Streamline Discharge Process / ED Management Services
advertisement

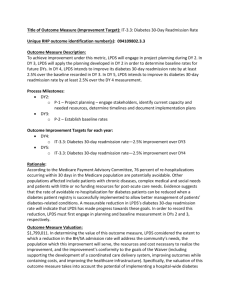
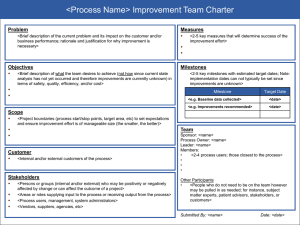
STREAMLINE DISCHARGE PROCESS / ED MANAGEMENT SERVICES Identifying Project and Provider Information: Category 2: Implement/Expand Care Transitions Programs; Project Option 2.12.2: Implement one or more pilot intervention(s) in care transitions targeting one or more patient care units or a defined patient population; 094109802.2.4; HCA Las Palmas Del Sol (094109802). o Required Core Project Component: Conduct quality improvement for the project using methods such as rapid-cycle improvement. Activities may include, but are not limited to, identifying project impacts, “lessons learned,” opportunities to scale all or part of the project to a broader patient population, and key challenges associated with expansion of the project, including special considerations for safety-net populations. Project Description: This project will establish case management and coordinated discharge planning processes; those processes will be used to identify top chronic conditions that are common causes of avoidable readmissions and develop strategies to reduce readmissions in those specific populations. ED discharge is a prime target for improvement in the delivery of effective discharge instructions, follow-up care recommendations, referrals to community providers or resources, matching patients with appropriate community-based resources, and increasing patient satisfaction. One goal of the project is to create a mechanism to track unnecessary ED visits and admissions to the hospital and to use this mechanism to refer the patients to the appropriate community resources. This project will also incorporate the emergency screening process (ESP). ESP refers to a low-acuity strategy used to redirect non-urgent patients to appropriate alternative community resources after they have had a medical screening exam (MSE) performed by a Qualified Medical Professional (QMP). The goals of the ESP are decreased Left Prior to Medical Screening Exam (LPMSE), decreased frequent returns to the emergency department, increased community education and awareness, improved satisfaction of patients, physicians, and ED staff, and improved overall turn-around times for truly emergent conditions. o Challenges: Patient participation; educating practitioners on best practices; collecting and accurately interpreting the data collected from patients; identifying the reasons behind and solutions for the most common preventable ED visits and admissions. Starting Point/Baseline: As of 2011, the ED does not have case management to be able to review unnecessary ED visits or admissions and refer to the appropriate community resources. There is also no mechanism in place to be able to track or review unnecessary ED visits. Currently, there is no case management representation in the ED and no processes in place to review unnecessary ED visits for QI purposes. Rationale: Case management in the emergency department would reduce overcrowding, decrease wait times, increase patient and physician satisfaction, and appropriately utilize community resources. Case managers would also serve as a resource to the physicians and staff by providing appropriate discharge planning guidance. Additionally, poorly designed discharge processes create unnecessary stress for medical staff, causing failed communications, rework, and frustrations. A comprehensive and reliable discharge plan, along with post-discharge support, can reduce readmission rates, improve health outcomes, and ensure quality transitions. Patient transition is a multidimensional concept and may include transfer from facility to home, or to nursing home, or to home and community-based services, etc. Related Category 3 Outcome Measure(s): OD-3: Potentially Preventable ReAdmissions—30 day Readmission Rates; IT-3.1: All cause 30 day readmission rate; (094109802.3.9). Relationship to Other Projects: This project is part of LPDS’s larger plans to expand and develop primary care and specialty care services, while improving access to care and containing the costs of care. It is one of a group of several LPDS delivery system reforms (i.e., LPDS’s Physician Training and Quality project (094109802.1.5), Electronic Medical Records project (094109802.2.1), and Evaluate Hospitalist Model project (094109802.2.3)) which are primarily aimed at improving models of inpatient care through the implementation of technology, provider education, quality improvement, and other means. Similarly to LPDS’s Congestive Heart Failure Clinic project (094109802.2.2) and Develop Diabetes Management Registry project (094109802.1.3), this project will help individuals with specifically targeted health conditions to better manage their use of healthcare services from LPDS and other providers in the El Paso community, ensuring that the delivery and utilization of healthcare is more efficient from the provider’s perspective and more effective from the patient’s perspective. Relationship to Other Performing Providers’ Projects in the RHP: TBD Plan for Learning Collaborative: TBD Project Valuation: $4,683,408. The valuation of each LPDS project takes into account the transformational impact of the project, the population served by the project (both number of people and complexity of patient needs), the alignment of the project with community needs, and the magnitude of costs avoided or reduced by the project. In particular, this project has been valued based on the fact that this project will identify populations in need of care management to ensure that the project’s services will be targeted to those populations; this project has also been valued based on the need of the community in general for more effective and extensive care management in the ED setting to reduce improper utilization of emergency healthcare services. 094109802.2.4 Related Category 3 Outcome Measure(s): Year 2 (10/1/2012 – 9/30/2013) Milestone 1: Establish baseline for metrics P-6.1, P-7.1, P-8.1, I10.1, I-11.1, and I-14.1. Metric 1: Establish baseline for future years. Milestone 1 Estimated Incentive Payment: $1,145,395 2.12.2 2.12.2.X HCA Las Palmas Del Sol 094109802.3.9 IT-3.1 Year 3 (10/1/2013 – 9/30/2014) Milestone 2 [P-6]: Train/designate more ED case managers. Metric 1 [P-6.1]: Number of trained and/or designated ED case managers over baseline. Baseline/Goal: n/a Data Source: HR; job descriptions; training curriculum. Milestone 2 Estimated Incentive Payment: $624,783 Milestone 3 [P-7]: Develop a staffing and implementation plan to accomplish the goals/objectives of the care transition program. Metric 1 [P-7.1]: Documentation of the staffing plan. Baseline/Goal: n/a Data Source: Staffing and implementation plan. Milestone 3 Estimated Incentive Payment: $624,782 STREAMLINE DISCHARGE PROCESS / ED MANAGEMENT SERVICES 094109802 All cause 30 day readmission rate Year 4 (10/1/2014 – 9/30/2015) Milestone 4 [I-10]: Identify the top chronic conditions (e.g., heart attack, heart failure, and pneumonia) and other patient characteristics or socioeconomic factors that are common causes of avoidable readmissions. Year 5 (10/1/2015 – 9/30/2016) Milestone 6 [I-11]: Improve the percentage of patients in defined population receiving standardized care according to the approved clinical protocols and care transitions policies. Metric 1 [I-10.1]: Identification and report of those conditions, socioeconomic factors, or other patient characteristics resulting in highest rates of readmissions. Baseline/Goal: Report for DY4. Data Source: Registry or EHR report/analysis. Metric 1 [I-11.1]: Number over time of those patients in target population receiving standardized, evidence-based interventions per approved clinical protocols and guidelines. Baseline/Goal: 10% improvement over DY 2 baseline. Data Source: Registry or EHR report/analysis. Milestone 4 Estimated Incentive Payment: $626,599 Milestone 6 Estimated Incentive Payment: $517,625 Milestone 5 [I-14]: Implement standardized care transition process in specified patient populations. Milestone 7 [I-14]: Implement standardized care transition process in specified patient populations. Metric 1 [I-14.1]: Measure adherence to processes. Baseline/Goal: 10% improvement over DY 2 baseline. Data Source: Hospital administrative data and patient medical records. Metric 1 [I-14.1]: Measure adherence to processes. Baseline/Goal: 5% improvement over DY 4. Data Source: Hospital administrative data and patient medical records. Milestone 5 Estimated Incentive Payment: $626,598 Milestone 7 Estimated Incentive Payment: $517,625 094109802.2.4 Related Category 3 Outcome Measure(s): Year 2 (10/1/2012 – 9/30/2013) Year 2 Estimated Milestone Bundle Amount: $1,145,395 2.12.2 2.12.2.X HCA Las Palmas Del Sol 094109802.3.9 IT-3.1 Year 3 (10/1/2013 – 9/30/2014) Year 3 Estimated Milestone Bundle Amount: $1,249,565 All cause 30 day readmission rate Year 4 (10/1/2014 – 9/30/2015) Year 4 Estimated Milestone Bundle Amount: $1,253,197 TOTAL ESTIMATED INCENTIVE PAYMENTS FOR 4-YEAR PERIOD: $4,683,408 91313 STREAMLINE DISCHARGE PROCESS / ED MANAGEMENT SERVICES 094109802 Year 5 (10/1/2015 – 9/30/2016) Year 5 Estimated Milestone Bundle Amount: $1,035,250