P172 `ONE-STOP` MULTIDISCIPLINARY CLINIC FOR A MULTI
advertisement

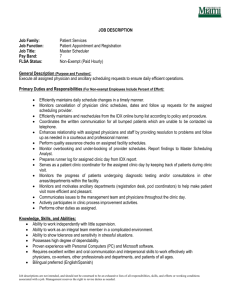
P172 ‘ONE-STOP’ MULTIDISCIPLINARY CLINIC FOR A MULTI-SYSTEM CONDITION – A MODEL FOR ALL? Borrows S, Tomlinson J, Williams D, Tsaloumas M, Searle Y, Golding L, Foggensteiner L LMBBS Clinic, Queen Elizabeth Hospital Birmingham. UK Background: A successful bid to the National Commissioning Group in 2010 has supported the development of designated ‘one stop’ annual clinics for patients with diagnosed or suspected Lawrence-Moon-Bardet-Biedl Syndrome (LMBBS). Aims: The objectives for these new clinics included provision of expert attention and management for patients, development of a model of care which embraces and immediately reacts to patient experiences of the service, enhanced multidisciplinary working, and partnership working with charities such as the LMBBS society. The monitoring, investigations and interventions offered by this service cover a wide range of areas including ophthalmology, Chronic Kidney Disease (CKD) management, genetic screening, weight management, comprehensive endocrine assessment and holistic support. The team includes of 4 consultants, 3 of which traditionally work in silos within separate directorates within the Trust and 1 that works for a neighbouring Trust. It also includes a dietician, a psychologist and is led and coordinated by the Clinical Nurse Specialist (CNS). Patient and public experience: Our collaboration with the LMBBS Society allows us to continually monitor, review and then redesign the service we provide. Unlike traditional out patient clinics, LMBBS Society co-ordinators (who are carers for patients with LMBBS) take an active role within all clinics. A clinic room is converted to a “meet and greet” room which is used throughout the day. LMBBS Society co-ordinators give us real-time feedback of what is and is not working for the patients, which allows immediate improvements to be made. For example, due to the clinical features of LMBBS (such as poor vision/learning difficulties) patients found the traditional way of working where the patient goes into 6 different clinic rooms daunting and impractical. Instead, with the exception of the ophthalmic assessment where specific equipment is required, the specialists rotate round the patients enabling our patients and families to stay in the same clinic room. This unique approach is managed and coordinated by the CNS who coordinates each session to ensure the clinic meets individual patient needs and runs efficiently and to time. Audit:Data from the first two years of the LMBBS clinic have informed us of the specific needs of this cohort of patients and we are now able to start to refine the clinic according to these needs.For example, we now know the incidence and prevalence of renal disease in LMBBS is low, affecting only 5% of the patient group, with our data suggesting it starts in early childhood. This means that we no longer arrange investigations for patients at low risk. The clinic is continually monitored and develops. For example, a patient satisfaction audit illustrated that there were delays in the communication to patients and GPs following the clinic, which in turn led to delays in commencing or altering treatments. The CNS set up and chairs an MDT meeting after each clinic session. The CNS records action points for each individual patient and, as a nurse prescriber, then sends out summary letters to patients and GPs. This is then followed up with the individual clinician’s letter. We have already developed a system for home clinics which aim to take the clinic to the patients, as some are unable to attend the multidisciplinary clinic for reasons of mental or physical disability, or requirement for additional support other than an annual review. Comment: This novel service provides a unique clinic where disciplines from different directorates of the Trust, different Trusts and sectors of healthcare work together as a team. A key aspect is thatthe patient remains central in the process, with the clinic co-ordinated around and healthcare workers rotating to meet individual patient requirements.These unique aspects of the clinics could be transferred to other specialties and centres, providing a comprehensive care pathway. The role of the CNS is integral in engaging these groups, working with clinicians and service providers in both primary, secondary care and the voluntary sector.Timetabling of these complex clinics in order to meet each of the individual patient’s needsis challenging. Clear leadership by the CNS ensures the success of the clinic is maximised.