Pharmacy Department Justification to Conduct a Residency
advertisement
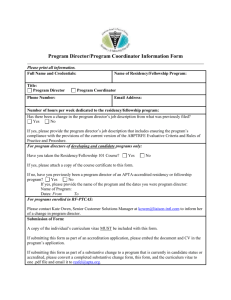
DEVELOPMENT OF A PHARMACY RESIDENCY PROGRAM: What is the value of a residency training program to your institution? Many authors have already documented multiple advantages and value of providing residency training to new pharmacy graduates. They include, and are not limited to: Positive impact on patient care, medication use safety, and quality within the institution Positive financial impact related to medication interventions and formulary review services Positive impact on departmental clinical practice and scope of services and expansion of services Positive impact on patient, departmental, interdisciplinary, and external (pharmacy student) education Positive impact on recruitment and retention Institutions should start the investigative process, by asking and answering several important questions including: Why should our pharmacy department start a residency training program? What will be the benefit to our department, our institution, and ultimately to our patients if we have a pharmacy resident or residents training with us? What opportunities are unique to our institution and what do we have to offer a potential resident training at our facility? What similarities do we have with other residency programs in our area? What kind of programs do other local residency programs offer and how long have they been in place and are they also accredited? Do we have a professional relationship with these institutions for some collegial advice in planning for a residency program at your site? Do we have the clinical and administrative talent in our department to support residency training? Should we partner with a college of pharmacy? Are we financially able to support the residency training program and how can we fund it with outside resources if necessary? Do we understand the value and need for ASHP accreditation of our program? This process may take 3-6 months or longer meeting regularly with an exploratory committee. Include your pharmacy director and one or two other pharmacy administrators or clinicians if possible. Preparation to turn your idea into reality requires the abilities of research and inspection of your pharmacy practice site and services, your staff, and the mission and goals of the department. Residency programs often support the mission, goals, and the vision for your pharmacy department. GETTING STARTED: THE BASICS ASHP Resources The following documents need to be thoroughly reviewed by members of the committee and all are located on the ASHP website link for “Residency and Technician Program Accreditation” located at www.ashp.org “How to Start a Residency Program, What You Really Need to Know” http://www.ashp.org/s_ashp/docs/files/RTP_HowStartResidencyPrgm.pdf The ASHP Accreditation Standard for Postgraduate Year One (PGY 1) Pharmacy Residency Programs http://www.ashp.org/s_ashp/docs/files/RTP_PGY1AccredStandard.pdf Or, if you feel your new program should be in a specialized area of practice, use The ASHP Accreditation Standard for Postgraduate Year Two (PGY 2) Pharmacy Residency Programs http://www.ashp.org/s_ashp/docs/files/RTP_PGY2AccredStandard.pdf If your practice site is located in a managed care or community setting, accreditation standards for these practice sites are also available for review on the website: Community Pharmacy Residency (PGY 1), prepared jointly by ASHP and American Pharmacists Association (APhA),Managed Care Pharmacy (PGY 1), prepared jointly by ASHP and The Academy of Managed Care Pharmacy (AMCP. Additionally APhA, AMCP, and the American College of Clinical Pharmacists (ACCP) have representation and are involved with the work of the ASHP accreditation Commission on Credentialing that recommends new standards, recommends lengths of accreditation and major changes in the accreditation process to ASHP. Required and elective educational outcomes, goals, objectives and instructional objectives for the residency programs are also posted on the website for each level of PGY 1 or PGY 2 residency program training. These statements need to be reviewed alongside the respective standard to understand the scope and magnitude of training that is expected by your preceptors. ASHP offers a new web based, on-line evaluation tracking system (ResiTrak™) for those residency programs in the accreditation process to help track their evaluations and completion of residency goals and objectives on-line. Finally, review the sections in the appropriate standard related to pharmacy practice at your site. Does the level of service described in the standard exist at your institution? THE BOTTOM LINE: “SHOW ME THE MONEY” Administrators in your institution will want three things from you when reviewing your proposal. They want a concise summary of why you should implement a residency program at your institution, the benefits of the program to the institution and pharmacy department, and the bottom line, how much will it cost? The summary of the residency program proposal and the list of benefits to the department and institution will be generated from the introspective analysis you have performed with the assistance of your committee. RESIDENCY PROGRAM COSTS Direct Costs Salary and Benefits Use your Human Resources Department to determine a stipend commensurate with other residency programs in your area. Consider doing a salary analysis of what local residents earn. What are the typical benefits that can be offered to this type of “short time” or “contract” employee? Determine a travel budget amount that the resident can be provided to be able to attend the ASHP Midyear Clinical Meeting and the regional residency conference. Consider conference registration fees as part of the overall amount. Other direct costs associated with the program include ASHP fees for accreditation (application fee and annual accreditation fee) and recruitment fees such as the annual Residency Showcase and CareerPharm’s Personal Placement Service (PPS) during the MCM to advertise and interview for your new program. The residency program director and perhaps several preceptors in addition to the residents will be required to attend these events and their costs should be taken into consideration. Indirect Costs Factor in the amount of time that preceptors and the residency program director will need to set aside from their daily functions to focus on teaching the resident and performing duties related to the administrative tasks of the residency program. This can be quite substantial in beginning a new program. FUNDING THE RESIDENCY PROGRAM Reimbursement may be available to institutions via CMS (Medicare Graduate Medical Education (GME) Pass-through Funding) for accredited PGY 1 pharmacy residency programs. A full review of this topic is also located on the website: http://www.ashp.org/s_ashp/cat1c.asp?CID=3567&DID=5667 Does your institution train medical residents and does it care for Medicare patients? You may be eligible for this funding for your PGY 1 residency program. Consult your finance office and human resources department. They may be aware of the process to file for this type of funding for the department. Pharmacy Pass-Through in Brief ( ) Reimbursement available to hospitals for share of certain expenses associated with accredited first year pharmacy residency programs Itemization and documentation of approved expenses required Reimbursement varies; approximately equivalent to percent of hospital’s Medicare patients Details available in Federal register sections 412, 413 What if your pharmacy department does not qualify for Medicare Graduate Medical Education Pass-through funding? Will you be able to incorporate one or more residents based on your current FTE budget? Should you consider converting unfilled pharmacist or tech positions to cover the salaries? If you are in the Veteran’s Administration you have different sources of funding offered for programs in the accreditation process. Some states or grants may also exist in your area to be considered for start up costs for a residency. Starting a residency is a major commitment for the long term of your organization. Evaluate all the critical decisions above when considering discussions with your administrator. Create your financial chart and set off on your new adventure. Literature Search and information adapted from ‘HOW TO START A RESIDENCY PROGRAM” Ross, Swanson, Bott, 1995 Update, Nelson 2005 “Developing an Approved Residency Program” Janet Teeters, presentation VHA Leadership Conference 2006 Funding of pharmacy residency programs 1996, AJHP Vol 55 Aug 1 1998, p.1618-1619 Annecchini and Letendre Understanding reimbursement for pharmacy residents, AJHP vol 55 Aug 1 1998, p. 1620-1623, Miller and Woller Justifying pharmacy staffing by presenting pharmacists as investments through return on investment analysis, AJHP vol 56 Nov 1, p. 2230-2234, McDaniel and DeJong Pharmacy residency training in the future: a stakeholder’s roundtable discussion, AJHP vol 62 Sep 1 2005, ASHP report 2003 ASHP Leadership Conference on Pharmacy Practice management executive summary, Looking to the future: leading and managing change, AJHP Vol 61 May 15 2004, ASHP report Advisory Board documents: HR Investment Center interviews and analysis. PG 77 University of Utah University Health Care PowerPoint presentation C:\Documents and Settings\jteeters\My Documents\Starting a Residency\Pharmacy Department Justification Strategy to Conduct a Residency Training Program Ver 4.doc