Operative Report 4
advertisement
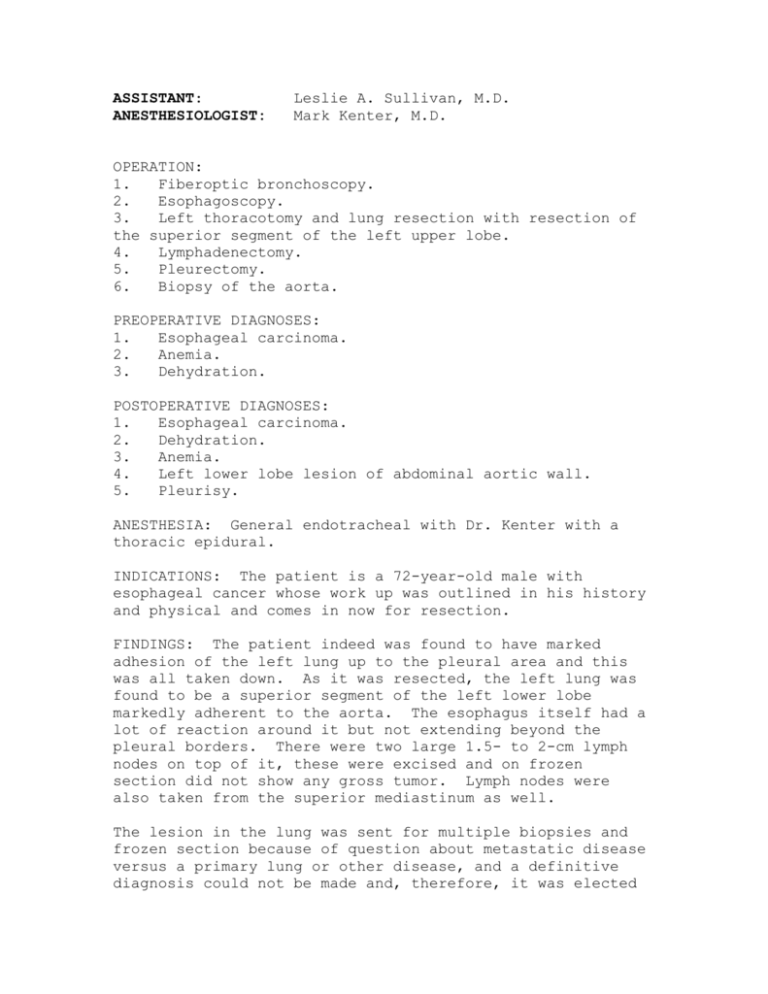
ASSISTANT: ANESTHESIOLOGIST: Leslie A. Sullivan, M.D. Mark Kenter, M.D. OPERATION: 1. Fiberoptic bronchoscopy. 2. Esophagoscopy. 3. Left thoracotomy and lung resection with resection of the superior segment of the left upper lobe. 4. Lymphadenectomy. 5. Pleurectomy. 6. Biopsy of the aorta. PREOPERATIVE DIAGNOSES: 1. Esophageal carcinoma. 2. Anemia. 3. Dehydration. POSTOPERATIVE DIAGNOSES: 1. Esophageal carcinoma. 2. Dehydration. 3. Anemia. 4. Left lower lobe lesion of abdominal aortic wall. 5. Pleurisy. ANESTHESIA: General endotracheal with Dr. Kenter with a thoracic epidural. INDICATIONS: The patient is a 72-year-old male with esophageal cancer whose work up was outlined in his history and physical and comes in now for resection. FINDINGS: The patient indeed was found to have marked adhesion of the left lung up to the pleural area and this was all taken down. As it was resected, the left lung was found to be a superior segment of the left lower lobe markedly adherent to the aorta. The esophagus itself had a lot of reaction around it but not extending beyond the pleural borders. There were two large 1.5- to 2-cm lymph nodes on top of it, these were excised and on frozen section did not show any gross tumor. Lymph nodes were also taken from the superior mediastinum as well. The lesion in the lung was sent for multiple biopsies and frozen section because of question about metastatic disease versus a primary lung or other disease, and a definitive diagnosis could not be made and, therefore, it was elected not to proceed with the esophagectomy. The lesion was growing into the aortic wall and on the adventitia there was about a 4.5 x 5-cm area of the adventitia that was involved. Care was taken not to disturb this and several biopsies were taken around the edges of it and some sent for cultures as well as for final pathology. After the lung was resected, there was no significant air leak. On the esophagoscopy the patient did have a tumor that was extruding into the lumen at 34 cm, though some of it, however, did not show any obvious abnormalities. At the end of the procedure, the patient was able to be awakened and extubated and taken to the postoperative anesthesia recovery room in stable condition. PROCEDURE: The patient was placed on the table in the supine position and after placement of an IV, arterial line, Foley catheter, general endotracheal anesthesia was induced. A thoracic epidural had previously been placed. The fiberoptic bronchoscope was passed and there was no evidence of any endobronchial lesions. The scope was removed, esophagoscope was passed with the findings as noted above. The scope was then removed and the patient was then placed in the right lateral decubitus position, the left chest prepped and draped in the usual sterile fashion. A left lateral thoracotomy was performed sparing the latissimus dorsi going into the 6th intercostal space. The esophagus was found as noted; however, the lung was markedly adherent to the whole area of the posterior chest wall around the spine and this was carefully freed up and a pleurectomy was done. Then it was found that the left lower lobe, as we went through the fissure, separated that with the GIA stapler, was markedly adherent to the aorta. After this was freed up and dissected out, the aorta could be seen more medially and this was freed up and indeed there was marked reaction around the pleura but there was no evidence of tumor spreading beyond the pleural surface. There were two several large lymph nodes about 1.5 to 2 cm on the superior surface of the aorta as noted on the ultrasound and these were both resected and biopsied. There were also nodes up along the superior mediastinum which were dissected off and indeed on frozen section showed no cancer. Returning attention then to the lung, it became apparent that there was a lesion in the superior segment of the left upper lobe, it was about 4.5 to 5 cm, that was adherent to the aorta. It was, therefore, elected to carefully resect the lung around where they entered through the pleura and then a space was able to be made and a segmental resection was done of the left lower lobe superior segment and leaving it adherent to the aorta. After this was freed up, it became apparent there were no other nodes around in the hilum to suggest it was small metastatic disease, it was then carefully freed up and it was found to be adherent to the adventitia. This was taken off and indeed there was a space left that was about 4.5 x 5 cm in the adventitia to the aorta. Several biopsies were taken around the edge of this and again on frozen could not be sure there was metastatic disease and some was sent for final pathology. A portion also was sent for cultures as well. After this was freed up, the remainder of the lung expanded well. This whole segment was abnormal but the remainder of the left lower lobe did not have any obvious abnormalities and any evidence of metastatic disease. The inferior pulmonary ligament was freed up from the inferior pulmonary vein. Not being sure whether this was metastatic disease, infection or what the inflammation was and knowing that we would not necessarily want an esophagogastrectomy in the area if indeed anything needed to be done to the aorta such as putting a graft in, it was elected not to proceed with esophageal resection and attention was turned to closure. The area of the segment of resection was oversewn with interlocking #3-0 chromic suture and right angle and straight #36 French chest tubes were placed through stab wounds and secured with #0 silk suture. Attention was turned to closure. Double pericostals were placed and the muscles were reapproximated with #0 Vicryl suture. The subcutaneous tissue was closed with continuous suture of #2-0 Vicryl and the skin was approximated with subcuticular stitch of #3-0 Vicryl. At the end of the procedure, the sponge, needle and instrument counts were correct. ESTIMATED BLOOD LOSS: 500 mL through pleurectomy. REPLACEMENT: Two (2) units of packed cells, 500 mL of albumin and 800 mL of crystalloid. DRAINS: Two #36 French chest tubes. The patient's wound was dressed, he was placed in the supine position, was extubated and taken to the postoperative anesthesia recovery room in stable condition. The patient had minimal air leak and on the chest x-ray showed good expansion of the left lung. He was awake and moving all extremities well and alert and conscious.