemia). Only effective if glycogen stores in liver Adult: 1mg IM/SC, may repeat in 5 mins Pediatrics: 0.1mg/kg IM/SC/IV (<10kg); 1mg/kg IM/SC/IV (>10kg) Beta-blocker OD: 50-150 mg/kg IV/IO Monosaccharide, carbohydrate Distributed in tissues / CNS producing rapid increase in circulating blood sugar AMS with history of diabetes & demonstrated low blood sugar Not alert, unable to swallow, depressed gag Hyperglycemia Do not given to patient with suspected stroke and normal blood sugar 25-50gm IV/IO IPRATROPIUM / ATROVENT Class: Anticholinergic, parasympatholytic Actions: Chemically related to atropine. Blocks acetylcholine receptors, inhibiting parasympathetic stimulation. Causes bronchodilation, dries respiratory secretions. Indications: Asthma, reversible bronchospasm associated with COPD C/I: Soybean / peanut allergy Side Effects: Arrhythmia, anxiety, dizziness, HA, tremor, HTN, CP, N/V Critical Info: Caution in elderly, cardiovascular disease, HTN Dose: Adult: 500mcg in 2.5-3mL NS via nebulizer; 2 sprays of a MDI Pediatric: 125-250mcg in 2.5-3ml NS via nebulizer, 1-2 sprays of a MDI LIDOCAINE Class: Actions: Class Ib antiarrhythmic, amide anesthetic Decreases ventricular automaticity, depresses ventricular depolarization automaticity but increases VF threshold by increasing phase IV repolarization Prehospital Pharmacology Cheat Sheet and Page 5 Indications: C/I: Side Effects: Critical Info: Dose: VF/VT, malignant PVCs 2nd/3rd degree HB AMS, seizures, hypotension, bradycardia, heart blocks, N/V High doses can result in seizures, coma, death; effects potentiated with other antiarrythmics. No longer 1st line ACLS medication as of 2010 VT/VF 1-1.5 mg/kg IV repeated every 3-5min to 3mg/kg, follow with 2- 4 mg/min drip Peds: 1mg/kg IV, repeat every 3-5 min to 3mg/kg, follow with 20-50 mcg/kg/min drip MAGNESIUM SULFATE Class: Antiarrhythmic, mineral, electrolyte Actions: Essential for numerous biochemical reactions (ATD, ADP). Limits seizure by blocking neuromuscular transmission and decreasing acetylcholine liberated at motor endplates. CNS depressant without effects on fetus (eclampsia). Peripheral vasodilatator. Indications: Refractory VF / VT, torsades, post-MI for arrhythmia; severe bronchospasm, eclampsia C/I: Shock, 3rd degree HB, dialysis, hypocalcemia; arrhythmias with digitalis Side Effects: Flushing, sweating, bradycardia, decreased DTRs, drowsiness, respiratory depression, arrhythmia, hypotension, hypothermia, itching, rash. Critical Info: As hypermagnesemia can occur, calcium chloride should be available as an antidote Dose: VF/VT/Torsades: 1-2g IV over 2 min followed by infusion of 0.5-1g/hr AMI: 1-2g IV over 5-30 min Eclampsia: 2- 4g IV/IM METHYLPREDNISOLONE / MEDROL Class: Synthetic corticosteroid, anti-inflammatory Actions: Potent anti-inflammatory related to natural adrenal cortex hormones Indications: Allergic reactions, asthma, anaphylaxis, COPD C/I: None in prehospital setting Side Effects: GI bleed, prolonged wound healing, adrenal gland suppression, edema, CHF, HTN, vertigo, HA, nausea, malaise, hiccups Critical Info: Onset of action 20-40 mins, ½ life 3- 4 hours Dose: 125mg IV/IO/IM MIDAZOLAM / VERSED Class: Benzodiazepine Actions: Potent, short-acting CNS depressant, sedative / hypnotic / amnestic Indications: Premedication before cardioversion, anti-seizure, muscle relaxant C/I: Hypersensitivity, narrow angle glaucoma, shock Side Effects: Laryngo/bronchospasm, respiratory depression, AMS, arrhythmia (bradycardia), N/V Critical Info: Potential for respiratory depression. 2-4 times more potent than diazepam Dose: Adult: 0.5-2.5 mg slow IVP; may repeat to max 0.1mg/kg Pediatric: To facilitate ETI medical control may order: 0.05-0.1mg/kg IV to max 5 mg MORPHINE Class: Actions: Indications: C/I: Side Effects: Narcotic analgesic Acts on CNS opiate receptors causing analgesia and sedation. Decreases preload, increases peripheral vasodilatation, decreases myocardial oxygen demand Severe pain Volume depletion, hypotension, hypersensitivity, head injury, +/- abdominal pain N/V, abdominal cramps, miosis, AMS, HA, respiratory depression Prehospital Pharmacology Cheat Sheet Page 6 Critical Info: Dose: Can cause severe respiratory depression; Naloxone available as an antagonist. Adult: 1-3 mg(0.1mg/kg) IV/IM/SC/IO every 5 mins titrated to maximum of 10 mg Pediatric: 0.1-0.2 mg/kg/dose IV/ IO/IM/SC every 5 mins titrated to max 5 mg NALOXONE / NARCAN Class: Narcotic antagonist Actions: Antagonizes opiate effects by competing at same receptor sites Indications: Chemically similar to narcotics but with antagonistic properties reversing respiratory depression from OD. Competitively displaces narcotic molecules from opiate receptors. C/I: Known hypersensitivity; abrupt and complete reversal can cause acute withdrawal Side Effects: Hypotension, HTN, ventricular arrhythmias, N/V Critical Info: Almost Immediate effects. Rarely causes non-dose dependent pulmonary edema Dose: Adult: 0.4-2mg IV/IM/IN; may repeat up to max 10mg Pediatric: 0.01 mg IV/IM/IN; may repeated up to max 10mg MORPHINE Class: Actions: Indications: C/I: Side Effects: Critical Info: Dose: Schedule II opiod analgesic Suppresses CNS pain, anxiety, respiratory centers. Decreases venous return, preload, afterload and myocardial oxygen demand. Analgesia for moderate to severe pain, CHF, pulmonary edema, chest pain Head injury, apnea, hypotension, AMS, hypovolemia; pregnancy category C. Respiratory depression, hypotension, AMS, N/V bradycardia, tachycardia, syncope, facial flushing, euphoria, bronchospasm, dry mouth Caution in geriatrics, COPD, asthma; vagotonic effect in inferior STEMI (bradycardia, heart block); naloxone readily available as antidote. Adult: 0.1mg/kg every 5 mins to max of 10mg IV/IO/IM/SC Pediatric: 0.1-0.2 mg/kg every 5 mins to max of 5mg IV/IO/IM/SC NITROGLYCERIN Class: Nitrate, direct vasodilator Actions: Potent smooth muscle relaxant and direct vasodilator acts primarily on peripheral venous system, with direct effects on coronary arteries (vasodilatation). Decreases venous return (decreases cardiac workload and myocardial oxygen demand) Indications: CP, angina pectoris, STEMI/NSTEMI, pulmonary edema, HTN emergency C/I: Hypotension, increased intracranial pressure Side Effects: HA (cerebral vessel vasodilation), dizziness, weakness, tachycardia, hypotension, orthostasis, rash, dry mouth, N/V Critical Info: Profound hypotension if used within 24hrs of erectile dysfunction meds (compounded vasodilatation). Rapidly deteriorates in sunlight. Tolerance over time. Dose: 0.4 mg SL/spray; may repeat x 3 every 5 mins. ½ inch topical ointment ODANSETRON / ZOFRAN Class: Selective serotonin-antagonist, antiemetic Actions: Blocks serotonin peripherally (vagus nerve terminals), and at CNS chemoreceptor zon Indications: Treatment and prevention of nausea and vomiting C/I: Allergy, QT prolongation; pregnancy category B Side Effects: Headache, drowsiness, pruritus Critical Info: May prolong QT interval causing arrhythmia (torsades) Dose: Adult: 4mg IV/IM Pediatric: <30kg 1 mg. IV/IM; >30kg 2 mg. IV/IM. Prehospital Pharmacology Cheat Sheet Page 7 PROCAINAMIDE / PRONESTYL Class: Class Ia antiarrhythmic, ester-type local anesthetic Actions: Reduces automaticity of AV/SA nodes, slows intra-ventricular conduction Indications: Ventricular arrhythmias refractory to lidocaine C/I: 2nd / 3rd degree HB, sick sinus syndrome, multifocal PVCs Side Effects: Hypotension, lethargy, seizures, AMS, bradycardia, heart blocks, N/V, cardiac arrest Critical Info: No longer 1st line ACLS medication as of 2010 Dose: Adult: 20-50 mg/min until arrhythmia controlled, hypotension occurs, QRS complex widens by 50% original width, or max 17 mg/kg Pediatric: 3-6 mg/kg (max 100mg/dose); may repeat every 5mins to max 15 mg/kg SODIUM BICARBONATE Class: Alkalinizing salt Actions: Acts as by combining with excess body acids to form a weak acid which is broken down into CO2 and H2O. Increases urine pH speeding excretion Indications: TCA / phenobarbital antidepressant OD, severe acidosis, hyperkalemia C/I: No significant prehospital interactions Side Effects: May deactivate catecholamines and vasopressors (i.e epinephrine, dopamine) Critical Info: Metabolic alkalosis (large quantities) eventually causes metabolic acidosis secondary to CO2 production. Causes calcium chloride precipitation if used in save IV line Dose: Adults/Pediatric: 1mEq/kg IV/IO, then 0.5 mEq/kg/10min THIAMINE Class: Actions: Indications: C/I: Side Effects: Dose: Vitamin BI Converts pyruvic acid to acetyl coenzyme A allowing utilization of energy from glucose Coma, especially in alcoholics (Wernicke’s encephalopathy, Korsakoff’s psychosis, DTs) None Hypotension, dyspnea, respiratory failure Adult: 50-100mg IV/IM Pediatric: 10-25 mg IV/IM VASOPRESSIN Class: Pituitary antidiuretic hormone, non-adrenergic peripheral vasoconstrictor Actions: Effects via direct stimulation of smooth muscle. Increases coronary perfusion pressure, vital organ blood flow and oxygen delivery. Vasoconstriction of splanchnic, portal vessels, peripheral, cerebral, pulmonary, and coronary vessels Indications: Alternative to epinephrine (VF/VT), hemodynamic support in vasodilatory shock, vasoconstriction for esophageal varices C/I: Vascular disease, angina pectoris. Side Effects: N/V, tremor, sweating, vertigo, skin blanching, bronchoconstriction, water intoxication (lethargy, HA, coma, convulsions). Critical Info: May provoke cardiac ischemia. High doses of epinephrine, heparin, or ETOH decrease response to Vasopressin. Dose: Arrest: 40 units IV (single dose) Esophageal Varices: 0.2 to 0.4 units/min IV drip. REFERENCES www.Drugs.com, www.id44.com, www.EMSNOTES.com, OEMS Prehospital Protocols. 2013, www.NAEMSE.org, www.EMSSuccess, Brian Bledsoe MD, Brady 11th Edition Prehospital Pharmacology Cheat Sheet Page 8