Sunset Country FHT QIP Narrative
advertisement
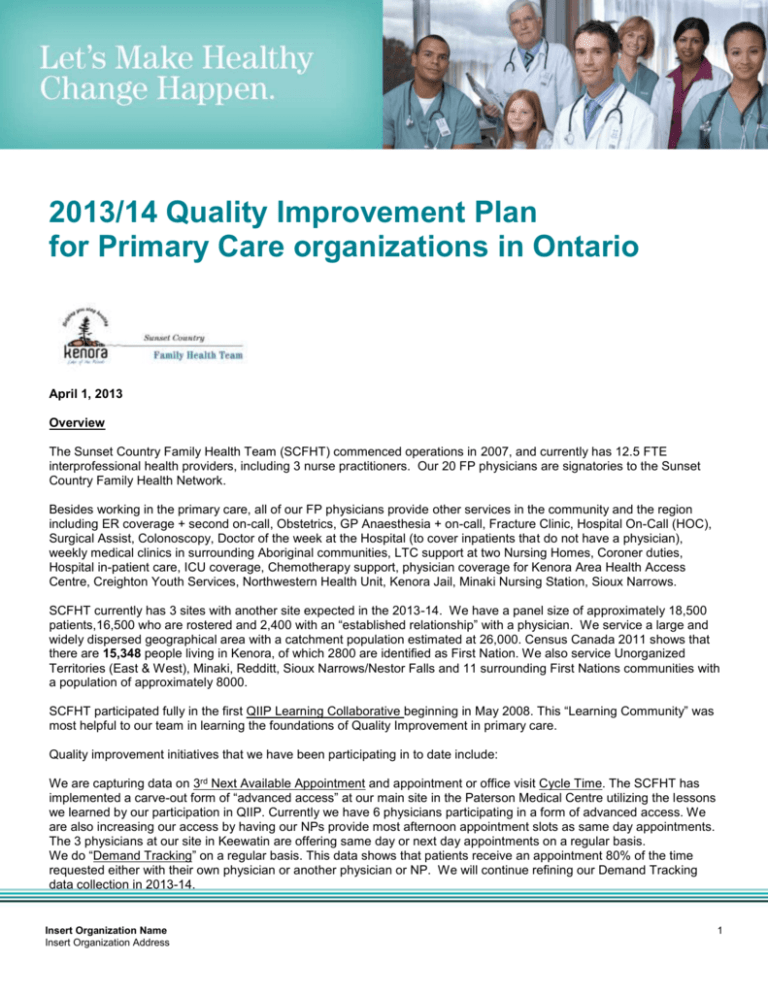
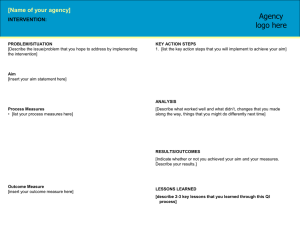
2013/14 Quality Improvement Plan for Primary Care organizations in Ontario April 1, 2013 Overview The Sunset Country Family Health Team (SCFHT) commenced operations in 2007, and currently has 12.5 FTE interprofessional health providers, including 3 nurse practitioners. Our 20 FP physicians are signatories to the Sunset Country Family Health Network. Besides working in the primary care, all of our FP physicians provide other services in the community and the region including ER coverage + second on-call, Obstetrics, GP Anaesthesia + on-call, Fracture Clinic, Hospital On-Call (HOC), Surgical Assist, Colonoscopy, Doctor of the week at the Hospital (to cover inpatients that do not have a physician), weekly medical clinics in surrounding Aboriginal communities, LTC support at two Nursing Homes, Coroner duties, Hospital in-patient care, ICU coverage, Chemotherapy support, physician coverage for Kenora Area Health Access Centre, Creighton Youth Services, Northwestern Health Unit, Kenora Jail, Minaki Nursing Station, Sioux Narrows. SCFHT currently has 3 sites with another site expected in the 2013-14. We have a panel size of approximately 18,500 patients,16,500 who are rostered and 2,400 with an “established relationship” with a physician. We service a large and widely dispersed geographical area with a catchment population estimated at 26,000. Census Canada 2011 shows that there are 15,348 people living in Kenora, of which 2800 are identified as First Nation. We also service Unorganized Territories (East & West), Minaki, Redditt, Sioux Narrows/Nestor Falls and 11 surrounding First Nations communities with a population of approximately 8000. SCFHT participated fully in the first QIIP Learning Collaborative beginning in May 2008. This “Learning Community” was most helpful to our team in learning the foundations of Quality Improvement in primary care. Quality improvement initiatives that we have been participating in to date include: We are capturing data on 3rd Next Available Appointment and appointment or office visit Cycle Time. The SCFHT has implemented a carve-out form of “advanced access” at our main site in the Paterson Medical Centre utilizing the lessons we learned by our participation in QIIP. Currently we have 6 physicians participating in a form of advanced access. We are also increasing our access by having our NPs provide most afternoon appointment slots as same day appointments. The 3 physicians at our site in Keewatin are offering same day or next day appointments on a regular basis. We do “Demand Tracking” on a regular basis. This data shows that patients receive an appointment 80% of the time requested either with their own physician or another physician or NP. We will continue refining our Demand Tracking data collection in 2013-14. Insert Organization Name Insert Organization Address 1 Office Practice Redesign (OPR) is a multidisciplinary group that has a number of initiatives underway to increase efficiency and enhance access in our largest site at the Paterson Medical Centre. OPR is currently working on 16 projects including forms flow, dictation/transcription(Dragon Medical) improvements, EMR templates, Primary Care Groups, morning “huddles”, prescriptions/refills, internal communication processes, no shows, office time (physician scheduling for time in office), access, HMPs, appointment notifications, patient flow, locums, QIP (as mandated by MOHLTC) and staff efficiency. Primary Care Groups – At the Paterson Medical Centre site we have initiated a trial of primary care groups. 3 groups of physicians + a NP who will have support staff (eg. Appointment Bookers) dedicated to scheduling appointments in a more timely basis. There are plans to also develop a triage system (phone staff to RPN to RN/NP) in order to schedule appointments in a timely manner and with the most appropriate provider. No Shows - In 2012 we had approximately 3200 booked appointments where the patient failed to show up for the appointment (8% of our total appointment bookings). We are displaying this information publicly in the clinic and in ER, in order to increase the awareness of implications of “no shows”. We are also summarizing this information for each physician and clinic staff to review how they can reduce the number of no show appointments. SCFHT is reviewing the ”no show” rates for all IHPs and has drafted a new procedure/policy for booking appointments for referrals to SCFHT providers/programs, reminder phone calls for booked appointments, and consistent messaging of reminder phone calls. If approved, our new Administrative Assistant will work directly with our IHPs to better coordinate referrals, initial and follow-up appointments. We also have a Diabetes Working Group and an Integrated Cancer Screening Group meeting on a regular basis. Focus In 2013/14 the SCFHT will focus on organizational-wide (at all 3 sites) improvements in: 1. Timely access to primary care, when needed by improving data collection at the PMC site and initiating data collection at our other 2 sites. This will include training staff at all 3 sites in consistent data collection. We will also collect information via survey regarding patients perception of receiving a visit or appointment on the same day or when needed. 2. Timely access to primary care appointments post discharge. We will strive to maintain the current level of 90% by improving on receiving discharge information from both the hospital and CCAC in a more reliable and consistent manner. We also plan to develop a referral and intake process (by May 2013) for all asthma patients (as part of our new PCAP Program*) discharged from ER and inpatient discharges. We will also improve our baseline data by 50% for our Post Discharge Medication Follow-up Program and expand eligibility criteria for patients in the program. 3. Receiving and utilizing feedback regarding patient/client experience with the SCFHT. We plan to update our existing survey to include physicians and NPs as well as initiate the survey at our other 2 sites. Our goal for 2013-14 is for 10% of patients seen September 2013 to March 2014 to complete a survey. *PCAP – Primary Care Asthma Program Use of the Electronic Medical Record (EMR) The functionality of our EMR is limited in meaningful data extraction and accuracy. While the SCFHT participated in Wave 1 of QIIP (in May 2008), we have since struggled with implementing many of the “lessons learned” and Quality Improvement Initiatives. Basically we have struggled with the lack of expertise and resources to utilize the limited functionality of our EMR. We continue to struggle with standardization of data, data extraction and analysis, enhancing data and information management. Other than on a very limited basis, we are unable to extract and analyze data to create reports that would help inform managers and clinicians in decision making processes. We recognize the need for good data to support clinical staff (including physicians and IHPs) with clinical process change and improvement. We continue to create and update HMPs (Health Maintenance Plans) to include ACR, PAP, Mammogram, FOBT. We have also created “Registries” for Hypertension Management, INR, Smoking Cessation, COPD and soon Diabetes Programs. New CDM “flowsheets” for Diabetes Management and INR have been developed. We will continue to work on processes to enable improved data accuracy and standardization of data input by our team resulting in enhanced retrievability of data to support quality improvement. Insert Organization Name Insert Organization Address 2 Integration and continuity of care Sunset Country FHT is a member of the Kenora Area Continuum of Care Coalition. We will continue meeting with this group of community health organizations and other community partners to explore service integration, collaboration and quality improvement opportunities. Practice/community profile Our Mission Statement reads “We, a community multidisciplinary team, provide and advocate for compassionate, collaborative, coordinated primary health care for our patients”. Two of our values state – “We will provide quality care” and “We will work in a culture of improvement”. An Interprofessional Best Practice Team has been formed. The intent of this team is to look at scope of practice, competencies and interests of team members to have the most appropriate provider(s) providing timely quality client care. It is intended as a forum to communicate, network and collaborate to exchange information related to evidencebased client-centered primary care practice and programming. We intend to post our QIP on the SCFHT website. We will continue to develop and nurture relationships with our community partners. Chronic disease management and prevention Registries for INR, Hypertension Management, Smoking Cessation, COPD and soon Diabetes have been developed. We will utilize these registries to monitor and enhance outcomes and quality improvement in these programs. We developed and implemented HMPs (Health Maintenance Plans) in our EMR for ACR, PAP, FOBT and Mammograms. The SCFHT Diabetes Program is working this year to further develop and implement a collaborative patient-centred approach through integration of existing family health team IHPs with Diabetes Education Services (formerly a DEC NDHN program). Through collaborative practice it is expected that patients of SCFHT living with or at risk for diabetes will receive consistent coordinated quality care based on best standards of practice. Accountability management Our OPR, Diabetes and ICS teams, along with the Interprofessional Best Practice Team will continue to advance our quality improvement initiatives in 2013-14. The SCFHT Board will be engaged directly in the advancement of our organizational wide Quality Improvement Plan. Challenges and risks In summary, we have been unable to move forward in our efforts to use data to guide clinical decision making, and develop and implement patient-centered programs and other improvement activities. We anticipate having continuing difficulties (due to lack data accuracy and management, standardization, and retrievability of meaningful data) in implementing and enhancing quality improvement initiatives organization wide. This document is intended to provide primary care organizations with guidance as to how they can develop a quality improvement plan. While much effort and care has gone into preparing this document, this document should not be relied on as legal advice and organizations should consult with their legal, governance and other relevant advisors as appropriate in preparing their quality improvement plans. Furthermore, organizations are free to design their own public quality improvement plans using alternative formats and contents, provided that they submit a version of their quality improvement plan to HQO (if required) in the format described herein. Insert Organization Name Insert Organization Address 3 Our Improvement Targets and Initiatives See attached Template Sign-off (see attached) I have reviewed and approved our organization’s Quality Improvement Plan Dr. S. Pedersen Dr. C. Hammett Randy Belair Board Chair Clinician Lead Executive Director/Admin. Lead Insert Organization Name Insert Organization Address 4