Acute Coronary Syndrome
advertisement
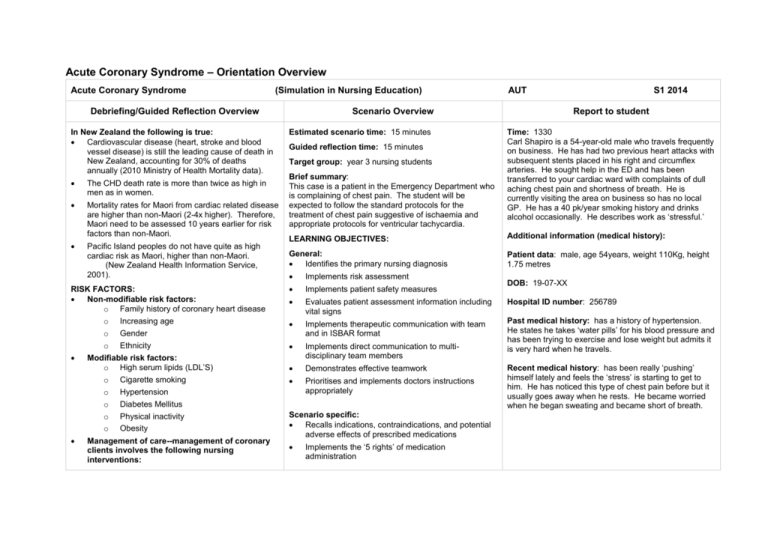
Acute Coronary Syndrome – Orientation Overview Acute Coronary Syndrome (Simulation in Nursing Education) Debriefing/Guided Reflection Overview In New Zealand the following is true: Cardiovascular disease (heart, stroke and blood vessel disease) is still the leading cause of death in New Zealand, accounting for 30% of deaths annually (2010 Ministry of Health Mortality data). The CHD death rate is more than twice as high in men as in women. Mortality rates for Maori from cardiac related disease are higher than non-Maori (2-4x higher). Therefore, Maori need to be assessed 10 years earlier for risk factors than non-Maori. Pacific Island peoples do not have quite as high cardiac risk as Maori, higher than non-Maori. (New Zealand Health Information Service, 2001). RISK FACTORS: Non-modifiable risk factors: o Family history of coronary heart disease o Increasing age o Gender o Ethnicity Modifiable risk factors: o High serum lipids (LDL’S) o Cigarette smoking o Hypertension o Diabetes Mellitus o Physical inactivity o Obesity Management of care--management of coronary clients involves the following nursing interventions: AUT Scenario Overview Estimated scenario time: 15 minutes Guided reflection time: 15 minutes Target group: year 3 nursing students Brief summary: This case is a patient in the Emergency Department who is complaining of chest pain. The student will be expected to follow the standard protocols for the treatment of chest pain suggestive of ischaemia and appropriate protocols for ventricular tachycardia. S1 2014 Report to student Time: 1330 Carl Shapiro is a 54-year-old male who travels frequently on business. He has had two previous heart attacks with subsequent stents placed in his right and circumflex arteries. He sought help in the ED and has been transferred to your cardiac ward with complaints of dull aching chest pain and shortness of breath. He is currently visiting the area on business so has no local GP. He has a 40 pk/year smoking history and drinks alcohol occasionally. He describes work as ‘stressful.’ LEARNING OBJECTIVES: Additional information (medical history): General: Identifies the primary nursing diagnosis Patient data: male, age 54years, weight 110Kg, height 1.75 metres Implements risk assessment Implements patient safety measures Evaluates patient assessment information including vital signs Hospital ID number: 256789 Implements therapeutic communication with team and in ISBAR format Implements direct communication to multidisciplinary team members Past medical history: has a history of hypertension. He states he takes ‘water pills’ for his blood pressure and has been trying to exercise and lose weight but admits it is very hard when he travels. Demonstrates effective teamwork Prioritises and implements doctors instructions appropriately Scenario specific: Recalls indications, contraindications, and potential adverse effects of prescribed medications Implements the ‘5 rights’ of medication administration DOB: 19-07-XX Recent medical history: has been really ‘pushing’ himself lately and feels the ‘stress’ is starting to get to him. He has noticed this type of chest pain before but it usually goes away when he rests. He became worried when he began sweating and became short of breath. o o o o o o o o Securing the airway and assessing oxygen saturation. Starting oxygen at 4L/min. until SpO2 is >92% Administer Aspirin (chewed) Evaluate pain and scale it (0-10) Administer GTN (get history first and check for medications for erectile dysfunction) Monitor vital signs closely for hypotension every 2-5 minutes Morphine—only administered if not pain free after GTN (3 doses every 5 minutes) 12-lead ECG obtained and evaluated within 10 min. of admission to the ward/unit When ventricular tachycardia CPR 30:2 when unresponsive AED hooked up and shock delivered CPR 30:2 again AED shock delivered Adrenaline after 2nd shock (1mg IV) Recognises signs and symptoms of an adverse reaction Implements a focused respiratory assessment Recalls indications and contraindications for oxygen therapy Initiates relevant cardiac and respiratory monitoring Applies cardiac chest pain protocol according to DHB Acute Coronary Syndrome – Resources Equipment checklist Equipment to have in the room for this scenario: Proposed correct treatment (outline) Potential nursing problems Gloves on Acute pain related to cardiac ischaemia Identify patient name from ID band (DOB, hospital ID number) Defining characteristics: Verbal report Standard precautions equipment Stethoscope Obtain BP, pulse, RR, Temp, SpO2 Blood pressure cuff Attach ECG monitor leads SpO2 monitor and probe Give oxygen Thermometer Assess pain utilising pain scale Ineffective tissue perfusion, cardiopulmonary related to interruption of flow (arterial) Chest pain ECG monitor and leads Obtain 12-lead ECG if student has skills Dyspnoea Arrhythmias Changes in BP, resp. rate, AP Oxygen supply source Notify medical team (involve MDT) Oxygen delivery devices (nasal cannula, mask, and ambu bag) Administer medications per protocol MONA Monitor cardiovascular and respiratory state every 25 min. Activity intolerance related to imbalance between oxygen supply/demand Medication and fluids: Normal saline 1000ml infusing at 75ml/hour Aspirin 300mg in a bottle Number of participants: 1 student—recorder and calling SBAR ROLE GTN sublingual spray 0.4mg Morphine sulphate 10mg/10ml vial 1 student—doing primary assessment, giving medications 1 student—Vital signs and airway management 1 student—family member Documentation forms: Doctors instructions/DHB protocols Observation record, medication sheet, nursing notes Diagnostic equipment: AED machine with pads that stick Preparation of SimMan simulator: Location: cardiac ward hospital Dress SimMan in male clothing Sitting up on the bed (semi-fowlers) Secure ID band with patient name, DOB, and hospital ID number Defining characteristics: Verbal report of fatigue Electrocardiographic changes Exertional discomfort Acute Coronary Syndrome – Scenario SIM MAN settings Patient/manikin actions Initial state (0-2 minutes) Lung sounds: clear bilaterally Heart rate: 140/minute Peripheral pulses: strong Respiratory rate: 24/min. Vocal sounds: “It feels like an elephant sitting on my chest. The pain is ‘8!’” BP: 158/92 Rates pain as ‘8’ on scale of 1-10 SpO2: 94% Temp. 37 C Student interventions Student should do the following: Gloves on Introduce self, identify patient Obtain vital signs & assess pain Apply ECG leads Apply oxygen 4L/min. Obtain 12-lead ECG Give first dose NTG Administer Aspirin Role member providing cue: patient Administer 2nd dose of GTN & record Continue to monitor pain and vital signs continuously Check for responsiveness Call for help Commence CPR 30:2 Apply pads AED Press charge on AED State, “Shock advised, stand clear, shocking now” Deliver shock—check for responsiveness CPR again 30:2 Role member to provide cue: patient Note IV LINE Adrenaline 1mg every 2nd cycle Provide fluid bolus for ↓BP (500ml) Communicate therapeutically with patient when back to NSR Monitor and record vital signs (BP, AP, SpO2,) continuously Call ISBAR to physician and obtain orders Role member to provide cue: primary care provider ECG: 140/min. sinus tachycardia Vocal sounds: “The pain is ‘5’ out of 10 now.’ (after 1st dose of GTN) 2-5 minutes GTN trend: Vocal sounds: “The pain is getting worse” (after 2nd dose of GTN) BP: Not obtainable SpO2: not obtainable HR: 150/min. Resp. rate: Not breathing ECG: VTACH this frame after given 2nd GTN 7-10 minutes Heart rate: 90/min.. BP: 90/50 ECG: 90/min. Sinus rhythm BP: 90/7O, Resp: 28/min. Vocal sounds (with hypotension):—“I feel really light-headed and I see black spots in front of my eyes.” Vocal sounds: Eyes roll back and client groans. Patient becomes unconscious. Cue/prompt Cue: if student does not apply oxygen patient will say, “It feels like an elephant is sitting on my chest. Can you do something to help the pain?” “When will the doctor take a look at me? What do you think is happening here?” Cue: if nurse does not notify doctor when space allows, family member will ask, “What is going to happen next? Is he alright?” Cue (final orders): Transfer to CCU Call when blood results are available (Troponin-T, CK-MB, Myoglobin) Ventricular fibrillation and pulseless ventricular tachycardia are included in the Pulseless Arrest Algorithm. This is the most important algorithm in ACLS, and one that should be mastered. Both are shockable rhythms, in contrast to PEA and asystole, which fall on the right side of the algorithm. The ventricular fibrillation and pulseless ventricular tachycardia algorithm can be found here. The high resolution PDF for member download can be found here. Ventricular fibrillation is the most common rhythm experienced by patients who experience cardiac arrest. This is why so much emphasis in ACLS is placed upon learning and memorizing this rhythm and its treatment. Evidence reveals that rapid treatment of ventricular fibrillation using the ACLS pulseless arrest algorithm is the best way to achieve return of spontaneous circulation (ROSC). The following points are essential to remember when treating a patient using the Pulseless Arrest Algorithm for ventricular fibrillation and pulseless ventricular tachycardia: 1. Until the defibrillator is attached to the patient, high quality CPR should be performed. 2. Interruptions in chest compressions should be minimized. 3. Rapid use of the defibrillator is the key component of treatment for VF and VT. 4. Use of an AED may involve prolonged interruptions in chest compressions for analysis of the rhythm and administration of shock. Use a manual defibrillator if available. o Stacked shocks are no longer used. o CPR should be resumed for five cycles between each shock. Defibrillation and Shock We will be using AEDs as students have not been trained in defibrillation with paddles at this point. Paramedicine has advised use of AEDs due to lack of previous skill training with paddles. Vasopressors Definition: A vasopressor is a medication that produces constriction of the blood vessels, with a subsequent rise in blood pressure. In the treatment of ventricular fibrillation and pulseless ventricular tachycardia, the vasopressors used in the ACLS algorithm are Adrenaline and vasopressin. While Adrenaline is primarily used for its vasoconstrictor effects, vasopressin increases blood flow to the brain and heart, and has vasoconstrictor effects similar to those of Adrenaline. Anti-arrhythmic Amiodarone, lidocaine, and magnesium are the antiarrhythmic medications used in the pulseless arrest algorithm. More detailed information about these medications is located here. Rhythm checks should be limited to 10 seconds and should be performed after 5 cycles of CPR, to minimize interruptions in CPR.