DOCX ENG
advertisement

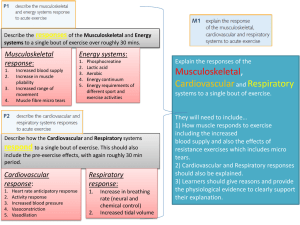
F-06 : cardiovascualr complications F- 06 : metabolic complications C- 05 : Hyperphospatemia Cinacalcet, Fibroblast Growth Factor-23, and Cardiovascular Disease in Hemodialysis. The Evaluation of Cinacalcet HCl Therapy to Lower Cardiovascular Events (EVOLVE) Trial Journal : Circulation Year : 2015 / Month : July Volume : 132 Pages : 27-39 DOI: 10.1161/CIRCULATIONAHA.114.013876 Sharon M. Moe, MD; Glenn M. Chertow, MD, MPH; Patrick S. Parfrey, MD; Yumi Kubo, MS; Geoffrey A. Block, MD;; Cinacalcet HCl Therapy to Lower Cardiovascular Events (EVOLVE) Trial Investigators* + Author Affiliations From Indiana University School of Medicine and Roudebush Veterans Administration Medical Center, Indianapolis (S.M.M.); Stanford University School of Medicine, Palo Alto, CA (G.M.C., K.W.M.); Health Sciences Center, St. John’s, NL, Canada (P.S.P.); Amgen Inc, Thousand Oaks, CA (Y.K., M.S., B.D., W.G.G.); Denver Nephrology, CO (G.A.B.); Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán, Mexico City, Mexico (R.C.-R.); Inserm Unit 1088, UFR Médecine/Pharmacie, Université de Picardie, Amiens, France (T.B.D.); University of Minnesota, Minneapolis (C.A.H.); Hôpital Manhès, Paris, France (G.M.L.); University College London, London, UK (D.C.W.); and Universitätsklinikum der RWTH Aachen, Germany (J.F.). Correspondence to Sharon M. Moe, MD, Indiana University School of Medicine, 950 W Walnut St, R2202, Indianapolis, IN 46202. E-mail smoe@iupui.edu ABSTRACT Background Patients with kidney disease have disordered bone and mineral metabolism, including elevated serum concentrations of fibroblast growth factor-23 (FGF23). These elevated concentrations are associated with cardiovascular and all-cause mortality. The objective was to determine the effects of the calcimimetic cinacalcet (versus placebo) on reducing serum FGF23 and whether changes in FGF23 are associated with death and cardiovascular events. Methods and Results This was a secondary analysis of a randomized clinical trial comparing cinacalcet to placebo in addition to conventional therapy (phosphate binders/vitamin D) in patients receiving hemodialysis with secondary hyperparathyroidism (intact parathyroid hormone ≥300 pg/mL). The primary study end point was time to death or a first nonfatal cardiovascular event (myocardial infarction, hospitalization for angina, heart failure, or a peripheral vascular event). This analysis included 2985 patients (77% of randomized) with serum samples at baseline and 2602 patients (67%) with samples at both baseline and week 20. The results demonstrated that a significantly larger proportion of patients randomized to cinacalcet had ≥30% (68% versus 28%) reductions in FGF23. Among patients randomized to cinacalcet, a ≥30% reduction in FGF23 between baseline and week 20 was associated with a nominally significant reduction in the primary composite end point (relative hazard, 0.82; 95% confidence interval, 0.69–0.98), cardiovascular mortality (relative hazard, 0.66; 95% confidence interval, 0.50–0.87), sudden cardiac death (relative hazard, 0.57; 95% confidence interval, 0.37–0.86), and heart failure (relative hazard, 0.69; 95% confidence interval, 0.48–0.99). Conclusions Treatment with cinacalcet significantly lowers serum FGF23. Treatment-induced reductions in serum FGF23 are associated with lower rates of cardiovascular death and major cardiovascular events. Clinical Trial Registration—URL: http://www.clinicaltrials.gov. Unique identifier: NCT00345839. Key Words: arrhythmias, cardiac ventricular remodeling calcium death, sudden, cardiac renal insufficiency, chronic COMMENTS Elevated levels of fibrobast growth factor 23 (FGF-23) are associated with cardiovascular and all-cause mortality in patients with kidney disease. A secondary analysis of the EVOLVE trial reports that cinacalcet-induced reductions in FGF-23 were associated with a reduced risk of cardiovascular events in patients with secondary hyperparathyroidism on dialysis. Disordered mineral metabolism, including secondary hyperparathyroidism and hyperphosphataemia, contributes to vascular calcification, which is associated with cardiovascular events and death. Fibroblast growth factor 23 (FGF-23)—an important hormonal regulator of circulating phosphate and calcitriol that is produced by osteocytes and osteoblasts—has also been implicated in poor cardiovascular disease (CVD) outcomes and increased all-cause mortality among patients with CKD and end-stage renal disease (ESRD).3 The question of whether reducing FGF-23 levels or inhibiting FGF-23 activity improves outcomes in patients with kidney disease has led to studies of various therapies that target FGF-23 levels, including phosphate binders, calcimimetics and FGF-23neutralization antibodies. Together with its co-receptor Klotho, FGF-23 induces renal phosphate excretion by reducing the activity of the sodium–phosphate cotransporter in the renal proximal tubule. FGF-23 is also a negative regulator of calcitriol and parathyroid hormone (PTH). Levels of FGF-23 increase early in the course of CKD5 (well before other abnormalities of mineral metabolism such as secondary hyperparathyroidism manifest) to compensate for phosphate retention in the setting of reduced glomerular filtration rate and nephron mass. As kidney function decreases, FGF-23 levels progressively rise and are highest among patients on dialysis. Large epidemiologic studies of CKD and ESRD populations show a strong relationship between high circulating FGF-23 levels and left ventricular hypertrophy (LVH) , CVD and all-cause mortality. This study shows that treatment with the calcimimetic cinacalcet significantly reduced serum FGF-23 levels in patients with secondary hyperparathyroidism on haemodialysis, and that these treatmentinduced reductions in FGF-23 levels were associated with reduced rates of cardiovascular death and major cardiovascular events, including heart failure and sudden cardiac death. This study provides the first evidence that lowering FGF-23 levels might improve clinical outcomes in patients on chronic dialysis, and provides proof-of-principle that. Pr. Jacques CHANARD Professor of Nephrology