Ready for Review - Paramedic.EMSzone.com
advertisement
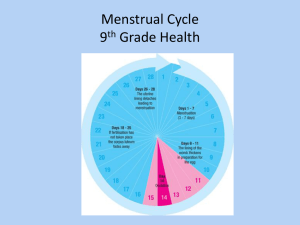
Gynaecology is the study of and care for diseases of the female reproductive system. The external anatomy of the female genitalia, sometimes referred to as the vulva, includes the mons pubis, labia majora, labia minora, perineum, clitoris, prepuce, and vestibule. The internal anatomy of the female genitalia includes the vagina, Bartholin glands, and the hymen (before rupture). Menstruation (menses or period) is the vaginal discharge of primarily blood that generally occurs every 25 to 34 days in premenopausal women. A woman can experience physical changes during the menstrual cycle that result in fluid retention, breast pain and tenderness, headache, cramping, and more intense emotional states. This premenstrual syndrome can be debilitating. The last menses is called menopause; it generally occurs between the ages of 40 and 50 years. Women may experience physical symptoms of menopause, including perspiring, hair loss, hot flushes, muscle aches and pains, headache, dyspnoea, vertigo, digestive problems, and emotional instability. Mittelschmerz is abdominal pain and cramping that occur about 2 weeks before menstruation. Dysmenorrhoea is painful menstruation. Prehospital treatment is supportive. Amenorrhoea is the absence or cessation of menses. The most common cause is pregnancy. Amenorrhoea can also occur in athletes and in people with anorexia nervosa or emotional problems. Endometritis is inflammation or irritation of the endometrium. Symptoms include malaise, fever, bowel problems, vaginal bleeding, abdominal distension, and lower abdominal or pelvic pain. Endometriosis is the growth of endometrial tissue outside of the uterus. It can cause infertility. Symptoms include low back, pelvic, or abdominal pain; pain experienced during sexual intercourse; elimination problems during menstruation; menstrual cramping; and heavy menstruation. Pelvic inflammatory disease (PID) is an infection of the female upper reproductive organs. One of the most common causes of abdominal pain in women, it can cause infertility. Interstitial cystitis is a chronically inflamed or irritated bladder wall. Symptoms may mimic those of gynaecological origin. In ectopic pregnancy, a fertilised egg implants somewhere other than the uterus, usually in a fallopian tube, which can lead to rupture of the fallopian tube. Ruptured ovarian cyst and tubo-ovarian abscess are other gynaecological conditions that can become an emergency. Toxic shock syndrome is a form of septic shock that can result from an infection in the body. Symptoms include syncope, mylagia, diarrhoea, vomiting, headache, fever, sore throat, petechiae, rash, and bloodshot eyes. Transport patients rapidly. Sexually transmitted infections (STIs) can cause PID. STIs include bacterial vaginosis, chancroid, chlamydia, cytomegalovirus, genital herpes, gonorrhoea, syphilis, and trichomoniasis. Symptoms of STIs can include itching, burning, pain, fishy smelling discharge, sores around the genitals, swollen or painful lymph glands, lower abdominal or back pain, nausea, fever, painful intercourse, bleeding between menstrual periods, fatigue, headache, and painful urination. When assessing a patient with a gynaecological emergency, begin by focusing on the ABCs. Protect the patient’s modesty at all times. Gynaecological emergencies can be very embarrassing for the patient. If the chief complaint is abdominal pain, investigate the pain by following the mnemonic LORDS TRACHEA: Location, Onset, Radiation, Duration, Severity, Timing, Relief, Aggravation, Character, History, Eating, and Associated symptoms. Determine when the patient had her last menstrual period, if it is unusual in any way, whether she could be pregnant, and whether she uses contraception. Vaginal bleeding that does not occur during the course of regular menstruation is cause for concern. Consider whether there is a mechanism of injury. Try to obtain an accurate description of the bleeding. During the patient history, obtain the patient’s obstetric history, including any previous pregnancies, miscarriages, or abortions. If the patient has a vaginal discharge, obtain a description of it. During the physical examination, determine whether there is a life-threatening condition. Inspect the abdomen for signs of abuse. Palpate the painful quadrant last. Abdominal pain can be visceral, parietal, or referred. Management should be psychologically supportive. General management for gynaecological emergencies is simple, including recognising immediate threats to life, preventing deterioration where possible, and protecting the patient’s modesty. Gynaecological trauma may cause profuse bleeding. Control external bleeding using pressure over the area, but never pack the vagina. Attempt to estimate the patient’s blood loss. Patients with PID will present with abdominal pain starting during or after menstruation. Take a thorough history and transport gently. The three life-threatening gynaecological emergencies are ectopic pregnancy, ruptured ovarian cyst, and tubo-ovarian abscess. Patients will present with abdominal pain and possibly vaginal bleeding, nausea, vomiting, or fever. Identify when each symptom began. Management includes airway maintenance, supplemental oxygen, positioning the patient on the left side, IV fluids, keeping the patient warm, monitoring the ECG, and transporting. Sexual assault is a category of crime that includes indecent assault and rape. Your compassion and professionalism in these situations are of the utmost importance. It may be difficult to obtain a history from a victim of rape. Have a female paramedic treat the patient when possible. Remember that your job is to clinically treat the patient. Ask only medical questions, and do not judge the patient. Limit the physical examination to addressing life-threatening injuries. Preserve evidence when possible. Try to persuade the rape victim not to clean herself. If a rape victim refuses transport, try to call a friend or relative with whom she can stay. Document cases of sexual assault properly and professionally. Report the patient’s words in quotation marks. Record facts obtained from the physical examination. Sexual emergencies may involve foreign objects stuck in the vagina or anus, which may potentially lead to internal injury. Do not remove the object. Remain professional, and transport the patient. Drugs used to facilitate rape include gamma-hydroxybutyrate (GHB), ketamine hydrochloride, ecstasy, and Rohypnol. These drugs can cause sleepiness, forgetfulness, numbness, loss of inhibitions, or rapid heart rate and increase in body temperature, depending on the drug.