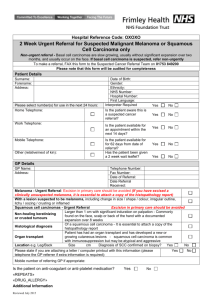
HAEMATOLOGY Suspected Cancer Referral
advertisement

HAEMATOLOGY Suspected Cancer Referral (2 Week Wait Referral) To support NICE guidance 2005 Please FAX within 24 hours to Cancer Pathways department: 020 8928 8836 Section 1 PATIENT INFORMATION (Please complete in BLOCK CAPITALS) Date of Referral Date of Birth NHS number UBRN SURNAME FIRST NAME Miss Mrs Ms Mr Other:_________ / / / / - - Home Tel. M[ ]F [ ] Mobile/Daytime Tel. Address Transport Y N Interpreter Y N Language Ethnicity Post Code Section 2 PRACTICE INFORMATION (Please use practice stamp if available) Referring GP Locum Practice Address Y N Telephone Fax Post Code Section 3 CLINICAL INFORMATION (please TICK all applicable entries) Please enclose print outs of CURRENT medications and PAST MEDICAL HISTORY [ ] UNEXPLAINED One or more of [ ] SIGNIFICANT BLOOD COUNT or PERSISTENT LYMPHADENOPATHY [ ] BONE PAIN / X-RAY BLOOD FILM SPLENOMEGALY suggestive of MYELOMA IF persisting for > 6 weeks suggestive of ACUTE [ ] HYPERCALCAEMIA without evidence of or > 2 cm or widespread LEUKAEMIA or [ ] RENAL IMPAIRMENT chronic liver disease or with splenomegaly or CHRONIC MYELOID [ ] ANAEMIA Please detail: with B symptoms LEUKAEMIA [ ] SPINAL CORD DISCUSS IMMEDIATELY BY TELEPHONE WITH DUTY HAEMATOLOGY CONSULTANT OR SpR WBC [ Hb [ Platelets [ Neutrophils [ Lymphocytes [ Investigations: ] ] ] ] ] COMPRESSION (If < 1cm, unlikely to be significant) With 2 or MORE of the following symptoms, particularly if [ ] SERUM PARAPROTEIN severe or associated with abnormal FBC [ ] URINARY BJP [ ] IMMUNE PARESIS [ ] Abdominal pain [ ] Bone pain [ ] Bruising/Bleeding Renal failure or spinal [ ] Fatigue cord compression in [ ] Fever suspected myeloma ~ [ ] Itching ~ generalised [ ] Night sweats ~drenching DISCUSS IMMEDIATELY [ ] Pain on drinking alcohol BY TELEPHONE WITH DUTY [ ] Recurrent infections HAEMATOLOGY [ ] Stomatitis/Mouth ulcers CONSULTANT OR SpR [ ] Weight loss One or more of Size [ ] cm Site(s) (please list) Before referring, please ensure glandular fever test is negative if patient <30 years and localised infections treated. Also consider HIV infection. Medical History, Known Allergies and Medication Discussed urgent suspected cancer referral with patient: Comments/other reasons for suspecting cancer Y N Hospital use only: (Tick where appropriate) Date Appointment Booked: Target Dates 2ww 62/7 / / / / / / Date of Referral receipt: Database: / Patient confirmed: / A separate letter only need accompany if you feel it necessary Approved by the North East London Cancer Network April 2006 LOCAL CONTACT DETAILS If you wish to discuss any clinical issues concerning this referral please contact: Dr Naim Akhtar Karen Bennett Consultant Haematology (Lead Clinician) 0208 535 6687 Clinical Nurse Specialist 0208 539 5522- Bleep 343 If you wish to discuss any other aspect of this referral please contact the Cancer Pathways Office on 020 8535 6856/ 020 8535 6768 x4348 x4350 CRITERIA FOR URGENT SUSPECTED CANCER REFERRAL1 Please FAX the referral form within 24 hours Refer a patient who presents with symptoms suggesting haematological cancer to a team specializing in the management of haematological cancer, depending on local arrangements. Be aware that haematological cancers can present with a variety of symptoms that may have a number of different clinical explanations. Combinations of the following symptoms and signs warrant full examination, further investigation (including a blood count and film) and possible referral: - fatigue - breathlessness - drenching night sweats - bruising - fever - bleeding - weight loss - recurrent infections - generalised itching - bone pain The urgency of referral depends on the symptom severity and findings of alcohol-induced pain abdominal pain lymphadenopathy splenomegaly investigations. For immediate referral above please telephone duty Haematology Consultant or SpR via switchboard Investigations In patients with: persistent unexplained fatigue carry out a FBC, blood film and ESR, plasma viscosity or C-reactive protein (according to local policy). Repeat at least once if the patient’s condition remains unexplained and does not improve unexplained lymphadenopathy carry out a FBC, blood film and ESR, plasma viscosity or C-reactive protein. Consider glandular fever test if age <30 and consider a course of antibiotics if lymphadenopathy localized. any of the following additional features of lymphadenopathy: - persistence for 6 weeks or more - lymph nodes increasing in size - lymph nodes greater than 2 cm in size - widespread nature - associated splenomegaly, night sweats or weight loss investigate further and/or refer unexplained bruising, bleeding and purpura or symptoms suggesting anaemia, carry out FBC, blood film, clotting screen and ESR, plasma viscosity or C-reactive protein (according to local policy) persistent and unexplained bone pain, carry out FBC and X-ray, urea and electrolytes, liver and bone profile, PSA test (in males) and ESR, plasma viscosity or C-reactive protein (according to local policy). 1 Based on Referral Guidelines for Suspected Cancer (NICE, 2005).. Notes in grey refer to the evidence grading used in the NICE guidelines, for more information see www.nice.org.uk/cg027NICEguideline