To: - Johns Hopkins Bloomberg School of Public Health
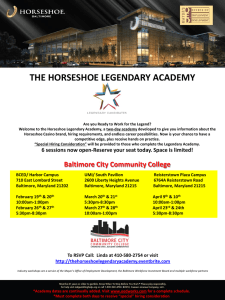
advertisement

Department of Mental Health Symposium Agenda 9:00-9:10 9:10-9:30 9:30-10:30 Bill Eaton Phil Leaf Panel Chair: Josh Sharfstein Secretary, Maryland Department of Health and Mental Hygiene 10:30-10:45 10:45-11:00 11:00-12:00 12:00-12:30 12:30-1:15 1:15-1:45 Audience Q & A Break 7 Breakout Groups Groups report back Lunch Richard Frank Harvard Medical School Department of Health Care Policy Panel Chair: Charles Milligan Deputy Secretary for Health Care Financing, State of Maryland 1:45-2:45 2:45-3:00 3:00-3:15 3:15-4:15 4:15-4:45 4:45-5:00 5:00-6:30 Audience Q & A Break 8 Breakout Groups Groups Report Back Phil Leaf or Bill Eaton Wine and cheese reception Welcome and opening comments Introduction to the Public Health Approach Improving Behavioral Health: the Public Health Approach Amanda Harris Chief Operating Officer, Pathways to Housing Dave Oslin Associate Chief of Staff for Behavioral Health, Philadelphia Veterans Affairs Medical Center Ron Manderscheid Executive Director, National Association of County Behavioral & Developmental Disability Directors Carl Bell President, Community Mental Health Council, Chicago Chacku Mathai Associate Executive Director, New York Association of Psychiatric Rehabilitation Services E2133, E2527, W2303, W2205, W2207, two in Feinstone What do ACA and Parity Act mean for the future of mental health care in the US? Mental Health Care reform 101 Financing Mechanisms for Behavioral Health Care Reform: Opportunities and Challenges Carolyn Quattrocki Executive Director, Governor’s Office of Health Care Reform Howard Goldman Editor, Psychiatric Services Barbara Leadholm Office of Behavioral Health, MassHealth Rita Vandivoort, Senior Public Analyst, HRSA Anna Marsh, Deputy Director, CMHS E2133,W2017,E2527,W2300,W2205,W2207,Feinstone(2) Closing comments 624 N. Broadway Baltimore, Maryland 21205 (410) 955-3910 Department of Mental Health Morning Breakout Sessions: The Public Health Approach: Opportunities and Challenges Group 1 Group 2 Group 3 Group 4 Covering the whole population How to serve those with dual diagnoses How to organize services for children and adolescents Process and outcomes of performance management Room W2207 Lisa Colpe (Chair) Chet Schmidt Alan Levitt Alexander Cowell Elspeth Ritchie Carol Payne Josh Sharfstein Charles Milligan Room E2527 Eric Strain (Chair) Jackie Duval-Harvey Frances Randolph Susan Cycyk Jeffrey Buck Tami Mark Robert Findling Carolyn Quattrocki Amanda Harris Room W2205 Jane Plapinger (Chair) Robert Heinssen Sarah Duffy Kirsten Beronio Thomas Bornemann William Narrow Tom Croghan Richard Frank Pierre Alexandre Note taker: Anna Flynn Note taker: Lareina LaFlair Room W2303 Larry Wissow (Chair) David Dean, Jr Anna Marsh Sandra Spencer Heather Ringeisen Judith Teich Dave Oslin Howard Goldman Mariana Salamoun Al Zachik Note taker: Lindsey Grimm Note taker: Ramin Mojtabai Group 5 Group 6 Group 7 Deciding which programs are successful Feinstone Hall Sharon Larson (Chair) Peggy Swarbrick Chacku Mathai Harold Perl Colleen Barry Ron Mandersheid Barbara Leadholm Rita Landgraf Gerard Gallucci Laysha Ostrow The place of primary care Reducing disparities Feinstone Hall Joyce West (Chair) Jill Rogers Joseph Gallo Bernadette Cullen Anita Everett Charlotte Mullican Kamala Allen Carl Bell Rita Vandivort-Warren Room E2133 Bradley Karlin (Chair) Kevin Keegan Jim Lafferty Marie Mann Alexander Ross John O'Brien Lisa Townsend Chacku Mathai Note taker: Sarah Racz Note taker: William Eaton Note taker: Emma McGinty 624 N. Broadway Baltimore, Maryland 21205 (410) 955-3910 Department of Mental Health Afternoon Breakout Sessions: Financing Mechanisms for Behavioral Health Care Reform: Opportunities and Challenges Group 1 Group 2 Group 3 Organizing finance mechanisms for children and adolescents Room W2207 Chet Schmidt (Chair) Marie Mann Heather Ringeisen Judith Teich David Dean, Jr Sandra Spencer Richard Frank Integrating funding streams for dual diagnoses Room E2527 Chacku Mathai (Chair) Jeffrey Buck Eric Strain Larry Wissow Charles Milligan Financing prevention and identifying resulting cost savings Room W2303 Bernadette Cullen (Chair) Kevin Keegan Joseph Gallo Alan Levitt Jane Plapinger Susan Cycyk Jim Lafferty Carolyn Quattrocki Note taker: Lindsey Grimm Note taker: Lareina LaFlair Note taker: Anna Flynn Group 5 Group 6 Financial implications of electronic health records Financing ancillary services and providers (e.g., case managers, psychiatric nurses) Feinstone Hall Frances Randolph (Chair) Charlotte Mullican Jackie Duval-Harvey Jill Rogers Dave Oslin Rita Vandivort-Warren Robert Heinssen Pay for performance Note taker: William Eaton Note taker: Christina Pate Feinstone Hall William Narrow (Chair) Sharon Larson Anna Marsh Lisa Townsend Robert Findling Lisa Colpe Barbara Leadholm Note taker: Michelle Colder-Carras 624 N. Broadway Baltimore, Maryland 21205 (410) 955-3910 Group 7 Room E2133 Thomas Bornemann (Chair) Tom Croghan Kamala Allen Peggy Swarbrick Gerard Gallucci Amanda Harris Group 4 Financing non-medical services Room W2205 Anita Everett (Chair) Joyce West Bradley Karlin Tami Mark Kirsten Beronio Carol Payne Alexander Cowell Rita Landgraf Laysha Ostrow Note taker: Sarah Racz Group 8 Risk adjustment and risk sharing arrangements in insurance market Room W2017 John O'Brien (Chair) Sarah Duffy Alexander Ross Harold Perl Carl Bell Note taker: Ramin Mojtabai Department of Mental Health Charges for Morning Breakout Sessions Morning Group 1: Covering the whole population 1. What are the priority groups not currently covered and who would be left out after the implementation of the healthcare reform? 2. What would be the impact of Supreme Court decision regarding Medicaid expansion of ACA on coverage of near-poor population? 3. What would be the impact of implementation of ACA on mental health care disparities? Morning Group 2: How to serve those with dual diagnoses 1. What are the best models for mental health care and substance use disorder integration/coordination? 2. What will be the impact of the ACA on the coordination of substance abuse and mental health care services? 3. How can we best define and measure outcomes in dual diagnosis services? Morning Group 3: How to organize services for children and adolescents 1. What is the best setting for administration of mental health services to children and adolescents? 2. What place will the schools have in provision mental healthcare of children and adolescents after implementation of the health care reform? 3. What would be the impact of the ACA on coordination of mental health services in primary care and specialty mental health services? Morning Group 4: Process and outcomes of performance management 1. What measures do we need to use for performance measurement? 624 N. Broadway Baltimore, Maryland 21205 (410) 955-3910 Department of Mental Health 2. The "when" and the "how" of measuring performance management. 3. What would be the impact of the ACA on measurement of process and outcome in performance management? Morning Group 5: Deciding which programs are successful 1. How should we define success? 2. How should we measure success? 3. How should we incentivize successful programs under the ACA? Morning Group 6: The place of primary care 1. What would be the role of medical homes in management of mental health conditions? 2. How do we get primary care to take on new roles for management of substance abuse and mental disorders? 3. What is the best model for coordinating mental health services with medical services? Morning Group 7: Reducing disparities 1. Would ACA reduce the disparities in access to mental health care? 2. Would ACA reduce disparities in quality of mental health care? 3. How can services be optimized to reduce disparities in access and quality? 624 N. Broadway Baltimore, Maryland 21205 (410) 955-3910 Department of Mental Health Charges for Afternoon Breakout Sessions Afternoon Group 1: Organizing finance mechanisms for children and adolescents 1. How would financing mental health care for children and adolescents change under the ACA? 2. What are the financial implications of the alternative models of delivery of children mental health services? 3. How can mental health and substance abuse prevention programs be optimally incorporated in child mental health services? Afternoon Group 2: Integrating funding streams for dual diagnoses 1. What are the challenges in integrating funding streams for dual diagnoses services after health care reform? 2. What are the implications of changes in block grants after the health care reform? 3. What would be the challenges in challenges staffing of integrated dual diagnosis services? Afternoon Group 3: Financing prevention and identifying resulting cost savings 1. How should we measure cost savings associated with prevention programs? 2. How would prevention services be funded under the ACA? 3. Can prevention services be included as part of the essential package of mental health services? Afternoon Group 4: Financing non-medical services 1. How would housing services be funded under the ACA? 2. How would employment services be funder under the ACA? 624 N. Broadway Baltimore, Maryland 21205 (410) 955-3910 Department of Mental Health 3. What are the essential non-medical services left out after the implementation of the ACA? Afternoon Group 5: Financial implications of electronic health records (EHR) 1. How much would EHR save health care costs? 2. How can EHR be best designed to safeguard patients' privacy? 3. How can EHR be best designed to improve quality of mental health services? Afternoon Group 6: Financing ancillary services and providers (e.g., case managers, psychiatric nurses) 1. How would the financing of ancilliary services change under ACA? 2. What would be the staffing needs for ancillary services and providers? 3. What are the financial implications of new technologies in the delivery of mental health services (e.g., tele-psychiatry)? Afternoon Group 7: Pay for performance 1. Have we learned any lessons from prior experience with pay for performance in delivery of physical healthcare that is transferable to mental healthcare? 2. What have we learned from prior experience with pay for performance in delivery of mental healthcare in the US and other countries? 3. How can we make gains in targeted outcomes of pay for performance generalizable to a broader set of mental health outcomes? Afternoon Group 8: Risk adjustment and risk sharing arrangements in insurance market 1. Would risk adjustment and risk sharing arrangements be successful in reducing adverse selection for the mentally ill in insurance exchanges? 624 N. Broadway Baltimore, Maryland 21205 (410) 955-3910 Department of Mental Health 2. What are the information needs for risk adjustment? 3. What are the implications of failure of risk adjustment and risk sharing arrangements in insurance markets for financing of mental healthcare? 4. Are risk adjustments and risk sharing arrangements different among psychiatric patients and patients with other chronic health conditions? 624 N. Broadway Baltimore, Maryland 21205 (410) 955-3910 Department of Mental Health Panelist and Presenter Biographies Carl Bell, M.D., F.A.P.A., F.A.C.P. Richard Frank, PhD Howard Goldman, MD, PhD Barbara Leadholm, MSN, MBA Philip Leaf, PhD Carl Bell is the CEO and President of the of the Community Mental Health Council, Inc, a large not-for-profit community mental health centers in the U.S. He is also Director of the Institute for Juvenile Research and a clinical professor of psychiatry and public health at the University of Illinois School of Medicine. After graduating from the University of Illinois in 1967 with a Bachelor’s of Science Degree in Biology, he went on to Meharry Medical College where he graduated with an M.D. His postgraduate training in psychiatry was at the Illinois State Psychiatric Institute in Chicago. Richard G. Frank, PhD, is the Margaret T. Morris Professor of Health Economics in the Department of Health Care Policy at Harvard Medical School. He is also a research associate with the National Bureau of Economic Research. Dr. Frank received a BA in economics from Bard College and a PhD in economics from Boston University. Howard H. Goldman is Professor of Psychiatry at the University of Maryland School of Medicine. He is a mental health services and policy researcher, who is the author of 300 publications in the professional literature. Dr. Goldman is the editor of Psychiatric Services. He served as the Senior Scientific Editor of the Surgeon General's Report on Mental Health for which he was awarded the Surgeon General’s Medallion. Dr. Goldman received his M.D. from Harvard University and Ph.D. in social policy research from Brandeis University. Barbara Leadholm has served as Commissioner of the Department of Mental Health since 2007. Under her leadership, the agency has made significant strides in implementing the Community First initiative as part of its continuum of quality services for people with serious mental illness. She earned her Master of Science in Psychiatric Nursing from Boston College and her Master of Business Administration from Boston University. Dr. Leaf is a professor in the Department of Mental Health at the Johns Hopkins Bloomberg School of Public Health and director of the Center for Prevention of Youth Violence. His 624 N. Broadway Baltimore, Maryland 21205 (410) 955-3910 Department of Mental Health Ron Manderscheid, PhD Anna Marsh, PhD Chacku Mathai, CPRP work focuses on preventing youth violence and promoting positive youth development. Dr. Leaf is also senior associate direct of the Johns Hopkins Urban Health Institute. He received his PhD from the University of Wisconsin. Ron Manderscheid, serves as the Executive Director of the National Association of County Behavioral Health and Developmental Disability Directors. The Association represents county and local authorities in Washington, D.C., and provides a national program of technical assistance and support. Concurrently, he is Adjunct Professor at the Department of Mental Health, Bloomberg School of Public Health, Johns Hopkins University, and President of ACMHA—The College for Behavioral Health Leadership. Dr. Manderscheid serves on the boards of the Employee Assistance Research Foundation, the Danya Institute, the FrameWorks Institute, the Council on Quality and Leadership, and the International Credentialing and Reciprocity Consortium. He also serves as the Co-Chair of the Coalition for Whole Health. Dr .Mandersheid received his PhD from University of Maryland. Dr. Anna Marsh is Deputy Director of the Center for Mental Health Services (CMHS) in the Substance Abuse and Mental Health Services Administration (SAMHSA) of the U.S. Department of Health and Human Service (DHHS). She has worked for SAMHSA and its predecessor agency, the Alcohol, Drug Abuse, and Mental Health Administration, since 1985. Dr. Marsh received her Ph.D. in Psychology from Yale University, where she was a Fellow at the Bush Center in Child Development and Social Policy. She received her B.A. in Psychology from George Washington University. Chacku Mathai has over twenty-five years experience in mental health and community based services in a wide variety of roles including peer advocate, peer support meeting facilitator, selfhelp educator, community organizer and educator, community residence manager, psychiatric rehabilitation practitioner, trainer and program administrator. He currently serves as the Associate Executive Director for the New York Association of Psychiatric Rehabilitation Services and is an implementation partner for the New York State Center of Excellence for the Integration of Care (CEIC) and the SAMHSA Recovery to 624 N. Broadway Baltimore, Maryland 21205 (410) 955-3910 Department of Mental Health Practice Resource Center for Mental Health Professionals. Charles Milligan, JD, MPH David Oslin, MD Amanda Harris, MPH, LGSW Joshua Sharfstein, MD Charles Milligan was appointed deputy secretary for health care financing at the Maryland Department of Health and Mental Hygiene in March 2011. In this role, he is responsible for the state’s Medicaid program. Previously Mr. Milligan was executive director of The Hilltop Institute at the University of Maryland, Baltimore County (UMBC), which is a public sector consulting and research organization that provides services to the Maryland Medicaid program, other state and local agencies, the federal government, and private foundations. Earlier in his career he was Medicaid and SCHIP director for the state of New Mexico. Mr. Milligan holds a J.D. from Harvard Law School, an M.P.H. from the University of California at Berkeley, and a B.B.A. from the University of Notre Dame. David Oslin is an Associate Professor of Psychiatry at the Philadelphia Veterans Affairs Medical Center and the University of Pennsylvania Medical Center. Dr. Oslin is the Director of the VISN 4 Mental Illness, Research, Education, and Clinical Center (MIRECC) and the Associate Chief of Staff for Behavioral Health at the Philadelphia VAMC. The MIRECC and BHL support research on comorbidity and integrated care, respectively, and facilitate a number of research projects for post-doctoral fellows and faculty. He is the author of over 75 research publications and 30 chapters, books, or editorials. Dr. Oslin received is MD from University Of Virginia School Of Medicine. Amanda Harris is the Chief Operating Officer at Pathways to Housing in DC. The mission of Pathways to Housing DC is to end homelessness for people living with psychiatric disabilities by providing housing first and giving support and treatment for their recovery and integration into the community. Ms. Harris received her Master of Art, Philosophy, and Public Policy from George Washington University and Master of Social Work from University of Michigan. Josh Sharfstein is the Secretary of the Maryland Department of Health and Mental Hygiene. Previously, he served as the Commissioner of Health in Baltimore, Maryland and as the Principal Deputy Commissioner of the U.S. Food and Drug 624 N. Broadway Baltimore, Maryland 21205 (410) 955-3910 Department of Mental Health Carolyn Quattrocki, JD Rita Vandivort-Warren, MSW Administration. In these positions, Dr. Sharfstein has pursued creative solutions tlongstanding public health problems -including drug addiction, school failure, unsafe consumer products, and most recently, cheap, candy-flavored cigars. Dr. Sharfstein received his MD from Harvard Medical School. Carolyn Quattrocki is the Executive Director of Maryland Governor O’Malley’s Office of Health Care Reform. Prior to her appointment, she served as a Deputy Legislative Officer and health policy advisor in the Governor’s Legislative Office, with primary responsibility for health care, insurance, and labor issues. Ms. Quattrocki has a law degree from Yale University and a B.A. from Northwestern University. Rita Vandivort-Warren is a Public Health Analyst on financing services and government project officer in the Quality Improvement and Workforce Branch, Division of Services Improvement, Center for Substance Abuse Treatment, Substance Abuse, Mental Health Services Administration. She currently manages, among other federal projects, the SAMHSA Spending Estimates Project, which determines the total national expenditures on mental health and substance abuse services from all public and private sources. She handles numerous other assignments in financing and organization of services, integrating state cross system databases, blending funding for children’s mental health and substance abuse services, financing services expert to grantees and is the CSAT lead on Medicaid issues. Ms. Vandivort-Warren received her Master’s in Social Work from University of Missouri-Columbia. 624 N. Broadway Baltimore, Maryland 21205 (410) 955-3910