Therapeutics – Viral Hepatitis
advertisement

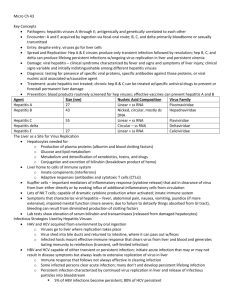
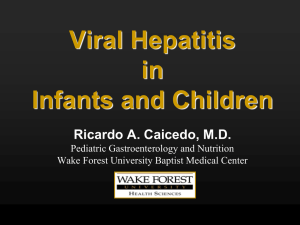
VIRAL HEPATITIS Hepatitis is an inflammation of the liver. The major hepatotropic viruses responsible for viral hepatitis are Hepatitis A Hepatitis B Hepatitis C Hepatitis D Hepatitis E Hepatitis A and E are transmitted by feco-oral route and B, C, and D parenterally. HEPATITIS A Hepatitis A virus (HAV) or infectious hepatitis is a self limiting and acute viral infection of the liver posing a serious health risk world wide. The infection is rarely fatal. Etiology : Hepatitis A virus is a RNA virus belonging to the genus hepato virus of picorna viridae family. Humans are the only known reservoirs for the virus. The virus is stable in the environment for atleast a month and requires heating foods to a minimum of 85° c for 1 minute. Pathophysiology : HAV infection is usually acute , self limiting and confers life long immunity. HAV‘s life cycle begins with Ingestion of the virus and continues Absorption in the stomach or small intestine allows entry into the circulation and uptake by liver. Replication of virus occurs with in hepatocytes and gastro intestinal epithelial cells. New virus particles are released into the blood and secreted into bile by liver. The virus is then reabsorbed to continue its cycle or excreted in the stool. The enterohepatic cycle continues until inerrupted by antibody neutralisation. On biopsy, acute hepatitis is marked by hepatocellular degeneration, inflammatory infiltrate and hepatocyte regeneration. Cytolytic T cells mediate hepatocyte lysis to eradicate the virus and mark the cellular immune response with raising hepatic enzyme levels. Clinical presentation: The incubation period of HAV is 28 days. The priecteric phase brings nonspecific influenza like symptoms consisting of anorexia, nausea, fatigue and malaise. Abrupt onset of all these symptoms and also fever, headache and right upper quadrant abdominal pain with acute illness. Icteric hepatitis is generally accompanied by dark urine, acholic stools and worsening of systemic symptoms. Pruritis. There are no specific symptoms unique to HAV. Physical examination: Icteric sclera, skin and secretions. Mild weight loss of 2-5 kg. Hepatomegaly. Laboratory investigations: Positive serum immunoglobulin M anti-hepatitis A virus. Mild elevations of serum bilirubin, γ-globulin and hepatic transaminase(ALT and AST). Diagnosis: diagnosis is based on clinical criteria of an acute onset of fatigue, abdominal pain, loss of appetite, intermittent nausea and vomiting, jaundice or elevated serum aminotransferase levels, and serologic testing for IgM and anti-HAV. Treatment: The goals of therapy: Complete clinical resolution Reduce complications Normalisation of liver functions Reducing infectivity and transmission. No specific treatment options exist for HAV infections, instead patient should receive general supportive care. In patients who develop liver failure, transplant is the only option. Prevention and prophylaxis are the key to managing the virus. Immunoglobulin is used for pre and post exposure prophylaxis and offers passive immunity. Active immunity is achieved through vaccination. Children often serve as reservoirs of the disease, vaccine programs have targeted children as the most effective means to control HAV. Vaccines to prevent Hepatitis: Two inactivated virus vaccines are concurrently licenced in the united states. Havrix and vaqta. Both are available for adult and paediatric use. The differences in the two vaccines are in the use of preservatives and in expression of antigen content. Recommended Dosing of Havrix and Vaqta VACCINE Havrix AGE 1-18 DOSE 720 ELISA units NO. OF DOSES 2 SCHEDULE (mo) 0, 6-12 Vaqta ≥19 1-18 1,440 ELISA units 25 units 2 2 0, 6-12 0, 6-12 ≥19 50 units 2 0, 6-12 The most common side effects of the vaccines include soreness and warmth at the injection site, headache, malaise, and pain. Reported serious adverse effects include anaphylaxis, multiple sclerosis, encephalopathy etc,. Immunoglobulin Ig is preferred for children < 12 months of age and for post exposure prophylaxis in patients aged > 40 years, patients with chronic liver disease and persons allergic to any part of the vaccine. Ig is available both as an IV and IM injection but for HAV exposure, only IM is used. For post exposure prophylaxis and for short term preexposure coverage of <3 months, a single dose of 0.02 ml/kg is given intramuscularly. For longterm preexposure prohylaxis of ≤5 months, a single dose of 0.06 mL/kg is used. HEPATITIS B Chronic infection with HBV is a major public health issue as it serves as a reservoir for continued HBV transmission and poses a significant risk of death resulting from liver disease. The HBV is a DNA virus of the family Hepadnaviridae. The acute infection is often asymptomatic particularly when aquired at birth. Chronic hepatitis associated with elevated serum transaminases, may occur and can lead to cirrhosis, usually after decades of infection. Vertical transmission from mother to child in the perinatal period is the most common cause of infection world wide. Upon infection, replication of the virus begins by attachment of the virion to the hepatocyte cell surface receptors. The particles are transported to the nucleus where the DNA is converted into closed, closed circular DNA that serves as a template for pregenomic RNA. Viral RNA is then transcribed and transported back to the cytoplasm where it can alternatively serve as a reservoir for future viral templates or bud into intracellular membrane with the viral envelope proteins and infect other cells. The viral genome has four reading frames coding for various protiens and enzymes required for viral replication and spread. Several of these proteins are used diagnostically. The HBsAg is the most abundant of the three surface antigens and is detectable at the onset of clinical symptoms. HBV itself doesnot seem to be pathogenic to cells, rather it is thought that the immune response to the virus. Cirrhosis: Cirrhosis results as the liver attempts to regenerate while in an environment of persistent inflammation. Like in other viral hepatitis induced cirrhosis, continued alcohol consumption exacerbates hepatocellular damage. Most patients with compensated cirrhosis are either asymptomatic or have mild symptoms of epigastric pain and dyspepsia. During cirrhosis, the liver enters a cycle of ongoing liver damage , fibrosis, and attempts at regeneration. Typically, the initial clinical findings of decompensated cirrhosis are ascites, jaundice, variceal bleed, encephalopathy or a combination of symptoms. Damage is irreversible. Hepatocellular carcinoma: HBV is a known risk factor for the development of HCC. HCC develops after years of inflammatory processes provoked by ongoing HBV infection. Development of HCC can be insidious, occurring in the absence of cirrhosis or the presence of clinically silent compensated cirrhosis. HBV infection is associated with worse survival rate. Several factors influence the development of HCC, as well as predict survival. Younger age and maintainence of liver function as evidenced by laboratory findings are the additional predictors of survival. Clinical presentation of Hepatitis B: Signs and symptoms: Easy fatigability, anxiety, anorexia and malaise. Ascites, jaundice, variceal bleeding, and hepatic encephalopathy can manifest with liver decomposition Hepatic encephalopathy is associated with hyperexcitability, confusion, obtundation and coma. Vomiting and seizures. Physical examination: Icteric sclera, skin, and secretions. Decreased bowel sounds, and detectable fluid wave. Asterixis Spider angiomata. Laboratory tests: Presence of hepatitis B surface antigen >6 months Intermittent elevation of hepatic transaminase Liver biopsies for pathologic classification as chronic persistant or active hepatitis or cirrhosis. Treatment: Non pharmacologic therapy All chronic HBV patients should be counseled on preventing disease transmission. Sexual and household contacts should be vaccinated. To minimize further liver damage, all chronic HBV patients should avoid alcohol and be immunized against HBV. Pharmacologic therapy: 1) INTERFERON It was the first approved therapy of HBV and improves long term outcomes and survival. Acting as a host cytokine, it has antiviral, antiproliferative, and immunomodulatory effects in chronic HBV. Seroconversion can occur during or after the therapy is complete. Additional benefits of interferon based therapy is reduction in cirrhosis, HCC and death. Pegylated interferon therapy is benificial when compared with conventional interferon therapy. 2) LAMIVUDINE It is a nucleoside analogue having antiviral activity against both HIV and HBV. Dosed at 100 mg daily in adults. In both HBeAg positive and negative patients, lamivudine demonstrates profound viral supression. HBV DNA serum levels are undetectable in 90% of lamivudine treated patients after 4 weeks. Advantage of lamivudine therapy include its safety profile, patient tolerability and the convenience of oral tablet. Lamivudine is safely used in immunosupressed and cirrhotic patients. The prognosis is poor for patients who have developed resistance. 3) ADEFOVIR Adefovir dipivoxil is an acyclic nucleotide analog of adenosine monophosphate. The drug acts by inhibiting HBV DNA polymerase. Dosed at 10 mg daily for 1 year in adults. 4) ENTECAVIR Entecavir is a guanosine nucleotide analog by inhibiting HBV polymerase. It is more potent than lamivudine and adifovir in supressing serum HBV DNA levels and is effective in lamivudine resistant HBV. Dosed at 0.5 mg daily for adults. 5) TELBIVUDINE Telbivudine is a HBV specific nucleoside analog that acts as a competitive inhibitor of viral reverse transcriptase and DNA polymerase. The drug inhibits HBV DNA synthesis. 6) TENOFOVIR Tenofovir is a nucleotide analog first approved for use in HIV and later for HBV. It is available either as a single agent oral tablet or as a combination therapy with emtricitabine. Dosed at 300 mg. HEPATITIS C HCV is the most common blood borne pathogen. HCV is a single stranded RNA virus of the family flaviviridae. The virus replicates with in hepatocytes. HCV replicates copiously with an estimated serum half life of 2-3 hours. The result is a proliferate, persistantly mutating virus posing an immense challenge for immune mediated control. Pathophysiology: During the early phases of the infection, natural killer cells are activated as HCV RNA levels rapidly rise. The eradication of HCV by cytotoxic T lymphocytes may occur either as a result of induced apoptosis by infected hepatocytes or by the release of interferon to stifle viral replication. The extent of hepatocyte apoptosis may correlate with the course of the disease. Liver damage and HCC are associated with high levels of hepatocyte apoptosis. Clinical presentation: In an acute HCV infection, most patients are asymptomatic and undiagnosed. HCV RNA is detectable within 1 to 2 weeks of exposure and levels rise quickly during the initial weeks. Symptoms include fatigue, anorexia, weakness, jaundice, abdominal pain or dark urine. Additional symptoms include right upper quandrant pain, nausea or poor appetite. On physical examination, hepatomegaly is usually seen. Treatment: The current standard of care for chronic HCV patients is a combination therapy of a once weekly injection of peginterferon and a daily oral dose of ribavirin. 1) Interferon: Interferon α is used in the treatment of HCV. The addition of pegylated moiety to interferon improved the pharmacokinetic profile of the drug to reduce injection frequency from three times to once a week. Two peginterferons are available, peginterferon α2a (pegasys)and peginterferon α2b(PEG-Intron). Pegasys is dosed at 180 mcg/week subcutaneously. PEG-Intron is dosed at 1.5 mcg/kg /wk subcutaneously. 2) RIBAVIRIN Ribavirin when given in combination with interferon increases SVR rates. Side effects of therapy are extensive and major obstacle. They include fatigue, fever, headache, arthralgia, nausea, anorexia, rigors, myalgia.,etc