New Zealand trigger tool adverse event subcategories
advertisement
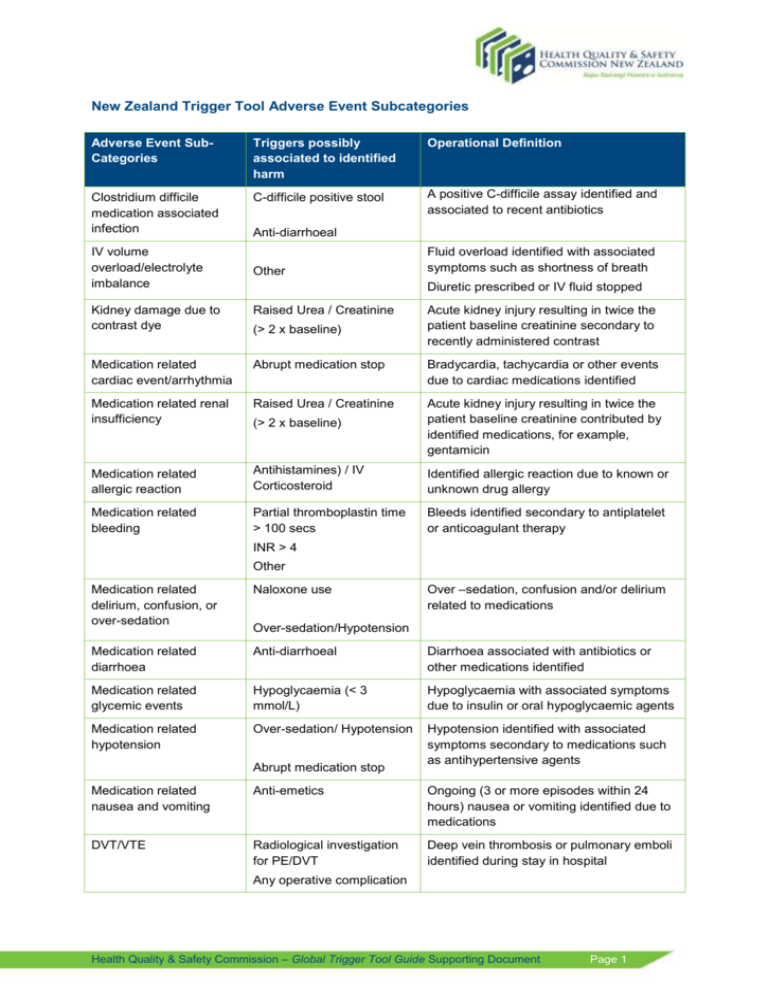
New Zealand Trigger Tool Adverse Event Subcategories Adverse Event SubCategories Triggers possibly associated to identified harm Operational Definition Clostridium difficile medication associated infection C-difficile positive stool A positive C-difficile assay identified and associated to recent antibiotics IV volume overload/electrolyte imbalance Anti-diarrhoeal Other Fluid overload identified with associated symptoms such as shortness of breath Diuretic prescribed or IV fluid stopped Kidney damage due to contrast dye Raised Urea / Creatinine Medication related cardiac event/arrhythmia Abrupt medication stop Bradycardia, tachycardia or other events due to cardiac medications identified Medication related renal insufficiency Raised Urea / Creatinine (> 2 x baseline) Acute kidney injury resulting in twice the patient baseline creatinine contributed by identified medications, for example, gentamicin Medication related allergic reaction Antihistamines) / IV Corticosteroid Identified allergic reaction due to known or unknown drug allergy Medication related bleeding Partial thromboplastin time > 100 secs Bleeds identified secondary to antiplatelet or anticoagulant therapy (> 2 x baseline) Acute kidney injury resulting in twice the patient baseline creatinine secondary to recently administered contrast INR > 4 Other Over –sedation, confusion and/or delirium related to medications Medication related delirium, confusion, or over-sedation Naloxone use Medication related diarrhoea Anti-diarrhoeal Diarrhoea associated with antibiotics or other medications identified Medication related glycemic events Hypoglycaemia (< 3 mmol/L) Hypoglycaemia with associated symptoms due to insulin or oral hypoglycaemic agents Medication related hypotension Over-sedation/ Hypotension Hypotension identified with associated symptoms secondary to medications such as antihypertensive agents Over-sedation/Hypotension Abrupt medication stop Medication related nausea and vomiting Anti-emetics Ongoing (3 or more episodes within 24 hours) nausea or vomiting identified due to medications DVT/VTE Radiological investigation for PE/DVT Deep vein thrombosis or pulmonary emboli identified during stay in hospital Any operative complication Health Quality & Safety Commission – Global Trigger Tool Guide Supporting Document Page 1 Fall with injury Patient fall A fall with injury as a result of medications, equipment failure or failure of adequate staffing or care Skin tear, abrasion, or other breakdown Any procedure/treatment complication Identified trauma to the skin from a medical intervention, for example, skin tear secondary to removal of plasters such as Tegaderm. Other Stage I or II pressure ulcer Pressure Ulcer/injury Pressure injury presenting as intact skin with redness over a localised area or partial thickness loss of dermis without slough. Stage III or IV pressure ulcer Pressure Ulcer/injury Pressure injury presenting as full thickness tissue loss with or without visible bone, tendon or muscle exposure Catheter associated urinary tract infection Healthcare associated infection Urinary tract infection identified due to the presence of a catheter Positive blood culture Central line associated blood stream infection Healthcare associated infection Central line associated septicaemia identified Positive blood culture Peripheral or central line non-blood stream infection Healthcare associated infection Respiratory infection (non-ventilator associated) Healthcare associated infection Surgical infection Healthcare associated infection Line Infection secondary to insertion of peripheral or central lines Positive blood culture Hospital acquired pneumonia or respiratory tract infection Positive blood culture Identified surgical site infections Positive blood culture Ventilator associated pneumonia Healthcare associated infection Respiratory infections associated to mechanical ventilation Pneumonia onset Abnormal bleeding following surgery or procedure Decrease of greater than 25% in Hb or Hct Transfusion/use of blood Excessive bleeding following surgery that required blood transfusion or return to theatres/ monitoring Blood clots and other occlusions related to surgery or procedure Decrease of greater than 25% in Hb or Hct Haematomas, pulmonary emboli or deep vein thrombosis identified following surgery Cardiac complications related to surgery or procedure Post-op troponin level greater than 1.5 ng/ml Radiological investigation for PE/DVT Any operative complication Any cardiac complications, for example, myocardial infarct, identified during surgery or postoperatively Health Quality & Safety Commission – Global Trigger Tool Guide Supporting Document Page 2 Complications related to peripheral venous or arterial puncture Any operative complication Complications such as pseudo-aneurysm or sepsis identified as a result of arterial or venous cannulation Hypotension/blood loss Transfusion/use of blood Hypotension with associated symptoms due to blood loss in surgery Decrease of greater than 25% in Hb or Hct Post-op acute renal failure Acute dialysis Raised Urea / Creatinine (> 2 x baseline) Acute kidney injury occurred as a result of surgery resulting in creatinine to be more than twice patient baseline Any operative complication Post-op spinal tap headache Any operative complication Headache associated with any procedure which can occur 1 – 5 days after Premature extubation causing respiratory failure Intubation/reintubation/BiPap in PACU Respiratory depression as a result of early removal of tube Mechanical ventilation > 24 hours post-op Prolonged post-op ileus Any operative complication Diagnosis of ileus with nil bowel movement for 3 days or more for non-abdominal surgery and 4 days or more for abdominal surgery, with associated symptoms. Radiation related injury Any procedure/treatment complication Any injury or associated symptoms due to radiation poisoning Any operative complication Removal retained foreign body Return to theatre X-ray intra-op or in PACU Surgical mishap identified as a result of retained foreign object after surgery Removal, injury or repair of organ Injury, repair or removal of organ Unintended removal, injury or repair of organ identified Respiratory complications related to surgery or procedure Intubation/reintubation/BiPap in PACU A complication postoperatively or due to any procedure that resulted in respiratory depression Other Other Mechanical ventilation > 24 hours post-op Any adverse event as a result of medical intervention that cannot be placed in any other subcategory Health Quality & Safety Commission – Global Trigger Tool Guide Supporting Document Page 3