Case Title - Drs. Fine, Hoffman and Packer
advertisement
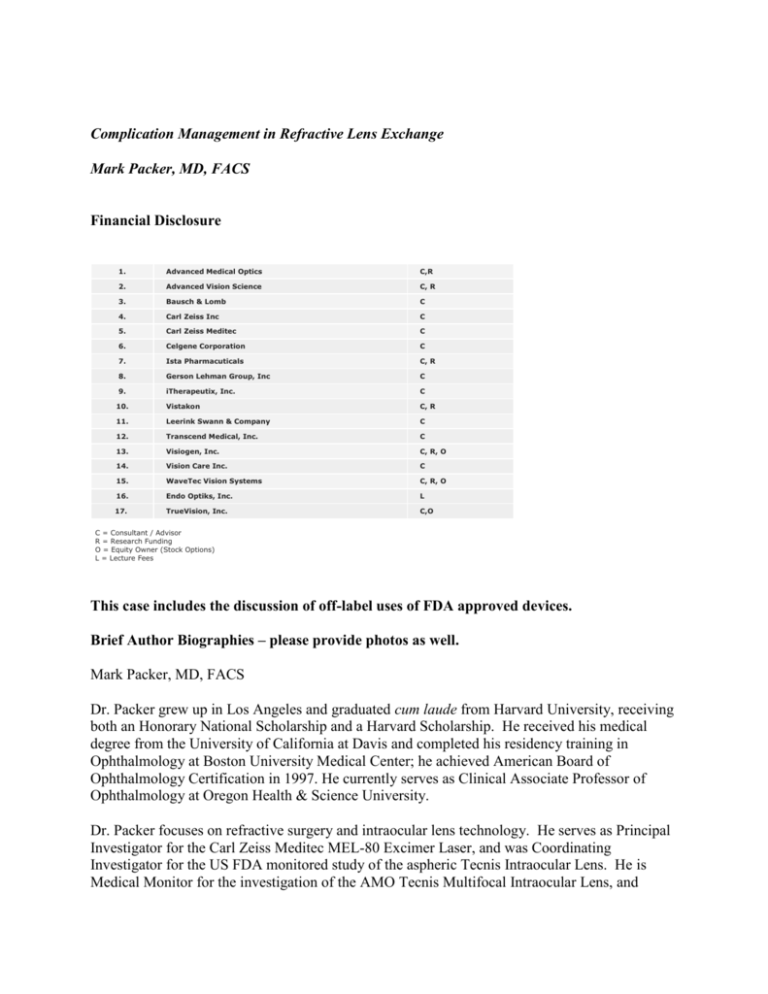
Complication Management in Refractive Lens Exchange Mark Packer, MD, FACS Financial Disclosure 1. Advanced Medical Optics C,R 2. Advanced Vision Science C, R 3. Bausch & Lomb C 4. Carl Zeiss Inc C 5. Carl Zeiss Meditec C 6. Celgene Corporation C 7. Ista Pharmacuticals C, R 8. Gerson Lehman Group, Inc C 9. iTherapeutix, Inc. C 10. Vistakon C, R 11. Leerink Swann & Company C 12. Transcend Medical, Inc. C 13. Visiogen, Inc. C, R, O 14. Vision Care Inc. C 15. WaveTec Vision Systems C, R, O 16. Endo Optiks, Inc. L 17. TrueVision, Inc. C,O C = Consultant / Advisor R = Research Funding O = Equity Owner (Stock Options) L = Lecture Fees This case includes the discussion of off-label uses of FDA approved devices. Brief Author Biographies – please provide photos as well. Mark Packer, MD, FACS Dr. Packer grew up in Los Angeles and graduated cum laude from Harvard University, receiving both an Honorary National Scholarship and a Harvard Scholarship. He received his medical degree from the University of California at Davis and completed his residency training in Ophthalmology at Boston University Medical Center; he achieved American Board of Ophthalmology Certification in 1997. He currently serves as Clinical Associate Professor of Ophthalmology at Oregon Health & Science University. Dr. Packer focuses on refractive surgery and intraocular lens technology. He serves as Principal Investigator for the Carl Zeiss Meditec MEL-80 Excimer Laser, and was Coordinating Investigator for the US FDA monitored study of the aspheric Tecnis Intraocular Lens. He is Medical Monitor for the investigation of the AMO Tecnis Multifocal Intraocular Lens, and serves as Principal Investigator for the Visiogen Synchrony Dual Optic Accommodative Lens. He has also participated in FDA monitored studies of the Eyeonics accommodative Crystalens, VisionCare’s Implantable Miniaturized Telescope and Rayner’s C-flex IOL. Dr. Packer works extensively with leaders in the ophthalmic industry on the development of new technology for cataract and refractive surgery. He is a consultant to Advanced Medical Optics, Bausch & Lomb, Advanced Vision Science and WaveTec Vision Systems. Dr. Packer’s recent peer-reviewed publications include “Immersion A Scan Compared to Partial Coherence Interferometry,” “The Physics of Phaco: A Review,” and “Intraocular Lens Power Calculation Following Incisional or Thermal Keratorefractive Surgery,” appearing in The Journal of Cataract and Refractive Surgery; “Initial Clinical Experience with an Anterior Surface Modified Prolate Intraocular Lens” appeared in the Journal of Refractive Surgery. He authored “Wavefront Technology in Cataract Surgery” in Current Opinion in Ophthalmology and edited the textbook Refractive Lens Surgery published by Springer. He also served as editor for the “Functional Vision” issue of International Ophthalmology Clinics and has edited the annual Cataract and IOL issue of Current Opinion in Ophthalmology since 2005. Dr. Packer has delivered hundreds of presentations at scientific meetings around the world and demonstrated cataract surgery on four continents. He serves on the Cataract Clinical Committee of the American Society of Cataract and Refractive Surgery (ASCRS) and represents ASCRS on the Council of the American Academy of Ophthalmology. He also chairs the Cataract Subcommittee of the American Academy of Ophthalmology Annual Meeting Program Committee. In 2005 he was elected to membership in The International Intra-Ocular Implant Club and named one of 50 Top Opinion Leaders by Cataract & Refractive Surgery Today. I. History (Slide 5) A 48 year old woman presented for a Refractive Screening. She stated that she likes to garden & quilt, and doesn’t want to wear bifocals or contact lenses. II. Examination Her refraction, best-corrected visual acuity, central corneal pachymetry, axial length and keratometry are shown below. The remainder of the exam was remarkable only for complete posterior vitreous detachment OU. -8.50 + 2.50 X 108 Pach 521 AL 26.66 43.04 X 44.88 @ 85 20/30 OD -7.00 + 1.25 X 90 Pach 534 AL 26.35 43.60 X 45.24 @ 67 20/20 OS III. Refractive Options (Slides 6 – 13) The refractive options for this woman with moderate to high myopia, astigmatism, presbyopia OU and mild refractive amblyopia OD included LASIK, phakic refractive lenses and refractive lens exchange with an accommodative or multifocal IOL. The primary limitation of LASIK would be continued worsening presbyopia or decreased stereopsis due to monovision; implantation of ICLs did not offer any significant advantages over LASIK. Refractive lens exchange combined with limbal relaxing incisions offered the potential to treat the myopia, astigmatism and presbyopia. The data from FDA clinical investigations of the various IOLs were discussed with the patient, including the percentage of spectacle independence and the potential for dysphotopsia. Additionally the possibility of an enhancement procedure (LASIK or piggyback IOL) to correct residual refractive error was discussed. The chance of her needing an enhancement was described by a review of data from our practice (11 & 12). The risks of refractive surgery in general and refractive lens exchange in particular were thoroughly discussed, with particular attention to the risk of retinal detachment following lens surgery in high myopia. In this case the patient already had bilateral PVDs; a careful peripheral fundus exam demonstrated the absence of any predisposing lesions. IV. Surgical Decision and Early Postoperative Course (Slides 14 – 22) Given the patient’s desire to be free of glasses and contacts for quilting and gardening, which are intermediate range visual activities, we selected the crystalens. Her corneal topography demonstrated significant astigmatism which required correction with limbal relaxing incisions. These were cut to 90% depth at the 10mm zone based on the Nichamin nomogram. The surgery was uncomplicated and her immediate postoperative course was unremarkable; however, she developed regression of her astigmatism by 2 weeks. The probable need for a LASIK enhancement following refractive stability was discussed. V. Postoperative Course and Complication Management (Slides 23 – 41) At the six week post op visit the best-corrected acuity had declined and slit lamp examination revealed anterior capsular phimosis with a thickened, fibrotic rim of capsule within the pupil. Anterior chamber optical coherence tomography demonstrated the phimotic ridge in both eyes. The YAG laser was used to gently dissect and lyse the tissue. Subsequent slit lamp exam showed complete resolution of the phimosis. AC OCT demonstrated a shift in the IOL position in both eyes (but in opposite directions) and refraction demonstrated the expected changes due to these shifts. The best-corrected acuity returned to normal. Once the refraction stabilized LASIK was performed to correct the residual astigmatism. VI. Final Postoperative Course and Discussion (Slides 42 – 47) Following LASIK the uncorrected distance acuity stabilized at 20/25 OD and 20/20 OS. The patient was happy that she could garden and quilt without correction, as she had desired. She did need reading glasses, however. The regression of her astigmatism was likely related to her relatively thick corneas. The capsular phimosis was effectively treated with YAG photolysis. LASIK provided a spectacular solution for her residual refractive error. VII. Remediation Treatment Paths Had the patient chosen LASIK in the first place she would have had continued progression of her presbyopia but avoided additional surgical procedures If she had chosen multifocal IOLs she might have achieved better uncorrected near visual acuity, but she would have likely experienced some level of dysphotopsia. In the case, she did not at any time complain of unwanted visual phenomena other than blurred vision due to the capsular phimosis. Dysphotopsia related to multifocal IOLs often improves over time. Treatments include the use of brimonidine to limit mydriasis and low minus spectacles for night driving. IX. References Packer M, Fine IH, Hoffman RS. “Refractive Lens Exchange With the Array Multifocal Lens.” J Cataract Refract Surg. 2002; 28:421-424. Hoffman RS, Fine IH, Packer M. "Refractive lens exchange with a multifocal IOL." Current Opinion in Ophthalmology 2003;14:24-30. Cumming JS, Colvard DM, Dell SJ, Doane J, Fine IH, Hoffman RS, Packer M, Slade SG. Clinical evaluation of the Crystalens AT-45 accommodating intraocular lens: Results of the U.S. Food and Drug Administration clinical trial. J Cataract Refract Surg May 2006; 32(5):812-825. Fine IH, Hoffman RS, Packer M. “Avoiding complications with refractive lens exchange.” Cataract and Refractive Surgery Today, July 2004; 4(7): 24-27. Hoffman RS, Fine IH, Packer M. Refractive lens exchange as a refractive surgery modality. Current Opinion in Ophthalmology 2004; 15: 22-28. Packer M. Editorial overview: the age of refractive lens surgery, in Packer M (editor). Cataract surgery and lens implantation, Current Opinion in Ophthalmology February 2005; 16 (1): 1. Fine IH, Hoffman RS, Packer M. The new challenge for cataract surgeons. Editorial review, Current Opinion in Ophthalmology February 2007; 18:1-3.