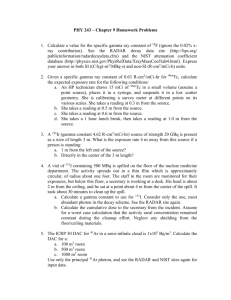
Perinatal Disaster Management tool
advertisement

Perinatal Disaster Management By Howard Roemer MD, et al. Published on ACEP.org Condition Influenza SARS Monkeypox Anthrax Botulism Hemorrhagic Fever Virus Treatment EMERGING INFECTIONS Vaccine. Indicated in pandemic for all pregnant women. Not approved for infants under 6 months of age. Antivirals. Neuraminidase inhibitors (oseltamivir and zanamivir) likely to be useful in a pandemic. Treatment should be initiated as soon as possible, ideally within 48 hours of onset of symptoms. Oseltamivir: 75 mg BID × 5 days for acute infection, Q day × 10 days for prophylaxis. Zanamivir: Two 5-mg inhalations (10 mg total) × 10 days for prophylaxis. Pregnant women: Although zanamivir can be used in pregnancy, oseltamivir is preferred because of its systemic absorption. Those with confirmed, probable, or suspected infection should receive oseltamivir, even if more than 48 hours have elapsed since illness onset. Beginning treatment as early as possible is critical. Efficacy of ribavirin and corticosteroids in the treatment of patients with SARS has been questioned. No specific recommendation. Smallpox vaccination. Pregnant women: Appears to be recommended as benefit from infection prevention appears to outweigh risk to fetus from vaccine. BIOLOGICAL WEAPONS Antibiotics. Prophylaxis limited to those exposed to a confirmed environmental contamination or a high-risk source, as determined by local public health officials. Inhalation or postexposure prophylaxis for 60 days. Pregnant and breastfeeding women: Ciprofloxacin 500 mg PO bid; alternate ampicillin 500 mg PO bid. Infants: Ciprofloxacin 10-15 mg/kg PO per dose BID (max 1 g/daily). Alternative: Amoxicillin 40 mg/kg/day divided into 3 doses q 8 hours. Cutaneous infection for 60 days. Pregnant and breastfeeding women: Ciprofloxacin as above. Alternate: doxycycline 100 mg PO BID. Infants: Ciprofloxacin as above. Alternative: Doxycycline 2.2 mg/kg PO per dose BID (max 200 mg/daily). Vaccine. All patients. Benefits in bioterrorism incident appear to outweigh risks. Antitoxin. Pregnant women: Currently equine form indicated. Human IG may become available for adults. Infants: BIG-IV safe and effective treatment for infant botulism type A and type B. Obtain from the California Department of Health Services (CDHS). Supportive treatment. Because of DIC and resulting hemorrhagic complications, invasive procedures such as central lines should be avoided whenever possible. Red blood cells (leukoreduced in pregnancy), platelets, and clotting factor transfusions may be necessary. Fluids should be used judiciously because of a propensity to develop pulmonary edema. Ribavirin. Ribavirin therapy for patients with HFV of unknown cause or known to be caused by an arenavirus or bunyavirus is not approved by FDA and must be used under an Investigational New Drug protocol, although in a masscasualty setting, this requirement may need to be modified. Contained casualty setting. Pregnant and breastfeeding women: Generally, ribavirin is contraindicated, but for infection with HFV of unknown cause or secondary to an arenavirus or Rift Valley fever, the benefits may outweigh the fetal risk. Loading dose of 30 mg/kg (max 2 g) IV, then 16 mg/kg (max 1 g) IV q 6 hr for 4 days, then 8 mg/kg (max 500 mg) IV q 8 hr for 6 days. Children: Same as pregnant women by weight. The decision to use oral rather than parenteral Plague Smallpox Tularemia Organophosphates (Nerve Gas) medication will depend on available resources. Mass casualty setting. Pregnant and breastfeeding women: Loading dose of 2000 mg PO, then weight over 75 kg: 1200 mg/day PO per dose BID for 10 days; weight less than 75 kg: 1000 mg/day PO in divided doses (400 mg in a.m. and 600 mg in p.m.) for 10 days. Children: Loading dose of 30 mg/kg PO, then 15 mg/kg/d PO in two divided doses for 10 days. Blood Transfusion. Pregnant women: CMV antibody-negative products or if unavailable, leukocyte-reduced products. Contained casualty setting. 10-day treatment. Pregnant and breastfeeding women: Gentamicin 5 mg/kg IM or IV Q day or 2 mg/kg load, then 1.7 mg/kg IV per dose TID. Adjustments based on renal function. First alternative: Oral doxycycline 100 mg IV per dose BID or 200 mg IV Q day as condition allows. Second alternative: Ciprofloxacin 400 mg IV per dose BID. Infants: Streptomycin 15 mg/kg IM per dose BID (max 2 g/day) or gentamicin 2.5 mg/IV per dose TID (only BID for newborns up to 1 week or preterm infants). First alternative: doxycycline 2.2 mg/kg IV per dose BID (max 200 mg/daily). Second alternative: ciprofloxacin 15 mg/kg IV per dose BID (max 1 g/ daily). Mass casualty setting and postexposure prophylaxis. 7-day treatment. Pregnant and breastfeeding women: Doxycycline 100 mg per dose PO BID. Alternative: Ciprofloxacin 500 mg PO bid per dose. Infants: Doxycycline 2.2 mg/kg PO per dose B.I.D. (max 200 mg/daily). Alternative: Ciprofloxacin 20 mg/kg PO per dose BID (max 1 g/daily). Vaccine. Administered within 4 days of first exposure. Pregnant and breastfeeding women: In the event of exposure or high risk for exposure, pregnant women are advised to receive the vaccine because the risk for death and serious illness from smallpox (particularly during pregnancy) outweighs the risk for fetal vaccinia. Infants: Vaccination has been successfully and safely administered to persons of all ages, from birth onward. Contained casualty setting. Pregnant and breastfeeding women: Gentamicin, 5 mg/kg IM or IV once daily for 10 days. First alternative: Streptomycin, 1 g IM per dose twice daily for 10 days. Switch to oral therapy as condition allows. Second alternative: Ciprofloxacin, 400 mg IV per dose BID for 10 days. Third alternative: Doxycycline, 100 mg IV per dose BID for 14-21 days. Infants: Streptomycin, 15 mg/kg IM per dose twice daily (should not exceed 2 g/d) for 10 days of treatment. First alternative: Gentamicin, 2.5 mg/kg IM or IV 3 times daily for 10 days. Second alternative: Doxycycline 2.2 mg/kg IV per dose (max 200 mg/daily). Third alternative: Ciprofloxacin 15 mg/kg per dose BID IV (max 1 g/daily). Mass casualty setting and postexposure. Pregnant and breastfeeding women: Doxycycline 100 mg PO per dose BID prophylaxis, 14-day treatment. Infants: Ciprofloxacin 500 mg PO per dose BID. First alternative: Doxycycline 2.2 mg/kg PO per dose BID (max 200 mg/daily). Second alternative: Ciprofloxacin 20 mg/kg per dose BID PO (max 1 g/daily). Pralidoxime chloride. 30 mg/kg bolus followed by 8-10 mg/kg/hour. Pregnant women: For significant exposure, same treatment as that given to other adults. Breastfeeding women: Stop nursing. Atropine 2 mg intravenously every 2-5 min, titrated to effect; although intravenous is preferred, also may be administered by intramuscular/endotracheal tube in similar doses. Prolonged 2 mg/kg/h IV infusion might be needed to control secretions. Infants: Pralidoxime 25-50 mg/kg bolus given over 30 minutes, then infusion of 9-19 mg/kg/hr. Atropine 0.02 mg/kg intravenously every 2-5 min, titrated to effect; 0.1 mg minimum dose. Seizures. IV lorazepam 1-2 mg/min up to 10 mg, or diazepam 2 mg/min up to 20 mg. Breastfeeding women: Discontinue nursing while receiving medications. Infants: IV lorazepam 0.1 mg/kg over 2 min (max dose 0.4 mg/kg). General Radiation Bone Marrow Recovery Plutonium, Americium, and Curium Cesium and Thallium RADIOLOGIC OR NUCLEAR EVENT Potassium iodide (KI). Pregnant women: Give KI to protect the growing fetus. However, pregnant women should take only one dose of KI following internal contamination with (or likely internal contamination with) radioactive iodine. Dose: 130 mg (one 130-mg tablet or two 65-mg tablets or 2 mL of solution). Breastfeeding women: One dose of KI if they have been internally contaminated with (or are likely to be internally contaminated with) radioactive iodine. CDC recommends stopping breastfeeding and feeding the child baby formula or other food if it is available. If breast milk is the only food available for an infant, nursing should continue. Women who are breastfeeding should take the adult dose of 130 mg. Infants (including breastfed infants): Infants need to be given the recommended dosage of KI for babies. The amount of KI that gets into breast milk is not enough to protect breastfed infants from exposure to radioactive iodine. The proper dose of KI given to a nursing infant will help protect it from radioactive iodine that it breathes in or drinks in breast milk. Newborns from birth to 1 month of age should be given 16 mg (¼ of a 65-mg tablet or ¼ mL of solution). This dose is for both nursing and nonnursing newborns. Neupogen. Children and pregnant women should take Neupogen with caution. It is not known if Neupogen is excreted in human milk, so breastfeeding women should take Neupogen with caution as well. DTPA. Pregnant women: Unless a pregnant woman has very high levels, treatment should begin and continue with Zn-DTPA. Ca-DTPA should be used in pregnant women only to treat very high levels of internal radioactive contamination. In this case, doctors and public health authorities may prescribe a single dose of Ca-DTPA, together with a vitamin and mineral supplement that contains zinc, as the first treatment. However, after the first dose of Ca-DTPA, treatment should continue 24 hours later with a daily dose of Zn-DTPA, as needed. Breastfeeding women: CDC recommends that women with internal contamination stop breastfeeding and feed the child baby formula or other food if it is available. If breast milk is the only food available for an infant, nursing should continue. Breastfeeding women who are internally contaminated with plutonium, americium, or curium should be treated with DTPA. Infants: Either Ca-DTPA or Zn-DTPA may be given to infants and children. Prussian blue. 500-mg capsules that can be swallowed whole. People who cannot swallow pills can take Prussian blue by breaking the capsules and mixing the contents in food or liquid. The dose depends on the person’s age and the amount of contamination in the body. It is given 3 times a day for a minimum of 30 days, depending on the extent of the contamination. Pregnant women: Safe for most adults, including pregnant women. Breastfeeding women: Women who are breastfeeding their babies should stop and consult with their doctors if they think they are contaminated with radioactive materials. Infants: Dosing for infants (0-2 years) has not been determined yet.