Preparation
advertisement

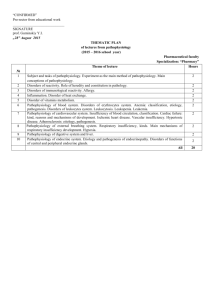
CAQ PAIN MANAGEMENT TOPICS LIST The following is list of topics to prepare for the Certificate of Added Qualifications (CAQ) in Pain Management. This list is extensive but in no way exclusive. The information can be found in most textbooks and updated information from published publications. PAIN PATHWAYS: AN OVERVIEW OF ANATOMY AND PHYSIOLOGY o Pain Pathways and Mechanisms o Nociceptors o Dorsal Horn Mechanisms o Ascending Pathways o Descending Control o Deafferentation Pain o Sympathetically Mediated Pain Psychological Aspects of Pain o Definition of Pain o Conceptual Model of Pain o Chronic Pain o Psychogenic Pain o o MANAGEMENT OF COMMON NONMALIGNANT PAIN SYNDROMES PATIENT EVALUATION Collection of History Data o Demographics o Pain History Physical Examination of the Pain Patient o General Principles Psychological Evaluation of the Chronic Pain Patient o Focus of Psychological Examination o Consequences of Pain o Patient Beliefs Related to Pain o Mood and Motivation o Psychological Tests Diagnostic and Prognostic Tests and Nerve Blocks o Evaluation of Coagulation Status o Diagnosis of Pain (plain radiographs, computed tomography, myelography, MRI, ra1 dionuclide bone imaging, EMG, thermography) Determining Pain Pathways (central vs. peripheral mechanism, somatic vs. visceral pathway, sympathetic vs. somatic) Determining Pain Mechanisms Prognostic Blocks Myofascial Pain o Definition o Etiology o Signs and Symptoms o Lab Findings o Clinical Course o Treatment (trigger point injections, psychological intervention, physical therapy, adjunct therapy Radiculopathy o Treatment of Discogenic Pain o Acute Lumbar Radiculopathy (signs and symptoms, laboratory, treatment objectives, conservative management, epidural steroid injections, physical therapy, surgery) o Chronic Lumbar Radiculopathy (epidural steroids, TENS, pharmacological management, CNS stimulation) o Cervical Radiculopathy (signs and symptoms, treatment objectives, epidural steroids, paravertebral blocks) Sympathetically Mediated Pain o Definitions (causalgia, reflex sympathetic dystrophy) o Mechanisms o Clinical Course o Clinical Findings (history, physical findings) o Special Studies (sweat test, skin conductance, plane radiographs, three-phase bone scan, differential block) o Therapy (physical therapy, stellate ganglion block, lumbar sympathetic block, pharmacological management) Herpes Zoster and Postherpetic Neuralgia o Definition o Epidemiology o Clinical Picture o Treatment of Acute Herpes Zoster o Treatment of Postherpetic Neuralgia Peripheral Neuralgia o Symptoms (dysthesias, neuralgias, polyneuropathies) o Laboratory Tests/Physical Examination o Management (pharmacological, physical therapy, surgery Postamputation Pain o Pathophysiology o Symptoms (stump pain, phantom limb sensation, phantom pain) o Goals of therapy o Treatment Options (pharmacological, surgical, sympathectomy) Joint Pathology of the Spine o Facet Joint Pain (symptoms, clinical findings, symptomatology, treatment options) o Sacroiliac Joint Pain (symptoms, pathology, diagnosis, treatment and management) Pancreatitis o Clinical Features o Pathogenesis o Diagnosis o Differential Diagnosis o Treatment Approach (objectives, for acute pancreatitis, for chronic pancreatitis) Facial Pain o Examination (anatomical, sensory distribution, cranial nerve function, occlusal analysis, joint motion, soft tissue, psychological factors) o Temporomandibular Joint Syndromes (symptoms, pathophysiology, treatment objectives, management) o Neuromas (symptoms, pathophysiology, treatment objectives, management) o Trigeminal Neuralgia (symptoms, pathophysiology, treatment objectives, management) o Atypical Facial Pain (symptoms, pathophysiology, treatment objectives, management) 2 Headache o History o Vascular Headache (definitions, pathophysiology, signs & symptoms, laboratory, treatment objectives, management) o Cluster Headache (characterization, pathophysiology, signs & symptoms, management) o Paroxysmal Hemicrania – Sjaastad’s Syndrome (characterization, pathophysiology, signs & symptoms, management) o Mixed Headache o Musculogenic Headache (characterization, pathophysiology, signs & symptoms, management) o Occiptial Neuralgia (characterization, pathophysiology, signs & symptoms, management) o Cervicogenic Headache (characterization, pathophysiology, management) o Post Dural Puncture Cephalgia (symptoms, treatment objectives, management) Chronic Pelvic Pain o Etiology o Characteristics o Evaluation (history, signs & symptoms, physical findings, psychological aspects) o Treatment Objectives o Management (pudendal block, paracervical block, caudal or epidural block, pharmacological) Postoperative Pain o Acute Pain in the Chronic Pain Patient o Pharmacological Considerations o Regional Blocks o Psychological Aspects Central and Post-Spinal Cord Injury Pain o Classification o Treatment Options (drug therapy, psychological support, regional blocks, sympathectomy) o Management of Patient with Spinal Cord Injury (classification of pain, treatment of post-SCI pain syndromes) Psychological Treatment of Chronic Pain o Patient Education o Cognitive-Behavioral Therapy o Biofeedback o Relaxation Therapy o Group Therapy MANAGEMENT OF COMMON CANCER PAIN SYNDROMES Classification and Assessment of Cancer Pain o Cancer Pain Syndromes (somatic, visceral, deafferentation) o Pain Assessment Pharmacological Treatment of Cancer Pain o General Principles (non-opioid analgesics, opioid analgesics) o Analgesic Management o Adjuvant Drugs Behavioral Treatment of Cancer Pain o Psychological Factors o Behavioral Therapy o Psychotherapy Non-neurolytic Nerve Blocks for Cancer Pain o Myofascial Pain o Reflex Sympathetic Dystrophy o Neuropathic Pain o Acute Herpes Zoster Intraspinal Narcotics for Cancer Pain o Drug Choices o Technique o Tolerance Electrical Stimulation for Cancer Pain Management o Spinal Cord Stimulation o TENS Neurolytic Nerve Blocks for Cancer Pain o Pharmacology of Neurolytic Agents o Complications o Patient Selection o Techniques Radiation Therapy in Cancer Pain Management o General Considerations o Clinical Applications Chemotherapy and Hormonal Therapy for Cancer Pain o General Considerations o Clinical Applications o Patient Selection o Adverse Effects Neurosurgical Management of Cancer Pain o General Principles (multidisciplinary approach, prognostic blocks) o Potential Techniques (spinal thalamic tractomy, percutaneous cervical cordotomy, commissural myelotomy, cingulotomy, pituitary ablation, midbrain stimulation) 3