RAID/Liaison - Hambleton, Richmondshire and Whitby CCG
advertisement
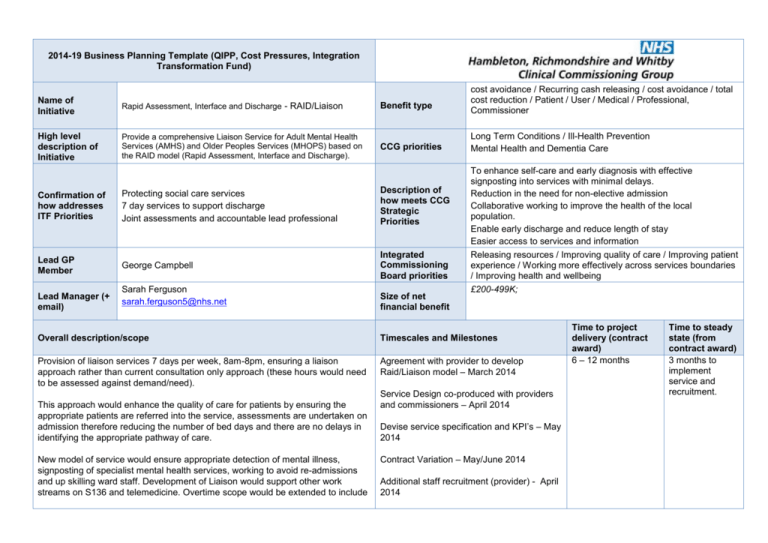
2014-19 Business Planning Template (QIPP, Cost Pressures, Integration Transformation Fund) cost avoidance / Recurring cash releasing / cost avoidance / total cost reduction / Patient / User / Medical / Professional, Commissioner Name of Initiative Rapid Assessment, Interface and Discharge - RAID/Liaison Benefit type High level description of Initiative Provide a comprehensive Liaison Service for Adult Mental Health Services (AMHS) and Older Peoples Services (MHOPS) based on the RAID model (Rapid Assessment, Interface and Discharge). CCG priorities Long Term Conditions / Ill-Health Prevention Mental Health and Dementia Care To enhance self-care and early diagnosis with effective signposting into services with minimal delays. Reduction in the need for non-elective admission Collaborative working to improve the health of the local population. Enable early discharge and reduce length of stay Easier access to services and information Confirmation of how addresses ITF Priorities Protecting social care services 7 day services to support discharge Joint assessments and accountable lead professional Description of how meets CCG Strategic Priorities Lead GP Member George Campbell Integrated Commissioning Board priorities Lead Manager (+ email) Sarah Ferguson sarah.ferguson5@nhs.net Size of net financial benefit Releasing resources / Improving quality of care / Improving patient experience / Working more effectively across services boundaries / Improving health and wellbeing £200-499K; Overall description/scope Timescales and Milestones Provision of liaison services 7 days per week, 8am-8pm, ensuring a liaison approach rather than current consultation only approach (these hours would need to be assessed against demand/need). Agreement with provider to develop Raid/Liaison model – March 2014 This approach would enhance the quality of care for patients by ensuring the appropriate patients are referred into the service, assessments are undertaken on admission therefore reducing the number of bed days and there are no delays in identifying the appropriate pathway of care. New model of service would ensure appropriate detection of mental illness, signposting of specialist mental health services, working to avoid re-admissions and up skilling ward staff. Development of Liaison would support other work streams on S136 and telemedicine. Overtime scope would be extended to include Service Design co-produced with providers and commissioners – April 2014 Devise service specification and KPI’s – May 2014 Contract Variation – May/June 2014 Additional staff recruitment (provider) - April 2014 Time to project delivery (contract award) 6 – 12 months Time to steady state (from contract award) 3 months to implement service and recruitment. outreach support to Nursing Homes and GP Liaison. Service go live – April 2014 This service model will be delivered by increasing the number of existing liaison nurses working into the Acute wards and A&E, increasing the specialist roles including medical (consultant Psychiatrist) and psychology to enable rapid intensive support which includes multidisciplinary assessments, which essential to support appropriate and safe discharge. Option 1: Implement Liaison Services for MHOPS (Older People only) Resource: 1 x B7 , 1 x B6, 0.5 WTE Consultant Psychiatrist, 0.5 WTE B8b Psychologist, 1 x B4 Admin Support. Total Cost: £281,874 Option 2: Implement Liaison Services for AMHS (Adults only) Resource:1 B6, Consultant Psychiatrist, B8b Psychologist, B4 Admin. Total Cost: £268,566 Option 3: Implement Liaison Services for MHOPS and AMHS (Older People and Adults). Total Cost: £472,880 Patient Acceptability & Experience The model will ensure patients mental health needs are addressed when they are in an acute hospital for treatment for their physical health needs. It would also enable earlier discharge and reduce readmission rates. Complexity of stakeholder engagement / providers working together It would increase the number of people receiving appropriate care and support and reduce the number of people developing mental illness within an acute hospital setting. Liaison services can reduce the risk of self-harm and suicide while also addressing the long-term conditions and medically unexplained symptoms with which many patients present. The Provider and Acute Trust would be required to liaise in order to establish a fully supported liaison service. As such we have established Service Improvement Group to ensure local delivery of key programmes of mental health related work and this has representation for public health, NYCC, TEWV, South Tees NHS Foundation Trust and local clinicians and is chaired by Dr Campbell, CCG Deputy Chair and GP Lead. This working group has already developed a detailed business case. We will also look further incentivise progress through embedding this as part of CQUINs for 2013/14 and 2014/15. Recent Rethink and mental health service user events have shown significant support for Liaison services, this model would address many of the emerging themes from service user events. Patient Safety Current limited liaison service provision provides a consultation only approach to urgent patients presenting in A&E, this service is only operational during office hours and Resources required to Implementation of this model would require project management support to recruit and establish a liaison team. The provider has already identified a project manager and a business case has Clinical Effectiveness there are no cover arrangements in place. The current model provides a piecemeal service operating on a part time basis, there is an unmet demand which cannot be quantified at the present time, the quality of this model is therefore compromised as it is not available to some individuals whom may benefit. The new model of service would provide more streamlined approach to care with appropriate medical input from clinical teams. implement project The model is based upon the principles of Birmingham & Solihull Mental Health NHS FT’s Rapid Assessment Interface & Discharge (RAID) Project, which has received accreditation from the Psychiatric Liaison Accreditation Network of the Royal College of Psychiatrists and also won a Health Service Journal Award for innovation in mental health in 2010. Certainty of service continuity The liaison model would enhance current service provision and ensure service continuity, rather than seek a new provider. Both Trusts would be using the same staff members which would ensure a reliable and responsive service. been prepared outlining the service requirements. To achieve the objectives it is also essential that links are developed and maintained with Adult Social Care, Acute Community Services, Mental Health Community Services, START Team and HIT. Engagement will be required with the Commissioning Support Unit Business Intelligence Team and providers performance management team to develop and implement performance management measures The economic evaluation study of RAID concluded that the RAID service is good value for money, particularly as the benefits included in the assessment are over and above any improvements in health and quality of life which are the fundamental justification for health spending. The Government’s Mental Health Strategy No Health Without Mental Health 2011, emphasises the importance of improved services that interface between mental and physical health where co-morbidities exist. Equity of Access The model would not present any negative impact on equity of access. It would enhance the identification of suitable patient pathways of care. Confidence in market Variation to an existing contract and existing pathways Sustainability / Corporate Social Responsibility This would reduce repeat attendances to A&E through early diagnosis and clinical intervention. It would also signpost to appropriate primary care services therefore avoiding unnecessary travel. Information Availability An economic evaluation has been undertaken by LSE, this evaluation has been reviewed internally in order to make assumptions on cost and potential savings. Risks Risks identified (including unintended consequences) Mitigating actions Timescale 1. Impact upon mental health community teams and inpatient units Staff recruitment to new service may lead to a loss of skills to existent services. Capacity issues with memory clinic services due to increased demand 2. Unable to evidence benefits in a timely manner Predominant information available from RAID is qualitative research and estimations with regards to Quantitative research. This business case includes a request to fund temporary project lead post to ensure we are able to collate and evaluate the enhancement of services. 3. Inability of community services to react in a timely manner to support discharge Provider to manage risk April/May 2014 Monitor activity closely June 2014 onwards Liaise with BI and provider analysts to identify effective collection and analysis of performance and quality data May 2014 Engage community services as part of implementation plan with expectations of discharge timescales April 2014 Benefits/Outcomes Enhance quality of care for patients Ensure appropriate patients are referred into the service Appropriate clinical input from medical staff Reduction in the number of bed days and readmissions No delays in identifying appropriate pathways of care Support crisis services and Section 136 workstream Stakeholder group and purpose Method of Identifying (including KPIs) Reduction in admissions to medical wards Early diagnosis of dementia Reduced admission to residential care following discharge from hospital Patient supported in the community for longer Reduced length of stay – where appropriate Reduced repeat attendance at A&E through early diagnosis and intervention Improved patient satisfaction Where are savings released? Method of engagement and frequency Exit plan Service provider and relevant staff groups Acute Trust and relevant staff groups Community Teams and GPs Feedback to be obtained on proposed new service specification Redeployment of staff and / or reduction in contract size if activity levels or outcome targets are not achieved. Benefits/Outcomes £’000 FY14/15 Expenditure 473 Saving (520) (47) Total net savings FY15/16 FY16/17 N.B The gross saving reflects costs before non-elective threshold and re-admission adjustments. FY17/18 National benchmarking statistics provide evidence for a much higher cost saving. However with other schemes potentially impacting on nonelectives a more realistic saving of 5% 20% saving would generate a cost saving of approx. £220k-£800k FY18/19 Total