REPAIR OF PRIMARY RHEGMATOGENOUS RETINA
advertisement

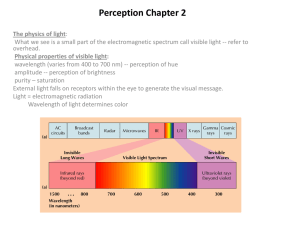
TOPIC : REPAIR OF PRIMARY RHEGMATOGENOUS RETINA DETACHMENT , WHICH SURGICAL TECHNIQUE IS BEST SUITED ? AUTHOR : OLUFEMI ODERINLO FRCS(Ed), DRCOphth (UK) CONSULTANT OPHTHALMOLOGIST AND VITREORETINA SURGEON EYE FOUNDATION HOSPITAL 27 ISAAC JOHN STREET GRA IKEJA LAGOS. NIGERIA INTRODUCTION A Rhegmatogenous retina detachment (RRD) is an ophthalmic emergency , surgical repair should be instituited as soon as possible to forestall irreversible damage to retina cells. The choice of surgical technique is very important to ensure primary anatomic success defined as successful anatomic retina reattachment without need of any futher surgical intervention. Primary anatomic success is important for good visual outcome and subsequent patient rehabilitation. Three major surgical techniques are available for repair of RRD, these include sclera buckling procedure (SB) with or with subretina fluid drainage, pars plana vitrectomy (PPV) with internal tamponade using either silicon oil or gas and pneumatic retinopexy (PR) which involves the use of intraocular gas. Surgeon preference, patient presentation and availability of facilities play a big role in deciding which technique of repair to use. No two cases of RRD are exactly the same, hence the choice of technique for repair should be individualized , a full understanding of the merits and demerits of each technique is required. In order to maintain and probably improve on present anatomic reattachment rates which is between 80 and 95% (1,2,3,4) .We need to thoroughly evaluate every patient before surgery, there is still no substituite for thorough preoperative evaluation , search for offending breaks and associated pathology and planning for possible operative complications. The aim of retina reattachment surgery still includes locating and sealing all retina breaks, relieving retina traction and bringing the retina and choroid in contact for sufficient time to allow adequate chorioretina scars to form ,after creating a chorioretina reaction with Laser or cryotherapy. A few other factors are important and these include Characteristics of the offending retina break : the size (giant retina tears, large breaks) , location ( macula, periphery , equator or posterior pole), number and type (dialysis, retinoschisis, round ,horse shoe). Associated pathology : posterior vitreous detachment (PVD), vitreous hemorrhage and debries and presence of proliferative vitreoretinopathy (PVR) are equally important considerations . Below are a few suggestions on techniques for particular RRDs 1. RRD associated with giant retina tear : Giant retina tears (GT)are retina breaks that extend over 90 degrees or more of the retina. RRDs from giant tears have certain peculiarities viz a tendency to roll over, difficulty with reattachment intraoperatively , difficulty maintaining reattachment, high risk of posterior slippage during exchange, prolonged surgical time ,tendency to multiple procedures, surgeons skill and experience is important, rapidly progressive, severe PVR can develop on both surfaces of the retina,hence redetachment surgery poses a challenge to the surgeon. Most surgeons however prefer PPV techniques for such cases, the question to use an encircling band or buckle in conjunction with PPV is seen in literature, in a recent study by Goezinne et al(5) ,they found the absence of use of an encircling sclera buckle to be associated with redetachment after vitrectomy with internal tamponade for RRDs from giant tears , this was however not corroborated by Ambresin et al (6) who had good surgical outcomes without using encircling buckles. Proponents of use of adjoining sclera buckle believe this will further relieve retina traction and support inferior retina if holes are present ,however buckles can also worsen the already rolled edges of the tears and constituite additional procedure specific complications, it also increases operative time and hence requires more resources. If an offending inferior hole exist a retinotomy and or retinectomy can be done to join all breaks when close together , a thorough fluid air exchange is important before injecting silicon oil, 5000cs may be used when longterm tamponade is required. SBs and PRs may not be effective in the longterm in managing RRDs from giant retina tears . • 2 RRD from Dialysis : A dialysis is a detachment of the neurosensory retina anterior to the ora serrata . It is important to differentiate it from a giant tear ,dialysis are 3 times more common than GTs and dialysis from trauma seen are often seen in superonasal retina quadrant, spontaneous ones in the inferotemporal . RRDs tend to progress relatively slower than with giant tears and are less likely to have rolled over edges. Scleral buckles are often successful with dialysis( 7), vitrectomy is indicated if there are other post traumatic pathologies like vitreous hemorrhage and associated irregular retina breaks, posterior breaks and significant vitreoretina traction. 3 Pseudophakic retina detachment : Scleral buckling (SB) is an established technique for the treatment of rhegmatogenous RDs. Recent advances in pars plana vitrectomy (PPV) techniques have encouraged retinal surgeons to expand the role of vitrectomy in the management of complicated and uncomplicated pseudophakic RDs. Several published reports compare anatomical outcomes following different surgical techniques in the management of pseudophakic RDs (8).A recent metaanalysis on the management of uncomplicated pseudophakic RDs revealed anatomical success rates of 81% following SB, 91% after PPV, and 97% for the combined technique of PPV with SB after a single surgery. Brazitikos et al conducted a randomized clinical trial and demonstrated a similar advantage of primary PPV over SB surgery in patients with early pseudophakic RDs (9). The retina was attached in 83% and 94% in the SB and PPV groups respectively following single surgery. Overall, the primary surgical success rate following SB varies from 61% to 97% in uncomplicated pseudophakic RDs, while the comparable anatomical outcome following PPV ranges from 84% to 98%. PPV offers the advantages of removing posterior capsular opacity, clearing vitreous debris, detecting unseen breaks, releasing vitreous traction, and removing gliogenic cells without inducing significant changes in refractive error postoperatively. Application of PPV in pseudophakic RDs is limited by inadequate endotamponade to inferior breaks , an inferior buckle can sometimes be used to support inferior breaks. PPV gives better control and satisfaction to remove all vitreous traction which often associate pseudophakic RD ,on few occasions where no significant traction or PVR occurs , a SB may be indicated, I now seldom do combined buckles and vitrectomy. 4 RRDs from Macular holes in High Myopes: In the pathogenesis of this type of detachment different types of vitreoretinal changes create both anterioposterior and tangential tractions resulting in different types of detachments. Both vitreous traction , sclera and chorioretina dysfunction play important roles while posterior vitreous detachment and posterior vitreous schisis are important considerations(10,11) A recent randomized clinical trial evaluated the use of posterior sclera buckling (PSB), pars plana vitrectomy (PPV)and pneumatic retinopexy (PR) in management and found slightly lower anatomic success (89%) at first surgeries in the PR group when compared to the other two (96% and 92%)(12) .PPV offers the advantage of relieving vitreous traction and an attempt at peeling epiretina membrane and internal limiting membrane to improve macula hole closure rates.PPV definitely has advantages for this type of detachment. 5 Inferior RRDs : RRD retina detachments involving the inferior hemisphere of the retina with the offending pathology within this area are quite challenging. SBs or PPV can be used and sometimes a combination of both. SB are useful in phakic eyes with round hole holes , minimal or no traction and when no PVR or early PVR of grade B(13) and less is present. PPV with either gas or silicon oil tamponade offers advantages in RRDs with other associated pathology such as advanced PVR, vitreous hemorrhage, old detachments and large tears. A Sharma and colleagues in a recent study (14) evaluated the use of PPV with intraocular gas tamponade and postoperative positioning in the management of inferior RRDs. Final anatomic success of 95.8 % was achieved in both the inferior RRD group and the comparative group which included other types of detachments. They concluded as follows “This study has shown that acceptable success rates can be achieved using PPV alone to treat RRD with inferior breaks. Complications are minimised and patients in this high risk group have an 81% chance of primary success. Pars plana vitrectomy and gas will successfully reattach the retina and a supplementary SB, to support the inferior retina, is unnecessary as the intraocular gas, and face up or, right or left side down positioning will tamponade breaks satisfactorily”. Similar findings were reported by Tanner et al (15). Different heavy tamponades have been evaluated for surgery in RRDs , most evalauations involve inferior detachment and are said to have theoretical advantages of better tamponading effects in the inferior retina, however , high complication rates are reported in the first two generation of these heavy tamponade (16,17). Although the newer preparations may be safer many surgeons still approach their use with caution. Inferiror retinectomy with radical anterior vitreous base dissection can be useful in many complicated cases(18,19). 6 Superior RRDs: PPV, SB or PR may be appropriate in different case scenerios of superior RRDs. A recent study (20) addressed RRDs with breaks located within 1 clock hours in the superior 2/3rds of the retina and PVR not exceeding grade B, Scleral buckling was compared with pneumatic retinopexy with regard to single-operation reattachment (82 versus 73%), reattachment with one operation and postoperative laser/cryotherapy (84 versus 81%), although the anatomic results of the two operations were not significantly different (P greater than 0.05), pneumatic retinopexy had less morbidity and better postoperative visual acuity (P = 0.01). Pneumatic retinopexy is recommended for cases meeting the admission criteria. PR offers advantages of single operation reattachment and that sometimes it can be done as an office procedure, however postoperative evaluation is very important as it has higher rates of missed breaks and limits air travel in the immediate period. It is also better suited for uncomplicated cases that meet the above criteria ( holes within 1 clock hours in the superior 2/3rds of the retina). PPV offers advantages in more complex cases and both air and silicon oil are good tampondes for the superior retina . Minimal Segmental buckles without drainage also have unique advantages as primary procedures in superior RRDs, there are no intraocular complications (except for a rare choroidal hemorrhage in about 0.3%).Secondary glaucoma, cataract, intraocular hemorrhage, intraocular infection, retina incarceration and iatrogenic breaks are almost completely eliminated (21,22,23,24). Saw et al concluded in their study(25) evaluating various interventions available for RRD as follows “Pneumatic retinopexy is a possible alternative to scleral buckling in the treatment of uncomplicated rhegmatogenous retinal detachment. The rates of missed or new retinal breaks after pneumatic retinopexy, however, are higher than following scleral buckling. The clinical outcomes of vitrectomy for rhegmatogenous retinal detachment compare favourably”. PPV has advantages in complex cases and intraocular tamponade with silicon oil is also good for superior breaks. Superior RRDs definitely have a higher number of options for primary repair. The African Dilema Patients with RRDs in African populations often present late with complex pathology, (26,27) The general expectation is that RRDs with complex pathologies achieve better anatomical results with PPV, giant tears , advanced PVR, Longstanding RRDs all tend to do better with PPV. The combined primary success rate of larger consecutive studies with SB in a recent review was 85% , compared with a between 75 -91% in PPV as summarized by Wilkinson (28) These results suggest that more of the cases presenting for surgery in Africa will require PPV, unpublished data from our department showed we use primary PPVs in 74.8% of RRDs. Unfortunately equipment for vitrectomy is expensive and only few instituitions in Africa have such facilities. Facilities for SBs are relatively less expensive and the procedure seemingly less difficult to learn. Provided early presentation is ensured and less complex pathology, SBs can be done in a large number of patients with RRD, others should be promptly refered to instituitions with available facilities. Tertiary Centres with facilities for PPV should not be too few and regular training and updates should be encouraged. JOIN THE DEBATE SO a twenty five year old apprentice presented with six months history of sudden loss of vision in his only seeing right eye following trauma during a confrontation with a fellow apprentice , examination revealed visual acuities of hand movements OD and No light perception, anterior segements were essentially normal OD with intraocular pressures of 03mmHg by applanation tonometry. The left eye was pthisical. Funduscopy OD revealed a rhegmatogenous retina detachment with a giant macula tear with rolled edges (Figure 1). What surgical procedure is best suited for SO. What intraoperative precursions should be taken. Please send your contributions about themanagement of SO or about the above topic to : olufemi_oderinlo@yahoo.com, I would very much like to know your views. Thank you Figure 1. REFERENCES 1. Gartry,Chingnel AH, Franks WA, Wong D. Pars plana vitrectomy for the treatment of rhegmatogenous retina detachment uncomplicated by advanced proliferative vitreoretinopathy.Br J Ophthalmol 1993: 77:199-203 2. Kiss CG, Richter-Muksch S, Sacu S, Benesch T, Velikay-Parel M. Anatomy and function of the macula after surgery for retinal detachment complicated by proliferative vitreoretinopathy. Am.J.Ophthalmol. 2007 Dec;144(6):872-877. 3. Laidlaw D A, Clark B, , Grey R H , Markham R H . Results of primary retina detachment surgery ( a prospective audit).Eye:12:751 4. Richardson EC, Verma S Green WT et al. Primary vitrectomy for rhegmatogenous retina detachment (an analysis of failure). Eur J Ophthalmol 2000; 10: 160-166. 5. Goezinne F, L A Heij EC, Berendschot T T, Gast S T, Liem A T, Lundgust I L, Hendrikse F. Low redetachment rate due to encircling sclera buckle in giant retinal teras treated with vitrectomy and silicon oil. Retina 2008 Mar; 28(3) : 485 -92 6. Ambresin A, , Wolfensberger T J, Bovey E H. Management of giant tears with vitrectomy, internal tamponade, and peripheral 360 degrees retina photocoagulation. Retina 2003 Oct ;23(5) :622-8 7.James M, O’Doherty M, Beatty S .Buckle related complications following surgical repair of retina dialysis Eye 2008 April; 22(4) : 485-90. Epub 2006 Dec 1 8. Erie JC, Raecker MA, Baratz KH, et al. Risk of retinal detachment after cataract extraction, 19802004 :a population based study. Ophthalmology 2006;113:2026-2032. 9. Brazitikos PD, Androudi S, Christen WG, Stangos NT. Primary pars plana vitrectomy versus sclera buckle surgery for the treatment of pseudophakic retinal detachment a. A randomized clinical trial Retina. 2005;25(8):957-964. 10. Wilkinson CP, Rice TA. Prevention of retina detachment .In : Wilkinson CP, Rice TA, eds. Michels Retinal Detachment.2nd ed St. Louis Mosby;1997: 1081 -133. 11.Moria H, Ideta H, Ito K et al.Causative factors of retinal detachments in macular holes. Retina 1991; 11: 281-284 12. Ripandelli G, Parisi V, Friberg TR, Coppe AM, Scassa C, Strirpe M. Retina Detachment associated with macula hole in high myopia: using the vitreous anatomy to optimize the surgical approach.Ophthalmology 2004 ; 111(4):726-731 13. Retina Society Terminology committee. The classification of retinal detachment with proliferative vitreoretinopathy. Ophthalmology 1983:90:121-125 14. Sharma A, Grigoropoulos V, Williamson T H. Management of primary rhegmatogenous retina detachment with inferior breaks. Br J Ophthalmol 2004 Nov ; 88(11): 1372-1375 15 Tanner V, Minihan M, Williamson T. Management of inferior retina breaks during pars plana vitrectomy for retina detachment. Br J Ophthalmol 2001 April ;85(4): 480-482 16 Heimain H, Stappler T, Wong D. Heavy tamponade 1: a review of indications, use, and complications. Eye 2008 Oct ;22(10):1342-59 17 Stappler T, Heimann H, Wong D, Gibran S K, Groenewald C, Pearce I A. Heavy tamponade 2 Densiron in routine clinical practice: anatomical and functional outcomes of a consecutive case series. Eye 2008 Oct; 22(10): 1360-5 18 Quiram PA, Gonzales C R, Hu W, Gupta A, Yoshizumi M O, Kreiger A E, Schwartz SD. Outcomes of vitrectomy with inferiror retinectomy in patients with recurrent rhegmatogenous retinal detachments and proliferative vitreoretinopathy. Ophthalmology 2006 Nov ; 113(11):2041-7 19 Grigoropoulus V G, Benson S, Bunce C, Charteris D G. Functional outcome and prognostic factors in 304 eyes managed by retinectomy. Graefes Arch Clin Exp Ophthalmol. 2007 May;245(5) :641-9 20. Tornambe P E, Hilton G F. Pneumatic retinopexy . A multicenter randomized controlled clinical trial comparing pneumatic retinopexy with sclera buckling. The Retina Detachment Study Group. Ophthalmology 1989 Dec :96 (12):1811-2 21. Barrie T, I Kreissig, H Heimann, Holz E R, Mieler W F. Repair of primary rhegmatogenous retina detachment. Br J Ophthalmol 2003;87:782-789 22 Kreissig I, Rose D, Jost B. Minimized surgery for retina detachment with segmental buckling and nondrainage. An 11-year followup. Retina 1992;12:221-31 23 Sivkova N, Katsarov K, Kreissig I et al. Our experience in minimized surgery for retina detachment: first results. Folia medica 1997;34:44-7 24 Kreissig I. A practical guide to minimal surgery for retina detachment. Vol 2.Stttgart,New York:Thieme 2000;13:305 25 Saw S M,Gazzard G,Wagle A M, Lim J, Au Eong K G.An evidence based analysis of surgical interventions for uncomplicated rhegmatogenous retina detachment. Acta Ophthalmol Scand 2006 Oct ;84(5):595-6 26 Peters AL. Retinal detachment in black South Africans. S Afr Med J. 1995;85:158–159. 27Kaimbo K, Maertens K, Kayembe L, et al.. [Retinal detachment in patients from Zaire: etiological, clinical aspects, surgical treatment]. Bull Soc Belge Ophtalmol. 1986;218:83–93. 28.Wilkinson CP, Rice TA. Results of retina reattachment surgery In: Michels retina detachement. 2nd ed. St Loius : Mosby, 1997:935-78