Kingthorne Patient Participation Enhanced Service Report 2014 to
advertisement
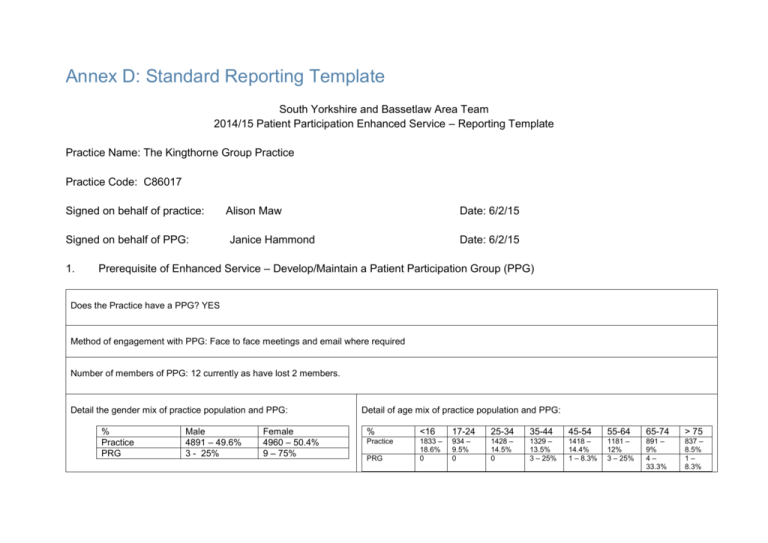
Annex D: Standard Reporting Template South Yorkshire and Bassetlaw Area Team 2014/15 Patient Participation Enhanced Service – Reporting Template Practice Name: The Kingthorne Group Practice Practice Code: C86017 Signed on behalf of practice: Signed on behalf of PPG: 1. Alison Maw Date: 6/2/15 Janice Hammond Date: 6/2/15 Prerequisite of Enhanced Service – Develop/Maintain a Patient Participation Group (PPG) Does the Practice have a PPG? YES Method of engagement with PPG: Face to face meetings and email where required Number of members of PPG: 12 currently as have lost 2 members. Detail the gender mix of practice population and PPG: % Practice PRG Male 4891 – 49.6% 3 - 25% Female 4960 – 50.4% 9 – 75% Detail of age mix of practice population and PPG: % <16 17-24 25-34 35-44 45-54 55-64 65-74 > 75 Practice 1833 – 18.6% 0 934 – 9.5% 0 1428 – 14.5% 0 1329 – 13.5% 3 – 25% 1418 – 14.4% 1 – 8.3% 1181 – 12% 3 – 25% 891 – 9% 4– 33.3% 837 – 8.5% 1– 8.3% PRG Detail the ethnic background of your practice population and PRG: Practice PRG Practice PRG British Irish 7512 – 76.3% 6 – 50% 34 – 3.5% 1– 8.3% White Gypsy or Irish traveller 5 – 0.5% Other white 853 – 8.7% 1 – 8.3% Asian/Asian British Bangladeshi Indian Pakistani 98 – 1.0% 225 – 2.3% 8 – 0.1% White &black Caribbean 21 – 0.2% Chinese 34 – 0.3% Mixed/ multiple ethnic groups White &black White African &Asian 14 – 0.1% 19 – 0.2% Other Asian 88 – 0.9% Other mixed 69 .07% Black/African/Caribbean/Black British African Caribbean Other Black 24 – 0.2% 13 – 0.1% 14 – 0.1% Other Any other 11 809 – .01% 8.2% 4– 33.3% Arab Describe steps taken to ensure that the PPG is representative of the practice population in terms of gender, age and ethnic background and other members of the practice population: The PRG is not representative of the Practice in any areas as we do not have different ethnic groups or a huge variety of ages. We have worked very hard to recruit additional members with GPs and the PRG targeting specific ages and ethnic groups. However there is a distinct lack of interest from patients. We have suggested having evening meetings for those who work but still we struggle to get a representative group. Are there any specific characteristics of your practice population which means that other groups should be included in the PPG? e.g. a large student population, significant number of jobseekers, large numbers of nursing homes, or a LGBT community? Yes – increasing number of Eastern Europeans shown by other white and any other which combined makes up 16.9% of the population. If you have answered yes, please outline measures taken to include those specific groups and whether those measures were successful: N/A Through our work with the nursing and residential homes we have engaged more with the careres and relatives of this vulnerable group. Although we have not managed to recruit someone from this area we do feel that we are gaining a perspective from the visits. As our number of Eastern European patients is growing we employed a Polish speaking receptionist. She has tried to engage with Polish patients to see if any of them would be willing to join the group but again without success. The PPG have themselves tried to recruit new members by attending the surgery and talking to patients whilst handing out surveys. We recruited 1 new member this way. They have targeted different ethnic groups and younger patients but again have not met with success. The GPs have also tried to target specific groups as they are aware of patients race and sexuality but again have had limited success as we have only recruited 1 patient this way. 2. Review of patient feedback Outline the sources of feedback that were reviewed during the year: Our own survey NHS Choices comments I Want Great Care comments Patient Complaints PPG Networking Meetings GP Patients Survey Practice Report Ipsos Mori Suggestion Box Significant Event Analysis CQC Feedback How frequently were these reviewed with the PRG? At each meeting where new information was provided. 3. Action plan priority areas and implementation Priority area 1 Description of priority area: Nursing and residential homes to have a dedicated Practice and preferably GP for each Practice across the central locality to ensure greater continuity of care within the homes. The PPG felt this was a worthwhile area as all had had experience of Care Homes and felt that anything that was done to improve the care of this vulnerable group was worthwhile. What actions were taken to address the priority? A GP and Practice Manager met with Practice leads across Central locality to discuss this and then allocated practices homes – we were allocated Amphion View and Victoria Lodge. We met with the Managers of the Homes to discuss the reasons behind the project and asked them to sign up to it. Both homes were more than happy to sign up to the project as they could see the benefits for both them and their patients. Our prescribing administrator then met with both homes to ensure that the service was working as smoothly as it could and to iron out any teething problems. Direct numbers into Administration were given to the homes to ensure ease of access to the Practice. The GPs are now doing ward rounds and the same GP is trying to do this each week where possible. We have also identified that staff at the homes need to be able to take temp, bp, pulse oximetry and urine analysis and are training staff as well as trying to assist them in getting funding for equipment. Result of actions and impact on patients and carers (including how publicised): The GPs have done Care Plans for all of the patients in the 2 homes and have started to get readings from them which is enabling a quicker assessment of patients. Therefore the patients are receiving better care and the staff feel more confident on what they are reporting in and the families appreciate the improved service. The weekly ward rounds are ensuring better communication between homes and the Practice and there are regular discussions with other Practices in the locality about the effectiveness of this. One area that has improved is that attendance at A&E for the homes has reduced due to the better communication channels. We have advertised this on our website, Facebook and a noticeboard in the waiting room. Priority area 2 Description of priority area: Invite patients aged over 45 who have not attended the surgery for 5 years or more to attend for an MOT. This was suggested by a member of the PPG and as it was discussed all the members saw the relevance as they could all think of friends or family who shy away from attending the surgery and so don’t have any checks. What actions were taken to address the priority? We searched the practice population for patients who were over 45 and had not attended the surgery in the last 5 years. There were 192 patients so we wrote to each of them inviting them to come in for a health check. Result of actions and impact on patients and carers (including how publicised): Seven patients rang to say thanks but did not feel they needed it and a further 6 came into the surgery for a check-up. Of the 6, 3 needed to follow up investigations. Other patients who had attended in the last 5 years also heard about this and asked for MOTs too. We have advertised this on our website, Facebook and a noticeboard in the waiting room. We also had an article about this published in the Doncaster Free Press. Priority area 3 Description of priority area: Members of the PPG alerted us to the fact that they don’t answer their phones if the number is withheld and as the Practice number is withheld we had trouble contacting some of them by phone. We also were advised that Polish people do not answer the phone if the number is withheld. We therefore decided that it would be useful to survey a broader number of patients to see if the consensus was that people would rather see our number when we call. As we discussed more, we thought we could also ask about other methods of communication and patients feelings about them so we decided to ask further questions around texting / emailing and skype. What actions were taken to address the priority? A survey was devised and then the PPG members came into the surgery to distribute the survey. It was also emailed out to patients for whom we have an email address. The results are attached. Survey results 2014.xls Result of actions and impact on patients and carers (including how publicised): The survey indicated that patients preferred to see the calling number so we contacted the phone company to change the system. Reception and admin now find patients answer the phone more often which means they are more efficient and patients are getting a better service. There seemed to be little appetite for skype but the response numbers were limited so we may look at this again. Texting was more popular so we have introduced a consent system and are starting to text regarding results, where appropriate. We also send text reminders for every appointment. Progress on previous years If you have participated in this scheme for more than one year, outline progress made on issues raised in the previous year(s): Comments in black are from last year’s report, comments in red are further updates on what has happened this year 2014 to 2015. Recruit 2 replacement nurses to assist in running the triage system. We have recruited 2 nurses, who are both very experienced in working in Primary Care. They have slotted into the team well and we can’t remember life without Pat and Wendy now. Our lead nurse, Julie, has now qualified as an Advanced Nurse Practitioner so has been promoted to this role and Wendy has taken over the role of lead nurse. We have managed to recruit one nurse to take some of Wendy’s old post but are advertising for a further nurse as Pat is going part time in February 2015. Cheryl has increased her hours so is now nearly full time and Louise now has permanent hours and is training to do triage. We feel to give patient’s the triage service they require we need at least another 20 hours of nurse time. Continue to offer a triage service by all clinicians until the nurses are fully trained and working in line with Practice protocols and procedures. The GPs found this a tough call during the months without trained nurses to help with the workload but feel that the on-going training of our nurses ensures that the patients get the best care we can provide. In fact this is being taken to the next level this year – read on to see why. Continue to monitor and fine tune the service to ensure that patients receive the appropriate care pathway dependent on their symptoms and urgency of need. This is an on-going piece of work that will probably never conclude as we are constantly looking at ways of improving the service. We don’t always get it right and some changes were less successful than others but we routinely monitor patient access to clinicians and look at ways to improve this. Develop our nurses to as high a standard as we are able, including considering training to Advanced Nurse Practitioner level. . Two of our nurses are now studying for exams that will ultimately enable them to work at Advanced Practitioner level and we also have another nurse who is hoping to do her Independent Nurse Prescribing course later this year. Julie is now qualified and Wendy is now able to consult on all areas of Contraception including fitting implants. Cheryl has started her prescribing course. Our new nurse, Carolyn, is doing her Asthma Diploma. We have also recruited 2 experienced full time Advanced Nurse Practitioners to further strengthen the team. Explain what triage is, what HCA vs Nurses do through literature in the Practice and on the website. Display notice boards were put up both in the main surgery and the branch surgery differentiating between the 2 roles of nurses and HCAs in the Practice. There was also information about the use of triage. Sadly one thing we would like to do is list on the automated booking system information about what the various health care professionals can do but to date our software provider has not enabled this to happen. As there is more pressure on Practices to use IT we hope that there will be further developments in this area. We are still working with the software developer but have not yet found a solution. Our website also carries information about appointment types and where patients should book in to get the best care. Advise patients again that not all GPs work full time so patients may not be able to see their preferred GP as soon as they would like. We have added notices in the waiting room about this and are also in the process of updating our Practice Leaflet so have added a comment regarding this. We are awaiting this to be added to the website. We are in the process of adding a lot of additional information to our website. Have news flashes on the website / Facebook / twitter when we have a turn of events that leads to fewer appointments than normal. We have tried to remember to do this but unfortunately have not always done so. Hopefully we will get better at this as we are all quite new to Facebook and twitter! We are still not great at this but are trying! 4. PPG Sign Off Report signed off by PPG: YES/NO Date of sign off: How has the practice engaged with the PPG: How has the practice made efforts to engage with seldom heard groups in the practice population? Through our work with the nursing and residential homes we have engaged more with the careres and relatives of this vulnerable group. Although we have not managed to recruit someone from this area we do feel that we are gaining a perspective from the visits. As our number of Eastern European patients is growing we employed a Polish speaking receptionist. She has tried to engage with Polish patients to see if any of them would be willing to join the group but again without success. The PPG have themselves tried to recruit new members by attending the surgery and talking to patients whilst handing out surveys. We recruited 1 new member this way. They have targeted different ethnic groups and younger patients but again have not met with success. The GPs have also tried to target specific groups as they are aware of patients race and sexuality but again have had limited success as we have only recruited 1 patient this way. The Practice Manager is looking at attending a seminar run by Healthdeafinitions to see if there are better ways to liaise with our deaf patients as well as buying portable induction loops for both surgeries as ours are no longer working. Has the practice received patient and carer feedback from a variety of sources? NHS Choices I Want Great Care – signed up and receive feedback Practice Survey – Ipsos Mori Our own survey CQC – visit where they spoke to patients and asked for cards to be filled in prior to the visit. Suggestion Box Complaints Significant Event Analysis Was the PPG involved in the agreement of priority areas and the resulting action plan? The PPG were asked what their areas of priority were – initially no one had any but through discussion around the Practice they came up with 2 of the areas themselves. When we mentioned the Care Home idea they all thought this was appropriate. They have been involved with each area and have discussed, amended and agreed the action plans. How has the service offered to patients and carers improved as a result of the implementation of the action plan? Nursing Homes – improvements in continuity of care, communication and more efficient use of resources have led to more timely interventions and increased confidence through the closer relationship. Telephones – we are able to contact patients more easily and in a timely manner so improved communication and therefore patient satisfaction. Disengaged patients – by contacting patients over 45 that we have not seen for more than 5 years we have managed to check 6 patients who may not have come to the surgery otherwise – 3 of whom required further investigations. Hopefully through our advertising of this, we may have reached a wider audience and may have encouraged more patients to attend the Practice. Do you have any other comments about the PPG or practice in relation to this area of work? The PPG and the Practice have worked hard as a team to achieve the results we have. The PPG feel that they are listened to by the Practice and so feel they can freely express their views. The Practice also come to them with queries when they are looking at services in the Practice so it is a reciprocal arrangement that works well. The PPPG is well led by the Chairperson who has done networking with other PPGs to see what else they can achieve. We will continue to strive the make the group more representative of the practice population but acknowledge that this may be an unattainable outcome.