Klaus Becker
advertisement
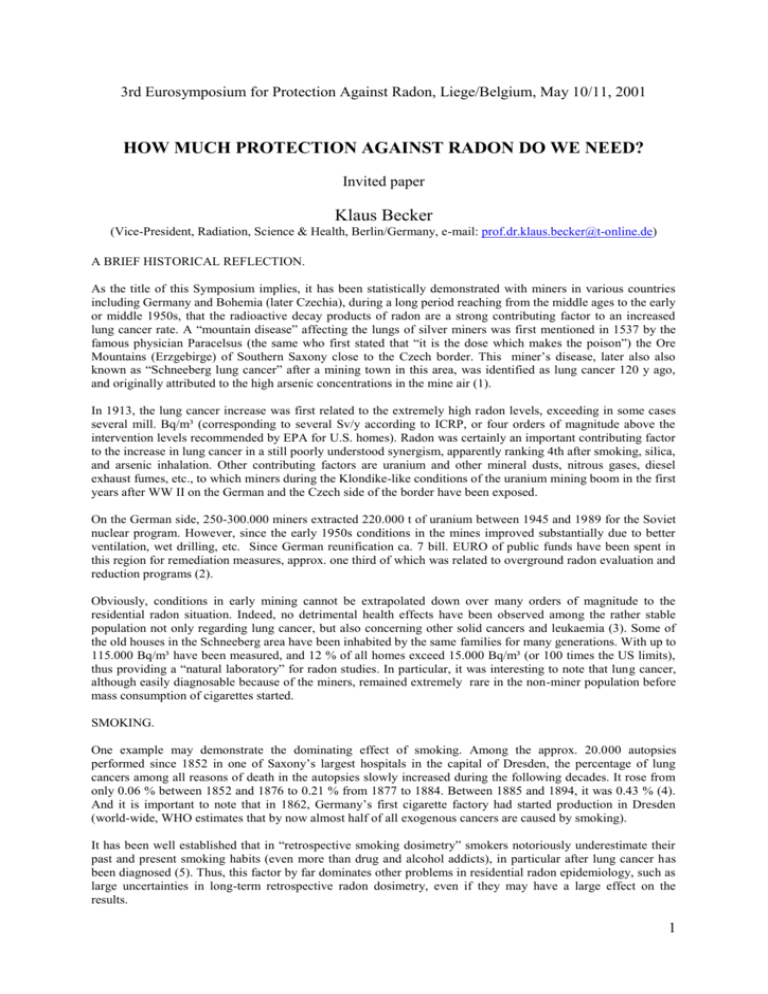
3rd Eurosymposium for Protection Against Radon, Liege/Belgium, May 10/11, 2001 HOW MUCH PROTECTION AGAINST RADON DO WE NEED? Invited paper Klaus Becker (Vice-President, Radiation, Science & Health, Berlin/Germany, e-mail: prof.dr.klaus.becker@t-online.de) A BRIEF HISTORICAL REFLECTION. As the title of this Symposium implies, it has been statistically demonstrated with miners in various countries including Germany and Bohemia (later Czechia), during a long period reaching from the middle ages to the early or middle 1950s, that the radioactive decay products of radon are a strong contributing factor to an increased lung cancer rate. A “mountain disease” affecting the lungs of silver miners was first mentioned in 1537 by the famous physician Paracelsus (the same who first stated that “it is the dose which makes the poison”) the Ore Mountains (Erzgebirge) of Southern Saxony close to the Czech border. This miner’s disease, later also also known as “Schneeberg lung cancer” after a mining town in this area, was identified as lung cancer 120 y ago, and originally attributed to the high arsenic concentrations in the mine air (1). In 1913, the lung cancer increase was first related to the extremely high radon levels, exceeding in some cases several mill. Bq/m³ (corresponding to several Sv/y according to ICRP, or four orders of magnitude above the intervention levels recommended by EPA for U.S. homes). Radon was certainly an important contributing factor to the increase in lung cancer in a still poorly understood synergism, apparently ranking 4th after smoking, silica, and arsenic inhalation. Other contributing factors are uranium and other mineral dusts, nitrous gases, diesel exhaust fumes, etc., to which miners during the Klondike-like conditions of the uranium mining boom in the first years after WW II on the German and the Czech side of the border have been exposed. On the German side, 250-300.000 miners extracted 220.000 t of uranium between 1945 and 1989 for the Soviet nuclear program. However, since the early 1950s conditions in the mines improved substantially due to better ventilation, wet drilling, etc. Since German reunification ca. 7 bill. EURO of public funds have been spent in this region for remediation measures, approx. one third of which was related to overground radon evaluation and reduction programs (2). Obviously, conditions in early mining cannot be extrapolated down over many orders of magnitude to the residential radon situation. Indeed, no detrimental health effects have been observed among the rather stable population not only regarding lung cancer, but also concerning other solid cancers and leukaemia (3). Some of the old houses in the Schneeberg area have been inhabited by the same families for many generations. With up to 115.000 Bq/m³ have been measured, and 12 % of all homes exceed 15.000 Bq/m³ (or 100 times the US limits), thus providing a “natural laboratory” for radon studies. In particular, it was interesting to note that lung cancer, although easily diagnosable because of the miners, remained extremely rare in the non-miner population before mass consumption of cigarettes started. SMOKING. One example may demonstrate the dominating effect of smoking. Among the approx. 20.000 autopsies performed since 1852 in one of Saxony’s largest hospitals in the capital of Dresden, the percentage of lung cancers among all reasons of death in the autopsies slowly increased during the following decades. It rose from only 0.06 % between 1852 and 1876 to 0.21 % from 1877 to 1884. Between 1885 and 1894, it was 0.43 % (4). And it is important to note that in 1862, Germany’s first cigarette factory had started production in Dresden (world-wide, WHO estimates that by now almost half of all exogenous cancers are caused by smoking). It has been well established that in “retrospective smoking dosimetry” smokers notoriously underestimate their past and present smoking habits (even more than drug and alcohol addicts), in particular after lung cancer has been diagnosed (5). Thus, this factor by far dominates other problems in residential radon epidemiology, such as large uncertainties in long-term retrospective radon dosimetry, even if they may have a large effect on the results. 1 In particular, the early radon dosimetry in uranium mines has been largely absent or very unreliable. Even today, radon concentrations in a room have been shown to fluctuate by a factor up to 500 depending on ventilation and other factors, structural changes over years are known to substantially influence radon levels, and changing construction codes (such as improved thermal insulation due to a new German energy Conservation Law) are likely to have a serious impact on the further development of residential radon levels. There have been many attempts to establish an equivalent between the assumed risks of residential radon and smoking habits. During a Biophysics Colloquium in the radon spa Bad Schlema near Schneeberg in 1993, top European radon researchers quoted numbers between 500 WLM equivalent to 1 pack of cigarettes/day, and as little as one cigarette/day (thus reaching the realm of passive smoking) corresponding to an assumed doubling risk of 400 Bq/m³ (6) - which is almost twice of the currently discussed European 250 Bq/m³ limit for new buildings. Obviously, a misjudgement of only one cigarette/day may thus falsify most case-control studies, unless they are restricted to never-smokers. Typically, in such studies the number of the ever-smokers among the lung cancer cases is much larger than among the controls, e.g. in the Iowa Lung Cancer Study (7) 86 % of the lung cancer cases were smokers, but only 32 % of the controls. EPIDEMIOLOGY HIDDEN BEHIND A SMOKE SCREEN? For a non-epidemiologist, the multitude of published results are confusing. The most frequently quoted metaanalysis of case-control studies (8) compiles the very different results of nine such studies in seven countries. Of about 30 data points with very large vertical error bars, but no horizontal bars relating to the rather difficult retrospective radon dosimetry, only one from Sweden is slightly above the control line (Fig. 1). Even this single indication of a slight lung cancer increase at 450 Bq/m³ has, by the same group recently been shown to be transferable into a decrease (9) similar to those of the well-known and widely discussed large-scale ecological studies in the USA (10) in case the same type of evaluation is used. There are other meta-analysis studies in progress in the U.K. and Canada, which will incorporate the results of more recent case-control studies, e.g. in the U.K. (11) and the USA (7), with similar results not unlikely. In the high radon areas of former East Germany, one government-funded 10 mill. $ study (12) claims a slightly positive trend, while another sponsored by the E.U. and restricted to non-smoking females, finds clear indications of an initially negative trend and a threshold around 1000 Bq/m³ (13) (Fig. 2). As the most obvious factor for the explanation of such confusing data appears to emerge cigarette smoking. Fig. 1(left): Relative lung cancer risk as a function of residential radon according to a meta-analysis of casecontrol studies in seven countries in Europe, North America, and China (8). Fig. 2 (right): The relative lung cancer risk according to the LNT hypothesis of ICRP and BEIR VI compared to the results of the case-control GRS German radon study (12), and of another international case-control study restricted to never-smoking females (Schneeberg study, (13). Such developments raise a number of interesting questions. Even the BEIR VI Report does not exclude the possibility of a threshold value. There are reasonable mechanistic models consistent with an U-shaped doseresponse relationship for radon (14), and it was recently stated (15) that „epidemiological evidence to support (EPA) conclusions is either absent or not convincing. A more reasonable conclusion is that lung cancer risk is insignificant for radon concentrations below 400 Bq/m-³. Radon does not pose a threat to the public health in the 2 domestic environment." This confirms a suspicion which was already expressed over a decade ago, that „with radon an artificial disease has been created by the multiplication of a very small risk with large populations, in order to obtain frightening numbers“ (16). SUPPORTING EVIDENCE AND RADON BALNEOLOGY. There are many research data which directly or indirectly support such conclusions, of which only a few can be listed here as examples: 1. Because of various factors which have so far been largely neglected, such as different aerosol size and daughter product attachment factors, as well as additional radiation factors such as the inhalation of Rn-220 (thoron) decay products, long-lived radioactive dust, and external gamma radiation, the actual lung exposures of underground miners are likely to be much higher (up to a factor of 5-10) than previously estimated (27), which implies an overestimate of residential radon effects by the same factor. 2. The bronchial alpha dose attributed to radon progeny has been subject to many modifications in the past, and still differs substantially depending on the lung model used. 3. The relative risk of lung cancer for external low-LET exposures decreases, contrary to the LNT hypothesis, before reaching a threshold around 2 Gy (17 - Fig. 3). 4. Experimental animal studies (18) demonstrate a RBE for lung cancer induction by alpha radiation of 2 instead of 20 as assumed by ICRP. 5. There is experimental evidence for a definitely non-linear radon effect, amounting to an overestimation of residential radon risks, which has recently been provided in single alpha particle exposures of mammalian cells (19). 6. Regarding incorporated alpha emitters such as Ra and Pu in humans and animals, there is substantial evidence for no detectable effect up to at least 2-4 Gy (20 - Fig. 4). 7. Animal experiments demonstrate that it is more the radon inhalation dose-rate than the integrated dose which determines the lung cancer induction (21). Moreover, radiobiological evidence accumulates demonstrating basic differences in radiobiological response between low and high doses and dose-rates. Fig. 3 (left): Relative lung cancer risk in humans as a function of external X- and gamma exposures (17). Fig. 4 (right): Bone sarcoma incidence in female radium dial painters, with the systematic intake of Ra 226 and 228 corresponding to a practical threshold of 10 Gy (20). Even more importantly, the substantial historical evidence of beneficial effects of radon on human health should not be forgotten - even if there could, in principle, be some overlap of effects with the beneficial dominating under some, and slightly negative under other circumstances, an effect well-known in pharmacology. In fact, radon may be one of mankind’s oldest therapies: The ancient Romans and other old civilizations appreciated radon spas; and in Japan, the springs on Misasa (up to 160.000 Bq/l of radon in drinking water), have been used for 800 years (for reviews, 22,23). Currently, about 75.000 patients annually are treated in German and Austrian radon spas, and many more in other countries, in particular in Russia, mostly for painful joint or backbone diseases such as rheumatic arthritis and spondilytis ankylosans (Morbus Bechterew). The treatment is by inhaling high radon concentrations (in the Bad Gastein „Heilstollen“, for example, about 170.000 Bq/m³), by drinking, or by bathing in radon water. The expenses (e. g. in Bad Gastein about $ 500 for 10 h of treatment) are 3 mostly paid by the public health insurance systems. Even in the more radiophobic USA, a “radon health mine“ has been operating successfully for half a century. Clinical studies including randomized double-blind studies clearly demonstrated the superior effect of radon in comparison with an otherwise identical treatment, lasting for several months after the end of the treatment. Various mechanisms have been suggested as explanation of such beneficial effects involving radiation doses in the order of only one mGy, including stimulation of repair or radical scavenger enzymes, or the production of neuropeptides, but there are still many open questions. However, considering the practical success and acceptance of radon treatments by the patients suffering from severe pains, radon balneology has recently been accepted (similar to other treatments for which there is not yet a profound scientific explanation) by German authorities. Thus it is not surprising that the radon medical treatment center of Bad Schlema, which has been very popular up to the end of WW II as “the world’s strongest radon source”, was officially reopened a few years ago and is again, like the nearby old “St. Joachimstal”, very popular among health-seeking patients. DISCUSSION AND CONCLUSIONS. The current residential radon “dangers” may be summarized as follows 1,24): 1. The regulatory situation is inconsistent, with suggested intervention levels fluctuating between countries by fairly large factors, and ICRP recommending a radon limit for the population which is by a factor of 10 larger than for external gamma radiation. 2. The underlying linear extrapolation from high miner exposures to low levels in homes appears to be not feasible because of significantly different confounding factors and dose levels, and different radiobiological response mechanism at high and low dose levels. 3. Epidemiological studies indicating a small relative risk increase for increased residential levels appear to be subject to large errors, in particular in the retrospective determination of smoking habits. 4. There is evidence for a threshold, or an U-shaped response curve, perhaps explaining some of the beneficial effects of radon balneology. Up to about 1000 Bq/m³, lung cancer appears to be to attributable to smoking only. 5. In all but very few exceptional cases, such as extremely high radon levels in the homes of heavy smokers, the cost/benefit ratio of residential radon programs does not justify the investment of private or public funds. In order to avoid the increasing habit of “selective quoting” in the discussion about residential radon and its relation to smoking, it should also be mentioned that there are data which appear to confirm that, despite the overwhelming effect of smoking, residential radon provides a contribution to the total lung cancer rate approximately in agreement with miner and ICRP data. Comparing, for example, the lung cancers in the Netherlands and in Sweden in 1995, it has been calculated that that “between 72 and 94 % of the registered lung cancer cases may be attributed to the combined effects of radon and smoking”, and that “in the Netherlands, a portion of about 4 % and in Sweden 20%… may be attributable to radon exposure…”(25). Apparently both sides in this discussion believe to have good arguments (26), but undisputed evidence is still missing in the muddy waters around the limits of detectability, and may remain forever hidden in the noise of the statistical background. So do we really have to worry about – and to spend substantial public funds – on possible public health problems too small to be clearly detectable? If considered in a larger social, economical and ethical context, the residential radon controversy thus has implications for other fields of risk/benefit assessment and regulatory control beyond radiation protection, because artificially created statistical problems should not require expensive solutions. Among the serious questions to ask are: Should we really care about potential small risks of small radiation doses which, if they exist at all, could not yet be detected despite immense research efforts over decades? How much of a society’s limited funds should be devoted to the further reduction of such hypothetical risks? How does the cost/benefit ratio of such measures compare to that for other natural and man-made hazards? And how could such a degeneration of over-conservative administrative concepts into serious hazards to national economies be quickly remedied and prevented in the future? These and many other topics clearly exceed the scope of such a brief summary. Some recent references and compilations: (1) K. Becker, Is residential radon dangerous? Excerpta Medica Int. Congr. Ser. 1203 “The Effects of Low and Very low Doses of Ionizing Radiation an Human Health, Elsevier 2000 (ISBN 0-444-50513-x), 191-173 (2) K. Becker, Wie teuer ist uns Radon – und weshalb? Atw 41/2, 108-109, 1996 4 (3) J. Conrady, N. Nagel, K. Martin, Vergleichende Analyse der räumlichen und zeitlichen Verteilung von Krebserkrankungsfällen, Report Staatsminist. Für Umwelt et., freistaat Sachsen, Dresden 1997 – see also paper, Ann. Meet. German Nucl. Soc. Munich 1998 (4) W. Schüttmann, Bewertung des Lungenkrebsrisikos durch Wohnungsradon, Strahlenschutzpraxis 5, No. 4, 35-40, 1999 (5) J. Conrady, K. Martin, J-. Lembcke, H. Martin, The true size of lung cancer risk from indoor radon: Hidden behind a smoke screen? Excerpta Medica Int. Congr. Series, Elsevier 2001 (in press) (6) K. Aurand et al., Nutzen und Risiko bei der Einwirkung kleiner Dosen ionisierender Strahlung, 2 nd Ed. (ISSN 0949-8540), 246-247, 1995 (7) R. W. Field., et.al., Residential radon gas exposure – The Iowa lung cancer study, Americ. J. Epidem. 151/11, 1091-1102, 2000 (8) J. H. Lubin, J.D. Boice, Lung cancer risk from residential radon: Meta-analysis eight epidemiological studies, J. Nt. Canc. Insz 89, 49-57, 1997 (9) F. Lagarde et al., Residential radon and lung cancer in Sweden : Risk analysis accounting for random error in the exposure assessment, health phys. 72, 269-276, 1997 (10) B. L. Cohen, Test of the linear no-threshold theory of radiation cancerogenesis for inhaled radon decay products, Health phys. 68, 157-174, 1995 (11) S. Darby et al., Risk of lunf cancer associated with residential radon in SW England : A case-control study. Br. J. Cancer78, 394-408, 1998 (12) H. E. Wichmann et al., Lungenkrebsrisiko durch Radon in der BRD (Ost) – Thüringen und Sachsen, ecomed (ISBN 3-609-51850-2), 1999 (13) J. Conrady, et al., High residential radon health effects in Saxony (Schneeberg Study), Contract F 14PCT95-0027, European Commission, DG XII, August 1999 (14) K. T. Bogen, Mechanistic model predicts a U-shaped relation of radon exposure and lung cancer risk, Human Experim. Toxicol. 17, 691-696, 1998 (15) K. L. Mossman, Is indoor radon a public health hazard? The BEIR VI Report, Radiat. Prot. Dos. 80, no. 4, 357-360, 1998 (16) J. L. Letourneau,, J. Americ. Medic. Assoc., Aug. 7, 578, 1987 (17) H. H. Rossi, and Zaider, M., Radiogenic lung cancer: The effect of low doses of low-LET radiation, Radiat. Environm. Biophys. 36, 85-88, 1997 (18) J. P. Kellington., et al., Effects of radiation quality on the lung cancer in CBA/Ca mice, Proceed. Internat. Conf. Health effects of Low Level Radiat., Stratford-on-Avon, BNED London, 44-51, 1997 (19) R. C. Miller,, et al., The oncogenic transformation potential of the passage of single alpha particles through mammalian cell nuclei. Proc. Nat. Acad. Sci. USA, 96, 19-22, 1999 (20) R. E. Rowland, dose-response relationship for female Ra dial painters: a new look, in: Health effects of internally deposited Radionuclides, World Scientific, London, 135-143, 1995 (21) G. Monchaud , J. P. Morlier, Influence of dose-rate on lung cancer induction in rats exposed to radon and its progeny, in: Excerpta medica, Internat .Conf. Ser. ICS 1225, Elsevier 2001, in print (22) P .Deetjen., and Falkenbach, A. (Ed.), Radon and Health, P. Lang Verlag (ISBN 3-631-35532-7), 1999 (23) G. Pratzel, P. Deetjen, Radon in der Kurortmedizin, ISMH Verlag (ISBN 3-9804437-2-8, 1997 (24) K. Becker, and Schüttmann, W., Was ist eigentlich aus dem Radon geworden? Strahlenschutzpraxis 4/1, 54-58, 1998 (25) H.P. Leenhouts, M.J.P. Brugmans, Calculation of the 1995 lung cancer incidence in the Netherlands and Sweden caused by smoking and radon: Risk implications for radon. Radiat. Environm. Biophys. 40, 11-21, 2001 (26) K. Becker, R. W. Field, Debate: How dangerous is residential radon? Radiat. Protect. Dos., in print (2001) (27) P. Duport, Is the radon risk overestimated ? Neglected doses in the stimation of the risk of lung cancer in uranium underground miners, submitted for publication 5