CMS Immunology Cancer notes BETA
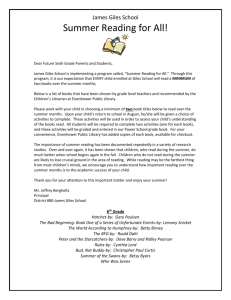
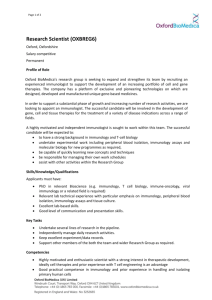
advertisement

Giles Kisby GE Y1 CMS Immunology Cancer CMS, Immunology and Cancer: Spring Term: LECTURES: CMS: Revision lectures: 06/03/14: - - - - TSGs best refer to direct cell cycle modulators but definitely can also be used to refer to other proteins such as those involved in dna repair and in apoptosis regulation Replication origin licensing occurs in interphase (specifically in G1) Most important: o Cdk2 binds cyclin E for G1 to S entry o MPF = (Cdk1 binds cyclinB = mitotic cyclin) for G2 to mitosis entry No DNA damage influence in the successful progression through the spindle assembly checkpoint; is just concerned with proper kinetochore:spindle attachments Cdk’s are not detectable in early G1 Nb APC/C: cdc20 and MPF/cdc25 pathways CAK, Wee1 and cdc25 all occur per successful MPF downstream signalling Chromatids move apart during anaphase; homologous chromosomes do not move apart (firstly because is a splitting event and secondly division is in series so each daughter inherits a copy of each homologue) APC/C:cdc20 targets securing for degradation and degrades cyclin B Is actin NOT tubulin in the contractile ring of cytokinesis Tubulin is involved in all chromosome movements including those during prophase Cdk1 functions: o To phosphorylate nuclear lamins so as to help degrade the nuclear membrane for mitosis o To phosphorylate histones so as to induce the relevant transcription for mitosis Rb is phosphorylated by Cdk2 during the G1/S phase transition o It is thought that cyclin D–cdk4/6 phosphorylates Rb early in G1, cyclin E–cdk2 phosphorylates the protein near the end of G1, and cyclin A–cdk2 may maintain phosphorylation of Rb during S phase 1 Giles Kisby GE Y1 CMS Immunology Cancer - Cdks are serine / threonine kinases P21 is an example of a Cdk inhibitor that is not a kinase Chk1 is a kinase Securin is degraded at anaphase Cdc25 is an example of a phosphatase that promotes mitosis - BRAF mutant presence is a positive indicator for the use of BRAF inhibitor treatment (RE skin cancer melanomas) but should be aware that if mutation not present the treatment would be detrimental because paradoxically would stimulate the downstream MAPK pathway (through unknown mech of the inhibitor; due to the crossover of pathways etc) Cytotoxics are used in the treatment of breast cancer Her 2 receptor genes become amplified (NOT mutated) in breast cancer treated with Herceptin Her2+ (breast cancer) and BRAF+ (melanoma) are indicators of worse prognosis despite the added drugs that can be used to treat the conditions - - - BRaf is a mutated form of Raf that is overactive! Imatinib = a tyrosine-kinase inhibitor used in the treatment of chronic myelogenous leukemia (CML) __imab = mAb; will not cross BBB __inib = small tyrosine kinase inhibitor; will cross the BBB, eg imatinib To treat ER+ breast cancer: aromatase inhibitor, remove ovarys, tamoxifen, goserelin [gonadotropin releasing hormone superagonist (GnRH agonist)], paclitaxel adjunctive therapy o initial increase in luteinizing hormone production, before the receptors are desensitised and hormonal production is inhibited. Breast cancer often metastasises to bone Breslow thickness as a diagnostic tool ER+ breast cancer is a case most often seen in older women [“defective signalling at the receptor has just built up through time”] PI3K mutations often occur in breast cancers Hormone production is generally a sign of benign tumours - Most common breast cancer is invasive - - ductal carcinoma Revision lectures: 11/03/14: [inc practice paper] General notes: - Note that some of the questions here are debateable / incorrect / would be taken out of an exam on review (though have all been used!) so don’t worry too much if seem wrong 2 Giles Kisby - GE Y1 CMS Immunology Cancer She says that certain topics are disproportionately represented in the exam: cell cycle [cyclins etc and when they act], cell apoptosis, genetics Aside: for regulatory the following is order of exam presence: Pharm > Neuro > Reprod = endo > musculoskeletal > psychology and gerontology - Exam: 70 SBA, 4 EMQ sets, 5 SAQ sets - Write in full sentences for SAQs; eg if asks what demonstrates a certain thing then finish with “…and this therefore means/demonstrates xyz” o Eg Is the womans unborn child likely to suffer from the disease? Give your reasons for your conclusions. (2 marks) “yes, person has allele 4 of marker which is segregating with the disease therefore will suffer from the disease later in life” Question notes: - - Innate response triggers = PAMPs or DAMPs ie triggered by pathogen or triggered by the host tissue damage Must know the symbols and system for generating family trees eg diamond for unborn child, triangle for miscarriage, filled in shape ONLY IF PRESENTING WITH SYMPTOMS; leave clear if genetics show will get it eventually, cross through if deceased, should use arrow pointing to person presenting to the doctors C-raf is a protooncogene but Bcl-2 is not considered a protooncogene despite being antiapoptotic; on wiki is classed as an actual oncogene – ie is already having procancer effect collagen found in basement membrane = type-IV collagen fibers Type I collagen is the most common collagen, contains two alpha1 chains and one alpha2 chain, is found in skin and bone, is found in cornea Platelet life span in circulation is about 5-10 days - in a normal person, 20% of the platelets are found in the spleen platelets contain adenosine diphosphate and serotonin platelet granule release causes aggregation and coagulation - p21 (CIP1/WAF1) protein binds to and inhibits the activity of cyclin-CDK2, -CDK1, and CDK4/6 complexes o on the paper says it does not act in S phase ie the following answer is false: “p21CIP1 is an S phase Cdk Inhibitor” Cyclin E can bind Cdk2 in G1 phase, which is required for the transition from G1 to S phase, while Cdk2 binding with Cyclin A is required to progress through the S phase [ie p21 will act here but answer not the best answer as p21 not exclusively acting in S phase due to its actions on the other cyclin/cdk complexes] CDK4 / cyclin D is important for cell cycle G1 phase progression CDK6 / cyclin D is important for cell cycle G1 phase progression and G1/S transition o MUST BE CLEAR ON ALL THESE CDKS / CYCLINS AND WHEN THEY ACT!! Cyclin D = cdk 4/6 [G1 and G1 S] - - 3 Giles Kisby GE Y1 CMS Immunology Cancer - Cyclin A = cdk2 [S phase] Cyclin B = cdk 1 [G2 M] = MPF [nb but according to examiners cyclin b also activates other cdks (1,2,4,5,6) so if there is another correct answer then prob best to go for that instead] the gene responsible for Duchenne muscular dystrophy (DMD) is located on chromosome locus Xp21 ie is X – linked (so is beckers) a female carrier of DMD may show disease symptoms due to skewing of X-inactivation the commonest type of mutation in DMD patients is a deletion, not a point mutation (beckers is point muts of varying severity) Becker muscular dystrophy is a less severe form of DMD / less severe relative to DMD A man with Becker muscular dystrophy will NOT pass the mutation on to all his sons Microtubules, not actin in flagella Actin assembled from monomers, not heterodimers 4 Giles Kisby GE Y1 CMS Immunology Cancer - Fatigue is the commonest complication of chemotherapy (nb anaemia, neutropenic sepsis, weight loss, alopecia can also occur but less common) - asbestos mesothelioma - - - Cytochrome P450 family can inactivate drugs but is also frequently involved in the activation of chemicals to metabolites that can damage DNA use of anti-oestrogens in treatment is the dominant factor responsible for the reduction seen in breast cancer mortality over the last 15 years In colorectal cancer the APC and B-catenin proteins are involved in DNA replication [note that B-catenin acts via c-Myc in its induction of cell cycle and thus replication] colorectal cancer: o it is NOT usually an inherited cancer Generally, most colorectal cancers (about 95%) are considered sporadic, meaning the genetic changes develop by chance after a person is born Most people who develop bowel cancer have no family history of bowel cancer. o Mutation of the tumour suppressor gene WT1 is NOT sufficient to induce polps of the colon; is for cancer of the kidney! o APC, KRAS, and p53 genes are NOT all frequently mutated in colorectal tumours o Familial breast cancer does NOT predispose to colorectal carcinoma There was a large increase in prostate cancer incidence in the USA in the early 1990s due to introduction of the screening method: PSA-antigen ERK is activated by phosphorylation Ras is activated by GTP binding o Ras is a G protein, or a guanosine-nucleotide-binding protein. Specifically, it is a single-subunit small GTPase, which is related in structure to the Gα subunit of heterotrimeric G proteins (large GTPases). Rb is inactivated by phosphorylation Grb2 is an adaptor protein; not activated by phosphorylation 5 Giles Kisby - - - - GE Y1 CMS Immunology Cancer the human genome contains around 20,000-30,000 genes FADH2 leads to the production of ATP Caspases: o Initiator caspases: 2,8,9,10 o Effector caspases: 3,6,7 o Neither effector nor initiator caspases: 4,5 Therefore caspase 5 is not an initiator caspase Apoptosis is stimulated by PTEN (acts as a tumor suppressor gene; o PTEN catalyses the dephosporylation of the 3` phosphate of PIP3, resulting in PIP2. This results in inhibition of the AKT signaling pathway) Apoptosis is inhibited by IAPS [“Inhibitors of Apoptosis”] thyroid cancer and leukaemia are the cancers associated with of childhood [medical] radiation exposure Prometaphase is the phase of mitosis following prophase and preceding metaphase o In prometaphase, the nuclear membrane breaks apart into numerous "membrane vesicles" o In prometaphase the chromosomes inside form protein structures called kinetochores o In prometaphase Kinetochore microtubules emerging from the centrosomes at the poles (ends) of the spindle will then attach to the kinetochores [ie In prometaphase sister kinetochores capture microtubules from opposite poles] mitotic spindle forms in Prophase nuclear envelope is re-assembled in Telophase (not G1 phase) cyanide blocks the flow of electrons through the respiratory chain; malonate only slows electron flow 6 Giles Kisby - - - - - GE Y1 CMS Immunology Cancer use “vertical transmission” term: (this is prob meaning the same as no generations skipped) always be comprehensive in SAQ replies eg comment on ALL people asked to consider, not just those that will become affected as will lose half the marks use the following/similar phrase when interpreting genetic electrophoresis results: “Has allele 4 of marker which is segregating with the disease…(therefore will suffer from the disease later in life)”; nb use a full reply like this – the part in brackets was worth a mark! The following is how blood groups were described in the mark scheme: o B D-positive o B D-negative o O D-positive o O D-negative “clinical circumstances” means is looking for clinical states rather than pathologies ie give relevant blood count figures/states rather than possible diseases: o Describe three clinical circumstances when a platelet transfusion is likely to be indicated (3 marks): As prophylaxis if platelet count is “very low”; very low meaning <10x10^9/L [ie is best to know reference ranges so that can do better than just saying very low and therefore get full marks] Bleeding with “low” platelet count; low probably means <20x10^9/L (ie low but not necessarily thrombocytopenic) Bleeding with platelet dysfunction [eg as occurs from aspirin use or as occurs after a coronary bypass] For both of the below platelet transfusion is not usually indicated, despite quite sever thrombocytopenia: o ITP: Idiopathic thrombocytopenic purpura [In most cases, an autoimmune response is thought to cause ITP] o TTP: Thrombotic thrombocytopenic purpura Reticuloendothelial system = macrophage system = mononuclear phagocyte system o Ie Macrophages in the spleen remove old or damaged red blood cells o Is a part of the immune system that consists of the phagocytic cells[1] located in reticular connective tissue o Reticular connective tissue is found around the liver, the kidney, the spleen, and lymph nodes, as well as in bone marrow o Reticular connective tissue is a type of connective tissue.[1] It has a network of reticular fibers, made of type III collagen 7 Giles Kisby GE Y1 CMS Immunology Cancer The Questions!: All the following are true about Type I collagen except: a) contains two alpha1 chains and one alpha2 chain b) is the most common collagen c) is the main type of collagen found in basement membrane d) is found in skin and bone e) is found in cornea Which one of the following is false regarding platelets? a) they are formed in the bone marrow from megakaryocytes b) their life span in circulation is about 30 days c) in a normal person, 20% of the platelets are found in the spleen d) they contain adenosine diphosphate and serotonin e) granule release causes aggregation and coagulation Actin filaments are found in all of the following structures except the: a) flagella of bacteria b) sarcomeres of skeletal muscle cells c) stress fibres of fibroblasts d) microvilli of the intestinal brush border e) contractile rings of dividing animal cells Actin filaments and microtubule share all of the following properties except: a) the are involved in cell motility b) they are intrinsically polar structures c) they can associate with motor proteins d) they are assembled from subunits that are heterodimers e) they can be cross-linked into bundles Which of the following is the commonest complication of chemotherapy? a) anaemia b) neutropenic sepsis c) fatigue d) weight loss e) alopecia The most common cause of mesothelioma is: a) arsenic b) ionizing radiation c) dietary fat d) asbestos e) smoking What enzyme system is most frequently involved in the activation of chemicals to metabolites that can damage DNA? 8 Giles Kisby a) b) c) d) e) GE Y1 CMS Immunology Cancer Glucoronyl Transferase Haem Oxygenase Cytochrome P450 Xanthine oxidase Glutathione transferase Inherited susceptibility to cancer is the result of: a) lifestyle b) smoking c) germline mutations d) radiation exposure e) somatic mutations Which one of the following is more responsible for the reduction seen in breast cancer mortality over the last 15 years? a) increase use of hormone Replacement therapy b) use of anti-oestrogens in treatment c) improved genetic screening d) a reduction in smoking e) use of gene therapy in treatment Considering colorectal cancer: a) it is usually an inherited cancer b) Mutation of the tumour suppressor gene WT1 is sufficient in inducing polps of the colon c) APC, KRAS, and p53 genes are frequently mutated in colorectal tumours d) The APC and B-catenin proteins are involved in DNA replication e) Familial breast cancer predisposes to colorectal carcinoma There was a large increase in prostate cancer incidence in the USA in the early 1990s. This was due to: a) increased exposure to environmental carcinogens such as cadmium b) introduction of the screening method: PSA-antigen c) more men got access to the health care system d) over-reporting to the cancer registries e) change in dietary habits including higher fat intake The following proteins are activated by phosphorylation: a) EGF b) Grb2 c) Ras d) ERK e) Rb Transcription factors have the ability to: a) synthesise DNA b) Repair mismatch errors in DNA 9 Giles Kisby GE Y1 CMS Immunology Cancer c) Usually bind to DNA upstream of the site of RNA synthesis d) Synthesise mature mRNA e) Splice exonic RNA into mature mRNA With respect to genes and the genome: a) the human genome contains around 20,000-30,000 genes b) the human genome encodes less than 10,000 proteins c) muscle cells have nuclei that contain only genes expressed in muscle d) DNA polymerase III transcribe RNA from the protein-encoding genes e) Telomerases occur in the middle of chromosomes Cytochrome C is involved in: a) the electron transport chain b) krebs cycle c) glycolysis d) lipolysis e) urea cycle In anaerobic respiration the fate of pyruvate is: a) Lactate b) Protein c) ATP d) NADH e) Amino acids Oxidation of FADH2 leads to the production of: a) glucose b) NADH c) ADP d) ATP e) Acetyl CoA Poor question: Insulin: a) is secreted into the blood in response to increased blood amino acids b) is secreted by the pancreas c) stimulates glucose form the blood to the body tissues d) increases glucose export by the liver e) if lacking, causes hypoglycaemia Glycogen: a) is produced during glycolysis b) is an intermediate in the glycerol phosphate shunt c) is an important reserve for the generation of blood glucose by the liver d) is secreted by the pancreas e) requires phosphorylase for its synthesis 10 Giles Kisby GE Y1 CMS Immunology Cancer In mammals, cholesterol can be converted by the action of enzymes into: a) acetate b) bile salts c) adenosine triphosphate d) glucose e) carbon dioxide Which of the following is not an initiator caspases: a) caspase 2 b) caspase 5 c) caspase 8 d) caspase 9 e) caspase 10 Regarding cell cycle progression: a) cyclin A activates Cdk2 [the best answer] b) cyclin D activates Cdk1 c) cyclin B activates Cdk1 [but also activates others] d) p21CIP1 is an S phase Cdk Inhibitor [nb is ~half right] e) p15INK4 is an S phase Cdk inhibitor Concerning muscular dystrophies: a) the gene responsible for Duchenne muscular dystrophy (DMD) is located on chromosome 7 b) a female carrier of DMD may show disease symptoms due to skewing of Xinactivation c) the commonest type of mutation in DMD patients is a point mutation d) Becker muscular dystrophy is more severe that DMD e) A man with Becker muscular dystrophy will pass the mutation on to all his sons The following are proto-oncogenes: a) E2F b) C-Raf c) PTEN d) Bcl-2 e) Rb Which of the following is false regarding apoptosis: a) associated with plasma membrane permeability b) associated with an inflammatory response c) inhibited by PTEN d) associated with membrane blebbing e) inhibited by IAPS Which of the following cancer listed below may be a consequence of childhood [medical] radiation exposure? a) thyroid cancer 11 Giles Kisby b) c) d) e) GE Y1 CMS Immunology Cancer osteocarcoma colon adenocarcinoma leukaemia melanoma EMQ: Cell cycle and its control: Options: a) S phase b) Cytokinesis c) Metaphase d) M phase e) G1 phase f) Telophase g) Prophase h) Anaphase i) G2 phase j) Prometaphase 1. 2. 3. 4. 5. When do daughter chromosome start migration towards the poles? - H When do sister kinetochores capture microtubules from opposite poles? - J When do the mitotic spindle form? - G When is the nuclear envelope re-assembled? - F When are chromosomes aligned at the equator of the spindle? – C EMQs - Metabolism:! A) phospholipid! B) ATP! C) cyanide! D) krebs cycle! E) glycolysis! F) ADP! G) triglycerides! H) malonate! I) pyruvate! J) acetyl Co-A! ! - 36. Mitochondria contain the key enzymes for the… D 37. The electron transport chain is used to synthesise…B 38. This compound blocks the flow of electrons through the respiratory chain…C 39. Cell membranes are formed of a bilayer of …A 40. The molecule used to start lipid biosynthesis is…J 12 Giles Kisby GE Y1 CMS Immunology Cancer SAQ 1 Genetics: - - - - - A) A woman attends your antenatal clinic informing you she is pregnant with her first child. The woman and her brother both suffer from late-onset severe cone-rod dystrophy that leads to blindness in the 4th decade of life. Their deceased father was blind in his early 40’s. Her brother has 2 daughters, 17 and 15 years old, neither show signs of the disease. The woman wants you to find out if her unborn child has inherited the disease. You agree to genotyping the family for a genetic marker that is known to be closely linked to the disease and the results are shown below. a) Draw the family tree and annotate with the correct genotype alleles (3 marks)! b) What is the likely mode of inheritance? Give your reasons. (2 marks) ! o autosomal dominant o due to vertical transmission (this is prob meaning the same as no generations skipped) o and because affects males and females c) Are either of the woman’s nieces likely to get the disease in later life? Explain your reasoning. (2 marks) ! [note: comment on ALL people asked to consider, not just those that will become affected as will lose half the marks; always be comprehensive in SAQ replies] o the 15 year old one will o …but the 17 year old one will not o because the disease is segregating with allele 4 of the marker which the 15 year old has o …but the 17 year old one does not have d) Is the womans unborn child likely to suffer from the disease? Give your reasons for your conclusions. (2 marks)! o Yes; o Has allele 4 of marker which is segregating with the disease o therefore will suffer from the disease later in life e) For future pregnancies what is the family risk of the woman having a child affected with conerod dystrophy (1 mark) ! ! o 0.5 SAQ 2 Immunology:! [see prev notes on this Q] - - a) How do the receptors that recognise infection differ between innate and adaptive immunity? (2 marks) ! o germline encoded vs rearrangement of genes o to PAMPs vs antigen specific b) Antibodies play an important role in linking innate and adaptive immune responses. List 3 ways in which IgG antibody bound to antigen may activate components of innate immunity (3 marks) ! o macrophages o NK cells o Complement o [not mast cells as is IgE instead!] 13 Giles Kisby - - GE Y1 CMS Immunology Cancer c) Name 2 diseases that involve defects in phagocytic cells of innate immunity (2 marks) giving the nature of the defect in each disease (2 marks) ! o CGD o IFNGRD o LAD d) Apart from the detection of infection what other basic mechanism may initiate innate immune responses? (1 mark) ! ! o DAMPs CMS - Immunology SAQ - - - - A) Innate immune receptors (PRRs) are germ-line encoded and recognise PAMPS (1 mark) whereas adaptives immune receptors are antigen-specific and are defied by rearrangement of gene segments during lymphocyte development. (1 mark)" B) Activation of complement via classical pathway (1 mark). Activate phagocytes via Fc Receptors (1 mark). Activation of NK cells by antibody bound to antigen on cell surfaces, leading to antibody-dependent cell mediated cytotoxicity (1 mark)" C) Chronic Granulomatous Disease - in which ROS-based killing is defective (NADPH oxidase mutations) (2 marks). Leukocyte adhesion deficiency, in which adhesion to vascular endothelium is defective, easing to poor migration of neutrophils out of blood vessels to sites of infection via integrin signalling. (2 marks)" D) Damage to cells or tissue ECM, leading to the generation of damage-associated molecular patterns." SAQ 3 Haematology! - - - - A) A 72 Year old man who is B rhD-positive requires transfusion of red packed cells. Give all possible Blood ABO and Rhesus groups which can be safely transfused (4 marks) ! o B D-positive o B D-negative o O D-positive o O D-negative B) Describe three clinical circumstances when a platelet transfusion is likely to be indicated (3 marks) ! o As prophylaxis if platelet count is “very low”; very low meaning <10x10^9/L o Bleeding with “low” platelet count o Bleeding with platelet dysfunction [eg as occurs from aspirin use or as occurs after a coronary bypass] C) Give an example of one disease when platelet transfusion is not usually indicated, despite quite sever thrombocytopenia. (1 marks) ! o ITP: Idiopathic thrombocytopenic purpura [In most cases, an autoimmune response is thought to cause ITP] o TTP: Thrombotic thrombocytopenic purpura D) Explain why the mechanism of thrombocytopenia influences whether or not platelet transfusion is appropriate (2 marks) ! 14 Giles Kisby GE Y1 CMS Immunology Cancer o Platelets may be coated and removed by the reticuloendothelial / RE system 15 Giles Kisby GE Y1 CMS Immunology Cancer Revision lectures: 06/03/14: - - - - - - - See the copies of the formative questions on fb / downloaded See videos om UG rsources to cement knowledge / fill gaps etc eg lack of info on colorectal cancer See his summary set of slides (ie from this rev lec) for the DNA/RNA etc section; he says all the exam question answers for his section are present on those slides TSGs best refer to direct cell cycle modulators but definitely can also be used to refer to other proteins such as those involved in dna repair and in apoptosis regulation Replication origin licensing occurs in interphase (specifically in G1) Most important: o Cdk2 binds cyclin E for G1 to S entry o MPF = (Cdk1 binds cyclinB = mitotic cyclin) for G2 to mitosis entry No DNA damage influence in the successful progression through the spindle assembly checkpoint; is just concerned with proper kinetochore:spindle attachments Cdk’s are not detectable in early G1 Nb APC/C: cdc20 and MPF/cdc25 pathways CAK, Wee1 and cdc25 all occur per successful MPF downstream signalling Chromatids move apart during anaphase; homologous chromosomes do not move apart (firstly because is a splitting event and secondly division is in series so each daughter inherits a copy of each homologue) APC/C:cdc20 targets securing for degradation and degrades cyclin B Is actin NOT tubulin in the contractile ring of cytokinesis Tubulin is involved in all chromosome movements including those during prophase Cdk1 functions: o To phosphorylate nuclear lamins so as to help degrade the nuclear membrane for mitosis o To phosphorylate histones so as to induce the relevant transcription for mitosis Rb is phosphorylated by Cdk2 during the G1/S phase transition Cdks are serine / threonine kinases P21 is an example of a Cdk inhibitor that is not a kinase Chk1 is a kinase Securing is degraded at anaphase Cdc25 is an example of a phosphatase that premotes mitosis BRAF mutant presence is a positive indicator for the use of BRAF inhibitor treatment (RE skin cancer melanomas) but should be aware that if mutation not present the treatment would be detrimental because paradoxically would stimulate the downstream MAPK pathway (through unknown mech of the inhibitor; due to the crossover of pathways etc) Cytotoxics are used in the treatment of breast cancer Her 2 receptor genes become amplified (NOT mutated) in breast cancer treated with Herceptin 16 Giles Kisby - - GE Y1 CMS Immunology Cancer Her2+ (breast cancer) and BRAF+ (melanoma) are indicators of worse prognosis despite the added drugs that can be used to treat the conditions BRaf is a mutated form of Raf that is overactive! Imatinib = a tyrosine-kinase inhibitor used in the treatment of chronic myelogenous leukemia (CML) __imab = mAb; will not cross BBB __inib = small tyrosine kinase inhibitor; will cross the BBB To treat ER+ breast cancer: aromatase inhibitor, remove ovarys, tamoxifen, goserelin [gonadotropin releasing hormone superagonist (GnRH agonist)] Breast cancer often metastasises to bone Breslow thickness as a diagnostic tool ER+ breast cancer is a case most often seen in older women PI3K mutations often occur in breast cancers Hormone production is generally a sign of benign tumours Most common breast cancer is invasive ductal carcinoma (much more common than lobular tumours); ductal tumours can be divided into basal, luminal A/B, Her2+ Even non severe breast cancer will need surgery and radiotherapy first; then the drugs Severe breast cancer will involve surgery and drugs but chemotherapy in the place of radiotherapy PgR+ (prostaglandin receptor +) status is analysed to differentiate between normal ER+ tumours (PgR+) and ER+ tumours likely to have dysfunctional downstream signalling (PgR-) Grade can be via general TNM scale or specific analysis to that tumour eg Duke’s - Learn the cancer namings for the diff tissues; eg leiomyoma Metaplasia (rev, diff cell type) dysplasia (some signs of neoplasia such as architecture disorganisation, loss of cell memb orientation, change in nucleus shape, loss of uniformity; is a preinvasive state neoplasia (benign; slow growth metastatic; many mitoses, invasive but not always metastatic – eg basal cell carcinomas [malignant] are famously not metastatic) Squamous cell carcinoma related to occupational exposure BRAF occurs in 50% of melanomas - Vemurafenib is the - Note the indicators of a malignant nevus o Melanoma in a dysplastic nevus: asymmetry, border irregularity, color variegation, >1/3 inch. Braf inhibitor that can be used to treat such cases 17 Giles Kisby GE Y1 CMS Immunology Cancer - A-helices normally right handed and 3.5 aa per turn Splice donor site is used to specify the binding of the U1 spliceosomal RNA [=U1 snRNP (small nuclear ribonucleoprotein); nb it is a small nuclear RNA (snRNA)] - tRNA does bind to the ribosome as well as to the mRNA at the ribosome SRP = signal recognition particle; do not confuse with the signal sequence (that it recognises) on the protein to be secreted 18 Giles Kisby - - - - GE Y1 CMS Immunology Cancer Think about differences that might be asked for in an SAQ; eg DNA vs RNA differences: bases involved; ribose vs deoxyribose, usually ds vs usually ss, double helix vs various shapes Start of transcription is not the TATAA box (though this is what is recognaised at initiation by the RNA pol); the start is not AUG either (that is for translation); the transcription start site varies in seq but is always the same as the first exon (never will start with an intron) Intron will start G (=acceptor) and end AG (=donor) Be clear on the replication enzymes and their general roles AA is attached to the 3’ CCA of tRNA Learn the specifics of the wobble rules Inosine is derived from guanosine Nucleoside analogue drugs used as chain terminators: o Acyclovir = Drug for Herpes o Cytosine arabinose = Used in Chemotherapy o dideoxycytosine (ddC) = Drug for HIV o azidothymidine (AZT) = Drug for HIV elongation factor hydrolysis at ribosome allows for AA fusion to the growing chain 19 Giles Kisby - - GE Y1 CMS Immunology Cancer sense = noncoding; antisense = coding in eukaryotes cap and tail are bound then scanning occurs for AUG from 5’ hence only the first ORF will ever be translated; in prok various AUG start sites can be used to initiate in manner dependant on mRNA complementary to the ribosomal rRNA (ie therefore polycistronic not just monocistronic) PCR: o 94 deg for 30 sec o 55 deg for 30 sec o 72 deg 1-5 mins (is Taq temp optimum) o o o DNA Purified total cellular DNA Boiled cells (<105) Mouthwash, hair roots Single sperm cells – haplotyping PRIMERS Synthetically made, 18 – 30 bases in length ~50% GC content Avoid runs of the same base (e.g. AAAA or GGGG) Anneal to opposite strands of DNA Direct synthesis towards each other TARGET 90 – 20,000 base pairs in length Ideally between 200 – 5,000 bp Not too GC-rich (will require higher denaturation temp and this will inc destruction of Taq) ACCURACY Taq DNA polymerase makes 1 error in every 5 – 10,000 bases Not a problem when analysing product en masse 20 Giles Kisby GE Y1 CMS Immunology Cancer - Errors are a problem analysing individual molecule (cloned PCR) Undergrad lec slides may be useful to put info in more contexts and use the self tests to check knowledge NOTE THAT IF ONLY TWO ANSWERS ASKED FOR THE EXAMINER JUST LOOKS AT THE FIRST TWO ANSWERS ONLY!! 21 Giles Kisby GE Y1 CMS Immunology Cancer Points from metabolism revision session: - Glucose 6 phosphatase is an ezyme at liver that dephosphorylates G6P to allow gluc release to body - FAD reoxidises lipoamide; not TTP - NADH to mt in different tissues: o Malate dehyd: liver, kidney, heart o Gl3P = skeletal muscle and brain 22 Giles Kisby - - GE Y1 CMS Immunology Cancer CO acts at Hb and cyt oxidase Substrate level phosphorylation in TCA gives GTP (ie not ATP but still is substrate level phosphorylation) Proton motive force NOT electron motive force which is completely wrong Rule: NADP+ cofactor for any biosynth so know that it is cofactor for RNA biosynth even though we have not studied this reaction specifically An SAQ may be to outline eg B – oxidation; can use diagram but definitely use text too as markscheme will be in this form an prob won’t get “carnitine shuttle” marks etc Beri Beri = TTP GL3P is “memb soluble” thus allowing shuttle function Inner mt membrane IS “selectively permeable to protons” Adrenaline increases glucose production at the liver Pyruvate dehyde complex must be occurring in mt Atp synthase converts “conformational energy to chemical energy” Glycolysis involved Substrate level phosphorylation of the ATP producing variety VLDLs are not a major phosplolipid transporter, are not made at the LARGE intestine, do not involve a single type of apoprotein BUT ARE 50-60% TAG!! Cholesterol decreases, not increases membrane fluidity Hmg-coA reductase step involves reduction of HMG-CoA to mevalonate Gluconeogenesis requires ATP hydrolysis Gluconeogenesis is a means of getting glucose from oxaloacetate SAQ: explaining with examples how positive dela G reactions possible: give the full story: by coupling to delta G neg reactions; as long as OVR delta G negative reaction will proceed; eg ATP ADP and ADP AMP; ie using their high energy bonds SAQ: differences between FA synth / ox: 1x enz vs many; NAD/FAD vs NADP; CoA carrier vs ACP carrier SAQ: transamination of alanine: ALT; alanine transaminase; transamination = amino group from one AA to a keto acid; to give a diff AA / KA pair; then give the reaction ie glutamate made etc 13/12/13: Quiz / practice question session [on metabolism]: - CELL TEST RESOURCE IS PRESENT ON 1ST YEAR UNDERGRAD BB PORTAL - SBA: [nb there may be misleading elements – need to choose the best answer] o substrate-level phosphorylation occurs during glycolysis and the Krebs cycle [ie both include production of ATP without O2 involvement] o TCA occurs in mitochondria 23 Giles Kisby GE Y1 CMS Immunology Cancer o o o o o o o o o o o In eukaryotes, five main protein complexes are involved in oxidative phosphorylation: complexes I IV and ATP Synthase ATP Synthase NOT Synthetase Proton motive force gives ADP conversion to ATP Glucagon stimulates gluconeogenesis Cholesterol decreases fluidity at membranes Cholesterol is a precursor to bile salts Hexokinase consumes ATP For acetyl-CoA to FA / palmitate iterative additions of 2C using malonyl CoA are involved Fas are highly reduced molecules Creatine kinase is involved in ATP synthesis ETC complex names: Complex I = NADH dehydrogenase also called NADH:ubiquinone oxidoreductase Complex II = succinate dehydrogenase Complex III = cytochrome bc1 complex Complex IV = cytochrome c oxidase - EMQ: o Given list of Q’s and list of answers, use the answers as the possibilities for each question o Can use same answer multiple times if necessary o Malonate as succinate dehydrogenase competitive inhibitor o Oligomycin as inhibitor of ATP synthase [made by Streptomyces] o Dinitrophenol as ETC uncoupler o Cyanide binds to haem of cytochrome oxidase o Rotenone is a specific inhibitor of NADH dehydrogenase complex action - SAQ: o o o o o o 2/3 lines expected Different number of marks for different questions May be half marks for different parts of answer so not 1:1 ratio necessarily Insulin & glucagon: when released? Insulin & glucagon: effects? Diabetes: complications? 24 Giles Kisby GE Y1 CMS Immunology Cancer Proteins, Nucleic Acids & Gene Expression Learning Objectives and Notes Core Learning Objectives basics of analysis of DNA, particularly the Polymerase Chain Reaction (PCR). Protein Structure Learning Objectives: particular protein conformation. -terminus, carboxyl terminus and side chains. -helix and a ß-pleated sheet and appreciate the bonds that stabilise their formation. nd the concepts of primary structure, secondary structure, tertiary structure & quaternary structure with respect to proteins. Nucleic Acids and Chromosomes Learning Objectives: difference between a nucleotide and a nucleoside. pyrimidines. -stranded helix of DNA (not atomic structure) showing basepairing, the major and minor grooves, and the directionality of the chains. -annealing of complementary strands and what is meant by Watson-Crick base pairing. Compare the genomes of E.coli and Homo Sapiens. chromosome structure. DNA replication, the cell cycle and mitosis Learning Objectives: -conservative replication. template, primer, leading strand, lagging strand, Okasaki fragment and replication fork. -reading and the use of RNA primers. 25 Giles Kisby GE Y1 CMS Immunology Cancer e the different phases of the cell cycle. Nucleic Acids and Gene Expression Gene Organisation & Transcription Part 1 - Gene Transcription Learning Objectives: ifferences between DNA and RNA synthesising each of these. Nucleic Acids and Gene Expression Gene Organisation & Transcription Part 2 - mRNA Processing Learning Objectives - mRNA processing -messenger (hn-) RNA. Nucleic Acids and Gene Expression: Protein translation & post-translational modification Learning Objectives sequence. State how a ribosome recognises the start and end of a sequence to be translated. -synthesised protein that are required for it to enter the secretory pathway. -synthesised proteins can be post-translationally modified. Nucleic Acids and Gene Expression Analysis of Nucleic acids Learning Objectives: 26 Giles Kisby GE Y1 CMS Immunology Cancer ll amounts of DNA for subsequent analysis. DNA sequence. explain their usefulness in analysis of DNA. Introduction to Cells and the Cell Membrane – Students should be able to: nucleolus, nuclear envelope, mitochondrion, rough/smooth endoplasmatic reticulum, ribosomes, Golgi apparatus, secretory granule, plasma membrane, cytoskeletal components • Draw the structure of phosphatidylcholine and identify the component parts macromolecules, ions, water, and organic compounds (including drugs) tated diffusion and active transport of ions and molecules across cell membranes gradient and the consequences of failure of such a movement gradient is coupled to ATP dependent Na+ transport Cellular Organisation of TissuesStudents should be able to: patterns of cell division. collagen in intracellular and extracellular structures. escribe the composition of the main body fluids and the mechanisms which control their volume. 24 factors which control the amount of force exerted by a muscle. nucleus. Cell behaviour 27 Giles Kisby GE Y1 CMS Immunology Cancer Students should be able to: division of normal and transformed cells. that define the cytoskeleton. f molecular motors and polymerisation engines that are responsible for biological movement at the cellular level. locomotion, with reference to phosphorylation, secondary messengers and G-proteins. derstand the functional roles of microtubules and describe the drugs that target these structures system ith relation to their involvement in disease -contraction coupling in muscle Metabolism Learning Objectives Core objectives The student should be able to: •Explain how ATP acts as a carrier of free energy and is used to couple energetically unfavourable reactions. • Summarise the metabolism of glucose by the process of glycolysis, citing the key reactions that consume ATP and generate ATP and the possible fates of pyruvate. • Summarise the Krebs or TCA (tricarboxylic acid cycle) with particular reference to the steps involved in the oxidation of acetyl Co-A and the formation of NADH and FADH2 and the cellular location of these reactions. • Define the process of transamination and how it may generate glycolysis/TCA intermediates from amino acids. • Summarise the chemiosmotic theory and describe ATP synthesis via the electron transport chain in mitochondria • Classify certain compounds in terms of their poisonous effects on specific components of the electron transport chain. 28 Giles Kisby GE Y1 CMS Immunology Cancer • Compare key mitochondrial shuttles and why these mechanisms are required. •Recall the chemical composition of unsaturated and saturated fatty acids. •Summarise the reactions by which the fatty acid palmitate is interconverted with acetyl-CoA and contrast the pathways for synthesis with those of fatty acid catabolism. •Recall the synthesis of cholesterol and other steroids from acetyl CoA and describe the mechanism of transport of cholesterol around the body and its uptake into cells. • Classify pharmacological agents that may be used to control cholesterol metabolism with reference to their mode of action. The following learning objectives relate to the lectures given by Dr James Pease and Dr Hector Keun. Further lectures will be given by Prof Karim Meeran, Dr Nick Oliver and Dr Radha Ramachandran, and learning objectives for these will be given on the day. All lectures will be covered in the revision session given by Drs Pease and Keun, to whom any queries should be directed in the first instance. METABOLISM 1: ATP Production I - Glycolysis and the TCA Cycle • Sketch a cartoon of the three stages of cellular metabolism that convert food to waste products in higher organisms, illustrating the cellular location of each stage. •Explain how ATP acts as a carrier of free energy and is used to couple energetically unfavourable reactions. • Illustrate the role of the coenzyme NAD in the reaction catalysed by dehydrogenases. • Outline the metabolism of glucose by the process of glycolysis, citing the key reactions that consume ATP and generate ATP and the possible fates of pyruvate. • Describe the reactions catalysed by lactate dehydrogenase and creatine kinase. • Outline the oxidative decarboxylation reaction catalysed by pyruvate dehydrogenase. • Describe the Krebs or TCA (tricarboxylic acid cycle) with particular reference to the steps involved in the oxidation of acetyl Co-A and the formation of NADH and FADH2 and the cellular location of these reactions. METABOLISM 2: ATP production II - Oxidative phosphorylation • Describe the process of transamination and how it may generate glycolysis/TCA intermediates from amino acids. • Outline the chemiosmotic theory. • Describe the electron transport chain in mitochondria with reference to the functions of coenzyme Q (ubiquinone) and cytochrome c. • Describe how ATP synthase is able to generate and utilise ATP respectively, with reference to its structure. • Explain why carbon monoxide, cyanide, malonate and oligomycin are poisonous in terms of their effects on specific components of the electron transport chain. 27 • Outline the glycerol phosphate shuttle and the malate-aspartate shuttle, in particular stating why these mechanisms are required. 29 Giles Kisby GE Y1 CMS Immunology Cancer METABOLISM 3: Lipid and Cholesterol Metabolism •Appreciate the chemical composition of unsaturated and saturated fatty acids. •Describe the reactions by which the fatty acid palmitate is metabolised to give acetyl-CoA. •Give an overview of the reactions by which fatty acids are synthesized from acetyl-CoA, contrast the pathways for synthesis with those of fatty acid metabolism. •Outline the synthesis of cholesterol from acetyl CoA. •Outline the synthesis of bile acids and steroid hormones from cholesterol. •Suggest why NADPH and not NADH is used in reductive biosynthesis. •Describe the mechanism of transport of cholesterol around the body and its uptake into cells. •Draw a diagram of low density lipoprotein (LDL) particle and its receptor (LDLR). •Explain how mutations of the LDLR give rise to familial hypercholesterolaemia. • Give examples of pharmacological agents that may be used to control cholesterol metabolism. 28 Cell Cycle & Cancer Learning Objectives Overall learning objectives: interfere with the cell cycle in cancer treatment how these are involved in carcinogenesis tumour suppressor genes benign and malignant tumours) and the cellular derivation of different tumour types and predictive markers and lead to the development of stratified medicine stand the similarities and differences between aetiology and treatment of skin, breast, colon and lymphoma and leukaemia The following learning objectives relate to the lectures given by Dr Andy Porter, to whom any queries should be directed in the first instance. Lectures 1 & 2. The Cell Cycle and its Regulation mean in terms of protein and DNA synthesis and chromosome dynamics. ) the named stages of mitosis. - dependent kinases, inhibitor proteins, proteosomes, other kinases and phosphatases. the principle of the molecular timing process which regulates the cell cycle through oscillating amounts or activities of cyclins and their kinases give examples of external factors, which provide signals allowing cells to pass these 30 Giles Kisby GE Y1 CMS Immunology Cancer checkpoints and enter cell division. differentiates or undergoes programmed cell death (apoptosis). tumour suppressor gene product. especially kinase cascades. though interactions with the cell cycle machinery diagnostic/therapeutic benefits resulting form such knowledge Lecture 3. DNA Damage and Repair ous and environmental factors. e main natural DNA repair mechanisms: BER, NER, MMR and DSB repair (NHEJ & HR) ways and key proteins involved the DDR diagnostic/therapeutic benefits resulting form such knowledge Lecture 4. Oncogenes and Tumour Suppressors . ne and tumour suppressor gene. ivated to an oncogene. disruption of tightly controlled pathways in the cell. are heritable cancers have led to an understanding of the type of cancer-causing gene called a tumour suppressor. 3 in cellular decision making. which successive gene mutations are thought to lead to clinical cancer. The following learning objectives relate to the lectures given by Prof Gerry Thomas, to whom any queries should be directed in the first instance. Cellular Pathology stand the nomenclature that differentiates malignant and benign cancers and their differentiation and development stage. t sites of metastases. 31 Giles Kisby GE Y1 CMS Immunology Cancer Breast Cancer • Understand the types of breast cancer and how it is treated • The differences between hormone and chemotherapy • The mechanisms by which oestrogen receptor signalling can be disrupted • How biology affects prognosis Skin Cancer • Understand the different types of skin cancer and their causes and prognosis • Understand risk factors for melanoma • Understand pathological grading and staging and how this affects treatment and outcome • Understand how and why melanoma patients may be stratified for treatment in the future 12/11/13: notes: - Splicing: lariat structure displaced starts GU and ends AG as in the diagram below: - Introns are present in eukaryotes but not prokaryotes Alternative splicing allows for more proteins than genes Euk = monocistronic genes, prok = polycistronic genes Euk have 5’ cap (ie the triphosphate of the initial nucleotide [usually a met codon]) and p(A) tail (post transcriptionally added). Prok have 5’ cap only Termination of mRNA transcription in prok is Rho dependant/independent; C/G rich region followed by p(T) for rho independent - Do not confuse this with euk p(A) tail - - Termination of mRNA transcription is different in eukaryotes than in prokaryotes (see here or here). Whereas the prokaryotic RNA polymerase recognizes terminator signals, which sometimes function with the aid of the (rho) protein (see here), eukaryotic mRNA transcription proceeds as follows: 32 Giles Kisby GE Y1 CMS Immunology Cancer - 1. The eukaryotic RNA polymerase II usually continues to transcribe well past the end of the gene. - 2. After the end of the gene has been reached, RNA golymerase II passes through one or more AATAAA sequences, which lie beyond the 3' end of the coding region (Figure 28.29). - 3. The pre-mRNA, carrying this signal as AAUAAA, is then cleaved by a special endonuclease that recognizes the signal and cuts at a site 11 to 30 residues to its 3' side. - 4. A tail of polyriboadenylic acid, poly(A), as much as 200 bases long, is added by a special non-template-directed polymerase. The function of the poly(A) tails of eukaryotic mRNAs is unknown. They cannot be essential for all messages, however, because some mRNAs (for example, most histone mRNAs in higher eukaryotes) do not have them. One idea is that they relate to message stability, because the tail-less messages typically have much shorter lifetimes in the nucleus. - Methionine is the first amino acid translated: equates to AUG codon on the mRNA and an ATG codon on the DNA Base: Nucleoside: Adenine (deoxy)adenosine Guanine (deoxy)guanosine cytosine (deoxy)cytidine Uracil uridine (deoxyuridine not found in nucleic acids) thymine thymidine (called this but is effectively deoxythymidine; nondeoxythymidine is called 5-Methyluridine) - - - ~50 tRNAs: satisfy the full 61 coding codons by wobble base pairing (all the possible codons are present in the DNA but same tRNA anticodon loops can recognise multiple different mRNA codons. (some tRNA anticodon options are absent) o Codon bias prob ensures wobble base pairing doesn’t have to occur too often 20 aminoacyl tRNA synthetases: ie recognise tRNA types (that all involved in inclusion of the same AA) not specific tRNAs o A check occurs at this step to ensure correct AA-tRNA charging has occurred - Stop codons: TCA, TAC, TAA Trp is heterocyclic Ser / thr / Asn can be posttranslationally modified (N/O linked glycosylation) Reverse transcriptase (a viral enzyme) can be used to give cDNA from mRNA Antisense = same seq as mRNA - Prok: 33 Giles Kisby GE Y1 CMS Immunology Cancer o o - o Euk: o o RNA Pol (no number after name) The sequence at -10 (the -10 element) has the consensus sequence TATAAT. (pribnow) The sequence at -35 (the -35 element) has the consensus sequence TTGACA. Tfs bind at TFBS TFII’s and RNA PolII bind at TATA box (TATAAA) Prokaryotes, on the other hand, splice rarely Introns are only found in eukaryotic cells; prokaryotes have only exons 29/11/13: ATP Production I - Glycolysis and the TCA cycle: Dr James E. Pease Los from booklet: METABOLISM 1: ATP Production I - Glycolysis and the TCA Cycle • Sketch a cartoon of the three stages of cellular metabolism that convert food to waste products in higher organisms, illustrating the cellular location of each stage. •Explain how ATP acts as a carrier of free energy and is used to couple energetically unfavourable reactions. • Illustrate the role of the coenzyme NAD in the reaction catalysed by dehydrogenases. • Outline the metabolism of glucose by the process of glycolysis, citing the key reactions that consume ATP and generate ATP and the possible fates of pyruvate. • Describe the reactions catalysed by lactate dehydrogenase and creatine kinase. • Outline the oxidative decarboxylation reaction catalysed by pyruvate dehydrogenase. • Describe the Krebs or TCA (tricarboxylic acid cycle) with particular reference to the steps involved in the oxidation of acetyl Co-A and the formation of NADH and FADH2 and the cellular location of these reactions. Notes: - Metabolism overview: o Metabolism can be split into catabolic and anabolic pathways: Catabolic pathways provide ‘useful’ energy in the form of ATP and also the biomolecules needed for synthesis. 34 Giles Kisby GE Y1 CMS Immunology Cancer o o o o - Each pathway driven by specific enzymes Metabolic pathways have two key attributes: Specific reactions (driven by enzymes). The reactions are energetically favourable. ΔG is negative, leading to an increase in disorder of the system, release of heat. Pathways within the cell that synthesise molecules are generally energetically unfavourable e.g. peptide synthesis They take place because they are coupled to an energetically favourable one. The majority of energetically unfavourable biochemical reactions rely on the hydrolysis of high-energy phosphate bonds such as those found in ATP. Phosphoanhydride bonds have a large negative DG of hydrolysis, and are thus said to be "high energy" bonds. ATP ADP + Pi : ΔG°'= - 31 kJ/mole !!! (ΔG°' = standard free energy change at pH 7) ATP structure: 35 Giles Kisby GE Y1 CMS Immunology Cancer - Glucose Combustion vs Glucose Metabolism o Glucose Combustion C6H12O6 + 6O2 6CO2 + 6H2O: Energetically favourable: ΔG°' = -2872 kJ/mole The Relatively large activation energy is overcome by heat source Free energy (from the OVR process) is released as heat o Glucose Metabolism Relatively small activation energies overcome by enzymes and body temperature Free energy liberated is invested in carrier molecules such as ATP: This is around 50% efficient, c.f. car engines which on average are only 20% efficient [ie some energy lost as heat and not invested] - The 6 types of reaction in metabolism: - Cofactors: 36 Giles Kisby GE Y1 CMS Immunology Cancer o NAD+ - NAD+ (Nicotinamide adenine dinucleotide) is a vital component of many dehydrogenation reactions within the body. NAD+ is a co-enzyme [If the cofactor is organic, then it is called a coenzyme] It has no effect on its own but functions only after binding to a protein. NAD+ is a critical co-factor for the dehydrogenation reactions found in key metabolic pathways by readily accepting a hydrogen atom and two electrons: Glycolysis: o Glycolysis is essentially an anaerobic process, occurring in the cytoplasm of cells and is probably a throwback to the pathways used by prehistoric anaerobic bacteria. o The net result of glycolysis: 37 Giles Kisby GE Y1 CMS Immunology Cancer o o o Within the ten reactions that make up the glycolysis pathway, there are two main concepts: Formation of a High Energy Compound: involves the investment of energy in the form of ATP. Splitting of a High Energy Compound: produces useful energy in the form of ATP generation. 1. This reaction is essentially irreversible and commits the cell to the subsequent reactions. Also traps glucose inside the cell by means of the negative charge. The isomerisation shuffles the glucose chair to give fructose. The logic behind this reaction is that fructose can be split into equal halves when subsequently cleaved. 2. 38 Giles Kisby GE Y1 CMS Immunology Cancer o 3. o 4. o Here a highly symmetrical, high energy compound is generated [suitable for cleavage in two] Regulation of phosphofructokinase exquisitely controls the entry of sugars into the glycolysis pathway. Opening of the fructose ring to generate two high energy compounds, one of which, (dihydroxyacetone phosphate) subsequently undergoes isomerisation. 5. 39 Giles Kisby GE Y1 CMS Immunology Cancer o o o o Metabolic Diseases - Deficiency in TPI is extremely rare (only 29 documented cases worldwide) since its diagnosis 35 years ago. Most sufferers die within the first 6 years of their lives. NADH is generated here which can be later used to generate yet more ATP within the mitochondria in a process known as oxidative phosphorylation ATP generation Shuffling of the phosphate group from the 3 to the 2 position. 6. 7. 8. 9. 40 Giles Kisby GE Y1 CMS Immunology Cancer o 10. - Substrate level phosphorylation: o Substrate-level phosphorylation can be defined as the production of ATP by the direct transfer of a high-energy phosphate group from an intermediate substrate in a biochemical pathway to ADP, such as occurs in glycolysis. o e.g. o - Transfer of the high energy phosphate group to ADP, generating one ATP molecule in the process. This is in contrast to oxidative phosphorylation, where ATP is produced using energy derived from the transfer of electrons in an electron transport system Fates of Pyruvate: o 1. Alcoholic Fermentation This is characteristic of yeasts and can occur under anaerobic conditions. o 2. Generation of Lactate 41 Giles Kisby GE Y1 CMS Immunology Cancer o During intense exercise, skeletal muscles have to function anaerobically, as oxygen is a limiting factor. As such, the metabolite pyruvate is converted into lactate. This also generates free NAD+ which is needed by the muscle for other reactions. Lactate diffuses from the muscle into the blood stream and is picked up by the liver, where the high levels of NAD+ can be used by lactate dehydrogenase to regenerate pyruvate. 3. Entry to TCA cycle via Generation of acetyl CoA Pyruvate acetyl CoA occurs in the mitochondria of the cell. mitochondrial pyruvate carrier (MPC) is responsible for pyruvate transfer to mitochondria before conversion to acetyl CoA can occur The acetyl CoA thus formed is committed to entry into the citric acid cycle and can ultimately produce ATP by the process of oxidative phosphorylation This is the committed step for the entry of pyruvate into the TCA cycle The overall reaction: Detail of pyruvate dehydrogenase complex action: The pyruvate dehydrogenase complex is gigantic (in molecular terms): o 60 polypeptides in total o three individual enzymes present: Pyruvate dehydrogenase (E1), Dihydrolipoyl transacetylase (E2), Dihydrolipoyl dehydrogenase (E3) o five co-factors: Thiamine pyrophosphate (TPP), lipoamide, FAD, CoA and NAD+ 42 Giles Kisby GE Y1 CMS Immunology Cancer TPP (in E1), lipoamide (in E2) and FAD (in E3) are prosthetic groups [Prosthetic groups are a permanent part of the complex, whereas other co-factors bind reversibly to enzymes] Thiamine pyrophosphate (TPP) Derivative of vitamin B1 (thiamine). Readily loses a proton and the resulting carbanion attacks that of pyruvate to yield hydroxyethyl-TPP. A deficiency of thiamine (vitamin B1) is the cause of Beri-Beri, whose symptoms include damage to the peripheral nervous system, weakness of the musculature and decreased cardiac output. The brain is particularly vulnerable as it relies heavily on glucose metabolism. Lipoamide: undergoes oxidation and reduction The long flexible arm of the molecule allows the dithiol group to swing from one active site to another within the complex. Arsenite (AsO33-) and mercury have a high affinity for neighbouring sulphydryl groups, such as those that occur in reduced lipoamide and will readily inhibit pyruvate dehydrogenase. 43 Giles Kisby GE Y1 CMS Immunology Cancer o Flavine Adenine Dinucleotide (FAD) FAD accepts and donates 2 electrons with 2 protons (2 H): FAD + 2 e- + 2 H+ FADH2 Reaction cycle: Decarboxylation of pyruvate to give hydroxyethyl TPP. Oxidation & transfer to lipoamide to give acetylipoamide. Transfer of the acetyl group to CoA to give acetyl CoA. Regeneration of oxidised lipoamide. Regeneration of oxidised FAD, generating NADH. 44 Giles Kisby GE Y1 CMS Immunology Cancer - Regeneration of NAD+: o Both alcoholic fermentation and the generation of lactate serve one common purpose: o They allow NAD+ to be regenerated and thus glycolysis to continue, in conditions of oxygen deprivation. o i.e. conditions in which the rate of NADH formation by glycolysis is greater than its rate of oxidation by the respiratory chain. o NAD+, you recall, is needed for the dehydrogenation of glyceraldehyde 3-phosphate, which is the first step in generating ATP for the body. - Lactate Dehydrogenase as a Diagnostic Tool: o LDH is present in many body tissues, especially the heart, liver, kidney, skeletal muscle, brain, blood cells and lungs. o LDH catalyses the inter-conversion of pyruvate and lactate. o LDH is released from cells if damage to them occurs and therefore can be used as a diagnostic tool o Elevated levels can be used to diagnose several disorders including: stroke heart attack liver disease (e.g. hepatitis) muscle injury muscular dystrophy pulmonary infarction 45 Giles Kisby GE Y1 CMS Immunology Cancer - Creatine Phosphate o In muscle, the amount of ATP needed during exercise is only enough to sustain contraction for around one second. o Thankfully a large reservoir of creatine phosphate is on hand to buffer demands for phosphate (25mM creatine phosphate c.f. 4mM ATP in resting muscle). o ΔG (hydrolysis) = -31 kJ/mole (ATP) & -43.1 kJ/mole (CP) o Hence the use of creatine by atheletes as a dietary supplement. o Creatine Kinase as a Diagnostic Tool When a muscle is damaged, creatine kinase leaks into the bloodstream. Either total levels of creatine kinase or the tissue specific isoform can be measured to help to determine which tissue has been damaged. Elevated levels can be used to: diagnose myocardial infarction (heart attack) determine the extent of muscular disease evaluate cause of chest pain help discover carriers of muscular dystrophy (Duchenne) - The Krebs Cycle o a.k.a. The Tricarboxylic Acid (TCA) cycle or The Citric Acid Cycle. 46 Giles Kisby GE Y1 CMS Immunology Cancer o o o o o A continuous cycle of eight reactions, starting with 2 carbon atoms from acetyl CoA being condensed with the 4 carbon unit of oxaloacetate to give a 6 carbon unit , citrate. Each turn of the cycle produces two molecules of CO2 (waste) plus three molecules of NADH, one molecule of GTP and one molecule of FADH2. The Krebs cycle enzymes are soluble proteins located in the mitochondrial matrix space, except for succinate dehydrogenase, which is an integral membrane protein that is firmly attached to the inner surface of the inner mitochondrial membrane. Here, it can communicate directly with components in the respiratory chain, as we shall see in the next lecture. The majority of the energy that derives from the metabolism of food is generated when the reduced coenzymes are re-oxidised by the respiratory chain in the mitochondrial inner membrane in a process known as oxidative phosphorylation. The Krebs cycle only operates under aerobic conditions, as the NAD+ and FAD needed are only regenerated via the transfer of electrons to O2 during oxidative phosphorylation. 47 Giles Kisby GE Y1 CMS Immunology Cancer o 1. o Transfer to the oxaloacetate of 2C from acetyl CoA Acetyl Co Enzyme A thioester bond is a high-energy linkage, so it is readily hydrolysed, enabling acetyl CoA to donate the acetate (2C) to other molecules. Acetyl Co Enzyme ARNA ancestry suggests it is of primeval origin. Acetyl Co Enzyme A structure: Isomerisation of citrate to give isocitrate 2. 48 Giles Kisby GE Y1 CMS Immunology Cancer o o o 3. Oxidation of isocitrate to give a-ketoglutarate Similar to the reaction catalysed by PDH. CoA is displaced by a phosphate molecule which is subsequently transferred to GTP. GTP = Guanosine Triphosphate (In bacteria and plants, ATP is formed instead). 4. 5. 49 Giles Kisby GE Y1 CMS Immunology Cancer o - 6. o 7. o 8. Oxidation of succinate generating some FADH2 Addition of a water molecule, breaking a double bond. The last step. Dehydrogenation of malate to give oxaloacetate, the starting point of the cycle. Glycolysis and the Krebs Cycle Provide the Starting Point for Many Biosynthetic Reactions: o The amino acids, nucleotides, lipids, sugars, and other molecules shown here as products, in turn, become the precursors for the many of the macromolecules of the cell. Each black arrow in this diagram denotes a single enzyme-catalysed reaction. Red arrows generally represent multi-step pathways 50 Giles Kisby GE Y1 CMS Immunology Cancer 12/12/13: Diabetes – the archetypal metabolic disease: Nick Oliver Los from slides: • • • • • • Describe the actions of insulin Summarise the metabolic changes seen in diabetes Outline the pathogenesis of type 1 diabetes Explain the principle complications of diabetes and the mechanisms involved in their development Illustrate the metabolism of free fatty acids to ketoacids Summarise the multiple metabolites, multiple organ systems, multidisciplinary nature and multiple pharmacology of diabetes Notes: 51 Giles Kisby - - Insulin o o o o o o o GE Y1 CMS Immunology Cancer 51 amino acid Protein hormone Secreted by beta cells of Islet of Langerhans ‘Store cupboard’ hormone Storage of energy, repair and growth Elevated post-prandially [after eating], basal secretion when fasting Anabolic action Upregulation of GLUT4 transport protein GLUT4 transports glucose into cells From there the glucose is converted to glycogen [in liver and muscle] or to fatty acids via glycolysis [insulin stimulates various steps in glycolysis [TRUE]; (Encourages preferential CHO metabolism); see below] Inhibits nutrient breakdown Lipolysis in adipose Proteolysis Stimulates fatty acid synthesis and esterification Effect of insulin on glucose uptake and metabolism. Insulin binds to its receptor (1), which starts many protein activation cascades (2). These include translocation of Glut-4 transporter to the plasma membrane and influx of glucose (3), glycogen synthesis (4), glycolysis (5) and triglyceride synthesis (6). 52 Giles Kisby GE Y1 CMS Immunology Cancer - Diabetes o Archetypal metabolic disease o Change in insulin changes metabolism of Glucose Lipid Protein Ketoacid o Alters ATP production o Multisystem chronic consequences to relative or absolute insulin deficiency - Type 1 Diabetes [ie only type 1 looked at here] o Autoimmune destruction of beta cells Glutamic Acid Decarboxylase (GAD) Ab [ie targeted] Islet cell Ab [ie targeted] Zn transporter targeted Insulin targeted o T-cell mediated: is Type IV hypersensitivity o Absolute insulin deficiency o Hyperglycaemia Normal range 4-6mmol/L fasting Definition of diabetes Fasting glucose > 7mmol/L 2hour glucose > 11.1mmol/L Glucose elevated in T1DM o Intracellular hypoglycaemia Declining ATP reserve 53 Giles Kisby GE Y1 CMS Immunology Cancer ‘Starving’ cell Alternative fuel sources Fatty acids o Mobilised from adipose in absence of insulin o Hormone sensitive lipase It is inhibited by insulin so high activity in insulin absence HSL functions to hydrolyze the first fatty acid from a triacylglycerol o Rich ATP source o Metabolised by beta oxidation o Utilised in heart and muscle Amino acids o Dietary or result of proteolysis o Depend on gluconeogenesis: gluconeogenesis can use amino acids as a substrate o But… in insulin deficiency cannot absorb glucose: ie increased usage of the AAs in gluconeogenesis Ketoacids o 3x different types: see below; o All can be metabolised as energy sources: β Hydroxybutyrate prob best though o Utilised by central nervous system o Synthesized in liver o Converted back to acetyl CoA o Mitochondrial ATP source o Important in starvation 54 Giles Kisby GE Y1 CMS Immunology Cancer o o o o Chemical structures of the three ketone bodies: acetone (top), acetoacetic acid (middle), and beta-hydroxybutyric acid (bottom). [redox state determines form of the second two] Potassium Insulin required for potassium influx into cells Hyperkalaemia extracellularly; hypokalemia intracellularly Cardiac instability [due to low gluc and K inside] Muscle weakness Metabolic effects (if untreated) Hyperglycaemia Elevated free fatty acids Ketosis Hyperkalaemia Acidosis Change in total cholesterol: HDL ratio, often elevated HDL cholesterol Symptoms: Prolonged high blood glucose can cause glucose absorption in the lens of the eye, which leads to changes in its shape, resulting in vision changes. Blurred vision is a common complaint leading to a diabetes diagnosis Diabetic nephropathy, the impact of diabetes on the kidneys, can lead to scarring changes in the kidney tissue, loss of small or progressively larger amounts of protein in the urine, and eventually chronic kidney disease requiring dialysis. Atherosclerosis of larger arteries occurs: largely responsible for the decreased life expectancy The reason is unclear but appears not so much as about what the change to cholesterol composition in body is but how it is achieved: statins give same changes but result in positive effects on atheroschlerosis levels. Insulin stimulates HMG CoA Reductase activity Increased de novo Cholesterol synthesis Insulin deficiency leads to: o fall in Cholesterol synthesis 55 Giles Kisby GE Y1 CMS Immunology Cancer o o o fall in LDL o Rise in HDL [ie often seen in treated type 1 diabetes] o Mobilisation of cholesterol from peripheral cell membranes Another risk is diabetic neuropathy, the impact of diabetes on the nervous system — most commonly causing numbness, tingling, and pain in the feet, and also increasing the risk of skin damage due to altered sensation. Together with vascular disease in the legs, neuropathy contributes to the risk of diabetes-related foot problems (such as diabetic foot ulcers) Short-term [ie but will continue to persist] Weight loss Osmotic symptoms: o Polyuria: abnormally large production or passage of urine o Nocturia: need to wake and pass urine at night o Polydypsia: excessive thirst o Dehydration o Pre-renal failure Dehydration 4 T’s: tired, thin, thirsty, toilet Long-term Blindness Renal failure Neuropathy o Autonomic o Peripheral Oxidative stress is triggered in diabetes: Will give damage at the thin blood vessels, nerves and kidneys Treatment: Insulin, but not just insulin Pharmacology Renal protection 56 Giles Kisby GE Y1 CMS Immunology Cancer Retinopathy prevention Neuropathic symptom control Macrovascular risk reduction Statin ACE inhibitor/ Angiotensin 2 blockade Anti-platelet Anti-hypertensives 13/12/13: Inherited Metabolic Diseases: Dr Radha Ramachandran Los from slides: • • • • • • Define Inherited Metabolic Diseases When should a diagnosis of inherited metabolic diseases be considered (likely presentations) Why is early diagnosis important Baseline investigations and emergency management of a patient with a possible diagnosis of IMD What are the diseases that are included in the routine newborn screening programme in the UK Basic understanding of some common disorders like phenylketonuria, MCADD, galactosaemia, Glycogen storage disorders Notes: - Inherited metabolic diseases o Group of diseases that manifest as a result of dysfunction of a single or multiple enzymes in one or more of the metabolic pathways o More than 600 separate disorders known so far o Collectively not that uncommon - 1 in 800 live births o 800 new diagnosis per year in the UK o 25% manifest after the age of 15 - Think IMD 57 Giles Kisby GE Y1 CMS Immunology Cancer o - In all neonates with unexplained overwhelming progressive disease after normal pregnancy and delivery o All children who are acutely unwell with decreased consciousness particularly if preceded by fasting, fever or vomiting o All patients with unexplained neurology, hypoglycaemia, acidosis or decreased consciousness o Family history of unexplained disease or premature deaths o Unexplained: Cardiomyopathy Liver disease Myopathy CNS manifestations Dysmorphia Apparently unrelated multisystem involvement o Metabolic emergency Usually due to disorders of fat, protein or glucose or other sugars metabolism/utilisation Hypoglycaemia may be a feature – in addition may present with acidosis, increased ketones, decreased level of consciousness (due to hyperammonaemia) Treatment: Stop all feeding Start a dextrose infusion – to give enough calories to prevent/reverse catabolic state [is rare for it to be a problem with glucose metabolism] Keep checking to make sure that normal acid base status is maintained Why think IMD o Non specific multi organ presentation o Diagnosis often missed o Missed diagnosis often fatal o Many can be treated o Time is of the essence o Early diagnosis can potentially enable life saving treatment and prevent long term morbidity o Other implications – genetic counselling etc 58 Giles Kisby - GE Y1 CMS Immunology Cancer Phenylketonuria: PKU o Autosomal recessive o Deficiency of phenylalanine hydroxylase (PAH) o One of most common IMDs o Aim is to keep plasma phenylalanine levels down: otherwise neurological deficits and death [Phe interferes with dopamine pathways in brain, etc] 59 Giles Kisby GE Y1 CMS Immunology Cancer o o o - Protein restriction [to keep Phe levels down] NO ANIMAL PROTEINs, no nuts, no legumes, no seeds, no beer, no chocolate, no sweetners and only limited portions of low protein vegetables, fruits and starchy foods Special protein supplements Newborn screening Newborn screening introduced for PKU in 1963 First IMD to be screened Guthrie cards – dried blood spots Very early introduction of treatment Normal neurological development with normal lifespan: had previously been poor prognosis despite diet due to late detection Most of the deleterious effects of excess phenylalanine occur during neurological development Very expensive: £ 65,000 pounds per person per year Pregnancies Phenylalanine can cross the placenta Hyper-phenylalaninaemia can cause foetal abnormalities low weight at birth, the congenital heart defects, digestive tract defects, osseous arrangements, microcephaly, handicap of intellectual development (Maternal PKU syndrome) Recommended to maintain very low phenylalanine levels during pregnancy < 360 µmol/L Diseases included in the UK Newborn Screening Programme o Sickle Cell Anaemia o Cystic Fibrosis o Hypothyroidism o Phenylketonuria o MCADD 60 Giles Kisby GE Y1 CMS Immunology Cancer - MCADD o Medium chain acyl-CoA dehydrogenase deficiency o Commonest of the fatty acid oxidation defects o Manifests late infancy/childhood o Treatment simple- don’t fast! o Prognosis excellent after diagnosis + counselling o However if undiagnosed first crisis can be fatal in 25% and often residual neurological deficit - Hypoglycaemia – differential diagnosis o If ketones are low and free fatty acids are low Defect in lypolysis - Hyperinsulinism o If ketones are low and free fatty acids are very high Defect in lipolysis - Disorders of fatty acid oxidation o If ketones are high Disorders of protein utilisation (e.g organic acidurias) Disorders of glucose utilisation / diabetes - Acidosis – differential diagnosis o Normal anion gap Renal or intestinal loss of bicarbonate Clue - increased chloride o Increased anion gap Organic acids – such as lactates or ketones Organic acidurias Respiratory chain deficits Gluconeogenesis Glycogen storage disease Fatty acid oxidation defects - Hyperammonaemia: o Severe liver failure o Urea cycle defects [any relevant defect on the below diagram; NH3 will be high if there is a defect in any of the downstream pathway steps] o Organic acidurias = Organic academia Ie due to buildup of AA derived acids o o o o Urea cycle defects can present at any age Consider diagnosis in any patient with unexplained hyperammonaemia Measure ammonia in any patient with encephalopathy 61 Giles Kisby - Metabolic Adaptation to Fasting/Starvation: disorders: o Galactosaemia relavant to exogenous phase o Glycogen storage diseases o Fatty acid oxidation defects - Galactosaemia o Primary starch in milk – lactose o Lactose is a disaccharide (glucose and galactose ) o Galactosaemia- deficiency of enzyme Gal-1 GE Y1 CMS Immunology Cancer 62 Giles Kisby GE Y1 CMS Immunology Cancer o o o o Failure to utilise Galactose and toxic metabolites accumulate Vomiting, diarrhoea, jaundice, liver and renal disturbance and cataract Galactose free diet – may be life saving Some countries offer newborn screening for this - Glycogen storage diseases o Presentation Consequences of pathological glycogen storage- hepatomegaly, myopathy Hypoglycemia o Commonest GSD 1 – mainly hepatopathic + hypoglycaemia GSD III – mixed hepatopathic and myopathic + hypoglycaemia o Therapy – frequent meals, overnight- continuous NG feed / uncooked corn starch - Fatty acid oxidation defects 05/12/13: Integrated metabolism: Prof. Karim Meeran Los: Notes: - - Split of F16BP gives both GAP and dihydroxyacetone phosphate Triglyceride stores must be deesterified before can be used as an energy source Lecturer calculate it as 38 ATP per full pathway from Glucose o But have to use ATP in ATP transport at mt and other transport steps of respiration so some not available for use Ischaemia (stroke/MI/angina/exercise) leads to anaerobic glycolysis occurring o Angina pain due to lactic acid buildup o There is no way to get energy from fats anaerobically o In ischaemia: FA oxidation glycolysis switch occurs o Angina patients: nitrates, GTN, BBs, asprin, statins, O2 o Nb but in prolonged, aerobic, exercise switch back to FA oxidation occurs [see below image] eg in a marathon – ie is not an ischaemic state o Anaerobic exercise: lactic acidosis will occur 63 Giles Kisby - - - - - GE Y1 CMS Immunology Cancer In resting muscle, fatty acids represent the major energy source; during exertion, glucose is the primary source. Weightlifting: generate more white muscle fibres o White as are rich in glycogen o Weightlifting involves glycolysis focus for fast, short term energy supply Marathon training o Increased fatty acid oxidation capability and oxidative phosphorylation capability o High mt levels o High myoglobin levels [this gives the red colour] o Eat little glycogen until day before race to enhance glycogen synth (relevant enzymes translated) then eat carbs for high storage for the race o Energy pathway source changes through the race: Lactate at the liver is turned to glucose via the corrie cycle Aspartate transaminase catalyzes the interconversion of aspartate and α-ketoglutarate to oxaloacetate and glutamate. o Oxaloacetate can then enter gluconeogenesis Liver function: High ALP levels can occur if the bile ducts are obstructed Insulin: o Switches on enzymes that store fat o Switches on glycolysis o Switches of gluconeogenesis o Switches on glycogen synthesis o Switches off glycogen degradation o Switches off ketogenesis Ketogenesis: o In starvation state conversion of fatty acids to ketones occurs to give brain an energy supply [fatty acids can’t cross the BBB] o However ketones are acidic so can cause loss of consciousness due to ketones in the brain 64 Giles Kisby - GE Y1 CMS Immunology Cancer o Diabetics that die die because of the ketones o Ketones give metabolic acidosis In starvation blood glucose stays constant and normal right up until very near the end. FAs are used as the energy source (with everything largely converted off using glucose): o The human starvation response is unique among animals in that human brains do not require the ingestion of glucose to function. During starvation, less than half the energy used by the brain comes from metabolized glucose. Because the human brain can use ketone bodies as major fuel sources, the body is not forced to break down skeletal muscles at a high rate, thereby maintaining both cognitive function and mobility for up to several weeks. This response is extremely important in human evolution and allowed for humans to continue to find food effectively even in the face of prolonged starvation.[8] o Initially, the level of insulin in circulation drops and the levels of glucagon and epinephrine rise, degrading high amounts of glycogen and upregulating gluconeogenesis, lipolysis, and ketogenesis. The body’s glycogen stores are consumed in about 24 hours. In a normal 70 kg adult, only about 8,000 kilojoules of glycogen are stored in the body (mostly in the striated muscles).The body also engages in gluconeogenesis in order to convert glycerol and glucogenic amino acids into glucose for metabolism. Another adaptation is the Cori cycle, which involves shuttling lipid-derived energy in glucose to peripheral glycolytic tissues, which in turn send the lactate back to the liver for resynthesis to glucose. Because of these processes, blood glucose levels will remain relatively stable during prolonged starvation. o However, the main source of energy during prolonged starvation is derived from triglycerides. Compared to the 8,000 kilojoules of stored glycogen, lipid fuels are much richer in energy content, and a 70 kg adult will store over 400,000 kilojoules of triglycerides (mostly in adipose tissue).[9] Triglycerides are broken down to fatty acids via lipolysis. Epinephrine precipitates lipolysis by activating protein kinase A, which phosphorylates hormone sensitive lipase (HSL) and perilipin. These enzymes, along with CGI-58 and adipose triglyeride lipase (ATGL), complex at the surface of lipid droplets. The concerted action of ATGL and HSL liberates the first two fatty acids. Cellular monoacylglycerol lipase (MGL), liberates the final fatty acid. The remaining glycerol enters gluconeogenesis.[10] o Fatty acids by themselves cannot be used as a direct fuel source. They must first undergo beta oxidation in the mitochondria (mostly of skeletal muscle, cardiac muscle, and liver cells). Fatty acids are transported into the mitochondria as an acylcarnitine via the action of the enzyme CAT-1. This step controls the metabolic flux of beta oxidation. The resulting acetyl-CoA enters the TCA cycle and undergoes oxidative phosphorylation to produce ATP. Some of this ATP is invested in gluconeogenesis in order to produce more glucose.[11] o Triglycerides and long-chain fatty acids are too hydrophobic to cross into brain cells, so the liver must convert them into short-chain fatty acids and ketone bodies through ketogenesis. The resulting ketone bodies, acetoacetate and βhydroxybutyrate, are amphipathic and can be transported into the brain (and muscles) and broken down into acetyl-CoA for use in the TCA cycle. Acetoacetate 65 Giles Kisby GE Y1 CMS Immunology Cancer o o breaks down spontaneously into acetone, and the acetone is released through the urine and lungs to produce the “acetone breath” that accompanies prolonged fasting. The brain also uses glucose during starvation, but most of the body’s glucose is allocated to the skeletal muscles and red blood cells. The cost of the brain using too much glucose is muscle loss. If the brain and muscles relied entirely on glucose, the body would lose 50% of its nitrogen content in 8–10 days.[12] After prolonged fasting, the body begins to degrade its own skeletal muscle. In order to keep the brain functioning, gluconeogenesis will continue to generate glucose, but glucogenic amino acids, primarily alanine, are required. These come from the skeletal muscle. Late in starvation, when blood ketone levels reach 5-7 mM, ketone use in the brain rises, while ketone use in muscles drops.[13] Autophagy then occurs at an accelerated rate. In autophagy, cells will cannibalize critical molecules to produce amino acids for gluconeogenesis. This process distorts the structure of the cells, and a common cause of death in starvation is due to diaphragm failure from prolonged autophagy.[14] 05/12/13: Cellular Organisation of Tissues: Cell Behaviour 1: Dr Anabel Varela Carver [tutorial but given as a lecture] 66 Giles Kisby GE Y1 CMS Immunology Cancer Los: Cellular Organisation of TissuesStudents should be able to: epithelial cells have specialised functions, and describe their different patterns of cell division. collagen in intracellular and extracellular structures. Describe the molecules of the extracellular matrix and the regulation of collagen assembly. volume. 24 n, excitable cells as well as the factors which control the amount of force exerted by a muscle. nucleus. Cell behaviour Students should be able to: cribe the roles of growth factors, cell contacts and tissue boundaries in the control of division of normal and transformed cells. that define the cytoskeleton. responsible for biological movement at the cellular level. locomotion, with reference to phosphorylation, secondary messengers and G-proteins. structures e assembled and describe their classification system disease the major structural features of a sarcomere -contraction coupling in muscle 67 Giles Kisby GE Y1 CMS Immunology Cancer Notes: - Integrins are important in cancer (re beta – catenin) Ras-map dysregulation can lead to either failure to grow or overgrowth Gap-Junction Channels Dysfunction in Deafness and Hearing Loss Removal of Ca2+ leads to high proliferation rates Cadherins, beta-catenin and integrins all crosstalk Hayflick limit is the number of times a normal human cell population will divide until cell division stops Protooncogene (eg ras) oncogene (eg v12RAS) Not all human cancers are carcinomas [tumor tissue derived from epithelial cells] Immunology: Learning Outcomes – Year 1 (2013) Autumn Term: [insert intro and booklet Los here] LECTURES: 68 Giles Kisby GE Y1 CMS Immunology Cancer 08/11/13: Introduction to immunology: Dr. Keith Gould [says do not have to know extensive detail – just understand how it works] Los (from slides): • • • • Explain the importance of immunology for human health Summarise the basic principles of immune responses, including the concept of clonal selection Recall in outline the anatomy of the immune system, with emphasis on primary and secondary lymphoid tissue and the mucosal immune system Briefly summarise the phenotype and function of cellular components of the immune system Notes: Explain the importance of immunology for human health - immune system overview: o Complex cellular and protein network that has evolved to protect the host from pathogenic microbes o Also involved in homeostasis e.g. tissue repair o Failure of the immune system (immunodeficiency e.g. SCID) leads to increased susceptibility to infection (and sometimes cancer) o Abnormal regulation of the immune system may lead to disease, e.g. autoimmune diseases, allergy Nb hygiene hypothesis o Therapies: Bone marrow transplantation SCID/leukaemia Immunoglobulin replacement Primary Antibody deficiency Specific cell deletion therapy Lymphoma Anti-cytokine therapy (anti TNF) Rheumatoid arthritis Cancer vaccination Prostate cancer Summarise the basic principles of immune responses, including the concept of clonal selection - Some distinctions can be made between innate and acquired immunity but they are closely linked and not wholly independent: 69 Giles Kisby - GE Y1 CMS Immunology Cancer Clonal selection: o Once a lymphocytes is activated by its antigen then it proliferates (clonal expansion) to give many effector and some memory cells Recall in outline the anatomy of the immune system, with emphasis on primary and secondary lymphoid tissue and the mucosal immune system 70 Giles Kisby GE Y1 CMS Immunology Cancer - Primary lymphoid organs are where lymphocytes are produced: o Lymphopoiesis B lymphocytes [develop in bone marrow] T lymphocytes [develop in thymus] - Secondary lymphoid organs are where lymphocytes can interact with antigen and with other lymphocytes spleen lymph nodes mucosal associated lymphoid tissues (MALT) gut associated lymphoid tissues (GALT) includes peyer’s patches (a GALT subset) where the lymphoid cells are [T/B are segregated] involve M-cells which mediate antigen transfer to the lymphocytes A peyer’s patch: - human thymic lobe: o thymus is a bi-lobed organ o no obvious changes during infections (but very important for T cell production) - Bone marrow: o Increased white cell production during infections [prob largely due to high myeloid production] o Liver/spleen also contribute while fetus 71 Giles Kisby GE Y1 CMS Immunology Cancer o o - Red marrow produces blood cells, yellow marrow is fat Mostly flat bones Vertebrae Iliac bones Ribs Ends of long limb bones lymphatic system: o Fluid drained from between tissue cells absorbed into lymph o 2 to 3 litres of lymph are returned to the blood each day (via superior vena cava) o Lymph node structure (see below): Germinal centers are site of B cell proliferation T cell area is more central [chemokines direct them to their site] B cell area more peripheral [chemokines direct them to their site] Blood supply to the node supplies the lymphocytes [via ‘high endothelial venules’: specialized post-capillary venous swellings characterized by plump endothelial cells as opposed to the usual thinner endothelial cells found in regular venules. HEVs enable lymphocytes circulating in the blood to directly enter a lymph node (by crossing through the HEV). In humans, HEVs are found in all secondary lymphoid organs (with the exception of spleen, where blood exits through open arterioles and enters the red pulp)] Lymph cycles through the lymphatic vessels DCs present antigen to the lymphocytes 72 Giles Kisby - GE Y1 CMS Immunology Cancer The spleen: o filter for antigens in the blood (blood passing through is directly filtered compared to other secondary tissues where filtration is more closely based on the lymphatic system) o White pulp immediately surrounds arteries with lymphocytes segregated: T cells immediately around the arteries (PALS: periarterial lymphoid sheath) Follicles of B cells present further out (primary follicles in marginal zone) o Red pulp more peripheral: function is to filter defective or worn-out red blood cells o Effects of removal: modest increases in circulating white blood cells and platelets, diminished responsiveness to some vaccines, (Splenectomy greatly diminishes the frequency of memory B cells) increased susceptibility to infection by bacteria and protozoa; in particular, individuals who do not have a spleen are highly susceptible to infections 73 Giles Kisby GE Y1 CMS Immunology Cancer with encapsulated bacteria (Splenectomy greatly diminishes the frequency of memory B cells involved in defence from them) Reservoir of blood lost so more susceptible to shock if trauma etc occurs - The skin: o Involve Epidermal Langerhans cells which are a type of dendritic cell and move from skin to lymph nodes to transfer antigens to lymphocytes o Involve intraepidermal lymphocytes in the skin (most are gamma-delta-T cells) - Problem: o There are a very large number of T cells with different specificities o There are a very large number of B cells with different specificities o There may only be limited amounts of antigen o How does the body ensure that the antigen meets lymphocyte with specific receptor? - Solution: o Anatomical structure of the immune system Ensures blood and lymph are circulated to secondary tissues o Lymphocyte recirculation Lymphocytes return to blood and move to nodes in different parts of body where the infection may be - Extravasation of naïve T cells into lymph nodes: o 1. Weak selectin binding o 2. Will interact with chemokine if present on endothelium surface o 3. This, if occurs, leads to strong integrin binding causing extravasation 74 Giles Kisby GE Y1 CMS Immunology Cancer Briefly summarise the phenotype and function of cellular components of the immune system - Lymphocytes: o Small cells with agranular cytoplasm and a large nucleus o Can be subdivided into 2 groups depending on where they were produced B lymphocytes (Bone Marrow) T lymphocytes (Thymus) o Distinguished using antibody – based tests: Cluster of Differentiation (CD) is an internationally recognised systematic nomenclature for cell surface molecules used to discriminate between cells of the haematopoietic system Some useful CD markers: CD3+ T cell CD19+ CD20+ B cell CD14+ Monocyte/Macrophage CD3+CD4+ T helper cells CD3+CD8+ Cytotoxic T cell CD3-CD16+CD56+ Natural Killer cell o T lymphocytes: Thymic output declines with age 3.75 x 1011 in body, but some same as others T cells make up about 90% of blood population ~2/3 expressCD4 ie are helper T cells ~1/3 express CD8 ie are cytotoxic T cells T cells make up about 10% of blood population CD4+ = T helper cells, regulatory T cells Secrete cytokines CD8+ = cytotoxic T cells Lyse infected cells, secrete cytokines T cells only recognise processed antigen presented at the surface of another cell using T cell receptor The antigen is presented by an MHC molecule (Major Histocompatibility Complex) [class I are on all body cells - eg if become infected; class II are on immune cells] o B Lymphocytes Produced by and develop in bone marrow Surface antigen receptor : immunoglobulin like molecule Express CD markers CD19 & CD20 (not CD3, CD4 or CD8) Express MHC Class II (can present antigen to helper T cells) Effector function is to produce antibodies B cells recognise intact antigen free in body fluids (so not presented by another molecule) 75 Giles Kisby GE Y1 CMS Immunology Cancer - Use B cell receptor, a membrane anchored form of antibody linked to signalling subunits Antigen presenting cells (APC) : o APC’s are cells that can present processed antigen (peptides) to T lymphocytes to initiate an acquired (adaptive) immune response. These cells include: Dendritic cells (DC) B lymphocytes Macrophages (activated) [NB follicular dendritic cells are present in the follicles of lymph nodes and do not process antigen (like other DCs do) they just aid presentation of the antigen to the B cells] 76 Giles Kisby GE Y1 CMS Immunology Cancer [included for reference; DHTK pathways of haematopoiesis] - Take home messages: o Microorganisms are abundant in our environment, many with the ability to cause disease, and a functional immune system is essential for human health. o Historically, immune responses have been termed “innate” and “acquired” or “adaptive”: these two types of response are functional definitions, “innate” responses being present from birth, and “acquired” responses only developing after exposure to foreign “antigen”. o These two types of response are not independent systems, but work closely together to ensure successful host defence: “innate” responses are initially more 77 Giles Kisby GE Y1 CMS Immunology Cancer rapid (minutes to hours), and help to direct appropriate “acquired” / “adaptive” responses (days to weeks). o Both types of response depend on soluble factors and specialised cell types. o “Acquired” / “adaptive” responses depend on the activation of lymphocytes that express appropriate “antigen”-specific receptors: binding of antigen to the appropriate receptor activates the lymphocyte, causing cell proliferation and production of “effector” cells to fight infection. This is the principle of “clonal selection”. o “Acquired” / “adaptive” responses lead to immunological memory: this forms the basis of vaccination. o The physical organisation of the immune system is essential for effective immune responses, allowing the appropriate components to access dangerous material. o The primary lymphoid organs (thymus and bone marrow) are the sites of production and maturation of lymphocytes. o The secondary lymphoid organs (lymph nodes, spleen and mucosa associated lymphoid tissue or MALT) help antigen come into contact with lymphocytes expressing appropriate specific receptors: they are the sites of development of acquired / adaptive immune responses. o Lymphocyte numbers are carefully regulated, and lymphocytes re-circulate from blood through secondary lymphoid organs and the lymphatic system back to blood again. o When a lymphocyte encounters its specific antigen in a secondary lymphoid organ, it stops re-circulating and an acquired / adaptive immune response develops (clonal selection). o There are different lymphocyte subsets that have the same physical appearance, but can be distinguished on the basis of molecules they express on their cell surface. o Surface molecules on cells of the immune system are named using the Cluster of Differentiation (CD) nomenclature system: this was originally developed using monoclonal antibodies (see later lecture), clusters of which recognised the same cell surface molecule. o T lymphocytes express CD3 and only recognise processed antigen presented on cell surfaces by specialised molecules: B lymphocytes express CD19 and CD20 and can recognise intact, free antigen. 78 Giles Kisby GE Y1 CMS Immunology Cancer 79 Giles Kisby GE Y1 CMS Immunology Cancer 08/11/13: The innate immune system: Dr. Keith Gould [says do not have to know extensive detail – just understand how it works] Los (from slides): • • • • Explain the basic principles of innate immune responses and recall the timescales in which they occur Summarise the major recognition strategies used by the innate system to detect the presence of infection and tissue damage Explain the role of mediators of innate immunity such as complement, inflammatory cytokines and chemokines in host defence against infection List examples of disorders in which defects of innate immunity are associated with human disease Notes: Explain the basic principles of innate immune responses and recall the timescales in which they occur - Innate immunity o “inbuilt”, present from birth o not antigen-specific, but recognises pathogen-associated molecular patterns (PAMP) or damage-associated molecular patterns (DAMP) using pattern recognition receptors (PRR) o not enhanced by second exposure (has no memory) o uses cellular and humoral (soluble) components o rapid response, minutes to hours, cooperates with and directs adaptive immunity o Overlap exists between the cells of innate and adaptive immunity: 80 Giles Kisby GE Y1 CMS Immunology Cancer Summarise the major recognition strategies used by the innate system to detect the presence of infection and tissue damage - Innate immune recognition strategies: o 1. Detect conserved microbial structures (PAMP) Toll like receptors (TLR) NOD like receptors (NLR) C-type lectin receptors (CLR) RIG-I like receptors (RLR) o 2. Detect metabolic consequences of cell infection or injury (DAMP) NOD-like receptors (NLR) o 3. Detect ‘missing self’ (NK cells) MHC Class I specific receptors - Natural Killer (NK) cells o large granulated lymphocytes: cytotoxic, lyse target cells and secrete the cytokine interferon-ϒ o 5-10% peripheral blood lymphocytes o no antigen-specific receptor, but express both activating and inhibitory receptors: balance of signals determines response: Ligation of inhibitory NK receptors = inhibition of target cell killing 81 Giles Kisby GE Y1 CMS Immunology Cancer o o Ligation of activating NK receptors [“Induced self” recognition] and absence of inhibitory NK receptor binding [“Missing self” recognition] = target cell killing Missing self is due to virus downregulating self-proteins to enhance virus synth have receptors which bind to antibody-coated cells (ADCC) important in defence against tumour cells and viral infections (esp. herpes) Note: leukocytes: include lymphocytes, baso,neutro,eosino, monocytes, and macrophages. - Phagocytic cells: o neutrophil (polymorphonuclear leukocyte) 50-70% of leukocytes; short lived cells, circulate in blood then migrate into tissues; first cells to be recruited to a site of tissue damage/infection diapedesis and chemotaxis: exactly the same as for T cells except the specific selectin & integrin involved is different: 1. Weak selectin binding 2. Will interact with chemokine if present on endothelium surface 3. This, if occurs, leads to strong integrin binding causing extravasation [then chemotaxis following the chemokines] key component of host defence when many neutrophils involved, abscess filled with pus may form Antimicrobial functions: neutrophil phagocytosis (is much more effective after opsonisation): o coating of micro-organisms with proteins to facilitate phagocytosis o opsonins are molecules that bind to antigen, and also can be bound by phagocytes o antibody and complement function as opsonins o Neutrophil killing mechanisms: oxygen-independent enzymes lysozyme hydrolytic enzymes antimicrobial peptides (defensins) oxygen-dependent respiratory burst: toxic metabolites superoxide anion hydrogen peroxide singlet oxygen hydroxyl radical reactive nitrogen intermediates nitric oxide 82 Giles Kisby GE Y1 CMS Immunology Cancer o Degranulation: o Neutrophils also release an assortment of proteins in three types of granules by a process called degranulation. The contents of these granules have antimicrobial properties, and help combat infection. Neutrophil Extracellular Traps (NETs): o Activated neutrophils release granule proteins and chromatin to form extracellular fibres o Bacteria become inactivated despite not yet being phagocytosed Macrophages are less abundant, dispersed throughout the tissues; signal infection by release of soluble mediators are derived from monocytes use pattern recognition receptors to detect bacteria then release soluble mediators (cytokines) to trigger immune response Explain the role of mediators of innate immunity such as complement, inflammatory cytokines and chemokines in host defence against infection - Cytokines o General: small secreted proteins cell-to-cell communication “messengers” of the immune system generally act locally have a biological effects at very low concentrations short-lived may act in autocrine (Eg. IL-1), paracrine (eg IFNs) or endocrine fashion (eg IL-6) o o o Types of cytokine: interleukins (IL-x): between leukocytes interferons (IFN): anti-viral effects chemokines: chemotaxis, movement growth factors (eg TGFs) cytotoxic tumour necrosis factor (TNF) Examples: IL-1 ALARM CYTOKINE, FEVER TNF-α ALARM CYTOKINE IL-6 ACUTE PHASE PROTEINS, LIVER IL-8 CHEMOTACTIC FOR NEUTROPHILS IL-12 DIRECTS ADAPTIVE IMMUNITY, ACTIVATES NK CELLS Bacterial septic shock systemic infection 83 Giles Kisby GE Y1 CMS Immunology Cancer - - bacterial endotoxins cause massive release of TNF-α and IL-1 by activated macrophages increased vascular permeability severe drop in blood pressure death in about 10% of cases Dendritic cells: o Network of cells located at likely sites of infection o Recognise microbial patterns, secrete cytokines o Capture pathogens, and migrate to local lymph node to present antigens to adaptive immune system Complement: o Plays a major role in complementing the activity of specific antibody, major role in innate and antibody-mediated immunity o The term complement was first applied by Ehrlich to describe the activity in serum (lost upon heating due to denaturation but not hot enough to have destroyed the antibodies) which could complement the ability of specific antibody to cause lysis of bacteria o complex series of ~30 proteins and glycoproteins, total serum conc. 3-4 mg/ml o triggered enzyme cascade system [Components are present as inactive precursors; Initial event is rapidly amplified] o rapid, highly amplified response o components produced mainly in the liver, but also by monocytes and macrophages o o o o o o The Classical Pathway initiated by antigen-antibody complexes The Alternative Pathway direct activation by pathogen surfaces The Lectin Pathway antibody-independent activation of Classical Pathway by lectins which bind to carbohydrates only found on pathogens Classical & Alternative Pathways converge at C3 C3 leads to the final Common Pathway (late phase of complement activation) Ends with the formation of the Membrane Attack Complex (MAC) 84 Giles Kisby GE Y1 CMS Immunology Cancer o o Control is achieved by: Lability of components Dilution of components in biological fluids Specific regulatory proteins circulating, eg C1-inhibitor, Factor I, Factor H, C4-binding protein membrane bound, eg CD59 (interferes with MAC insertion) and DAF (competes for C4b) Functions of complement: Lysis Opsonisation Activation of inflammatory response (via mast cell activation and stimulating diapedesis) Clearance of immune complexes (ie antibody to a soluble antigen and needs to be cleared but is not a pathogen in itself so isn’t really opsonisation. - Mast cells (not the same as M-cells): o secrete histamine and other inflammatory mediators, including cytokines leads to vasodilation and increased vascular permeability ( shock death in extreme cases) o mucosal mast cells (lung) o connective tissue mast cells (skin and peritoneal cavity, near blood vessels) o can recognise, phagocytose and kill bacteria o can be activated by complement products (anaphylatoxins) - A local acute inflammatory response overview: o Bacteria/tissue damage leading to: Complement activation Mast cell degranulation Macrophage activation Cytokine production 85 Giles Kisby GE Y1 CMS Immunology Cancer o o - Monocyte, Neutrophil, lymphocyte diapedesis and chemotaxis [inflammatory response] [ie Neutrophils are the first cell type recruited from the circulation to a localised site of infection. Macrophages are resident in tissues] Acute-phase proteins: (looked for on blood tests): fibrinogen (clotting) complement C-reactive protein (CRP) C polysaccharide of pneumococcus activates complement level may increase 1000 fold mannan binding lectin (MBL) opsonin for monocytes, activates complement [SAA: Serum amyloid A Involved in the recruitment of immune cells to inflammatory sites] Laboratory signs of being ill C-reactive protein rises Erythrocyte Sedimentation Rate (ESR) rises Acute phase response: increases in: Ferritin rises FVIII fibrinogen immunoglobulins Prolonged innate immune responses may be accompanied by an “acute phase response”, characterised by fever and increased production of components to fight infection: 86 Giles Kisby GE Y1 CMS Immunology Cancer o (Systemic) “acute-phase” response: local inflammatory response may be accompanied by a systemic response, “acute phase” after 1-2 days induced by cytokines “acute-phase” response: fever, increased production of white blood cells (leukocytosis), production of “acute-phase” proteins in the liver List examples of disorders in which defects of innate immunity are associated with human disease - Phagocyte deficiency o is associated with infections due to extracellular bacteria and fungi: o Staphylococcus aureus Pseudomonas aeruginosa Escherichia coli Candida albicans Aspergillus flavus Deep skin infections, impaired wound healing, poor response to antibiotics - Innate immunity defects of genetic origin: o Phagocytes Chronic granulomatous disease (CGD), diseases in which reactive oxygen based killing is defective Leukocyte adhesion deficiency (LAD), lack of migration of neutrophils out of blood vessels Interferon- receptor (IFNR) deficiency, poor macrophage activation, increased susceptibility to tuberculosis o Complement Defects in components of the membrane attack complex, increased susceptibility to Neisserial meningitis - A simplification: o Cellular bacteria: phagocytes viruses: NK cells o Humoral (body fluids) bacteria: complement viruses: interferons 87 Giles Kisby GE Y1 CMS Immunology Cancer Take home messages: - - - - - Innate immunity uses germline encoded “pattern recognition receptors” to recognise “pathogen associated molecular patterns” (PAMPs): these are chemical structures found on pathogens but not on human tissue. Phagocytes are the most important cell type in innate immunity: neutrophils and monocytes / macrophages. Neutrophils are more abundant and are the first cell type recruited from the circulation to a localised site of infection. Macrophages are resident in tissues. The process of phagocytosis is much more efficient after “opsonisation”, the process of coating antigen with molecules recognised by receptors on phagocytes. In addition to killing pathogens, phagocytes signal infection has occurred by releasing soluble “messenger” molecules, called cytokines. These help to coordinate appropriate immune responses. The complement system is the major soluble effector system of innate immunity, consisting of a complex series of glycoproteins that form an enzyme cascade system. The complement system may be activated in 3 different ways: by antibody that has bound to antigen (classical pathway), by lectins that have bound to carbohydrates found on bacterial surfaces (lectin pathway), and directly by bacterial surfaces themselves (alternative pathway). Prolonged innate immune responses may be accompanied by an “acute phase response”, characterised by fever and increased production of components to fight infection. 88 Giles Kisby GE Y1 CMS Immunology Cancer 08/11/13: B cell mediated immunity: Dr. Keith Gould [says do not have to know extensive detail – just understand how it works] Los (from slides): Explain briefly the developmental and maturational pathways of B cells Summarise how B cells can recognise and respond to antigens List the immunoglobulin classes and sub-classes in man. Summarise their functions and relate these to their individual structure Compare and contrast T cell dependent and T cell independent B cell immune responses to antigen Notes: - - - Antibodies are glycoproteins (see CHO indicated on diagrams) Antibodies belong to the immunoglobulin superfamily HEAVY CHAIN (e.g. 50kDa) both the same; divided to four parts: VH, CH1, CH2, CH3 (NB IgM and IgE actually have 4 CH domains) LIGHT CHAIN (25kDa) both the same; divided to two parts: VL and CL Note that N-termini of both chains are at the variable end The variable section of antibodies contains three loops that demonstrate especially high variation; these are the CDRs (=hypervariable regions); involved in binding the epitope of the antigen Note that the T-cell receptor has a Fab-like structure (ie demonstrate homology; similar to a membrane bound Fab) Disulf bonds: o In immunoglobulin motifs o In hinge region (hinge region may be of variable size and variable number of disulf bonds depending on Ab class) o In connection between heavy and light chains Enzymes: o Pepsin (cleavage below hinge region) F(ab’)2 + Fc o Papain (cleavage above hinge region 2 x F(ab’) + Fc o B-mercaptoethanol complete separation of chains and denaturation 89 Giles Kisby GE Y1 CMS Immunology Cancer 90 Giles Kisby - GE Y1 CMS Immunology Cancer B cell development: o occurs in bone marrow: involves surface interactions with bone marrow stromal cells with and important role of cytokines (IL-7 needed for B cell development) o committed lymphoid progenitor pro-b cell pre-b cell immature b cell o is independent of antigen o - Heavy chain gene rearrangement occurs first (ie VDJ recomb gives the set of V,D,J for the variable section of the heavy chain) followed by light chain gene rearrangement (ie VJ recob only; no D involved; VJ recomb gives the set of V,J for the variable section of the light chain) CRD3 is encoded by VJ of light chain and VDJ of heavy chain Receptor diversity generated by Combination of different genes (ie 39 diff V sections, 27 diff D’s, 6 diff J’s) Random insertion of extra nucleotides at junction between gene segments (N-nucleotide insertions at points between V,D,J) baseline somatic mutation combinatorial association between different light and heavy chains ie diff options possible until the alleic exclusion occurs o Potential antibody repertoire is 1016 different immunoglobulins but not all made per person and some would recog self-tissues so would be eliminated o C regions encoded by a single gene (always only IgM & IgD chains chosen to start with). o Once functional heavy and light chain rearrangement have occurred on one allele identical gene rearrangement are silenced on second B cell allele (allelic exclusion). o Immature B cell express surface IgM o Antigen naïve B cells express IgM and IgD (IgD is involved in the development process of B cells – probably to do with the selection of B cells but this is not looked at until next term) [note that the specificities of all the antibodies (including M/D) will all be identical] o Throughout development/maturation of the B cells movement from outer edge inward occurs in the bone marrow o Mature, activated antibodies secrete IgM upon first antigen exposure but then class switching (in germinal centers) can occur; also, on a second exposure (ie memory B cell activation) IgG is the dominant antibody (most memory cells are IgG) B cell recognition and response to antigen: o B cell generation and maturation occurs in bone marrow in the absence of pathogen antigen o antigen- induced B cell activation and differentiation gives antibody production and occurs in the periphery; largely in lymph nodes o Affinity maturation (stage after DC / correct Bcell initial interaction in which binding to the antigen is attempted to be improved) and class switching (constant region may be changed to a type more suited to the specific threat as elucidated by the cytokines being produced due to the threat) both occur in the germinal centers of the lymph nodes / peripheral lymphoid organ 91 Giles Kisby GE Y1 CMS Immunology Cancer - “Somatic hypermutation” is a major component of the process of affinity maturation o The B cell receptor: Transmembrane protein complex composed of IgM [ie are not always pentameric] and Heterodimers of Igα linked to Igβ Iga/Igb heterodimers contain immunoglobulin-fold structure Iga/Igb heterodimers are functionally analogous to CD3 of T cells The cytoplasmic tail of IgM is too short to signal The cytoplasmic tails of Iga/Igb contain ITAM motifs for signalling (contain Tyrosine’s that can be phosphorylated) DIFFERENT CLASSES OF ANTIBODIES: o DIFFERENT CLASSES OF ANTIBODIES DIFFER IN THE CONSTANT REGIONS OF THEIR HEAVY CHAINS: o May also have a different number of Ab units involved o The light chains are not important here: always either kappa or lambda [total kappa to lambda ratio is roughly 2:1 in serum] o IgG and IgA have subclasses: Are still the same heavy chain groups, just numbered subtypes exist of each (see table) IgG1-4 vary mainly in their hinge region length and number of disulf bonds present there 92 Giles Kisby GE Y1 CMS Immunology Cancer o o o o o IgG Antibody heavy chain Most abundant immunoglobulin in the body Occurs as a monomer, but 4 subclasses variability mainly located in hinge region Actively transported across the placenta unlike all other Abs and therefore are the means by which infant “passive immunity” is conferred until the infants immune system can initiate Present in blood and extracellular fluids Major activator of classical complement pathway (mainly IgG1 and IgG3) Proportion of total IgG: IgG1>IgG2>IgG3>IgG4 IgA Antibody heavy chain Second most abundant immunoglobulin after IgG Occurs as a monomer (in the blood) and as a dimer (in secretions) Major secretory immunoglobulin: here is released from B cell with J (“joining”) chain giving dimeric form and upon passage through epithelium picks up a “secretory component” (derived from the receptor it bound) which confers resistance to proteases that are present on most mucosal surfaces Protects mucosal surfaces from bacteria, viruses and protozoa IgM ANTIBODY heavy chain large pentameric molecule 5 monomers joined by J chain (therefore 10 x Fab) mainly confined to blood (80%) first Ig synthesised after exposure to antigen primary antibody response multiple binding sites compensate for low affinity (other Ab types have higher affinities) efficient at agglutination (clumps together bacteria) activates complement IgD ANTIBODY heavy chain extremely low serum concentrations surface IgD expressed in B cell development involved in B cell development and activation IgE ANTIBODY heavy chain present at extremely low levels produced in response to parasitic infections and in allergic diseases binds to high affinity Fc receptors (ie IgE-FcR’s) of mast cells and basophils 93 Giles Kisby GE Y1 CMS Immunology Cancer - - cross-linking by antigen triggers mast cell activation and histamine release (histamine gives hyper-secretion of mucus, vasodilation and increased capillary permeability to white blood cells etc) Antibody Effector Functions: o Neutralization of toxins: Inhibits toxicity o Neutralization of viruses: Inhibits infectivity o Neutralization at body surfaces: Inhibits infectivity of bacteria & viruses o Agglutination: Ag-Ab complexes/Lattice formation o Opsonization: Promotes phagocytosis o Complement activation: Classical Pathway o Mast Cell sensitisation & activation: Hypersensitivity & Expulsion o NK cell: Cytotoxicity, ADCC Antibody production by B cells: o General rule: o naïve antigen-specific lymphocytes (B or T; B cells looked at here) cannot be activated by antigen alone - require accessory signal: a. Directly from microbial constituents Thymus-independent directly activate B cells without the help of T cells B cell binds to an antigen and receives secondary activation by toll-like receptors, such as TLR4 for LPS and TLR9 for DNA Only IgM No memory Can induce antibodies in people with no thymus and no T cells (DiGeorge syndrome) b. OR from a T helper cell Thymus-dependent all Ig-classes Memory The membrane bound BCR recognises antigen (= signal 1) (MHCII and B7.1&7.2 (costimulatory molecules; bind CD28 of Tcell) are upregulated) The receptor-bound antigen is internalised and delivered to intracellular sites The internalised antigen is degraded into peptides Peptides associate with “self” molecules (MHC class II) The antigen/self-complex is expressed at the cell surface T lymphocytes with a complementary antigen receptor recognise the complex; o interaction CD40L and CD40 provides signal 2 for the B cell (B cells proliferate and differentiate into antibody secreting 94 Giles Kisby GE Y1 CMS Immunology Cancer o - plasma cell (and some memory cells) and cytokine receptors will now be upregulated) B7-CD28 interaction provide costimulation for T h cells ( produce cytokines which can further aid B cell activation, determine what class switching may occur (Cytokines influence Ig-classes; class switch occurs at DNA level but variable region unchanged) and have other effects too) Immunological memory o Initial antigen contact induces a PRIMARY RESPONSE o Subsequent encounter with the same antigen will induce a SECONDARY RESPONSE which is more rapid and higher magnitude o The secondary response reflects the activity of the clonally expanded population of MEMORY B CELLS 95 Giles Kisby GE Y1 CMS Immunology Cancer [ie primary response is mainly IgM (in this case with a late class switching to IgG) then secondary response is mainly IgG, faster and higher magnitude (note the secondary response is always mainly IgG, at least initially, because most memory B cells are for IgG antibodies)] Take home messages: B lymphocytes originate and develop in the bone marrow. During the process of their development, B lymphocytes express an antigen receptor on their cell surface in the form of a membrane anchored antibody molecule. This occurs in the absence of antigen. The huge diversity of B lymphocyte antigen receptors (and antibodies) in each individual is generated by recombination of different gene segments, rather than being encoded by a very large number of genes encoding complete antibodies. 96 Giles Kisby GE Y1 CMS Immunology Cancer B lymphocytes with antigen receptors that encounter and bind to self proteins are deleted early in their development, to help prevent immune responses against self. Antibody responses are of 2 basic types, T helper cell independent and T helper cell dependent. T-independent responses are of IgM class and have no memory, T-dependent responses are of all Ig classes and show memory (secondary responses). Antibody class switching is influenced by the cytokine environment. Primary antibody responses are slower and IgM predominates early in the response, whereas secondary responses are faster, of greatly increased magnitude, and IgG predominates. Natural antibody responses against pathogens are polyclonal (many specificities), but monoclonal antibodies (single specificity) may be produced artificially. An antibody is a soluble glycoprotein that is produced in response to a foreign molecule (antigen), and has the property of binding to that antigen. Antibodies form the class of proteins known as immunoglobulins, and are produced by B lymphocytes. Each individual has the capacity to produce a great diversity of antibodies, to fight different infections. Antibodies can be thought of as adaptor molecules, a variable part that binds to antigen, linked to a more constant part involved in biological function, such as activation of the complement system. Antibodies bind to antigen using non-covalent bonds: individually these are weak, but many interactions are involved so that overall binding may be very strong. Because non-covalent bonds only act over short distances, the shapes of antigen and the antigen-binding surface of the antibody must be closely complementary. There are different classes and sub-classes of antibodies in man: these differ in their constant regions, and have subtly different structures, functions, and locations in the body. In addition to their roles in host defence, antibodies are highly useful tools in medicine, for diagnosis and therapy. Antibodies against virtually any molecule may be generated artificially. 97 Giles Kisby GE Y1 CMS Immunology Cancer 19/11/13: T cell mediated Immunity: Prof Julian Dyson Los (from slides: these are the Los to be tested): Links between innate and adaptive immunity Role of dendritic cells in initiation of immunity Stages of T cell response to infection Role of host genetic polymorphism on disease susceptibility Notes: - - - Variability in susceptibility/host response to an infection: o General health and nutrition status o Previous exposure (memory) o Immune-deficiencies – genetic or acquired (HIV) o Polymorphisms in innate immunity genes o Polymorphisms in adaptive immunity genes, particularly HLA (=‘human leucocyte antigens’) Adaptive immunity is a ‘recent’ evolutionary device for host defense (500 million years) Though innate immunity is ‘primitive’, we depend on the interplay between innate and adaptive immunity Commensal microbiota o Commensal microbiota are essential for tissue integrity and immune function This partnership, forged over many millennia of coevolution, is based on a molecular exchange involving bacterial signals that are recognized by host receptors to mediate beneficial outcomes for both microbes and humans. Symbiosis eg: Clostridium forms a thick colonizing layer on the epithelium and enhances release of TGF-β and indoleamine 2,3-dioxygenase (IDO) from epithelial cells. [ie TGF-β encourages naïve T cells to become Treg thereby giving immunosuppressive environment (is often bad for the person to give inflam response etc)] Disordered microbial communities in disease: eg altered microbiota from the norm found in asthmatic airways o Host barriers to colonisation by pathogenic microbes: Structural barriers: skin, mucous membranes, respiratory cilia Competition with commensal microbiota for niches Chemical – eg low pH of stomach 98 Giles Kisby GE Y1 CMS Immunology Cancer - Anti-microbials - lysozyme in mucous sectretions, -defensins (intestine), -defensins (respiratory and skin) Collectins - Lung surfactant proteins A and D, mannose binding lectin (MBL) Collectins are soluble pattern recognition receptors (PRRs). Binding of collectins to microorganisms may trigger elimination of microorganisms by aggregation, complement activation, opsonization, activation of phagocytosis or inhibition of microbial growth. and interferons Complement activation Neutrophils Monocytes Natural killer cells NKT cells Links between innate and adaptive immunity: o INNATE Very rapid Many components Evolutionarily ancient (conserved) Lack of specificity Lack of memory o ADAPTIVE Slower Specific: antibody (B cell) : cellular (T cell) Multiple effector mechanisms Targeted to a specific antigen Memory o Immune deterioration (elderly)/ill health/poor nutrition/poor sanitation: increases infection risk o Neutrophil Most abundant white blood cell characteristic cell of the acute inflammatory infiltrate; phagocytoses bacteria; makes toxic products - defensins and peroxide, bactericidal enzymes o Monocyte (or in tissues, macrophage) Phagocytose and kill pathogens - activated by toll-like receptor recognition Release cytokines IL-1, IL-6, IL-8, IL-12, TNFα o Natural killer (NK) cells A lymphocyte population (but non B/T) Uses an array of cell surface receptors to scan for pathogen-associated molecular patterns (PAMPs) 99 Giles Kisby GE Y1 CMS Immunology Cancer Acts by direct killing (release of cytolytic granules) and cytokine release (interferon-) o o - NKT cells use a semi-invariant ab TCR to recognise microbial lipid antigens Secrete large amounts of gamma interferon: ie IFN-gamma Most pathogenic microbes do not kill Yersinia pestis Plague (~50% mortality) Bacillus anthracis Anthrax (~50% mortality) Killing is due to only recently starting to infect humans so no defence as yet; evolved in other species instead Adaptive immune response to microbes: o Dendritic cell The bridge between innate immunity and T cell activation in the immune response. Professional antigen presenting cells for priming naïve T cells. Respond to TLR activation, interferon Actions: phagocytosis [Main function of phagocytosis for antigen processing compared to neutrophils where Main function of phagocytosis for pathogen removal] antigen processing o B cells recognise external determinants that are exposed on the native molecule therefore antigen presentation to them is not needed o T cells recognise internal determinants of folded protein antigens hidden when the protein is in its native conformation therefore prior to T cell antigen recognition, antigen “processing” step is required: o This involves: 100 Giles Kisby GE Y1 CMS Immunology Cancer o o internalisation (phagocytosis) denaturation of the antigen proteolytic digestion presentation by MHCII (see below) Antigen presentation by MHC Class II: MHCII bound to invariant chain in ER to prevent binding to endogenous proteins golgi endolysosomal compartment where phagocytosed fragments end up invariant chain degraded allowing exogenous proteins to bind surface presentation Is 2x TM CD4 coreceptor allows binding to MHCII Antigen presentation by MHC Class I: Cytoplasmic protein degraded at proteasome peptides pass through TAP (transporter associated with antigen processing) to enter ER peptides attached to MHCI pass via golgi to be presented on surface Is 1x TM CD8 coreceptor allows binding to MHCI activation (via PAMP recognition) [prob then cytokine release etc] o Naïve T cells can only be activated by activated dendritic T cells 101 Giles Kisby GE Y1 CMS Immunology Cancer o o Pattern associated molecular patterns (PAMPs) are ‘read’ by Toll like receptors (TLRs) on dendritic cells leading to DC activation [upregulation of CCR7 (better exit at secondary lymphoid organs), B7.1/2 (costim molecules), MHCI/II; also depending on what PAMPs are detected different cytokines will be produced] and appropriate T cell differentiation migration to LN to present antigen o Migrated T cells present antigen to naïve T cells in draining lymph node: ie DCs access the lymph nodes via the afferent lymphatic vessels when are bringing antigen for T cell activation o Priming = The activation and differentiation of naïve T cells (as triggered by the dendritic cells) o Following the 3x signals that prime the T cell: T cell L-selectin is downregulated (L-selectin holds the T cells in the lymph nodes) T cell VLA-4 is upregulated: allows extravasation of the T cells at tissues [involves rolling, tethering, extravasation then migration to infection through tissues is by chemotaxis] T cell: Key cell-type mediating the adaptive immune response. Recognise peptidic fragments of foreign antigen presented by HLA molecules on antigen presenting cells. Leads to activation, cytokine release, killing, B cell help etc Signal 3 is the cytokine environment as established by the APC; determines what type of T cell differentiation occurs to: 102 Giles Kisby - GE Y1 CMS Immunology Cancer Role of host genetic polymorphism on disease susceptibility: o Certain MHC I/II variants give different conferred susceptibility / resistance to different pathogens 103 Giles Kisby GE Y1 CMS Immunology Cancer 10/01/14: Immune response to infection: Julian Dyson Los from slides: Give a brief overview of characteristics of the adaptive immune system. Describe the generation of antigen specific T and B cell receptors Describe how T cells and B cells recognise antigens Outline the principles of T cell development and maturation Los (from booklet): Lecture 5 – Immune response to infection initial events during the immune response to infection. and helminths. tures which prompt consideration of an underlying immune deficiency, listing examples of primary and secondary immune deficiencies. Notes: - In all cases D J occurs first then V DJ - NK cells = CD 16 - T cells = CD3 - NKT cells = CD16 and CD3 - TCR = alpha and beta chains; VDJ recombination occurs on both chains o o This VDJ region corresponds to CDR3 which recognises the peptide on the MHC molecule CDR 1 and 2 are germline encoded and recognise the MHC molecule itself 104 Giles Kisby GE Y1 CMS Immunology Cancer o MHC i/ii recognition / distinguishing is in this manner and via cd8/4 interactions with the mhc of that cell BCR - Light chain = VJ recomb Heavy chain = VDJ recombination BCR Fab fragment is homologous to TCR BCR also has CDR1/2/3 but all are involving recognising the target antigen (CDR 1 and 2 are prob still germline encoded though) Mhc i: - All cells Vs viruses Cd8+ recruited ‘closed’ antigen binding groove at each end Extensive polymorphisms observed at MHC peptide binding groove Cytosolic prot proteasome TAP ER mhc I surface TCR of cd8+ Mhc ii - APCs Endocytosed antigen ‘open’ antigen binding groove at each end Extensive polymorphisms observed at MHC peptide binding groove Endocytosis degradation mhcii recruited to endosome, invariant chain removed and antigen loaded presented at surface for CD4+ Central / primary tolerance: - For T cells occurs in thymus: o Neither CD4/8 both CD4 & 8 [positive selection occurs] CD 4 OR 8 [negative selection occurs] o AIRE = autoimmune regulator = a TF of medullary epithelial cells that expresses body antigens to facilitate selection events AIRE mutation gives APECED: Autoimmune PolyEndocrinopathy105 Giles Kisby GE Y1 CMS Immunology Cancer Candidiasis Ectodermal Dystrophy (autoimmune polyglandular disease, or APD) = Rare autoimmune disease which affects the endocrine glands: Thyroid Kidneys Chronic mucocutaneous candidiasis Gonadal failure Diabetes mellitus Pernicious anaemia - vitiligo (depigmentation of the skin) alopecia (baldness) o Thymic epithelial cell (TEC) or Dendritic cell (DC) present antigen on MHC in the thymus For B cells occurs in BM: o Both neg and pos selection occur o Receptor editing / anergy / apoptosis if self recog Peripheral / secondary tolerance: - - - - T cells have raised threshold for activation outside thymus T/B cell may never encounter target: ignorance (eg CD4+ cells need to have it presented but won’t happen properly with self cell antigens) o Occurs when relevant antigen presenting molecule is absent: most cells in the periphery are MHC class II negative o Failure of Ignorance: Example: sympathetic ophthalmia: damage to one ege give autoimmunity to both eyes (active immune cells can enter etc) Immunoprivaledged sites: CNS, PNS, testes Anergy occurs if innate signalling is not also occurring Tregs: o Fox P3+ Treg cells are present in the periphery o Regulatory T-cells = CD4+CD25+CTLA-4+FOXP3+ CD25 is the Interleukin-2 Receptor CTLA-4 binds to B7 and sends a negative signal FOX P3 is a transcription factor required for regulatory T-cell development Exposure to antigens soon after birth can lead to tolerance of those antigens via unclear mech [tolerance is acquired and active in neonates] Tolerance Dysfunction: 106 Giles Kisby GE Y1 CMS Immunology Cancer o o o - Autoimmune diseases result from a loss of tolerance vs self tissues IPEX: a failure in the regulation of peripheral tolerance = Immune dysregulation, Polyendocrinopathy, Enteropathy and X-linked inheritance syndrome Fatal recessive disorder presenting early in childhood Mutation in the FOXP3 gene which encodes a transcription factor critical for the development of regulatory T-cells Accumulation of autoreactive T cells occurs Symptoms include: early onset insulin dependent diabetes mellitus severe enteropathy eczema variable autoimmune phenomena severe infections How can infections affect the tolerant state?: Molecular mimicry of self molecules Induce changes in the expression and recognition of self proteins Induction of co-stimulatory molecules or inappropriate MHC class II expression: pro-inflammatory environment Failure in regulation : effects on regulatory T-cells Immune deviation: shift in type of immune response e.g. Th1-Th2 Tissue damage at immunologically privileged sites Take home messages: 107 Giles Kisby GE Y1 CMS Immunology Cancer 108 Giles Kisby GE Y1 CMS Immunology Cancer 10/01/14: Tolerance and Autoimmunity: Dr Keith Gould Los (from booklet): Lecture 6 – Tolerance and Autoimmunity List some examples of systemic and organ-specific autoimmune diseases. Notes: - Summary: human autoimmune reactions o Mechanisms in autoimmunity are the same as in normal responses against foreign antigens o Immune responses to autoantigens (self) have a direct role in the pathology of autoimmune diseases o Both B cells (antibody) and T cells can be involved o HLA associations strongly imply a role for T cells in initiating autoimmune disease - Autoimmunity: o Are examples of hypersensitivity reactions, types II, III, and IV (though these hypersensitivity groups can also refer to non-autoimmune disease) o Because self tissue is always present, autoimmune diseases are chronic conditions o most more common in females: exception = T1D - Autoimmunity is caused by: o genes being a woman means higher oestrogen levels which increased sensitivity through unknown mech Human MHC (HLA) is the dominant genetic factor affecting susceptibility to autoimmune disease o infections 109 Giles Kisby GE Y1 CMS Immunology Cancer o - Viruses give inflammation and this in turn can act a trigger for autoimmunity Environment Hygiene has been linked to autoimmunity, not just to type I hypersensitivities Will likely be an exam question, he strongly hinted we may be asked to list autoimmune diseases and give egs of systemic and organ specific: o systemic vs organ specific is a sliding scale ~but: systemic = SLE, RA organ specific = Grave’s, hashimoto, TID, Goodpasture’s - Hypersensitivity: Classified by Gell & Coombs into 4 types: o Type I: immediate hypersensitivity, IgE mediated Anaphylaxis Asthma Rhinitis Seasonal (hay fever) Perennial (house dust mite) Food Allergy o Type II: antibody binds to cell or matrix associated antigen, IgG mediated Goodpastures 110 Giles Kisby GE Y1 CMS Immunology Cancer o Vs TIV collagen of basement memb: greatest effect at kidney to inc GFR; triggers inflam and complement too Graves Anti TSH R antibodies activate the receptor hyperthyroid Type III: antibody binds to soluble antigen, IgG mediated SLE: immune complexes vs soluable antigen mean SLE is systemic: glomerulonephritis [immune complex deposition in glomerulus], vasculitis, arthritis Genes affected are involved in: o induction of tolerance (B lymphocyte activation: CD22, SHP-1): autoantibody production o apoptosis (Fas, Fas-ligand): failure in cell death o clearance of antigen (Complement proteins C1q, C1r and C1s): abundance/persistence of autoantigen o Type IV: delayed hypersensitivity, T cell mediated Non T cell responses can be involved too TID RA MS 111 Giles Kisby GE Y1 CMS Immunology Cancer 112 Giles Kisby GE Y1 CMS Immunology Cancer 10/01/14: Allergy and Transplantation: Dr Keith Gould Los (from booklet): Lecture 7 - Allergy and Transplantation loantigens. treat graft rejection. Notes: - Type I hypersensitivity: o Expression of disease requires two exposures 10 Antigen exposure IgE antibody production IgE binds to Mast Cells & Basophils 0 2 Ag Exposure More IgE Ab produced 113 Giles Kisby GE Y1 CMS Immunology Cancer o o Antigen cross-links IgE on Mast Cells/Basophils Degranulation: Both preformed (eg histamine) and newly synthesised compounds (eg PGs and leukotrienes) are released Predisposition to become IgE-sensitized to environmental allergens is called atopy prevalence of atopy is 50% in young adults in UK Polygenic: Prob downreg: IL-4 mutation: linked to raised IgE, asthma, atopy Prob upreg: IgE receptor mutations: linked to atopy and asthma risk factors Age - increases from infancy, peaks in teens, reduces in adulthood Gender - asthma more common in males in childhood, females in adults Family size - more common in small families Infections - early life infections protect Animals - early exposure protects Diet – breast feeding, anti-oxidants, fatty acids protect Types: Anaphylaxis Asthma Rhinitis Seasonal (hay fever) Perennial (house dust mite) Food Allergy Anaphylaxis severe generalised allergic reaction Symptoms: o itchiness around mouth, pharynx, lips o swelling of the lips, throat and other parts of the body o wheeze, chest tightness, dyspnoea o faintness, collapse o diarrhoea & vomiting o death if severe & untreated Systems: o Cardiovascular - vasodilatation, cardiovascular collapse o Respiratory - bronchospasm, laryngeal oedema o Skin - vasodilatation, erythema, urticaria, angioedema o GI - vomiting, diarrhoea Asthma Acute inflammation of the airways o mast cell activation and degranulation Pre-stored mediators histamine Newly synthesised mediators 114 Giles Kisby GE Y1 CMS Immunology Cancer - prostaglandins, leukotrienes o acute airway narrowing Chronic inflammation of the airways o Cellular infiltrate: Th2 lymphocytes, eosinophils o Smooth muscle hypertrophy o Mucus plugging o Epithelial shedding o Sub epithelial fibrosis General clinical details: o Reversible generalised airway obstruction o Bronchial hyperresponsiveness o Cough o Breathlessness o Chest tightness Rhinitis Seasonal (hay fever) Perennial (house dust mite) Symptoms o sneezing o rhinorrhoea o itchy nose, eyes o nasal blockage, sinusitis, loss of smell/taste Food Allergy Mild o Itchy lips, mouth, angioedema, urticaria Severe o Nausea, abdominal pain, diarrhoea o Anaphylaxis Type IV Delayed Hypersensitivity Responses [ie note that some diseases are share with other classes]: o Three Main Varieties Th1 Cytotoxic Th2 o Mechanisms Th cell activation of other cells: macrophages, CTLs T cell cytokines giving tissue damage: Much of tissue damage dependent upon TNF-α FGF gives Angiogenesis and Fibrosis o TID o RA 115 Giles Kisby GE Y1 CMS Immunology Cancer o o o o MS Hashimoto Crohns Contact dermatitis eg nickel o o o o o o o Chronic graft rejection Graft versus host disease (GVHD) Coeliac disease Contact hypersensitivity Asthma Rhinitis Eczema o Chronic graft rejection Graft types: Autografts: within the same individual (e.g. vein, skin) Isografts: between genetically identical individuals of the same species Allografts: between different individuals of the same species Xenografts: between individuals of different species (e.g. heart valve) Prosthetic graft (plastic, metal) The immune system recognises someone else’s organ as foreign 1. ABO blood group 2. HLA (human leukocyte antigens) encoded on chromosome 6 by Major Histocompatibility Complex (MHC) 1. ABO blood group 116 Giles Kisby GE Y1 CMS Immunology Cancer o A and B proteins on red blood cells but also endothelial lining of blood vessels in transplanted organ o Naturally occurring anti-B antibodies in A patients and vice versa etc; O patients have both anti-A and anti-B: Activates complement Complement mediated lysis Increased permeability Other cells rapidly recruited agocytes Disruption of endothelium Platelets activated Inflammation Thrombosis Hyperacute rejection [see other types below]] o In recent years, it has become possible to remove the antibodies in the organ recipient with good outcomes [ie even though the patient and donor bloods did not match] 2. HLA (human leukocyte antigens) o Cell surface proteins o Highly polymorphic o encoded Major Histocompatibility Complex (MHC) genes: [HLA molecules present processed fragments of antigens for possible recognition by the immune system] Class I HLA-A HLA-C HLA-B Class II HLA-DR HLA-DQ HLA-DP Highlighted are the HLA’s that are particularly important and which are typed and used to determine compatibility of transplants Ie HLA matching in organ allocation 117 Giles Kisby GE Y1 CMS Immunology Cancer Rejection types: Hyperacute rejection acute T-cell mediated rejection o Recognition of donor HLA antigens by CD4+ T cells o Activation of CD4+ cells Production of cytokines Help for CD8+ cells Help for B cells Recruitment and activation of macrophages and neutrophils acute antibody-mediated rejection o Antibody against graft HLA and AB antigen o Antibodies arise Pre-transplantation (“sensitised”) Post-transplantation (“de novo”) chronic rejection Rejection signs: Clinical o Kidney - creatinine o Liver - liver function tests o Pancreas – serum amylase and lipase, glycaemia Prevention of rejection Maximise HLA compatibility Life-long immunosuppressive drugs Treatment of rejection Increased immunosuppression 118 Giles Kisby GE Y1 CMS Immunology Cancer o o o o o o o o - Target T cell activation and proliferation Target B cell activation and proliferation, and antibody production Base-line immunosuppression: o Signal transduction blockade, usually a calcineurin inhibitor: Tacrolimus or Cyclosporin; sometimes mTOR inhibitor (Rapamycin) o +/- antiproliferative agent: Mycophenolate mofetil (MMF) or Azathioprine o +/- corticosteroids Treatment of episodes of acute rejection: o Cellular: steroids, anti-T cell agents o Antibody-mediated: give IVIG, plasma exchange, anticomplement C5 Immunosuppression risks: o Infection o Tumours o Drug toxicity Graft versus host disease (GVHD) Coeliac disease Contact hypersensitivity Eg nickel Asthma Rhinitis Eczema Take home messages o Hypersensitivity reactions are inappropriate adaptive immune responses against harmless environmental and self antigens: allergies and autoimmune diseases are hypersensitivity reactions. o Hypersensitivity reactions may be classified into 4 main types (I to IV) based on the immunological mechanisms involved. In practice, many conditions involve a mixture of different types, rather than a single type of reaction. o Genetic and environmental factors are involved in the risk of developing hypersensitivity reactions. o Type I reactions are immediate hypersensitivity reactions, and involve specific IgE production: allergies including asthma and hay fever are predominantly type I reactions. o Type II reactions involve autoantibodies (often IgG) binding to insoluble antigen on cell surfaces or extracellular matrix, and include some organ-specific autoimmune diseases. 119 Giles Kisby GE Y1 CMS Immunology Cancer o o - Type III reactions are immune complex-mediated reactions, in which autoantibodies bind to soluble antigen. Subsequent deposition of immune complexes causes immune activation and inflammation. Type IV reactions are immune cell-mediated delayed type hypersensitivity reactions. Take home messages o Organs are transplanted when they are failing or have already failed, or for reconstruction, for example after physical injury. Transplantation may be life-saving or life-changing. o Transplants may be within the same individual (autograft), between genetically identical individuals (isograft), between genetically different individuals (allograft), or even between species (xenograft). o For organs, the most common type of transplant is an allograft, from either a deceased or living donor: living donors are often a family member of the patient. o The most important protein variations in clinical transplantation that can lead to immunological rejection are the ABO blood group antigens and the Human Leukocyte Antigens (HLA), the name of the human MHC antigens. o Depending on the organ transplanted, minimising HLA differences between donor and recipient improves transplant outcome: complete matching is rarely possible, and therefore immunosuppressive treatment must be used to prevent transplant rejection. o The major problems in transplantation are a shortage of donor organs, graft rejection, and side effects from immunosuppression: increased susceptibility to infections and malignancy. Useful images: 120 Giles Kisby GE Y1 CMS Immunology Cancer 121 Giles Kisby GE Y1 CMS Immunology Cancer 122 Giles Kisby GE Y1 CMS Immunology Cancer Reduced lipoate is with 2H; oxidised is without 2H TPP = THIAMINE PYROPHOSPHATE [succinyl-CoA synthetase] 123 Giles Kisby GE Y1 CMS Immunology Cancer [and acyl coA synthetase] 124 Giles Kisby GE Y1 CMS Immunology Cancer 125 Giles Kisby GE Y1 CMS Immunology Cancer 126 Giles Kisby GE Y1 CMS Immunology Cancer Cancer: 10/01/14: Cellular Pathology of Cancer: Gerry Thomas, Los (from booklet): differentiation and development stage. s. metastases. loring Los (from slides): - Understand the nomenclature that differentiates malignant and benign cancers and their differentiation and development stage. Describe the microscopical features of carcinomas. Describe the mechanisms of invasion and metastasis and the factors that affect sites of metastases. Explain the terms 'grading' and 'staging', and how this relates to clinical outcome Notes: - Overview: o Non neoplastic lesions metaplasia, dysplasia, hamartoma o Neoplastic lesions benign vs malignant tumour nomenclature of tumours histopathological grading of tumours histopathological and clinical staging of tumours 127 Giles Kisby GE Y1 CMS Immunology Cancer - By end of lec should know the definitions of: o Metaplasia, dysplasia, neoplasia, tumour, malignancy, hamartoma o Carcinoma, sarcoma, teratoma, lymphoma, leukaemia, metastasis - Metaplasia: o A reversible change in which one adult cell type changes to another cell type e.g. squamous metaplasia: change to a stratified squamous epithelium from either transitional (bladder) simple columnar (gall bladder) o Distinguished from neoplasia as: does not involve excess proliferation cells remain differentiated reversible o eg Barrett Esophagus [goblet/columnar gut-like structures] - Dysplasia: o an abnormal pattern of growth in which some of the histological features of malignancy are present o pre-invasive stage o Intact basement membrane [ie lacks invasiveness] o Loss of architectural orientation o Loss in uniformity of individual cells o Variability in size and shape o nuclei hyperchromatic, enlarged o mitotic figures abundant, in places where not usually found o Common sites: CERVIX - HPV infection BRONCHUS - Smoking COLON - UC LARYNX - Smoking STOMACH -Pernicious Anaemia OESOPHAGUS- Barrett's metaplasia - Hamartoma: o Term used for tumour-like malformations in which there is a relative overgrowth of part of a tissue with disorderly structural arrangement 128 Giles Kisby GE Y1 CMS Immunology Cancer o Eg vascular origin = haemangioma o Eg naevus of skin: mole/birth mark; cf skin cancer - Benign neoplasm: [neoplasm = “new growth”] o Loss of growth control o Loss of feedback regulation by cell products o Normal regulation of motility o Mostly slow growth o Growth expansive, non destructive, non invasive Well differentiated; normal cells, resembles architecture of host tissue Non metastatic Rarely fatal o Benign neoplasms do not kill unless... In a dangerous place; damage from compression e.g. meninges, pituitary secretes something dangerous e.g. insulinoma gets infected eg bladder bleeds eg benign gastric muscle tumours ruptures eg cysts of ovary, liver adenoma - Malignant neoplasm: o Loss of growth control o Loss of feedback regulation by cell products o Loss of regulation of motility o Frequently rapid growth o Growth invasive and destructive Many mitoses (ie high growth rate) Poorly differentiated, pleomorphic, abnormal cells Metastatic Invariably fatal if untreated 129 Giles Kisby - GE Y1 CMS Immunology Cancer Naming tumour types o + “oma” for benign o + “carcinoma” – malignant epithelial o + “sarcoma” – malignant connective tissue Eg Squamous Squamous cell papilloma Squamous cell carcinoma Eg Glandular Adenoma Adenocarcinoma o Papilloma: surface epithelium o o Adenoma: glandular epithelium – commonly thyroid, stomach, pancreas, parathyroid, breast, colon etc – may secrete hormones (e.g. insulinoma or glucagonoma in pancreas) Exceptions: [tumours of pigment, neural tissue, Lymphoreticular and Haematopoietic] Pigment cells pigmented cell naevus Malignant melanoma Glial tissue Glioma Malignant glioma Nerve cells Neuroblastoma - – commonly skin, bladder, colon Lymphoreticular Malignant: Hodgkin’s Lymphoma; Non Hodgkin’s Lymphoma; Myeloma Haematopoietic Malignant: Acute Lymphoblastic Leukaemia (ALL); Chronic Lymphoblastic Leukaemia (CLL); Acute Myeloid Leukaemia (AML); Chronic Myeloid Leukaemia (CML) Examples of usage / naming (prob good to learn if pos): o Epithelial tissue tumours: o Connective tissue tumours: 130 Giles Kisby GE Y1 CMS Immunology Cancer o - - - Embryonic tissue tumours: Facts about leukaemias and lymphomas o Tumours of white blood cells o Leukaemia a malignant tumour of primitive bone marrow derived cells which circulate in blood stream. o Lymphoma is a malignant tumour of lymphocytes proliferating (usually) in LNs. Facts about teratomas o A teratoma is a tumour derived from germ cells, which has the potential to develop into tumours of all three germ cell layers - ectoderm, mesoderm, endoderm o Common in the gonads, but occur in midline situations Pituitary, pineal, mediastinum, sacrococcygeal areas o Gonadal teratomas in males, all malignant in females, most are benign “Carcinoma in situ” vs invasive o “Carcinoma in situ”: Malignant epithelial cells are still separated from the adjacent tissue by the basement membrane and do not invade the underlying tissue. o Invasive carcinoma Invasion of underlying tissue by cells which have penetrated the basement membrane 131 Giles Kisby GE Y1 CMS Immunology Cancer - Cells lose adherence, become motile, penetrate the basement membrane, produce proteolytic enzymes that dissolve the ground substance in the adjacent tissues Clinical sign of invasion: fixation to surrounding structures Metastasis: o development of secondary tumours at sites remote from the primary e.g. colonic cancer metastases via the portal vein to the liver o not all malignant cancers metastasise extensively e.g. basal cell carcinoma (cf later lec) o associated with genetic changes ability to penetrate vessels and to exit vessels ability to survive in the circulation ability to colonise o routes of travel via blood vessels to organs via lymphatics to lymph nodes transcoelomic - across body cavities (eg through peritoneum) iatrogenic (by doctors during surgery) o In general: carcinomas spread first via lymphatics sarcomas spread first via blood vessels o Common/rare sites etc: liver, bone, brain, lymph nodes - common sites spleen, skeletal muscle, heart - rare sites the primary sites of carcinomas that commonly go to bone are: breast, prostate, kidney, thyroid, lung - Effects of tumour on host: o Local: Obstruction, Ulceration Infection Invasion of local structures o Systemic: Weight loss; Anorexia ~ cachexia Anaemia and other haematological effects Immunosuppression (either from tumour or treatment) Systemic infections 132 Giles Kisby GE Y1 CMS Immunology Cancer Endocrine effects: hormone products of endocrine tumours - more common in benign than malignant ectopic hormone production by tumours of cells not normally producing hormones “paraendocrine syndromes” - Grading vs staging of tumours o how bad is the primary tumour? = grade o how far has it spread? = stage [this is the most important] - Grading vs staging of tumours o how bad is the primary tumour? = grade Defined by: architectural pattern of the tumour nuclear size and nuclear : cytoplasmic ratio (high prob bad) number and type of mitoses similarity to the cell type from which they have arisen [nb the criteria differ according to the cell type of origin] well grade = 1 moderately = grade 2 poorly = grade 3 Grade has been shown to demonstrate strong links to cancer survival o how far has it spread? = stage [this is the most important] Assessment of the size and extent of the spread of a tumour. clinical examination radiology operative assessment pathology Grading is I IV The aim of any staging system is: to provide prognostic information to plan most appropriate treatment (grade proportional to how extreme the treatment selected is) TNM system for staging: T - tumour size and local extent N - local lymph node spread M - metastases Some tumour types have specific staging systems Grade has been shown to demonstrate very strong links to cancer survival - stratified medicine (~personalised medicine): 133 Giles Kisby GE Y1 CMS Immunology Cancer o o o Past: cancer therapy just targeted all dividing cells; high side effects Now specific receptors on the tumours are targeted Not all cancers of the same type have the same surface molecules: ie personalised medicine; must treat the cancer specific to that patient Eg not all breast cancer has the oestrogen receptor so would just be getting the side effects with no benefits Ie in many breast cancers want to block the signalling at the receptor as this is the mechanism for the cancer; however in other breast cancers a downstream signalling molecule may be constit active so blocking the receptor will not help Stumbling blocks Research so far concentrates on DNA mutation – easier to do, and possible to do by high throughput methods Do we sequence individual genes, or sequence whole genome and select areas for analysis, or target sequencing Cost – who pays? Urgent need to validate assays and ensure that molecular testing is QA’d appropriately Should we carry out tests on all patients or use clinical parameters to prioritise expensive tests? Spanner in the works – tumour heterogeneity. Tests carried out small sample of tumour How many samples from each patient should we sample to be sure we give the right treatment? 134 Giles Kisby GE Y1 CMS Immunology Cancer 16/01/14: Breast Cancer: Gerry Thomas Los (from booklet): Breast Cancer • Understand the types of breast cancer and how it is treated • The differences between hormone and chemotherapy • The mechanisms by which oestrogen receptor signalling can be disrupted • How biology affects prognosis Los (from slides): • • • • Understand the types of breast cancer and how it is treated The differences between hormone and chemotherapy The mechanisms by which oestrogen receptor signalling can be disrupted How biology affects prognosis Notes: - Key points to remember o Breast cancer prognosis depends on grade, stage, ER status and molecular phenotype o Molecular subtype related to grade and age o Anti-ER therapy important in ER positive disease o Molecular targeted therapies being developed for different subtypes – need to have predictive tests to stratify patients - Misc stats: o Breast cancer is the leading female cancer o Breast Cancer Incidence is rising o Breast cancer mortality is falling - Risk factors: (+ or - ) o + western diet o + weight [but only a RF if post menopausal] or height o + alcohol o – fibre o – fresh fruit / veg o + family history 135 Giles Kisby GE Y1 CMS Immunology Cancer o o o o o + radiation + early age of first period or late age of menopause + nulliparity (no children) or older age of first birth + age (but higher incidence is mainly due to experiencing the given risk for more years) + certain gene mutations: [these are all involved in other cancers too] BRCA 1 / 2 [its implications for ovarian cancer risk are at least as dangerous] P53 PTEN [tumor suppressor phosphatase; see cell cecle lecs] Acts in opposition to PI3K ATM [Ataxia telangiectasia mutated: gives cell cycle arrest in healthy persons in response to double strand breaks] - NB also: Key pathways involved in breast cancers: [note: MAPK pathway is more applicable to skin cancers; less relevant here] o HER2 ie EGFR pathway Use anti-EGFR drugs eg antibodies: Herceptin o mammalian target of rapamycin (mTOR) regulates cell growth, cell proliferation drug: Rapamycin derivatives [to reduce mTORC2 signalling] o PI3K signalling anti-PI3K drugs acts in opposition to PTEN o ER Tamoxifen o Ki67 (have a high number of cancer cells actively dividing) The Ki-67 protein is a cellular marker for proliferation - Breast cancer treatment o Surgery o Endocrine therapy [ie Oestrogen withdrawal or anti-oestrogens vs estrogen receptor positive cancers eg Tamoxifen] o Radiotherapy o Chemotherapy [used on top of endocrine therapy in estrogen receptor positive cancers but gives increasingly little further advantage with age (prob due to decreased tolerance to the chemo)] o Targeted agents (e.g. Herceptin [monoclonal antibody that interferes with the HER2 receptor]) - Histological subtypes 136 Giles Kisby GE Y1 CMS Immunology Cancer o o Ductal Clumps of cells Lobular Lines of cells / linear arrangement of cells o By grade: Higher grade if more mitoses and greater change in appearance from normal sparse cell arrangement: o By molecular subtypes: Luminal A ER+, PR+, HER2 - (nb ie estrogen receptor positive; progesterone receptor-positive) Luminal B ER+, PR+, HER2+ Triple negative/basal-like ER-, PR-, HER2HER2 type ER-, PR-, HER2+ Prognosis o determined by: tumour size, grade, Age, axillary node status 137 Giles Kisby GE Y1 CMS Immunology Cancer greater spread to nodes indicates a worse prognosis ER, [better prognosis]: [if is expressing estrogen receptor (as a means of giving the cancerous prolif)] over expressed in around 75% of breast cancers A) is biologically a less aggressive tumour type than non-ER B) gives inc treatment options: o Oestrogen withdrawal (eg ovary removal) or competition for binding to the ER using anti-oestrogens (eg tamoxifen) results in a response in about 70% of ER-positive cancers o Oestrogen withdrawal: Ovary removal LHRH agonists [Luteinizing-hormone-releasing hormone = GnRH: responsible for the release of (FSH) and (LH) from the anterior pituitary which than would give oestrogen production at ovaries] Aromatase inhibitors: Aromatase is the enzyme that synthesizes estrogen at ovaries and the adrenal glands [ie here more important in post menopausal women] Before menopause (pre-menopause) oestrogen is made mainly by the ovaries. After menopause (post-menopause), the body still makes small amounts [ie lower levels so LH and FSH rise] of oestrogen by changing hormones called androgens into oestrogen. Androgens are produced by the adrenal glands, which are above the kidneys. A hormone called aromatase changes androgens into oestrogen. Aromatase is produced mainly by fatty tissue Other biological factors such as: HER2 (nb is also predictive), o In HER2+ cancers the HER2 gene (which has a single copy and is expressed at a low level in normal people) gains multiple copies on genome and is overexpressed o similar structure to human epidermal growth factor receptor; this receptor can then be targeted by antibodies o HER2 presence can be determined by: Immunostaining FISH Ki67 o (have a high number of cancer cells actively dividing) 138 Giles Kisby GE Y1 CMS Immunology Cancer o o The Ki-67 protein is a cellular marker for proliferation About 30% of all newly diagnosed patients with early stage disease will eventually relapse and die with secondary disease 139 Giles Kisby GE Y1 CMS Immunology Cancer 16/01/14: Skin Cancer: Gerry Thomas Los (from booklet): Skin Cancer • Understand the different types of skin cancer and their causes and prognosis • Understand risk factors for melanoma • Understand pathological grading and staging and how this affects treatment and outcome • Understand how and why melanoma patients may be stratified for treatment in the future Los (from slides): • • • • Understand the different types of skin cancer and their causes and prognosis Understand risk factors for melanoma Understand pathological grading and staging and how this affects treatment and outcome Understand how and why melanoma patients may be stratified for treatment in the future Notes: - Take home messages o Exposure to UV light major risk factor for skin cancer o Genetic and behavioural risk factors o Basal cell carcinoma metastasises rarely o Melanoma metastasises frequently o Treatment – mainly surgery, some radiotherapy and more targeted therapy on its way (biologicals and immunotherapy) - Types of skin cancer: o Summary: The Good BCC The Bad SCC The Ugly (worst) Melanoma o malignant melanoma [which is less common but more serious] 86% of malignant melanomas in the UK in 2010 were linked to sun / sunbeds Incidence is increasing Risk factors: 140 Giles Kisby GE Y1 CMS Immunology Cancer strongly linked to intermittent exposure to high-intensity sunlight, rather than to chronic exposure o often low in hot countries because of this, genetic adaption and a culture of avoiding the hottest sun; AUS/NZ are exceptions History of sunburn doubles the risk of melanoma Light eyes, skin or hair Large number or unusually shaped moles [dysplastic naevae] Freckling Family history of melanoma Higher socioeconomic groups but reduced cost of travel to sunny locations is narrowing the gap Arsenic exposure in farmers Airline pilots / Airline cabin crew: Ionising radiation on plane, & sun at destinations Age: More common with increasing age [dec suncream used in past etc], but malignant melanoma is disproportionately high in younger people; age also linked to reduced survival rates Prev case: Once you have had one, more likely to get another Genetic factors o Family history (mutation in CDKN2A [tumor suppressor]) o Possibly non-Hodgkin’s lymphoma, breast cancer o Transplant patients (pos linked to Immunosuppression) o Atopic dermatitis (eczema) o Oncogenes: BRAF, AKT3 o Tumor suppressors: CDKN2A, PTEN (as for breast cancer), APAF1, P53 (may be written TP53) Targeted therapy for melanoma Ras inhibition o But not proven to be successful as single agent (use with others) o Ie vs Ras – Map pathway Braf inhibitors 141 Giles Kisby GE Y1 CMS Immunology Cancer o o Ie mutated raf But normal BRAF can be stimulated by non-mutation specific BRAF agents; therefore patients now stratified according to mutation status o Use vemurafenib o Four clinical sub-types: Superficial spreading melanoma o - 30% arise from pre-existing melanocytic naevus. o - Horizontal growth phase through the epidermis is followed by vertical growth Nodular o - no horizontal growth phase Lentigo maligna melanoma o - mainly elderly o - mainly developing in a lentigo maligna (non-invasive melanoma) Acrolentigenous o - starting on feet or hands, o - commonest in Afrocaribeans Prognosis and depth of invasion the higher the Breslow thickness [ie depth thickness], the worse the prognosis o low Breslow thickness = surgery only o high Breslow thickness = surgery and other treatments Treatment of skin cancer [other types of skin cancer treated in similar ways]: Surgery Radiotherapy (usually only if surgery not an option or to reduce possibility of relapse) Immunotherapy (melanoma only) Targeted agents for melanomas: o Eg anti-BRAF/VEGFR non-melanoma skin cancer, [which is very common but not so serious] Risk factors similar to prev; also: Family history of SCC or BCC increased risk of non-melanoma skin cancer basal cell carcinoma Generally a tumour of the elderly Sunburn, especially in childhood, increases risk of basal cell carcinoma commonest in certain sun exposed areas o common at: face, ears, neck and are frequently seen on the back, chest and legs o but rarely on the backs of the hands or arms locally destructive but generally not metastatic 142 Giles Kisby GE Y1 CMS Immunology Cancer - Regional lymph node metastases are only seen with large and long standing tumours [ie hence is the “good cancer”] squamous cell carcinoma strongly related to long-term occupational exposure to sunlight. [eg farmers] Tumours of the elderly These tumours develop from basal keratinocytes Tumours are commonest in sun exposed areas Tumours are metastatic spreading to regional lymph nodes then to solid organs particularly the lung May arise from precursor lesions o – solar keratoses and Bowen’s disease UV light types: o UVB is the most important wavelength in skin carcinogenesis [More UVA penetrates to earth but less carcinogenic (though still some cancer caused); UVC more harmful but less penetrates to earth] o UVA is the major cause of skin ageing o UVA used therapeutically in PUVA therapy (for eczema or psoriasis) can induce squamous cell carcinoma 143 Giles Kisby GE Y1 CMS Immunology Cancer 03/03/14: Dysplasia and carcinogenesis: Jayson Wang Los (from Booklet): appreciate that cancer is a genetic disorder, resulting from an accumulation of nonlethal mutations to growth regulatory genes. -carcinoma model of progression to different cancers. Notes: - Definitions o Hyperplasia - Increase in cell number without significant structural change (reversible) o Hypertrophy - Increase in cell size (reversible) o Metaplasia - Change from one cell type to another (reversible) o Dysplasia - Disordered growth, with loss of cell uniformity and pleomorphism (reversible) o Anaplasia - De-differentiation of cells, usually associated with malignancy (irreversible) o Neoplasm; Tumour = neoplasm - (new growth) abnormal and autonomous growth of cells which exceeds and is uncoordinated with the surrounding tissues o Benign - Tumour which grows locally without invasion or metastasis Benign tumours end with …oma eg. Lipoma, fibroma, papilloma, adenoma (?) o Malignant; Cancer = malignant - Tumour which invades locally and metastasizes Malignant tumours are usually either epithelial or mesenchymal ……carcinoma (if epithelial) ……sarcoma (if Mesenchymal) o Carcinoma-in-situ - severe full thickness dysplasia without invasion (pre-malignant) 144 Giles Kisby GE Y1 CMS Immunology Cancer - Genes and cancer o Four classes of regulatory genes: Promoters = proto-oncogenes eg. EGF, EGFR, K-ras, c-myc, Cyclins/CDKs Inhibitors = tumour suppressor genes [“Knudson two-hit hypothesis”] Lag period = Time between exposure of first hit and development of clinically apparent cancer; Altered cell shows no abnormality during lag period eg. Rb, p53, APC, WT-1, TGFR nb In WAGR syndrome the Wilms tumour is a tumour of the kidneys associated with WT-1 TSG gene Genes regulating apoptosis [may also be considered TSGs but the above egs are better for this] eg. Bcl-2 DNA repair genes [may also be considered TSGs but the above egs are better for this] eg. BRCA-1, BRCA-2 e.g. BRCA2 involved in HRR - Aetiology o Inherited mutations o Acquired mutations infections carcinogens ionizing radiation o Other causes Nutrition and diet Chronic cellular damage Hormones 145 Giles Kisby - GE Y1 CMS Immunology Cancer Aetiology o Inherited mutations Retinoblastoma (Rb) Wilm’s tumour (WT-1) Li Fraumeni (p53) Familial adenomatous polyposis [FAP]: (APC) HNPCC (MSH) o Acquired mutations Infections Human Papilloma Virus = HPV: o Oral/throat cancers o Papilloma (warts are a subset) o Cervix cancer n-Barr virus – o Burkitts Lymphoma [a cancer of the lymphatic system] o Nasopharyngeal cancer Epstei Hepatitis B & C virus o Liver: Hepatocellular carcinoma Bacteria: H pylori o gastric cancer Parasites: Schistosomiasis o bladder cancer carcinogens direct-acting (carcinogen): o Alkylating agents - cyclophosphamide Indirect acting (procarcinogen): carcinogenic only after being metabolised into active compounds: o Polycyclinc hydrocarbons – Benzpyrene o Aromatic amines, dyes - Benzidine o Natural products: Aflotoxin o Others: Vinyl chloride, turpentine etc. Childhood radiation exposure / ionizing radiation [is via dysjunction followed by random fusion] X Ray workers – Leukemia Radio-isotopes – Thyroid carcinoma Atomic explosion – Skin cancer, Leukemia o Other causes Nutrition and diet Eg red meat and colon cancer 146 Giles Kisby GE Y1 CMS Immunology Cancer Chronic cellular damage Eg alcohol and liver cancer Eg reflux can lead to esophageal cancer via causing dysplasia Hormones Eg estrogen role in enhancing breast cancer - Cancer traits: o Cancer stem cells: initially one forms; then different CSCs develop o Angiogenesis occurs: Angiogenesis genes are selected o Interactions with host cells: Interaction of cancer with the surrounding stroma allows for local invasion and metastasis o Counter immune system: Evasion of the host immune response - Summary o Cancers result from DNA damage - loss of control over cell division o Radiation, Chemicals & Viral infections are some known causes of cancers o Cancer evolves in multiple steps by sequentially acquired DNA damages o The accumulation of genetic mutations results in the dysplasia-carcinoma progression 03/03/14: Malignancy in Clinical Practice (Dr Rathi Ramakrishnan) Los (from Booklet): 147 Giles Kisby GE Y1 CMS Immunology Cancer -situ and invasive cancer and the importance of screening in prevention of cancer. Notes: 148 Giles Kisby GE Y1 CMS Immunology Cancer [during metastasis the cancer cells interact with leukocytes and platelets to form tumour cell emboli during their transit through the body] - Small window between cancer detectability and lethal burden: Therefore it is important to detect cancer early - Cancer Screening Programmes o NHS Cervical Screening Programme All women aged between 25 and 64 o NHS Breast Screening Programme Nb Estrogen receptor = use tamoxifen; Her-2 = use herceptin o NHS Bowel Cancer Screening Programme o Prostate Cancer Risk Management Programme No organised screening programme for prostate cancer but an informed choice programme - Staging: o TNM staging [Higher the number (1-4) = worse] T : DESCRIBES THE PRIMARY TUMOR SITE N : DESCRIBES THE REGIONAL LYMPH NODE INVOLVEMENT M : DESCRIBES THE PRESENCE OR OTHERWISE OF DISTANT METASTATIC SPREAD EACH SITE HAS IT’S OWN TNM CLASSIFICATION o Duke’s staging system [A = getting worse] re bowel Dukes' A: Invasion into but not through the bowel wall Dukes' B: Invasion through the bowel wall but not involving lymph nodes Dukes' C: Involvement of lymph nodes Dukes' D: Widespread metastases 149 Giles Kisby - GE Y1 CMS Immunology Cancer Grading: o Grade 1-3; 3= worse o Based on: • Tubule formation • Mitotic activity • Nuclear pleomorphism 150