Male Slings - Laborie Medical Technologies
advertisement

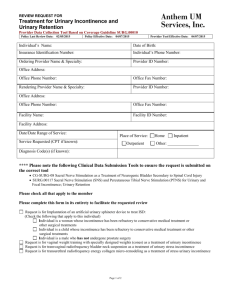
Male Slings: Past, present, and Future. Issues in Incontinence: Spring/Summer 2008 By Edward Zoltan, MD and Alexis Te, MD Incontinence following prostatectomy can be a devastating complication significantly impacting quality of life. The prevalence of post-prostatectomy urinary incontinence (PPI) varies from 2.5%–87%, with 2%–10% reported in more recent series.1,2 Incontinence can also occur in 1% of patients undergoing surgical treatment for benign prostatic hypertrophy. 1 Although the incidence of PPI has decreased with better understanding of neurovascular anatomy and the advent of the robotic prostatectomy with its novel techniques of urethral reconstruction,3 it continues to be one of the most feared complications after surgery. Part of the reason for the wide range in reported PPI lies in the use of different definitions of incontinence with accompanying divergent methods of assessment. Evaluation The evaluation of patients with PPI should begin with a comprehensive history, including onset, duration, evolution, cause of the leakage, and the number of pads used. It is important to assess how the incontinence affects daily activities and if the patient is bothered by it. The pad-weight test may be used to objectively assess the severity of incontinence. Any history of surgery or radiation should be noted. A voiding diary can be helpful to quantify fluid intake and functional bladder capacity. Physical examination is performed with emphasis on neurological assessment of the S2-S4 spinal segments, including anal sphincter tone, perineal sensation, and bulbocavernosus reflex. Abdominal palpation may detect a distended bladder with overflow incontinence. Urodynamic evaluation may differentiate between the various causes of PPI in addition to ruling out poor bladder compliance,high-pressure detrusor overactivity during filling, and bladder obstruction during the flow portion of the study. Bladder capacity is also measured, as most patients with severe incontinence have low functional bladder capacity because of poor storage ability. Management Male stress urinary incontinence (SUI) may be addressed by numerous established methods. These vary from relatively noninvasive methods of pelvic floor stimulation or biofeedback to progressively more invasive methods involving the use of various injectable bulking materials, bulbourethral slings, and the artificial urinary sphincter. Since spontaneous improvement of urinary incontinence may take up to 12 months, it has been recommended that surgical intervention be postponed in men with PPI until 12 months after the prostatectomy.1 Other contraindications to surgical intervention include the inability to operate a device, and any disorders jeopardizing the upper urinary tract, including diminished bladder compliance, frequent highpressure detrusor contractions, or vesicoureteral reflux at low intravesical pressures. Any urinary tract abnormalities requiring future transurethral management may also be considered relative contraindications to outlet surgery. Stress incontinence surgery is not recommended in patients with untreated low-volume detrusor overactivity that would not permit adequate symptomatic improvement. Chronic infection of the urine or skin, anatomic abnormalities, immunosuppression, and poor urethral tissue quality are also relative contraindications.4 Artificial urinary sphincter The artificial urinary sphincter (AUS) is the gold-standard treatment for postprostatectomy SUI. The AMS 800 device (American Medical Systems, Minnetonka, MN) provides acceptable social continence in approximately 90% of patients. Introduced over 30 years ago, the device has continually evolved to its current and sophisticated form. It is widely used in clinical practice, and over 100 000 devices have been implanted worldwide. Several complications may occur in AUS patients. Urethral erosion occurs in 1%–3% of patients and may be precipitated by infection, excessive cuff pressure, decreased vascularity from prior radiation, an undersized cuff, or traumatic catheterization through an activated cuff. 5,6 Infection occurs in 1.8%–10% of patients.7 AUS revision rates currently hover around 9%, with an expected 5-year survival of narrow-backed AUS of 75%.7 Persistent stress incontinence may occur in up to 15% of patients after AUS insertion.8 Urethral atrophy may cause residual incontinence despite AUS placement, with an incidence of 3%–9%; management options include downsizing the cuff or placing a tandem cuff. 6 Post-AUS SUI may also be due to an excessively loose cuff or low reservoir pressure. Bulking agents Introduced in 1993, bovine glutaraldehyde cross-linked collagen (Contigen; CR Bard, Covington, GA) has been used extensively as a bulking agent in the treatment of intrinsic sphincter deficiency in men. Collagen implantation is well tolerated and has a low complication rate. Although recommended for mild to moderate male SUI, repeated injections are often necessary to establish and then maintain continence; indeed, the longterm results of such injection therapy have been disappointing. 9,10 It has been reported 11 that the best results can be obtained in patients with mild degrees of incontinence and a preoperative Valsalva leak-point pressure > 60 cm H2O. Previous male slings Before the AUS was introduced, a variety of urethral compression procedures was attempted to control urinary incontinence. One of the first prosthetic devices was described by Berry 12 in 1961. It was an acrylic device placed beneath the bulbocavernosus muscle, designed to kink and compress the bulbous urethra at a point just distal to the urogenital diaphragm. The procedure was then modified to include the use of stainless steel sutures, passed through drill holes in the ischial and pubic rami. 13 However, high rates of perineal pain and fistula formation in the presence of only modest success led to the abandonment of the Berry prosthesis. 14 In 1970, Kaufman 15 described a surgical method for compressing the urethra. In this Kaufman type-I anti-incontinence procedure, the penile crura were crossed over the bulbous urethra to produce urethral compression, but success rates were low (30%). In the Kaufman type-II procedure, 16 the crura were approximated in the midline using a polytetrafluoroethylene mesh tape. The synthetic tape was folded in such a manner as to compress the bulb of the urethra. Success rates increased to 50%. The Kaufman type-III procedure 17 used a silicone-gel-filled hemispherical prosthesis, surrounded by external velour of polyurethane and 2 polyurethane straps, leading to success rates approaching 70%. Kishev 18 next described a combined abdominoperineal approach utilizing a pliable prosthetic wad under the bulbar urethra, with tension provided by nylon sutures that are passed through the retropubic space and secured over small Marlex pledgets above the abdominal fascia. The Kaufman and Kishev prostheses ultimately fell out of favor, however, because of high failure rates, infectious complications, pelvic pain, and the introduction of the AUS. Based on the Kaufman and Kishev techniques, Clemens et al. 19 described a bulbourethral sling procedure in 64 men with severe PPI. A suture with a series of tetrafluoroethylene bolsters was passed underneath the bulbar urethra with a Stamey needle and brought through suprapubically lateral to the urethra and bladder neck, thus compressing the bulbar urethra. At a mean followup of 18 months, 56% of patients became dry, while 8% were significantly improved; this resulted in a 38% cure rate and a 49% pad-free rate. However, sling revision was required in 21% of patients, while bolster removal was necessary secondary to infection or erosion in 6%. Moreover, 52% of patients complained of chronic perineal numbness or pain, although this decreased to 18% at 4-year followup. 20 This discomfort was most likely due to high-pressure entrapment of pudendal nerve branches during blind suprapubic suture passage. Current male slings More recently, bone-anchored perineal male slings were introduced by Franco and Baum 21 and Madjar et al. 22 These were later popularized by Comiter 23 and Rajpurkar et al. 24 The use of bone anchors obviates the need for blind suprapubic transfer of sutures to achieve bulbourethral compression and eliminates the need for abdominal incisions. Such slings utilize 6 titanium 5-mm screws drilled into the anteromedial aspects of each descending pubic ramus using the InVance bone drill (InVance, American Medical Systems) (see Figure 1). These screws are preloaded with a pair of number-1 polypropylene sutures. The topmost bone screws are placed just beneath the junction of the descending ramus and pubic symphysis; the remaining sutures are placed 1 cm apart on each side. A rectangle (4 x 7 cm) of polypropylene mesh alone or in combination with the dermis as a composite graft is used as sling material. After 1 side of the sling is anchored to the pubic ramus, sling tension is adjusted, guided either by the retrograde leak-point pressure method or, if the patient is awake, by the simple cough method. The sling is then tied down to the opposite pubic ramus. Persistent scrotal/perineal pain is a relatively unusual occurrence (10%); however, small pudendal nerve branches do travel along the medial aspect of the descending pubic rami and may be injured during dissection or screw insertion. Complaints of pain without evidence of infection should be managed conservatively with narcotics and anti-inflammatory medication. If pain persists after 6–8 weeks of conservative management, consideration should be given to sling removal. One must always consider the risk of osteomyelitis or osteitis pubis in these cases. As is the case with pubic symphyseal bone anchors in women, bone anchor removal is a difficult procedure and usually recommended only in cases of bony infections. Unlike the AUS, which circumferentially compresses the urethra—thereby interfering with venous blood flow and thus predisposing the urethra to atrophy and even erosion—the male sling compresses only the ventral aspect of the bulbar urethra, leaving the dorsal and lateral blood flow intact. Moreover, the bulbospongiosus muscle and other tissue are left intact over the urethra, serving as a cushion between the urethra and the sling and further minimizing the risk of erosion. The infection and erosion rate for perineal slings is low (2.1%), with an accompanying low rate of revision caused by bone anchor dislodgement (4.2%). 25 Another advantage of the male sling over the artificial urinary sphincter is that voiding occurs sans device manipulation. There is no postoperative activation necessary: as soon as the urinary catheter is removed, normal voiding may occur. In addition, without the hydraulic system as found in the AUS, the risk of mechanical malfunction is minimized. Sling implantation also does not preclude later AUS use. 26 In this study where an AUS was placed after male sling failure, 72.7% of patients were dry following AUS implantation, while another 9.1% reported improved continence. No complications were reported during urethral dissection in patients with prior male sling procedures. Excellent cure rates have been reported with the bone-anchored perineal sling, ranging between 70% and 90%. 21-24 Comiter recently reported 25 intermediate-term results with a median followup of 48 months: mean pad usage decreased from 4.6 ± 2.1 to 1.0 ± 1.7 pads per day (p < .01); 65% were considered cured of leakage while another 15% were significantly improved. Similar results were obtained by Rajpurkar et al. 24 who reported a success rate of 74% in patients with a mean follow-up of 24 months. Onur et al. compared the use of synthetic with absorbable graft material in perineal slings. In a study 27 of 46 men, success rates were significantly higher in patients receiving synthetic mesh, either alone or as composite graft, compared with patients receiving absorbable material alone (75% vs. 97% vs. 0% respectively, p < .05). All patients with failed procedures had absorbable graft-type slings. Patients with mild to moderate incontinence (< 5 pads/ day) had a significantly better outcome compared to those with severe incontinence (≥ 5 pads/day). The future of male slings A new transobturator male sling system (AdVance, American Medical Systems) (see Figure 2) has recently been approved for use in the United States. With this system, a midline perineal incision is made, exposing the bulbospongiosus muscle, which is then split centrally and retracted laterally. The dissection is extended to the perineal body. After exposure of the urethral bulb, blunt-finger dissection is used to identify the space between the corpora cavernosa laterally and the corpus spongiosum medially. A small skin incision is made in the leg fold on the lateral side of the scrotum, 1 cm below and lateral to the insertion of the adductor longus tendon at the medial border of the obturator foramen. The index finger of the surgeon is then placed between the urethral bulb medially and the proximal corpus cavernosum laterally, just inside the bulbospongiosus muscle. The helical curved introducer needle is placed over the skin incision and mild force is used to perforate the subcutaneous tissue and obturator fascia, maintaining a constant axis of rotation at 45°. The needle is passed towards the tip of the finger and the tape is then positioned through both obturator fossae. With 2 absorbable sutures the middle part of the polypropylene tape is then fixed distally onto the bulb and proximally onto the perineal body. The tape is then pulled at both ends to its final position, and the ends are cut at skin level. Short-term results of this technique have shown it be effective in 70% of patients. 28 Recently, various adjustable male slings such as ProACT (Uromedica, Plymouth, MN),29 Remeex (Neomedic, Barcelona, Spain), 30 and Argus (Promedon SA, Cordoba, Argentina)31 have been introduced in Europe; these slings can be variably tensioned according to patient needs and the degree of recurrent urinary incontinence. The ProACT device (see Figure 3) is constructed from silicone elastomer, similar to the materials used in the AMS 800 AUS. Two ProACT balloons are attached to a reinjectable titanium port with a short length of tubing and are then implanted periurethrally, on either side of the bladder neck, just proximal to the remnant external sphincter. The ports are sited subcutaneously under the scrotal dartos fascia to allow for future percutaneous adjustments of the balloon volume. A recent paper comparing the last 50 patients to the first 50 patients using ProACT showed a significant improvement in results.31 Pad usage was reduced significantly in both groups (p < .001). Overall, lategroup patients obtained more consistent outcomes than early-group patients (80% vs. 60% dry). I-QOL (incontinence quality of life scale) scores improved in both groups although more significantly in the late group (p = .005). Operative time and range of complications decreased with evolution of technique. The Argus sling (see Figure 4) possesses 3 components: a silicone foam cushion (4.2 x 2.6 x 0.9 cm) designed to provide bulbourethral compression, silicone columns attached to both ends of the pad for fixation against the abdominal rectus fascia, and silicone washers. All components are radio-opaque to allow sling repositioning after implantation. The device can be regulated by moving the washers up and down to create the desired tension. The Argus device is inserted through both a suprapubic and a perineal incision, in the same fashion as that described by Schaeffer et al. 32 A European multi-center trial enrolling 48 patients found the device to be very effective. At a mean followup of 7.5 months, 35 (73%) of the patients were dry, and 5 (10%) were improved, although 8 (17%) were incontinent, including 4 (8%) who needed sling adjustment.32 There were 3 (6%) urethral perforations during surgery that were resolved by re-passing the needle. The sling was removed from 3 men (6%) due to erosion and from 2 (4%) due to infection. This compares favorably to the complication rate associated with artificial urinary sphincters. The male Remeex system is composed of a monofilament suburethral sling connected to a suprapubic mechanical regulator with 2 monofilament traction threads (see Figure 5). The mechanical regulator, or varitensor, is a subcutaneous permanent implant, placed over the abdominal rectum fascia 2 cm above the pubis, used to wind and tighten the traction threads. The suburethral sling is also placed in a fashion similar to that for the Schaeffer sling. In a recent multi-center European study, 33 51 patients with mild to severe stress urinary incontinence were treated with the Remeex system. Of these, 44 (86%) patients required a single adjustment of tension between 1 and 4 months after surgery, while 17 (33%) other patients required more than 1 delayed tension adjustment. Overall, 33 (65%) patients were considered cured, another 10 (20%) showed improvement, while 8 (16%) were unchanged. The average follow-up time was 32 months. The mesh was removed in 1 (2%) case due to urethral erosion, and the varitensor in 2 (4%) cases was removed due to infection. There were 5 (10%) uneventful intraoperative bladder perforations and 3 (6%) mild perineal hematomas reported. Conclusion Male stress urinary incontinence may be treated with multiple modalities. Current surgical options for post-prostatectomy incontinence include bulking agents such as collagen and devices such as the AUS. Low success rates with bulking agents and high revision rates with the AUS have prompted a resurgence of interest in fixed urethral compression procedures. The modern male sling is an exciting development in fixed urethral compression. Patients with mild to moderate SUI may benefit greatly from use of this technology. References 1. Haab F, Yamaguchi R, Leach GE. Postprostatectomy incontinence. Urol Clin North Am. 1996;23:447-57. 2. Majoros A, Bach D, Keszthelyi A, Hamvas A, Romics I. Urinary incontinence and voiding dysfunction after radical retropubic prostatectomy (prospective urodynamic study). Neurourol Urodyn. 2006;25:2-7. 3. Tewari A, Jhaveri J, Rao S, Yadav R, Bartsch G, Te A, et al. Total reconstruction of the vesico-urethral junction. BJU Int. 2008;101:871-7. 4. Staskin DR, Comiter CV. Surgical treatment of male sphincteric urinary incontinence: the male perineal sling and artificial urinary sphincter. In: Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, eds. Campbell-Walsh Urology. 9th ed. Philadelphia, PA: SaundersElsevier; 2007:2391-404. 5. Elliott DS, Barrett DM. Mayo Clinic long-term analysis of the functional durability of the AMS 800 artificial urinary sphincter: a review of 323 cases. J Urol. 1998;159:1206-8. 6. Litwiller SE, Kim KB, Fone PD, White RW, Stone AR. Post-prostatectomy incontinence and the artificial urinary sphincter: a long-term study of patient satisfaction and criteria for success. J Urol. 1996;156:1975-80. 7. Tse V, Stone AR. Incontinence after prostatectomy: the artificial urinary sphincter. BJU Int. 2003;92:886-9. 8. Hübner WA, Schlarp OM. Treatment of incontinence after prostatectomy using a new minimally invasive device: adjustable continence therapy. BJU Int. 2005;96:587-94. 9. Schneider T, Sperling H, Rossi R, Schmidt S, Rübben H. Do early injections of bulking agents following radical prostatectomy improve early continence? World J Urol. 2005;23:338–42. Epub 2005 Nov 1. 10. Westney OL, Bevan-Thomas R, Palmer JL, Cespedes RD, McGuire EJ. Transurethral collagen injections for male intrinsic sphincter deficiency: the University of TexasHouston experience. J Urol. 2005;174:994–7. 11. Sánchez-Ortiz RF, Broderick GA, Chaikin DC, Malkowicz SB, Van Arsdalen K, Blander DS, et al. Collagen injection therapy for post-radical retropubic prostatectomy incontinence: role of Valsalva leak point pressure. J Urol. 1997;158:2132-6. 12. Berry JL. New procedure for correction of urinary incontinence: a preliminary report. J Urol. 1961:771-5. 13. Kishev SV. Surgery for male urinary incontinence. In: Glenn JF, ed. Urologic Surgery. 2nd ed. Philadelphia, PA: JB Lippincott; 1975:596-611. 14. Engel RM, Wade JC. Experience with the Berry prosthesis. J Urol. 1969;102:78-80. 15. Kaufman JJ. A new operation for male incontinence. Surg Gynecol Obstet. 1970;131:295-9. 16. Kaufman JJ. Surgical treatment of post-prostatectomy incontinence: use of the penile crura to compress the bulbous urethra. J Urol. 1972;107:293-7. 17. Kishev S, Blakely G, Sanford E. Experience with Kaufman’s operation for correction of postprostatectomy urinary incontinence (sagging urogenital diaphragm—a theory for the cause of incontinence). J Urol. 1972;108:772-7. 18. Kishev SV. Surgery for male urinary incontinence. In: Glenn JF, ed. Urologic Surgery. 2nd ed. Philadelphia, PA: JB Lippincott; 1975:596-611. 19. Clemens JQ, Bushman W, Schaeffer AJ. Questionnaire based results of the bulbourethral sling procedure. J Urol. 1999;162:1972-6. 20. Stern JA, Clemens JQ, Tiplitsky SI, Matschke HM, Jain PM, Schaeffer AJ. Long-term results of the bulbourethral sling procedure. J Urol. 2005;173:1654-6. 21. Franco N, Baum N. Suburethral sling for male urinary incontinence. Infect Urol. 2001;14:10-8. 22. Madjar S, Jacoby K, Giberti C, Wald M, Halachmi S, Issaq E, et al. Bone anchored sling for the treatment of post-prostatectomy incontinence. J Urol. 2001;165:72-6. 23. Comiter CV. The male sling for stress urinary incontinence: a prospective study. J Urol. 2002;167(2 Pt 1):597-601. 24. Rajpurkar AD, Onur R, Singla A. Patient satisfaction and clinical efficacy of the new perineal bone-anchored male sling. Eur Urol. 2005;47:237-42. 25. Comiter CV. The male perineal sling: intermediate-term results. Neurourol Urodyn. 2005;24:648-53. 26. Broghammer J, Singla A, et al. Feasibility of artificial urinary sphincter after male sling failure. Paper presented at: Society for Urodynamics and Female Urology Annual Meeting; 2006; Bahamas. 27. Onur R, Rajpurkar A, Singla A. New perineal bone-anchored male sling: lessons learned. Urology. 2004;64:58-61. 28. Rehder P, Gozzi C. Transobturator sling suspension for male urinary incontinence including post-radical prostatectomy. Eur Urol. 2007;52:860-6. Epub 2007 Feb 12. 29. Hübner WA, Schlarp OM. Treatment of incontinence after prostatectomy using a new minimally invasive device: adjustable continence therapy. BJU Int. 2005;96:587-94. 30. Sousa-Escandén A, Rodríguez Gómez JI, Uribarri González C, Marqués-Queimadelos A. Externally readjustable sling for treatment of male stress urinary incontinence: points of technique and preliminary results. J Endourol. 2004;18:113-8. 31. Moreno Sierra J, Victor Romano S, Galante Romo I, Barrera Ortega J, Salinas Casado J, Silmi Moyano A. New male sling “Argus” for the treatment of stress urinary incontinence. [In Spanish]Arch Esp Urol. 2006;59:607-13. 32. Schaeffer AJ, Clemens JQ, Ferrari M, Stamey TA. The male bulbourethral sling procedure for post-radical prostatectomy incontinence. J Urol . 1998;159:1510–5. Erratum in: J Urol 1998;160:136. 33. Sousa-Escandón A, Cabrera J, Mantovani F, Moretti M, Ioanidis E, Kondelidis N, et al. Adjustable suburethral sling (male remeex system) in the treatment of male stress urinary incontinence: a multicentric European study. Eur Urol. 2007;52:1473-9. Epub 2007 Jun 4.