AE_presentation_summary
advertisement

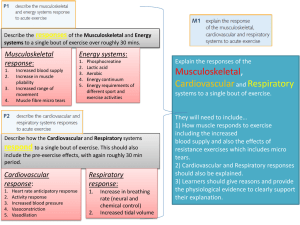
DATA-DRIVEN MULTISCALE ANALYSIS IN MUSCULOSKELETAL BIOMECHANICS Ahmet Erdemir, PhD Computational Biomodeling (CoBi) Core and Department of Biomedical Engineering Lerner Research Institute, Cleveland Clinic During many movement tasks of daily activities such as walking, motor control system sends signals to the muscles to activate; muscles fire to generate forces; these forces are applied to the bones and joints to balance external loading as well as to achieve the goals of locomotion. In the meanwhile, the loads on the joints are distributed to various tissue structures; and within tissue structures the loads are distributed to the various components of the microstructural architecture and cells. Adequate function of this mechanical pathway is not only important for desired mobility but also for tactile sensation as well as mechanobiological response at various spatial scales. Existence of mechanical forces (or their lack of) significantly influence the processes of growth, healing, and adaptation, all a result of cells responding to body level loading changes. It is possible for example, to encourage bone remodelling (dictated by cellular processes) simply by prescription of standing on a vibrating platform to those at risk of osteoporosis1. The mechanical pathways of load sharing may be disturbed by disorders at different spatial scales. In aging, neuromuscular control patterns diminish2, joints become stiffer3, the movement patterns alter4, tissue morphology changes5, and microstructural and cellular properties of the tissue degrade6. If primary mechanical load characteristics at various spatial scales can be measured, diagnostics and interventions relying on such information can be devised. For example, we may be able to identify age related risk factors associated with cartilage degeneration. From a musculoskeletal perspective, at the spatial scale of the body (as well as organs and joints), measurements of joint and organ kinematics, i.e., how they move (such as knee rotations), and kinetics, e.g., their load bearing capacity, have significance for biomechanics research and implications in clinics. Combined with data on overall tissue loading (muscle forces, contact loads, ligament forces, etc.), such information can have diagnostics value, acts as an accessible intervention target, and relates to daily activities of living, which can be assessed in the field with ease. One can use gait analysis, for in vivo measurement of musculoskeletal movements, muscle activity and external body loading. Yet, such examinations provide only partial data for joint and tissue function. To advance our scientific understanding of musculoskeletal function, controlled experiments can be conducted on cadaver specimens allowing detailed joint structural response and overall tissue forces under lifelike loading scenarios7. At the spatial scale of the tissues, localized tissue stress and strain distributions (for example deformation of individual ligament bundles, cartilage contact pressures) are data of interest. Tissues are common mechanical intervention targets, e.g., tendon reconstruction, and patient-specific data on their localized response has diagnostic value for pathological conditions and can be utilized for damage risk assessment. Unfortunately, in vivo measurements of tissue mechanics can be challenging. It is not surprising that many investigations focused on cadaver experimentation to understand localized tissue response such as patellofemoral joint contact mechanics, or relied on isolated loading conditions on special occasions, i.e. using magnetic resonance imaging for in vivo measurement of tissue deformations in the foot under compressive loads8. Recent investigations to accurately quantify in vivo bone movements, e.g. bi-planar fluoroscopy9, also provided the capacity to implicitly determine ligaments strains and contact mechanics. At the spatial scale of cells (and the tissue microstructure), it is desirable to measure cell deformations (dictated by volume and aspect ratio change for example) and also microstructural loading, i.e. fiber forces. Cells, due to their mechanobiological response and their capacity to maintain the structural integrity of their environment, are intervention targets from a biological and chemical perspective. Their mechanical damage risk, if identified, may help establishing preventive measures to accommodate their healthy function. Cell deformations can be measured by a handful of imaging modalities, i.e. confocal laser scanning microscopy, yet commonly under simplified loading conditions. The test samples are usually single cells and cell-seeded constructs and in some cases in situ tissue testing is also possible. Through these measurements, identification of cell damage is possible along with the relationship between cell deformations and local macroscopic deformations. Multiscale measurements of musculoskeletal function has recently become possible through animal studies. A handful of investigations attempted to relate muscle and joint loading with deformation of chondrocytes in the mouse knee10. Translation of this knowledge (as well as the technology) to evaluate musculoskeletal function of the human body remains challenging. Our lack of technology to directly measure mechanical variables of musculoskeletal loading can be accommodated through computational modeling and simulation that has the potential to establish such knowledge. Musculoskeletal movement simulations can utilize body level measurements, i.e., those obtained from gait analysis, to estimate organ, joint, and tissue level forces. These simulations rely on the abstraction of muscles, joints, passive structures, external loading, and neuromuscular control. The approach has significance to understand motor control strategies, muscle function, and the interactions of the body with its environment. Such simulations can be conducted in a purely predictive fashion to evaluate strategies for management of mobility disorders, movement related rehabilitation, surgical outcome, and performance enhancing interventions. Traditional tools of mechanical engineering, in particular inverse dynamics, forward dynamics, and optimal control, are commonly utilized to estimate muscle forces and net joint loading from gait data11. For example, this approach has been used to quantify forces in the plantar aponeurosis and toe flexors based on movement data obtained from a toe rise task12. In following, compensation mechanisms, i.e. increased muscle forces, were also predicted, if one wanted to conduct the same task but following plantar fasciotomy (release of plantar aponeurosis for management of heel pain). At the interface of joint and tissue spatial scales, simulations of organ loading help relate joint level measurements to tissue level deformations. Models of this spatial scale abstract joints and organs, tissue components, interactions between tissues, and joint and organ loading. Simulations help establish load sharing between tissues. In return, they can be utilized for the exploration of injury mechanisms, joint and tissue reconstruction, surgical corrections, and joint and tissue related dysfunction. Finite element analysis is a commonly utilized technique13. For example, a model of the knee joint can provide stress-strain distributions within its structures ( cartilage, menisci, ligaments) along with overall joint kinematics and kinetics. At a lower spatial scale, simulations of tissue deformations establish the mechanical pathway between tissue level measurements and cell level deformations. Cells, pericellular matrix, and extracellular matrix (sometimes including fiber architecture) are all represented in models of this scale with abstractions of cell-extracellular matrix interactions and tissue loading. These simulations can significantly enhance our understanding of the mechanical role of microstructure14, cell mechanobiology and its dysfunction, and microscopic damage mechanisms. They also have implications for tissue engineering that commonly relies on micromechanical environment of cells. Among many techniques, finite element analysis serves as a powerful tool to simulate micromechanics. Not only isolated investigation of a single cell is possible but multi-cell volume constructs can be investigated to explore mechanical interactions between cells. Multiscale simulations go further and associate mechanical variables of different spatial scales to each other. One can couple musculoskeletal movement simulations and modeling of tissue deformations in a sequential post-processing manner or in a concurrent way where different spatial scales provide feedback. Such investigations have significance to identify compensatory movement strategies to accommodate tissue relief. They can link the function of somatosensory system to movement. Ultimately, designing musculoskeletal rehabilitation programs targeted at tissue level adjustments may be possible. Our recent studies was able to couple movement simulations with finite element analysis to identify neuromuscular control strategies that relieve plantar foot tissue stresses, while maintaining a normal walking pattern15. Multiscale simulations coupling organ/joint loading with cell deformations are also possible16. Again, this can be done in a post-processing sense, or simultaneous simulation approaches such as computational homogenization can be employed. Such analysis approaches have to potential to portray macro-level loads that can induce cell or fiber damage, can link body level forces to cell level mechanobiological processes. Cell targeted interventions prescribed at musculoskeletal joints can be designed. Our recent work for example, quantified chondrocyte (cells of the cartilage) deformations as a function of tibiofemoral joint loading, relying on thousands of micro-level simulations. In our research, one of our short-term goals is to quantify the mechanical environment of the knee cartilage during daily activities through a subject-specific modeling and simulation platform driven by movement data. Another one targets at incorporating in our models age related changes of the musculoskeletal system at various spatial scales, in order to explore age-related mechanical markers of potentially harmful chondrocyte deformations within the cartilage. Our long term goal is to establish a data integrated modeling and simulation platform spanning the body, joints, tissues, and cells, i) to identify body level musculoskeletal indicators of micro level cell mechanics, and ii) for personalized assessment of musculoskeletal function at multiple scales. Multiscale simulations of the musculoskeletal systems are driven by movement data, require data for representation of anatomy and mechanical properties, and are confirmed by data for evaluation of predictions against known cases. While anatomical information can be acquired easily, in vivo identification of mechanical properties rely on sophisticated analysis done in an inverse fashion 17. Scientific research exploring the assumptions of multiscale coupling, e.g. scale separation, representative models at lower spatial scales, will help establish confidence in multiscale modeling approaches. Combined with work on uncertainty estimation (potentially through sensitivity analysis) and verification & validation, predictions can be relied on for clinical decision making. Scientific investigations directed at establishing the minimum amount of data required for reliable predictions will likely increase the applicability of data-driven simulations as it may diminish subject-specific data collection burden in the field. Technological developments that will lead in to robust engineering tools will provide accessible, cost-effective, practice-oriented platforms preventing current potentially error prone and difficult to use “duct-tape” approach in multiscale simulations. Development of consensus driven standards for data collection and storage, for model exchange, and for reporting will facilitate reusability, and establishes a foundation for reproducibility and accountability. Progress in engineering approaches, i.e. costeffective coupling strategies such as adaptive surrogate modeling18, and automated model generation, will facilitate investigations relying on multiscale simulations. Organized dissemination (documented, versioned, standard compliant) of data, models, and simulation results will provide building blocks for model development and simulation efforts. Unnecessary reproduction of work can be avoided through accessibility. Streamlined access to model libraries and databases, particularly when supported by non-restricting licensing for use and redistribution, will help expedited data-driven simulation studies. Robust and interchangeable software with liberal licensing mechanisms will allow efficient prototyping of simulation-based data processing approaches for descriptive and predictive analysis. Similarly, easy to use computational hardware, i.e. supercomputing architectures, available on a timely basis, will improve delivery of results back to the field of application. Open-community driven development of models19 have the potential for expediting incorporation of new features, implementation of models for different problems, and crowd-sourced testing. Translation of data-driven simulation approaches from research environments to practice in the clinics is certainly possible. Yet, the modeling and simulation community needs to match the promise of scientific and technological advancements with the need in the medical field. Capacity to easily collect data in a practical setting, and transfer it to the modeling analyst, are important to realize simulation-based medicine. Modeling and simulation process should be feasible and reliable, in order to accommodate clinical urgency and to establish confidence for decision-making. Consistency of communication of modeling approaches and simulation results within and across disciplines is a commonly neglected issue. To overcome cultural barriers and to prevent ambiguity, guidelines may need to be established20. Mechanobiology of the musculoskeletal system dictates understanding of its mechanical environment at multiple spatial and temporal levels. With current state-of-the-art, direct and easy access to primary data of musculoskeletal system is limited. Data-driven simulations at single spatial scales provide opportunities for estimation of primary musculoskeletal variables. Multiscale simulations can further provide opportunities for estimation of primary musculoskeletal variables of different scales in a relational manner. Focused research on temporal coupling will also provide exploration of time-dependent activities including development, growth, and aging processes. Research efforts should accommodate novel data acquisition techniques to measure primary musculoskeletal variables. Concurrent work on multiscale modeling and simulation will not only support measurement technology but will also provide a predictive platform for “what if” type of questions. Developments should address many different aspects of our research culture; scientific, technological, social, and translational. Ahmet Erdemir's contributions were funded by National Institute of Biomedical Imaging and Bioengineering, National Institutes of Health (R01EB009643). Keywords. musculoskeletal system, tissue biomechanics, cell mechanics, finite element analysis, optimization References 1. Establishing the compliance in elderly women for use of a low level mechanical stress device in a clinical osteoporosis study. Hannan MT, Cheng DM, Green E, Swift C, Rubin CT, Kiel DP. Osteoporos Int. 2004 Nov;15(11):918-26. 2. Dynamics and stability of muscle activations during walking in healthy young and older adults. Kang HG, Dingwell JB. J Biomech. 2009 Oct 16;42(14):2231-7. 3. Age-related changes in the interactive mobility of the hip and knee joints: a geometrical analysis. Nonaka H, Mita K, Watakabe M, Akataki K, Suzuki N, Okuwa T, Yabe K. Gait Posture. 2002 Jun;15(3):236-43. 4. Evidence of mechanical load redistribution at the knee joint in the elderly when ascending stairs and ramps. Karamanidis K, Arampatzis A. Ann Biomed Eng. 2009 Mar;37(3):467-76. 5. Age-related changes in the morphology and deformational behavior of knee joint cartilage. Hudelmaier M, Glaser C, Hohe J, Englmeier KH, Reiser M, Putz R, Eckstein F. Arthritis Rheum. 2001 Nov;44(11):2556-61. 6. Age- and site-associated biomechanical weakening of human articular cartilage of the femoral condyle. Temple MM, Bae WC, Chen MQ, Lotz M, Amiel D, Coutts RD, Sah RL. Osteoarthritis Cartilage. 2007 Sep;15(9):1042-52. 7. Dynamic loading of the plantar aponeurosis in walking. Erdemir A, Hamel AJ, Fauth AR, Piazza SJ, Sharkey NA. J Bone Joint Surg Am. 2004 Mar;86-A(3):546-52. 8. An MRI-compatible foot-loading device for assessment of internal tissue deformation. Petre M, Erdemir A, Cavanagh PR. J Biomech. 2008;41(2):470-4 9. Measurement of in vivo anterior cruciate ligament strain during dynamic jump landing. Taylor KA, Terry ME, Utturkar GM, Spritzer CE, Queen RM, Irribarra LA, Garrett WE, DeFrate LE. J Biomech. 2011 Feb 3;44(3):365-71. 10. A novel method for determining articular cartilage chondrocyte mechanics in vivo. Abusara Z, Seerattan R, Leumann A, Thompson R, Herzog W. J Biomech. 2011 Mar 15;44(5):930-4 11. Model-based estimation of muscle forces exerted during movements. Erdemir A, McLean S, Herzog W, van den Bogert AJ. Clin Biomech. 2007 Feb;22(2):131-54. 12. Changes in foot loading following plantar fasciotomy: a computer modeling study. Erdemir A, Piazza SJ. J Biomech Eng. 2004 Apr;126(2):237-43. 13. Finite Element Procedures. Bathe KJ. 2007, published by Klaus-Jurgen Bathe. 14. In-situ measurements of chondrocyte deformation under transient loading. Chahine NO, Hung CT, Ateshian GA. Eur Cell Mater. 2007 May 31;13:100-11. 15. Concurrent musculoskeletal dynamics and finite element analysis predicts altered gait patterns to reduce foot tissue loading. Halloran JP, Ackermann M, Erdemir A, van den Bogert AJ. J Biomech. 2010 Oct 19;43(14):2810-5. Epub 2010 Jun 22. 16. On the multiscale modeling of heart valve biomechanics in health and disease. Weinberg EJ, Shahmirzadi D, Mofrad MR. Biomech Model Mechanobiol. 2010 Aug;9(4):373-87. 17. An inverse finite-element model of heel-pad indentation. Erdemir A, Viveiros ML, Ulbrecht JS, Cavanagh PR. J Biomech. 2006;39(7):1279-86. 18. Adaptive surrogate modeling for efficient coupling of musculoskeletal control and tissue deformation models. Halloran JP, Erdemir A, van den Bogert AJ. J Biomech Eng. 2009 Jan;131(1):011014. 19. Open Knee: A Three-Dimensional Finite Element Representation of the Knee Joint, https://simtk.org/home/openknee, last accessed September 27, 2011. 20. Considerations for Reporting Finite Element Analysis Studies in Biomechanics, http://www.imagwiki.nibib.nih.gov/mediawiki/index.php?title=Reporting_in_FEA/JB_Edition, last accessed September 27, 2011.