File - Rachael Woods
advertisement

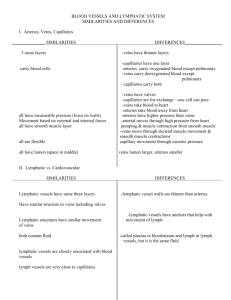
Rachael Woods Minor Case Study: Hodgkin’s Lymphoma in the Pediatric Population February 25th, 2014 Figure 1.1 (1) Introduction: B.T. is a 17-year-old Hispanic female who weighs 90.8 kg (199.8 lb) and has a height of 154.5 cm (60.8in). Additional anthropometrics of B.T. are provided below in Table 1.1. B.T. was admitted for generalized back pain and neutropenia secondary to Hodgkins Lymphoma (HL). B.T. was chosen for this study because the nutritional implications for cancer, specifically HL are of great interest; especially since proper nutrition is one factor that can be used to prevent the occurrence of cancer altogether. This study began on January 22nd, 2014, and ended on January 24th, 2014. The objective of this study is to closely examine the nutritional requirements for patients, particularly pediatric patients who are battling HL. Table 1.1 B.T.’s Anthropometrics Height for Age 5-10th Weight for Age >95th IBW 44 kg % IBW 206% BMI 37.9 (Obese Class II) BMI for Age >95th Social History: B.T. is currently a junior in high school and resides at home with her mother; she does not have any siblings. B.T. is Catholic and receives Florida Medicaid. Family responsibilities for B.T. are those of a typical teenager: She does the dishes, takes out the trash, and does her own laundry. B.T.’s mother is responsible for grocery shopping and preparing meals. B.T. denied drinking alcohol and smoking cigarettes. 1 Normal Anatomy and Physiology: HL manifests within the lymphatic system, or the immune system. HL typically arises in one lymph node and then begins spreading to “anatomically contiguous lymphoid tissues”(2). A normally functioning immune system fights off pathogenic organisms that may cause harm to the body. The lymphatic system is comprised of lacteals, lymph, lymph nodes, lymphatic vessels, tonsils, the thymus gland and the spleen (3). The lymphatic system begins its circuit in the lymphatic capillaries and lacteals; lymphatic capillaries are located in tissues throughout the body and lacteals are lymph vessels located around the small intestines. Excessive fluid build-up in tissues drain into lymphatic capillaries and fats that have been digested are absorbed from the intestines into lacteals (3). Lymphatic capillaries merge into larger lymphatic vessels and flow unidirectionally toward the thoracic cavity. Valves along their length prevent lymph from flowing in the opposite direction (3). The lymphatic vessels drain into either the right lymphatic duct or thoracic duct; the right lymphatic duct drains into the right subclavian vein and the thoracic duct drains into the left subclavian vein (3). Throughout the lymph’s journey from the body to the subclavian veins, it encounters components of the lymphatic system: the lymph nodes and the spleen. Lymph nodes are comprised of lymphatic tissues (tissues consisting of lymphocytes and antibodies) and are located throughout the length of the lymphatic system. The purpose of the lymph nodes is to remove pathogens and cell debris as the lymph makes its way to the thoracic cavity (3). Although lymph nodes are spread throughout the lymphatic system, they are more concentrated in the armpits, neck, groin, and chest areas (3). 2 The spleen, located in the abdominal cavity, is another element of the lymphatic system. The purpose of the spleen is to filter blood for pathogens, remove old erythrocytes and recycle iron from old erythrocytes. Like other components of the lymphatic system, the spleen is comprised of lymphatic tissue. The lymphatic tissue in the spleen is flourished with blood vessels, which are spread out into blood sinuses (3). The blood sinuses are lined with macrophages whose purpose is to engulf pathogens that it encounters via phagocytosis (3). The thymus gland is an important component of the immune system and is responsible for producing a type of lymphocytes called T Cells (4). The thymus glad is located behind the sternum near the heart (4). T Cells are lymphocytes that have two functions; some help the immune system, and thus they are called “Helper T Cells”, while others have a direct impact and are called “Cytotoxic T Cells” (5). Helper T Cells help the immune system by alerting other immune cells to an invader and instructing those cells to create antibodies (5). Cytotoxic T Cells do not assist; instead they destroy invaders when they come into direct contact with them (5). Similar to the thymus gland, the bone marrow is also responsible for producing immunological cells. The bone marrow is the tissue that is accountable for producing all cells that are considered to be white blood cells including lymphocytes, monocytes, granulocytes, neutrophils, eosinophils, and basophils (6). Lymphocytes have two forms: B Cells and T Cells. T Cells were described previously, B Cells form antibodies to foreign particles that enter the body helping fight off infection and disease (6). The ability to be immune to a certain pathogen can be attributed to the work of lymphocytes. Once an individual becomes infected by a pathogen, lymphocytes form antibodies to that pathogen 3 so that the body is able to recognize and fight off the pathogen should it encounter that particular pathogen again. Monocytes are the immature form of macrophages, which are responsible for engulfing and removing foreign particles (6). Granulocytes get their name from the granules that are present within their cytoplasm and consist of neutrophils, eosinophils and basophils (7). Neutrophils destroy bacteria and viruses, eosinophils destroy parasites and basophils respond to allergens (6). As mentioned previously, tonsils are another component of the lymphatic system. Tonsils are composed of lymphatic tissue and are located on either side of the pharynx; acting as filters to protect the body from pathogens entering the body via the upper digestive and respiratory tract (3). HL is one of the most common cancers among children and young adults and is characterized by the presence of Reed-Sternberg cells, which are illustrated below in Figure 1.2 (2). Reed-Sternberg cells cause the body’s lymphatic system to release immunologic factors such as lymphocytes, macrophages and granulocytes, which comprise tumors that are characteristic of HL. Figure 1.2(8) 4 HL typically presents itself initially as a painless enlarged lymph node and as the disease progresses it spreads further among lymphatic nodes and tissues. The nodes most commonly affected by HL are localized among a group of nodes: cervical, mediastinal, and para-aortic (2). The staging of HL is of great significance as the stage determines how it should be treated. For example, individuals who are stage I-II are most often free from systemic manifestations (2). However, once individuals progress to stages III-IV they begin having symptoms such as drenching night sweats, weight loss and fevers (2). The stages of the disease and the associated symptoms are shown below in Table 1.2. Upon the initial diagnosis of B.T.’s HL, she was classified as stage IIIB. Table 1.2 Clinical Stages of Hodgkin’s Lymphoma (2) Stage I Involvement of a single lymph node region or a single extra-lymphatic organ or site Stage II Involvement of two or more lymph node regions on the same side of the diaphragm alone or localized involvement of an extra-lymphatic organ or site Stage III Involvement of lymph node regions on both sides of the diaphragm without or with localized involvement of an extra-lymphatic organ or site Stage IV Diffuse involvement of one or more extra-lymphatic organs or sites with or without lymphatic involvement All stages are further divided on the bases of the absence or presence of the following symptoms: unexplained weight fever, drenching night sweats, and/or unexplained weight loss of great than 10% of normal body weight Past Medical History: Prior to the diagnosis of HL, B.T’s medical history was unremarkable, however it was noted in her chart that she had undergone some surgeries since her diagnosis. The surgeries were performed to remove lymph nodes that were affected by HL, but the exact 5 dates of those surgeries were not documented. B.T. had also undergone chemotherapy to treat her HL and was receiving chemotherapy during the admission in which this study was conducted. Present Medical Status and Treatment: The HL stage is very important when it comes to determining how invasive the treatment should be. There are currently 5 different types of treatment options (9): 1. Chemotherapy- usage of drugs whose purpose is to stop the growth of cancer cells 2. Radiation therapy- high energy x–rays used to either kill cancer cells or prevent them from growing any further; radiation therapy can also be used internally and is typically placed directly into a site where the cancer is located 3. Targeted therapy- treatment that uses drugs capable of identifying and targeting cancer cells without harming normal cells 4. Surgery- surgical removal of tissues containing cancerous cells 5. High-dose chemotherapy with stem cell transplant – as it’s name implies, high doses of chemotherapy drugs are given and stem cells are implanted to replace cells that have been killed as a result of chemotherapy As mentioned previously, B.T. was diagnosed with stage IIIB, a more advanced stage of the disease. B.T. had also undergone surgery to remove the affected lymph nodes in her neck and was also undergoing chemotherapy. B.T. was admitted on the basis of back pain and neutropenia. The cause for her radiating back pain was not made clear but was most likely secondary to cancer and/or cancer treatment. The neutropenia was secondary to B.T.’s chemotherapy treatments. B.T. 6 received a neutropenic diet during her admission due to her neutropenia diagnosis and also received an extensive amount of medications to control her symptoms. A list of B.T.’s medications can be found in Appendix 1 (10). In addition to B.T.’s observable signs and symptoms, it is also important to note her laboratory values to help visualize symptoms that aren’t always apparent externally. Table 1.3 shows B.T.’s laboratory values with their reference ranges denoted in parenthesis. Table 1.3 B.T.’s Laboratory Values (1/22) Glucose Sodium Potassium Chloride BUN Creatinine Hemoglobin Hematocrit 111 (70-99 mg/dL) 137 (135-145 mEq/L) 4.0 (3.5-5.0 mEq/L) 101 (101-111 mEq/L) 11 (5-20 mg/dL) 0.51 (0.5-1.1 mg/dL) 7.7 (12.0 - 16.0 g/dL) 25.4 (35-47%) Glucose can be elevated during times of stress, which is definitely a factor to be considered in B.T.’s case. Furthermore, glucose may also be elevated when individuals receive steroids, which B.T. was receiving during her admission. These labs also reveal that B.T.’s hemoglobin and hematocrit were decreased. This could be the result of the chemotherapy treatment that she was receiving since chemotherapy stops the growth of cells, including the bone marrow cells that are responsible for producing red blood cells. Observable physical and psychological changes: B.T. was asleep during the first visit and so all information was obtained thorough B.T.’s mother. B.T.’s mother did not comment much on B.T.’s physical health; all that was discussed was her nutrition. However, it was found in B.T.’s chart that she was not 7 ambulating since she was in a lot of pain. During the second visit with B.T., she was awake and alert and was able to answer all questions for herself. Like the first visit, nutrition was the primary topic discussed. However, during the second visit B.T. stated that she was having some troubles swallowing because her throat was sore, she was unaware of the cause and that it wasn’t preventing her from consuming meals. Treatment: As mentioned previously, B.T. was admitted for back pain secondary to HL and so her treatment focused mainly on medications to reduce pain. Also mentioned previously, B.T. was admitted with neutropenia secondary to chemotherapy. Again, B.T. was receiving a neutropenic diet to decrease the risk of infection from eating items such as raw food that could carry harmful microorganisms that a healthy individual’s immune system could fight off. Medical Nutrition Therapy: Nutrition History: B.T. follows a neutropenic diet (avoidance of raw/undercooked food items) while she is at home and her mother is responsible for grocery shopping and preparing meals. B.T. and her mother eat all of their meals family style at a dining room table where a television set is not visible. Two weeks leading up to B.T.’s admission, B.T. had not attended school and so all meals had been prepared by her mother and had been eaten at home. Table 1.4 shown below shows a summary of B.T.’s typical intake at home along with the nutritional analysis of those food items. During the initial interview, a 24-hour recall was also conducted to determine if B.T. was meeting her caloric needs while at the hospital. B.T.’s 24-hour recall along with the nutritional analysis can be found below in Table 1.5. 8 Table 1.4: Nutrient Analysis for B.T.’s Typical Intake CHO Protein 1 cup frosted flakes 1 cup 2% milk 1 Ensure 34g 12g 40g 1g 5g 9g ¾ cup black beans 1 cup white rice 2 servings potato chips 1 cup pre-packaged fruit cocktail 29g 53g Fat Breakfast Kcals Fe Ca A C 0g 12g 6g 140 120 250 25% 0% 25% 0% 29% 30% 10% 1% 25% 10% 0% 50% 11g 4g 1g 0g 169 228 10% 15% 4% 1% 0% 0% 0% 0% 30g 4g 20g 360 4% 0% 0% 20% 18g 1g 0g 76 0% 0% 2% 100% 1 Ensure 40g 9g 6g 250 25% 30% 25% 50% 1/3 cup white pasta ¼ cup pasta sauce 3 oz ground beef ½ cup cooked broccoli 1 slice bread 1 can Pepsi TOTAL 42g 7g 0g 6g 1g 23g 1g 1g 9g 201 41 173 10% 4% 14% 0% 2% 1% 0% 15% 0% 0% 8% 0% 5g 3g 0g 32 3% 5% 19% 61% 15g 41g 366g (64%) 2g 0g 80g (14%) 1g 0g 57g (22%) 77 164 2281 5% 0% 140% 3% 0% 105% 0% 0% 97% 0% 0% 299% Lunch Snack Dinner 9 Table 1.5: Nutritional Analysis for B.T.’s 24-Hour Recall CHO Protein Fat Kcals Breakfast Fe Ca A C Hard boiled egg Breakfast Potato Sausage Chicken Patty Turkey Bacon Blueberry Muffin Orange Juice 0 20 6 3 5 6 68 141 3% 0% 2% 0% 6% 0% 0% 0% 1 7 10 120 0% 2% 1% 0% 0 25 14 11 3 0 11 8 0 141 178 57 9% 7% 1% 0% 5% 0% 0% 1% 3% 0% 1% 71% White Bread (2) Tuna Salad Provolone Cheese Baked Potato Chips Mac & Cheese Chocolate Chip Cookie Lipton Brisk diet 2 packet mayonnaise 26 3 1 4 13 7 2 5 8 130 111 98 12% 11% 12% 4% 3% 23% 0% 4% 5% 0% 8% 0% 20 1 5 131 2% 4% 0% 0% 26 6 13 223 12% 9% 3% 0% 24 2 10 184 8% 2% 1% 1% 0 0 0 0 0% 0% 0% 0% 4 0 0 20 0% 0% 0% 0% White bread (2) Turkey (cooked) Provolone Cheese Fruit Cocktail Chocolate pudding Pepsi TOTAL 26 0 1 15 4 7 7 1 2 0 8 0 130 28 98 58 12% 2% 12% 4% 4% 0% 23% 2% 0% 0% 5% 10% 0% 2% 0% 8% 24 4 4 140 8% 6% 1% 1% 26 256 (45%) 0 86 (15%) 0 97 (40%) 96 2152 0% 115% 0% 89% 0% 40% 0% 92% Lunch Dinner 10 During the first visit B.T. consumed 100% of her meals equating to 2152 kcals and 86g protein based on the nutritional analysis of the 24-hour recall; meeting her daily requirements for calories. B.T.’s requirements were calculated using her adjusted body weight of 55.7 kg. Although using adjusted body weight in pediatrics is usually contraindicated, it was necessary in this case as B.T.’s weight is >95% percentile, she is obese and is 206% of her IBW (11). According to ASPEN, the equation for nutrient requirements in childhood cancer for obese children uses a stress factor ranging from 1.51.6, which is then multiplied by the BMR using the child’s adjusted body weight (12). Furthermore, ASPEN also states protein requirements for children with pediatric cancer are 1.8g/kg/day (12). Since adjusted body weight was used to calculated caloric requirements, adjusted body weight was also used to determine B.T.’s protein needs. The calculations performed for B.T.’s caloric and protein requirements are shown below: BMR (females) = [655 + (9.6 x wt (kg)) + (1.8 x ht (cm)) – (4.7 x age)] x Injury Factor BMR = [655 + (9.6 x 55.7kg) + (1.8 x 154.5cm) – (4.7 x 17) = 1388 kcals 1388 kcals x (1.5-1.6) = 2082-2221 kcals/day Protein = 1.8 x adjusted body wt 1.8 x 55.7 = 100g protein/day Although B.T. did not consume enough protein to meet her needs during the first visit (adjusted body wt x 1.5), she was consuming 100% of her meals and was consuming adequate calories (BMR x 1.5) to meet her needs, so no acute nutrition related problems were identified and a formal nutrition diagnosis was not made. Accordingly, per hospital protocol, a follow-up was scheduled but an intervention was not performed. Since a nutrition problem was not identified, there was not a specific aspect of her intake to be 11 monitored during follow up; it was scheduled simply to ensure B.T. did not develop any nutrition related problems. A 24-hour recall was not obtained during the second visit; however, during the second visit B.T. was still consuming 100% of her meals. Based on the 24-hour recall from the initial visit and the kcals calculated from B.T.’s typical caloric intake, it was assumed B.T. was still consuming enough calories to meet her needs at that time and so, again, no acute nutrition related problem was identified and a formal nutrition diagnosis was not made. Similar to the first visit, a formal intervention was not made since a nutrition diagnosis was not performed and a follow up visit was scheduled to continue to monitor B.T.’s nutritional status. Prognosis: HL is considered to be one of the most curable cancers if diagnosed early enough in the disease. The medical prognosis for HL depends on the stage at which it is diagnosed; the earlier it is diagnosed, the less invasive the treatments. The cure rate for individuals presenting with stages I and IIA is ~90%; with advanced disease (Stage IVA-IVB) the 5-year survival rate is 60-70% (2). Based on these statistics, B.T.’s medical prognosis is difficult to determine since she was diagnosed as Stage IIIB. Unfortunately individuals surviving HL have an increased risk of developing other cancers such as lung cancer, breast cancer, gastric cancer, sarcoma, and melanoma secondary to chemotherapy and radiation therapy received to treat HL (2). Cancer treatment can cause nutrition related side effects including: anemia, neutropenia, electrolyte imbalance, constipation, diarrhea, malabsorption, dysphagia, stomatitis/mucositits, dehydration, anorexia, dysgeusia, fatigue, weight loss, and pain (13). 12 The nutritional prognosis for B.T. is considered to be quite good since during the visit, B.T. did not mention that she had any of the listed side effects other than neutropenia (at least during that admission). It did not appear that B.T. had any problem with anorexia/weight loss since she is considered to obese and did not have a problem consuming 100% of her trays. Summary and Conclusion: Although there was not much I could do for B.T. because a formal nutrition diagnosis was not made, I still learned a lot from B.T. Prior to this study I was not too familiar with the pediatric population and was even more unfamiliar with cancer and the nutritional implications of the disease. Cancer has always provoked great interest since it is the second leading causes of death and because it has afflicted many in my family (14). I found it very interesting to learn just how important nutrition’s role is in the fight against cancer. This case study was also very eye opening for me because prior to this I didn’t realize just how sick so many children are. Prior to this internship I had an interest in going into pediatric dietetics but then became unsure. This rotation has definitely reassured me that pediatric nutrition is where my heart is. The future of our nation lies within our children’s hands; it is our job as health care professionals to ensure our children are as healthy as possible so that our nation as a whole will thrive. 13 Appendix 1: Medications (10) Medication Purpose Celecoxib Pain Reliever Cetirizine Antihistamine Clindamycin Antibiotic Famotidine H2 Blocker Ferrous Sulfate Iron Supplement B.T.’s Medications Drug Interactions ACE inhibitors, angiotensin II receptor blockers, anticoagulants, diuretics Antidepressants, antianxiety medications, antiepileptic, tranquilizers Erythrocin Not to be taken with other drugs that treat GERD Chloramphenicol, cimetidine, levodopa, methyldopa, penicillamine, cinoxacin, ciprofloxacin, demeclocycline, doxycycline, enoxacin, Nutrition Implications Other Side Effects Diarrhea, gas, weight gain, loss of appetite Sore throat, cold symptoms Dry mouth, stomach pain, diarrhea, vomiting Drowsiness, excessive tiredness Nausea, vomiting, heartburn Joint pain, white patches in mouth, vaginal discharge Diarrhea, constipation Headache, dizziness Constipation, stomach upset Constipation, stomach upset 14 levofloxacin, oxytetracycline, sparfloxacin, Buprenorphine, butorphanol, ipratropium, medications for: glaucoma, IBD, parkinsons disease, ulcers, and uriniary problems Nausea, vomiting, constipation, dry mouth Lightheadedness, dizziness, drowsiness, sweating, itching, mood changes Hydromorphone Pain reliever Bleomycin Treats head and neck cancer (HL) Brentuximab, vedotin Cyclophoshamide Treats Hodgkin’s Lymphoma Alkylating agents, allopurinol, hydrocortisone Doxorubicin Treats Hodgkin’s Lymphoma Cytarabine, dexrazoxane, mercaptopurine, streptozocin, phenobarbital, phenytoin Nausea, vomiting, loss of appetite, weight gain, diarrhea, increased thirst Unusual tiredness or weakness, dizziness, hair loss, separation of nails from nail beds, burning on hands/feet Etoposide Treats Hodgkin’s Lymphoma Cisplatin, cyclosporine Nausea, vomiting, stomach pain, diarrhea, constipation, loss of Unusual tiredness or weakness, pale skin, fainting, hair loss, Sores on mouth/tongue, vomiting, loss of appetite, weight loss Nausea, vomiting, loss of appetite, diarrhea, sores on the mouth, should drink plenty of water when taking this medication Redness & blistering of skin, rash, hair loss, darkened skin color Changes in skin color, sore throat, fever, chills, hair loss 15 appetite, weight loss, Filgrastim Gabapentin Ondansetron Prednisone Helps fight infection in those with neutropenia Lithium Increased water needs Anticonvulsant Hydrocodone, morphine, naproxen, antacids Nausea, vomiting, heart burn, diarrhea, constipation, increased appetite, weight gain, difficulty swallowing Anti nausea for chemotherapy Treats multiple symptoms, most likely used for the purpose of pain relief in B.T. Apomorphine, amidarone, azithromycin, sotalol, quinidine, procainamide, tramadol, thioridazine, soltalol, erythromycin Amiodarone, anticoagulants, antifungals, ketoconazole, aspirin, lovastatin, phenobarbital, oral contraceptives burning on hands/feet Bone,joint, or muscle pain, fever, shortness of breath, wheezing, dizziness, hives, rash, sweating, unusual bruising Drowsiness, tiredness, dizziness, headache, blurred vision, anxiety, memory problems, fever, itching, seizures Constipation, diarrhea Headache, drowsiness, chills, fever, rash, itching, shortness of breath, fainting Follow a low-salt, high potassium, high calcium diet, heartburn Headache, dizziness, extreme changes in mood, thin, fragile skin, increased hair growth, acne, weak muscles, increased sweating 16 Bibliography: 1. Krames. When Your Child Has Non-Hodgkin Lymphoma. Krames Patient Education Website. Available at: http://missionrmc.kramesonline.com/HealthSheets/3,S,40357?PrinterFrien dly=true. Accessed February 2nd, 2014. 2. Kumar V, Abbas AK, Fausto N, Aster JC. Pathologic Basis of Disease. 8th ed. Philadelphia, PA: Sunders Elsevier; 2010:616-621. 3. Fregmen BF, Frucht SS. Medical Terminology: A Living Language. 4th ed. Upper Saddle River, NJ: Pearson; 2009:180-184. 4. Healthline Body Maps:Thymus. Healthline Website. Available at: http://www.healthline.com/human-body-maps/thymus. Accessed February 16th, 2014. 5. National Institute of Allergy and Infectious Diseases. Immune System:T Cells. Available at: http://www.niaid.nih.gov/topics/immunesystem/immunecells/pages/tcells. aspx. Accessed February 16, 2014 6. MDS Foundation. What Does My Bone Marrow Do? 1st ed. Myelodysplastics Syndromes Foundation; 2012. 7. Medline Plus Trusted Health Information for You. Granulocytes. Available at: http://www.nlm.nih.gov/medlineplus/ency/article/003440.htm. Accessed February 16th, 2014 8. Reed-Sternberg Lymphocyte. Available at: http://en.wikipedia.org/wiki/File:Reed-Sternberg_lymphocyte_nci-vol7172-300.jpg. Accessed February 14th, 2014. 9. National Cancer Institute. Child Hodgkin Lymphoma Treatment Option Overview. Available at: http://www.cancer.gov/cancertopics/pdq/treatment/childhodgkins/Patient /page4. Accessed February 16th, 2014 10. Medline Plus Trusted Health Information for You. Drugs, Supplements, and Herbal Information. Available at: http://www.nlm.nih.gov/medlineplus/druginformation.html. Accessed February 16th, 2014. 11. Samour PQ, King K. Pediatric Nutrition. 4th ed. Jones and Bartlett Learning, LLC; 2012:363-367. 12. Corkings MR, Balint J, Bobo E, Plogsted S, Yaworski JA. The A.S.P.E.N. Pediatric Nutrition Support Core Curriculim. Silver Spring, MD: American Society for Parenteral and Enteral Nutrition; 2010:350-373. 13. American Dietetic Association. Nutrition Care Manual®. Treatment Modalities: Chemotherapy. Available at: http://nutritioncaremanual.org/topic. Accessed February 7th, 2014. 14. Center for Disease Control and Prevention. Leading Causes of Death. Available at: http://www.cdc.gov/nchs/fastats/lcod.htm. Accessed February 22nd, 2014. 17