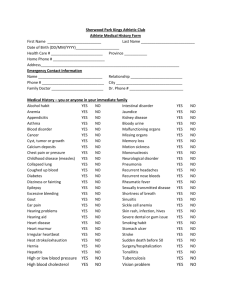
Supplementary Table 1: Negative investigations in 17 patients with
advertisement

Supplementary Table 1: Negative investigations in 17 patients with basal ganglia encephalitis. All investigations on serum or plasma unless stated. Biochemical Number Autoimmune or infectious Urine amino acids 17 Antinuclear antibody 15 Urine organic acids 17 Anti-ds DNA Ab 9 Urine Glycosaminoglycan 9 Extractable nuclear antigen antibody 5 Ammonia lactate 9 Anti-cardiolipin Ab 3 Copper + caeruloplasmin 9 ANCA 3 CSF Neurotransmitters 8 Anti-thyroid antibodies 2 Biotinidase 6 Coeliac antibodies 2 White cell enzymes 5 Very long chain fatty acids 5 CSF herpes simplex PCR 14 B12 folate 5 CSF enterovirus PCR 8 Transferin isoforms 4 CSF mycobacteria PCR 4 Thyroid function 4 CSF Varicella zoster PCR 3 Plasma amino acids 3 CSF Cytomegalovirus PCR 2 Carnitine 3 CSF Epstein Barr virus PCR 2 Urine toxicology 3 CSF fungal stain 2 Urine VMA 3 CSF JC virus PCR 1 Heavy metals 3 CSF measles IgG 1 ACE 2 Complement 2 Mycoplasma IgM 12 Urate 2 Epstein Barr virus IgM 12 Urine Porphyrins 2 Anti-Streptolysin-O titre 10 Malaria film 2 Varicella zoster IgM 6 Lipids 2 Human Immunodeficiency virus IgG 6 Alpha fetoprotein 2 Cytomegalovirus IgM 6 Herpes Simplex virus IgM 5 Toxoplasma IgM 5 Measles IgM 4 Lyme serology 3 Influenza IgG 3 Enterovirus IgM 3 Rubella IgM 3 Human Herpes virus 6 IgM 3 Hepatitis serology 2 Parvovirus, serology, mumps, Q fever, Cat stratch 1 Arbovirus, Japanese B, Flavivirus, Coxiella, Legionella, Chylamydia Nasopharyngeal aspirate for 7 respiratory virus panel Throat swab IgG = immunoglobulin G IgM = immunoglobulin M 6 Supplementary Table 2: Clinical details and demographics of controls (n = 67) Control Healthy Other First episode of Viral Anti- Group control Neurological demyelination encephalitis NMDAR (HC) disorders (OND) (DEM) (V ENC) ‡ encephalitis (NMDAR ENC) Number 18 22 8 11 8 Males 10 12 5 8 2 Mean, 11, 11 8.4, 8 9.25, 9.9 4.8, 3.2 6.5, 6.5 9-13 1-15 1.8-14.6 0.5-14 3-13 Healthy Basal Acute disseminated Enterovirus Positive children metabolic or genetic encephalomyelitis CSF pcr (n = serum (and disease#, or clinically isolated 6) CSF) anti- syndrome* Herpes NMDAR neurodegeneration, Simplex CSF antibodies¶ developmental pcr (n = 4) disorders Varicella median age (yrs) Age range (yrs) Details ganglia epilepsy, stroke, Zoster CSF pcr (n = 1) # Basal ganglia controls included Wilson’s disease, Leigh disease, Glutaric aciduria type 1, basal ganglia stroke, Huntington disease * 4/8 children with DEM were positive for anti-myelin oligodendrocyte glycoprotein (MOG) antibodies (Brilot et al., 2009). ‡ Viral encephalitis confirmed aetiology using CSF PCR (Granerod et al., 2010). ¶ Clinical phenotype and investigation as described (Dale et al., 2009). Supplementary Table 3: Ancillary tests, treatment, and outcome in 12 anti-D2R antibody positive basal ganglia encephalitis children Characteristic Number Brain MRI Total abnormal 6/12 Putamen lesions (bilateral) 6/12 Caudate lesions (bilateral) 5/12 Globus Pallidus lesions (bilateral) 3/12 Midbrain, cerebral peduncle 3/12 Pons, frontal cortex, thalamus 1/10 each Cerebrospinal fluid Total with abnormal findings 9/12 Lymphocyte pleocytosis (>5 cells/mm3)* 3/12 Protein (>0.4 mg/dl) 6/12 Intrathecal oligoclonal bands 4/10 Mirrored oligoclonal bands 3/10 Electroencephalography Normal 5/10 Slowing 5/10 Epileptic activity 0/10 Treatment IVMP, then oral prednisolone ‡ 5/12 IVMP, then oral prednisolone, IVIG¶ ♯ 2/12 Nil 5/12 Outcome Length of follow-up, mean, median (range) years 5.3, 5.25 (1-10) Full recovery 5/12 Dystonia 3/12 Motor tics 1/12 Cognitive disorder 5/12 ADD† 4/12 Psychosis 2/12 OCD, ODD, ASD, anxiety§ 1/12 each * CSF Lymphocyte range 0-30 cells/mm3, median 1 cell/mm3 ‡ IVMP= Intravenous methyl-prednisolone ¶IVIG= Intravenous immunoglobulin ♯ = complete treatment: 30mg/kg/day of Methylprednisolone for three days followed by three months of tapered oral prednisolone (starting 2mg/kg/day for one month). In addition, patients were given 2g/kg of intravenous immunoglobulin at the same time as the intravenous steroid. †ADD = Attention deficit disorder §OCD = Obsessive compulsive disorder, ODD= Oppositional defiant disorder, ASD = autistic spectrum disorder Supplementary Table 4: Clinical features, acute Magnetic resonance imaging features and outcome of basal ganglia encephalitis patients with anti-D2R antibodies Age Movement Psychiatric sex disorder Other MRI and Outcome lesions cognitive symptoms 1.6 Chorea Agitation F Insomnia Normal Hypotonia Loss Relapse (2mth) Normal (1.5 yr) ** of ambulation 3.5 Chorea Personality Ataxia F Ocular flutter change tremor Normal Relapse (3m, 12m) Normal (2 yr) ** cognitive decline 3.5 Parkinsonism M Dystonia Agitation Lethargy Caudate Coordination disorder Slurred speech Putamen Anxiety Encephalopathy Cognitive disorder, mild (8 yr) 4M Dystonia - Dystonic Encephalopathy Caudate, Seizure putamen, tremor 5F Normal (1 yr) * frontal cortex Parkinsonism Emotional Insomnia Normal ADD Dystonia lability Confusion ODD Pyramidal Rigid behaviours weakness Hemidystonia (5 yr) * 5M 6F Parkinsonism Parkinsonism - - Somnolence Putamen Normal (10 yr) Ophthalmoplegia Thalamus Pyramidal Midbrain weakness Pons Lethargy Caudate Motor tics Ataxia Putamen ADD Cerebellar signs Globus Rigid thinking (4 yr) Pallidus 7F Chorea Aggression Encephalopathy Caudate Inattentive ADD Seizure Putamen Impulsive Globus Anxiety Pallidus Cognitive Cerebral mild (8 yr) * disorder, peduncle 9F Hemi- Hallucinations Ophthalmoplegia Caudate Relapse (8 yr) dystonia Disinhibition Mutism Putamen Dystonia Hemi-chorea Compulsive Hiccough Globus ADD OGC touching Pallidus Autistic Cerebral disorder peduncle OCD spectrum Bipolar disorder Cognitive deficit (9 yr) * 14 Dystonia Agitation M Encephalopathy Normal Dystonia Cardiac Cognitive arrhythmia mild disorder, (5.5 yr) * 15 Dystonia Psychosis Mutism M (orofacial) Paranoia Poor eye contact Normal Psychosis (9yr) * OGC Agitation Compulsive touching 15 Parkinsonism Psychosis Somnolence M OGC Paranoia Hiccough Anxiety, Pupillary agitation dilatation Normal Normal (2 yr) *Patients receiving intraveneous Methyl prednisolone then oral prednisolone for 4 or more weeks in acute phase. **Patients receiving intravenous Methyl prednisolone and oral prednisolone for 4 or more weeks, and IVIG ADD = Attention deficit disorder, ODD = oppositional defiant disorder, OCD = obsessive-compulsive disorder, OGC = oculogyric crises Supplementary Table 5: Clinical comparison of anti-D2R antibody-positive (n = 10) and –negative Sydenham chorea patients (n = 20) Characteristic Anti-D2R Anti-D2R antibody- antibody- positive (n = negative (n = 10) 20) Female sex 9/10 15/20 Age mean (range) 8.4 (2-13) 11.9 (7-16) Non-white 5/10 6/20 Infection 7/10 12/20 Positive ASOT >200 IU/ml 10/10 18/20 Chorea 8/10 14/20 Hemichorea 2/10 6/20 Any psychiatric symptoms 7/10 16/20 Emotional lability, anxiety 7/10 14/20 Personality change 6/10 14/20 Attention deficit hyperactivity disorder 2/10 4/20 Demographics Prodromal symptoms Movement disorder Psychiatric symptoms Generalised anxiety disorder 0/10 5/20 Dysarthria 6/10 13/20 Carditis 6/10 13/20 Arthritis or arthralgia 5/10 8/20 Fever 1/10 4/20 Other ASOT = anti-Streptococcal-O titre Supplementary figure legends: Supplementary Fig. 1: Basal ganglia encephalitis is not associated with anti-D3R, anti-D1R, and anti-DAT antibody. Anti-human surface D3R (A), D1R (B) and DAT (C) IgG antibody were detected using flow cytometry cell-based assays. Patients with Basal ganglia encephalitis do not have anti-D3R, anti-D1R, or anti-DAT antibody. 15/17 (D3R and D1R) and 14/17 (DAT) basal ganglia encephalitis sera were available for testing. Representative dot plots out of three experiments are shown. Supplementary Fig. 2: Anti-D2R antibody-positive encephalitis sera do not bind hemagglutinin. Because the extracellular N-terminus of D2R cDNA is tagged with the human influenza hemagglutinin (HA) tag, we controlled that anti-D2R IgG antibody detected in basal ganglia encephalitis (BG ENC) did not bind to the hemagglutinin tag using hemagglutinin-D5R and hemagglutinin-syntaxin 4. Extracellular N-terminal hemagglutinin-D5R (A) and extracellular C-terminal hemagglutinin-syntaxin 4 was expressed at the surface HEK293 cells (C), and we performed cell-based assays. Threshold was defined as mean of healthy control + 3SD (dotted line on graph). (B) Anti-surface human hemagglutinin-D5R antibody were detected in 0/67 controls and 0/17 basal ganglia encephalitis (BG ENC) sera. (D) Anti-surface rat hemagglutinin syntaxin-4 IgG antibody was detected in 0/13 healthy control (HC), 0/8 anti-NMethyl D-Aspartate Receptor encephalitis (NMDAR ENC), and 0/17 basal ganglia encephalitis sera. Representative dot plots out of three experiments are shown. (E) Representative flow cytometry histograms are shown for an anti-D2R antibody positive basal ganglia encephalitis serum. MFI values are noted in legend. Supplementary Fig. 3: Acute (A) and convalescent (C) anti-D2R antibody in three basal ganglia encephalitis patients. Patients A and B were diagnosed retrospectively with anti-D2R antibody-positive encephalitis, whereas patient C was diagnosed prospectively. Patient A, a 5 year old female presented with encephalitis, dystoniaparkinsonism, and confusion. Her MRI was normal and she was treated with oral prednisolone 2mg/kg for 2 weeks then a 6 week taper. The patient was reported to have made little improvement at annual reviews, and at 5 year follow-up she has residual hemidystonia, attention deficit disorder, rigid behaviours, and her anti-D2R antibodies remain elevated. Patient B, a 3 year old male presented with encephalitis, encephalopathy, dystonia-parkinsonism, and agitation. His MRI showed caudate and putamen lesions. He was treated with intravenous methylprednisolone 30mg/kg for 3 days then oral prednisolone 2mg/kg for 2 weeks, then an 8 week steroid taper. The patient was reported to have made little improvement at annual reviews, and at 8 year follow-up he has residual coordination disorder, anxiety, and mild learning difficulties, and his anti-D2R antibodies remain elevated. Patient C, a 3 year old female presented with encephalitis with chorea, ataxia, ocular flutter, developmental regression, and two relapses in the first 12 months. Her MRI was normal. She was given 2g/kg of intravenous immunoglobulin monthly for three months. She was also given oral prednisolone 2mg/kg/day for one month and remains on 1mg/kg prednisolone on alternate days. One year after starting treatment, her chorea and ataxia have resolved, she has made significant developmental gains, and her development is now normal. Her anti-D2R antibody is now within the healthy control range (below threshold of positivity). Dotted lines on graphs represent the positivity threshold (obtained with 24 HC samples). P: prednisolone; IVIG: intravenous immunoglobulin. Representative dot plot out of three experiments is shown. Supplementary Material: Brief case histories of anti-D2R antibody-positive Tourette syndrome patients Case 1: A male Caucasian patient whose father had Tourette syndrome and attention deficit hyperactivity disorder presented with his tic disorder at 5 years of age. At the time of serum testing (15 years), he had severe Tourette syndrome plus comorbid attention deficit hyperactivity disorder, oppositional defiant disorder, obsessive compulsive disorder, generalised anxiety disorder and depression, and was severely impaired despite multiple medication trials. His anti-Streptolysin-O titre (ASOT) at time of serum testing was elevated at 400 IU/ml, but there was never any infectionassociated exacerbations during his disease course. Case 2: A male Asian patient with no family history of note presented at 6 years of age with tic disorder. At the time of serum testing (7 years of age) he had motor and vocal tics for more than 12 months, but had no associated comorbidity. His course waxed and waned but his impairment did not require medical treatment. His ASOT was negative at 50 IU/ml, and there has never been any infection-associated exacerbations during his disease course. Case 3: A female Caucasian patient whose mother has longstanding throat clearing presented at 7 years of age with tic disorder. The patient has had motor and vocal tics for 8 years, and her course has relapsed and remitted in a more exaggerated way than typical Tourette syndrome, but there has never been a deterioration associated with infection. At the time of serum testing (15 years old), she still has Tourette syndrome, but no associated comorbidity. Her ASOT at the time of serum testing was negative at 55 IU/ml. Case 4: A female Caucasian patient whose sister has alopecia and father has obsessive-compulsive disorder presented at 4 years of age with tic disorder. At the time of serum testing (8 years), she had Tourette syndrome, generalised anxiety disorder, separation anxiety, and obsessive compulsive behaviour. She has had a predisposition to Streptococcal infections, but there have not been any clear infectionassociated exacerbations. Her ASOT at the time of serum testing was elevated at 455 IU/ml.