PSYCHOSIS
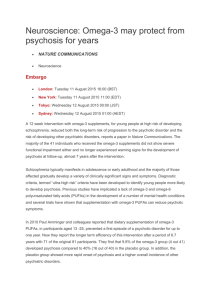
advertisement

PSYCHOSIS 2007 Summary Common psychiatric emergency may present to health services other than mental health team. Co-morbidities are common - increase with age First episodes best treated by specialist multidisciplinary teams delivering psychosocial interventions as well as drugs. Treatment achieves complete remission without relapse in 25% Use of low dose well tolerated atypical antipsychotic increases compliance and reduces future relapses Terminology Psychosis Positive symptoms Delusions, hallucinations, thought disorder Negative symptoms disorder of thinking and perception where typically patients do not ascribe their symptoms to a mental disorder A deficit state – what is not there Delusion False unshakeable belief out of keeping with the patients cultural educational and social background Terminology Hallucination A sensory perception experienced in the absence of a real stimulus Prodrome A definable period before the onset of psychotic symptoms during which functioning becomes impaired. Frequency 1 yr prevalence of non organic psychosis is 4.5/1000 community residents. Commonest age of presentation men < 30 women < 35 and people >60. Schizophrenia has a 1 yr prevalence of 3.3/1000 and life time morbidity of 7.2/1000 Psychotic symptoms have a 10.1% prevalence in non demented community > 85yrs Disorders in which psychotic symptoms occurs Schizophrenia Bipolar disorder Depression Substance misuse particularly cannabis Dementia Parkinson’s disease Other causes of psychosis Neurological Epilepsy Head injury CVA Infection Tumours Most causes of delirium Schizophrenia Incidence increased by Ethnic origin Migration Economic inequality in areas of high deprivation Diagnosis Diagnosis based on clinical findings No confirmatory tests Investigations might be required to rule out organic psychosis. Most information gained on first assessment Antipsychotic treatment can reduce strength of delusion Patients learn quickly that disclosing symptoms can lead to implications for drugs and liberty History Important to gain patients trust by Recording presenting complaints first Listening empathically Open questions How have things been for you lately Do you think something funny has been going on Have you heard unusual noises or voices Could someone be behind this History Enquire about 3 core mood symptoms Mood Energy Interest and pleasure Psychosis + major alterations in mood may indicate bipolar or schizoaffective disorders. Other aspects of history Symptoms in other systems especially neurological and endocrine Past psychiatric symptoms Past medical history and medication Family history of mental health and suicide Alcohol and substance misuse Allergies and adverse drug reactions Mental state examination Thorough documentation improves accuracy now and in later years General behaviour over arousal and hostility suggestive of positive symptoms. Irritability suggestive of elevated mood Catatonia and negativism rare Altered consciousness unusual in non organic psychosis Intermittent clouding suggests delirium Mental state examination General behaviour Disorganised speech indicates thought disorder Stilted and difficult conversation occurs with negative symptoms New words – neologisms best written down Random changes in conversation Fast or pressured speech suggests mania Mental State Examination Mood Depressed or elevated Affect Normal or flat Asses suicidal risk Cognitive impairment Grossly abnormal indicates learning disability or organic disorder Differential diagnosis Bipolar affective disorder Schizoaffective disorder Severe depression with psychotic features Delusional disorder Post traumatic stress disorder Obsessive compulsive disorder Schizotypal or paranoid personality disorder Aspergers ADHD Collateral history Important as family or friends may have noted strange behaviour May identify a prodrome Acute stress causing symptoms Gain information about premorbid personality Are beliefs culturally sanctioned and not delusional Positive psychotic symptoms Paranoid delusion Delusions of thought interference Delusions that others can hear read insert or steal one’s thoughts Passivity phenomena Any delusion that refers back to self Beliefs that others can control your will, limb movements, bodily functions or feelings. Thought echo Hearing own thoughts spoken out loud Positive psychotic symptoms Third person auditory hallucinations Voices speaking about the patient, running commentaries – common in non affective psychosis Hallucinations without affective content Second person auditory hallucinations Voices speaking to patient - may give commands Thought disorder Thought block, over inclusive thinking, difficulties in abstract thought – can’t explain proverbs Negative symptoms Apathy – disinterest blunted affect Emotional withdrawal – flat affect Odd or incongruous affect Smiling when recounting sad events Lack of attention to personal hygiene Poor rapport Reduced verbal and non verbal communication no eye contact Lack of spontaneity and flow of conversation Which treatment setting Best treated in least restrictive setting 70% of first episodes end up in hospital Older adults, adolescents and post partum women have complex needs and require admission to specialist units. Treatment Patients declining treatment need assessment under the mental health act Danger to self –suicide, unsafe behaviour, exploitation by others Danger to others – over arousal, potential to harm, risk of acting on delusion Special Groups Groups Older requiring special units Adults Adolescents Post- partum women Management Listen to patients relatives to catch relapse early and identify harmful components of ward environment Consult with early intervention team Identify and change environmental factors that perpetuate psychosis When new symptoms occur consider drug side effects Start psychosocial interventions early Test for substance misuse Management All antipsychotics cause Sedation Weight gain Impaired glucose tolerance – metabolic syndrome insulin resistance increased risk cardiovascular events measure waist circ. Lower seizure threshold ? Increased risk of thromboembolism Typical antipsychotic drugs Cause more Extrapyramidal sideffects Raised prolactin – sexual dysfunctions and galactorrhoea Anticholinergic sideffects – dry mouth tachycardia urinary obstruction Antiadrenergic – postural hypotension impotence Management Psychosocial for benefit CBT with strong evidence reduces impact of symptoms Family interventions prevent relapse Psycho educational interventions Supported employment Prognosis Relapse at one year Antipsychotic treatment but on psychosocial intervention 40% but 62% if in stressful environment 27% of patients with first psychotic episode 48%when 5th or more psychotic episode Prognosis Relapse at one year Placebo treatment no psychosocial intervention 61% with first psychotic episode 87% with 5th or more psychotic episodes Prognosis Relapse at one year Antipsychotic treatment with psychosocial interventions 19% with family education 20% with social skills training 0% with both interventions Prognosis Recovery at 15-25 years defined as global assessment of function >60 37.8% with schizophrenia 54.8% with other psychosis Maintenance After recovery Single antipsychotic for one year after first episode followed by gradual withdrawal in asymptomatic patients Multiple psychotic episodes require longer prophylaxsis There are high personal and health service costs for relapse so decisions need to be made carefully Risk of Relapse Indicators of relapse are Residual disability Family history of psychosis Current substance misuse