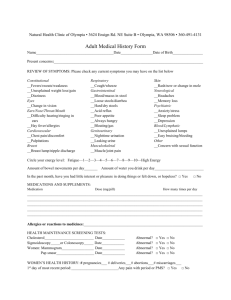
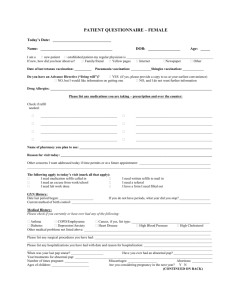
New Patient History Form
advertisement

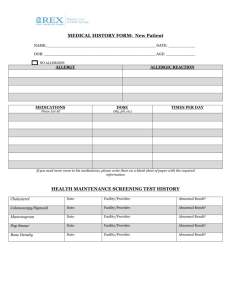
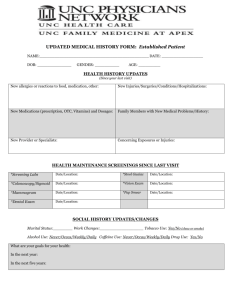
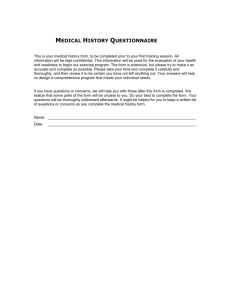
MEDICAL HISTORY FORM: New Patient NAME:_____________________________________________ DATE: _________________ DOB: ______________________________________________ AGE: __________________ NO ALLERGIES ALLERGY MEDICATIONS Please List All ALLERGIC REACTION DOSE (Mg, pill, etc.) TIMES PER DAY If you need more room to list medications, please write them on a blank sheet of paper with the required information HEALTH MAINTENANCE SCREENING TEST HISTORY Cholesterol Date: Facility/Provider: Abnormal Result? Colonoscopy/Sigmoid Date: Facility/Provider: Abnormal Result? Mammogram Date: Facility/Provider: Abnormal Result? Pap Smear Date: Facility/Provider: Abnormal Result? Bone Density Date: Facility/Provider: Abnormal Result? VACCINES HISTORY Last Tetanus Booster or TdaP: Last Pnuemovax: Last Flu Vaccine: Last Zoster: PERSONAL MEDICAL HISTORY DISEASE/CONDITION CURRENT PAST COMMENTS Alcoholism/Drug Abuse Asthma Cancer (type) Depression/Anxiety/Bipolar/Suicidal Diabetes (type) Emphysema (COPD) Heart Disease High Blood Pressure (Hypertension) High Cholesterol Hypothyroidism/Thyroid Disease Renal (kidney) Disease Migraine Headaches Stroke Other: Other: Other: SURGERIES List what type of surgery (specify left/right), date of surgery, and location __________________________________________________________________ __________________________________________________________________ __________________________________________________________________ __________________________________________________________________ __________________________________________________________________ WOMEN’S HEALTH HISTORY Total Number of Pregnancies: ___________ Number of Live Births: _____________ Date of Last Menstrual Cycle: ____________ Age of First Menstruation: ___________ Age of Menopause: ___________________ Pregnancy Complications: __________________________________________________________________ __________________________________________________________________ FAMILY MEDICAL HISTORY Other Other Other Migraines Thyroid Disease Stroke Kidney Disease High Blood Pressure High Cholesterol Heart Disease Early Death Diabetes Depression/Anxiety Bipolar/Suicidal Emphysema (COPD) Cancer (type) Asthma Alcohol/Drug Abuse No Significant Family History is Known Mother Father Sibling Child MGM MGF PGM PGF SOCIAL HISTORY Occupation (or prior occupation): ___________________ retired/unemployed/LOA/disabled Employer: ____________________ Years of Education or Highest Degree: ________ Marital Status (circle): Single / Partner / Married / Divorced / Widowed / Other Who Lives at Home with You? _____________________________________________ OTHER HEALTH ISSUES Tobacco Use Smoke Cigarettes? Never No Yes (If you never smoked, please move to Alcohol Use) Quit date: _________ How many years: ______ Alcohol Use Do you drink alcohol? Yes #of drinks/week: ______ No Beer Wine Liquor How many packs did you smoke a day: ________ Drug Use Do you use marijuana or recreational drugs? Yes No Current smoker: Packs/day ____ #of Years ____ Have you ever used needles to inject drugs? Yes No Other Tobacco: Pipe Cigar Have you ever taken someone else’s drugs? Yes No Snuff Chew Sexual Activity Sexually involved currently? Yes Sexual partner(s) is/are/have been: Male Diet How would you rate your diet? Good Fair Poor No Female Birth control method: None Condom Condom Pill/Ring/Patch/Inj/IUD Vasectomy Exercise Do you exercise regularly? Yes No What kind of exercise? ____________________ ____________________________________ ____________________________________ How long (mins) _______ How often ________ Would you like advice on your diet? Yes No Safety Do you use a bike helmet? Do you use seatbelts consistently? Working smoke detector in home? Yes Yes Yes No No No If you have guns at home, are they locked up? Yes No Is violence at home a concern for you? No Yes Have you completed an Advance Directive for Health Care (ADHC), Living Will, or Physical Orders for Life Sustaining Therapy (POLST)? Yes No OTHER PROVIDERS/SPECIALISTS SPECIALIST Cardiology GI GYN Neurology Pulmonary Other: Other: NAME LAST VISIT REVIEW OF SYSTEMS SKIN Rash Sores Changes with a Mole Itching/Dryness Hair and Nail Changes EARS Loss/decrease of hearing Drainage from ears Ringing Earache EYES Blurry Vision Drainage from eyes Pain Vision loss/changes Flashing lights/Dots HEART Heart Murmur/Palpitations Chest pains/discomfort/ Tightness Swelling Leg pain when walking SKELETON Pain in joints Stiffness GASTRO Change in appetite Problems swallowing Abdominal Wheezing Nausea/Diarrhea Change in bowel habits Rectal Bleeding Constipation URINARY Frequency Urgency Burning or Pain Blood in Urine Incontinence Change in Urinary strength NEUROLOGIC Dizziness Fainting Seizures Weakness Numbness Tingling Tremor ENDOCRINE Heat/Cold Intolerance Sweating Thirst Change in appetite HEAD Headaches/Migraines Neck Pain Head Injury PSYCHIATRIC Nervousness Stress Depression Memory Loss BREAST Lump(s) Pain Discharge Tenderness Color Changes VAGINAL Discharge Hot Flashes Change in Periods Itching or Dryness Pain with Sex Loss of Sex Drive Lesions/Sores PROSTATE Lump(s) Pain/Pain with Sex Lesions/Sores Loss of Sex Drive Hernia LUNGS Cough Difficulty/Painful breathing Coughing up blood Wheezing Swollen joints Back Pain