file
advertisement
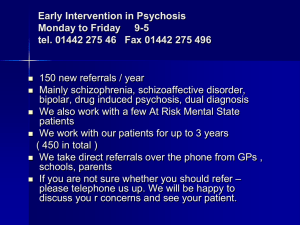
Psychosis 1. Description a. Psychosis a general term which includes all severe mental disorder e.g. acute or chronic psychosis is a sever disturbance of thought and behavior It is severe disturbance of thoughts and behavior resulting in individual losing touch with reality. This leads to gross impairment of the individual's ability to carry out his responsibilities and day to day functions. The individual being not aware of his illness refuses treatment and usually the relatives bring him for treatment. (1) b. Classification: There are different types of psychosis: a. b. c. d. e. f. g. Acute psychosis (including psychosis that is induced by drugs such as cannabis) Schizophrenia or chronic psychosis Postpartum psychosis There are also other disorders that present with psychotic symptoms: Bipolar disorder, mania Depression with psychotic symptoms (for discussion see the section on depression) Psychotic disorder due to Organic conditions affecting the brain(2) 2. Diagnosis: 1. Common clinical symptoms and signs: Positive symptoms includeing:1)Delusions 2)Hallucinations 3)disturbed behavior4)agitation or bizarre behavior 5)disorganized or strange speech 6)extreme and rapidly changing emotional states 7) negative symptoms(absence of emotions, initiative, movement and interest) 2. Diagnosis: As a general guideline when a person has more than two of the above mentioned symptoms, a doctor can make a diagnosis of psychosis. This diagnosis may be further supported by observations of the patient’s behavior or reports made by the patient’s family If the duration of the illness less than one month the diagnosis is acute psychosis and if more than that it is chronic psychosis(1) 3. Differential Diagnosis: - Differentiation between different types of psychosis mentioned above - Physical disorders: which can cause psychotic symptoms include: Epilepsy, Intoxication or withdrawal from drugs or alcohol, Infectious or febrile illness - Prescription medicines like steroids - If psychotic symptoms are recurrent or chronic, also see chronic psychotic disorders if symptoms of mania are prominent, the patient may be experiencing a manic episode. See Bipolar disorder if low or sad mood is prominent, also see Depression.(2) 3. Management: A. Non-pharmacological Treatment: - Ensure the safety of the patient and those caring for him/her: - Family or friends should stay with the patient - Ensure that the patient’s basic needs (e.g., food and drink) are met - Take care not to harm the patient. - Minimize stress and stimulation. o o - Do not argue with psychotic thinking (you may disagree with the patient’s beliefs, but do not try to argue that they are wrong). Avoid confrontation on criticism unless it is necessary to prevent harmful or disruptive behavior. Agitation which is dangerous to the patient, the family or the community requires hospitalization or close observation in a secure place. If patients refuse treatment, measures may be needed, see - management of violent/aggressive patient Encourage resumption of normal activities after symptoms improve. In chronic psychosis: In case of need for admission and presence of co-morbid physical conditions consider referral. In cases of severe motor side-effects or the appearance of fever. Rigidity, hypertensions, stops antipsychotic medication and refer.(2) B. Pharmacological Treatment: 1. The same medication is used for acute psychosis and for chronic psychosis (schizophrenia) - a. The main difference is that in acute psychosis the duration of medication can be much shorter (several weeks to months) while in schizophrenia it is much longer. Duration of treatment for acute psychosis is about one month, most patient recover within this period and may not have second episode. b. Antipsychotic medication will reduce psychotic symptoms (e. g., haloperidol 2-5mg two to three times a day or chlorpromazine 100—200mg up to three times a day). The dose should be the lowest possible for the relief of symptoms, though some patients may require higher doses. Oral antipsychotics :Chlorpromazine 200 mg at the beginning in divided doses, increase 100 mg every 2-3 days (max 600 mg) Haloperidol 5-15 mg, starting with low dose and increase gradually every 2-3 days. - If these do not work properly given in an appropriate dosage for an appropriate duration, it is important find out why. If the treatment does not work because the patient refuses to take tablets by mouth, then switch to injections of flufenazine. c. Anti-anxiety medication may also be used in conjunction with neuroleptics to control acute agitation (e. g., Diazepam 2-5 mg up to 3 times a day). d. Continue antipsychotic medication for at least three months after symptoms resolve. e. Monitor for side—effects of medications: f. Long acting antipsychotics When a patient is unable to take the medication orally one can prescribe long acting injections with antipsychotics. In the Afghan Essential Drug list one long acting antipsychotic is mentioned: Fluphenazine decanoate (25 mg/ml) g. In general, antipsychotic medication should he continue for at least three months following a first episode of illness and longer after a subsequent episode? h. If the patient fails to take medication as requested, inject able long-acting antipsychotic medication may ensure continuity of treatment and reduce risk of relapse. 2. acute dystonias or spasms may he managed with inject able benzodiazepines or antiparkinsonian drugs akathisia (severe motor restlessness) may he managed with dosage reduction or beta-blockers parkinsonian symptoms (tremnor, akinesia) may he managed with oral antipankinsonian drugs (e. g., trihexyphenidyl hydrochloride 2-5 mg/day or biperiden 2mg up to three times a day).(1), (2) 3. Duration of treatment: - Anti-psychotic medication works gradually. It may take weeks before it shows its full effect. Within hours: A patient who is very agitated becomes less aggressive. S/he feels more relaxed and sleepy. Within days to weeks: The patient sleeps better and hallucinations (voices/sounds) occur less frequently or are not as loud. After weeks: The delusions decrease. The patient may seem less convinced that her/his ideas are the truth, or even doubt about her/his delusions. (2) C. Referral: In case of need for admission and presence of co-morbid physical conditions consider - referral. In cases of severe motor side-effects or the appearance of fever. Rigidity, hypertensions, stops antipsychotic medication and refer.(1) 4. Prevention: prevention of relapse (regular medication), follow up , prevention side effect of medications and psycho-social care( Improve social skills, Contributing to family income, Divert the mind of the person, Increase self esteem, Reduce stigma, Bring an order to life, Integrate the person into community)(2)(1) 5. Patient Instructions: A. General advise to the patient and family: - Advise the family that the strange behavior and the agitation of the patient are caused by the disease. - Discuss the importance of medication. - Discourage the use of hashish - Inform them about the importance of minimizing stress: Do not argue with the patient about her/his psychotic beliefs. Do not say that you agree with her/his ideas, either, but respect them. Avoid confrontation or criticism. When the symptoms are severe, rest and withdrawal can be helpful. Recommend a structured daily life: the same pattern every day helps the patient feel safe. Advice them to find activities that help distract the person from her/his thinking, and make him/her feel valuable. Encourage them to find suitable work for the person. Occupational or vocational training and employment in a protected environment will help.(1)(2) B. Medication instructions: - Discuss treatment plan with patient - Antipsychotic drugs should be chosen after considering their relative side effects - Use only one antipsychotic drug at a time - Start with low doses - increase slowly - Use minimum dose required to maintain remission and avoid side effects - Monitor symptoms and side effects - Switch to another AP if symptoms does not respond to adequate dose in 4 weeks (2)(1) C. Follow-up instructions: During follow-up, doctor should monitor the patient for signs of psychosis, mood swings, violence and self-harmful behaviors and most important for psychosocial interventions. When the patient's condition has become stable, the doctor may not need to see the patient as often, although the frequency of follow-up visits depends on the course of the illness, the patient's adherence to treatment, medication requirements, the need for ongoing psychotherapy and patterns of care in a particular geographic area.(1) Psychosis after Childbirth - - After childbirth, a mother may develop an acute and serious psychotic disorder. The symptoms of psychosis become obvious in the first 2 weeks after the delivery. When alone, she may harm herself or the baby, or neglect the baby. A woman with post-partum psychosis and her baby require immediate attention. When the condition is severe (for example, if she intends to harm herself or the baby), they will have to be admitted to the hospital. In this case, family members should be instructed to remain with the patient at all times. If the patient stays home, she should not be left alone with the baby. Other people should stay with her, reassure her and help her take care of the baby. They should also ensure that she takes the medicines. With medication, the woman will completely recover.(1) DEALING WITH POST- PARTUM PSYCHOSIS: When psychotic symptoms appear in the post-natal period: - Talk to the husband and family members to arrange for the mother to be taken to the nearest health facility. The baby should only be separated for the mother if she has ideas to harm the baby or if she is violent or aggressive. The mother can continue to breast feed, even when she is receiving medicine for psychosis. Ensure that somebody is continuously available to ensure that the baby if taken care of until the mother can take full responsibility.(1) - Medications used to treat postpartum psychosis are the same of for other psychosis. Antipsychotic medications do pass into the mother's breast milk. Subsequently if the mother has been breastfeeding and continues to do so, the baby needs to be monitored for drowsiness or lethargic behavior, and prescribing the least amount of anti-psychotic medication in order for symptom reduction to occur is also crucial.(1) 6. References: 1. Pages 152-160 Mental Health in Primary Care training Manual for health workers Based on the WHO Primary Care Guidelines 2010 WHO 2. Pages 51-67 Professional Package For Medical Doctors for Mental Health Working in the BPHS in Afghanistan 2009 MoPH