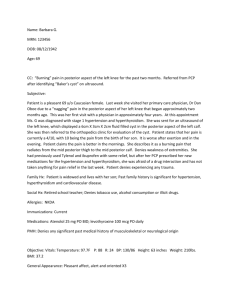
Consult 2
advertisement

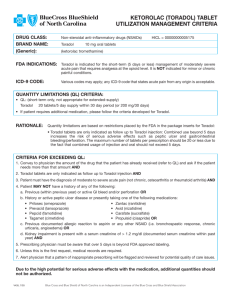
EXAMPLE Nimisha Shah, M.D. CONSULTATION ________________________________ REFERRING PHYSICIAN: Barry Tuch, M.D. (cc to this physician) CONSULTANT: Nimisha Shah, M.D. REASON FOR CONSULTATION: Postoperative medical management. complaints nausea, vomiting, hiccups, and knee pain. Chief HISTORY OF PRESENT ILLNESS: The patient is an 83-year-old elderly male, known case of hypertension, hyperlipidemia, myocardial infarction, status post angioplasty who underwent left total knee replacement on 04/05/06 for advanced left knee osteoarthritis. He tolerated the procedure well. Yesterday, he was noted to have 3 to 4 episodes of vomiting followed by nausea, which has resolved, but now complains of persistent hiccups for the last few hours. He denies any abdominal pain. There is no history of chest pain or shortness of breath. He has been receiving IV Toradol, oral Norco, and morphine p.r.n. for postoperative pain control. He denies any constipation or abdominal pain. PAST 1. 2. 3. MEDICAL HISTORY: Hypertension. Hyperlipidemia. MI status post angioplasty 2003 and follows up with a cardiologist. SURGICAL HISTORY: Appendectomy, tonsillectomy, left knee cruciate ligament repair, left total knee replacement postoperative day #2 as above. HOME MEDICATIONS: Aspirin, nifedipine, isosorbide, niacin, Lipitor, folic acid. CURRENT HOSPITAL MEDICATIONS: Subcutaneous Lovenox, Colace, Toradol, Norco, Lipitor, Imdur, nifedipine capsule, IV fluids D-5 0.5 normal saline, morphine p.r.n. ALLERGIES: No know drug allergies. SOCIAL HISTORY: He is married and retired. Currently a resident of Morgan Hill. Denies smoking, alcohol or other substance abuse. FAMILY HISTORY: Positive for diabetes. PHYSICAL EXAMINATION: VITALS: T-max 96.5, pulse 74, respirations 20, blood pressure 106/57, O2 saturation 94%. GENERAL: The patient is an 83-year-old elderly male lying on bed with left knee in brace. Noted to have continued hiccups but no other acute major distress. HEENT: Atraumatic, normocephalic, normal sinus mucosa. EYES: Pupils equal, reactive to light and accommodation. Extraocular movements intact. NECK: Supple, no thyroid swelling, no JVD. CHEST: Air entry equal on both sides, no wheezing or crackles heard. CARDIOVASCULAR: S1-S2 regular, no gallop or murmur heard. ABDOMEN: Bowel sounds present, soft, nontender, no organomegaly. CENTRAL NERVOUS SYSTEM: Awake, alert, oriented times three, no obvious focal neurologic deficit noted. EXTREMITIES: Left lower extremity in brace noted. Distal neurovascular intact. Peripheral pulses well heard. Cyanosis or clubbing absent. PERTINENT LABORATORY FINDINGS: Sodium 138, potassium 3.6, chloride 103, CO2 31, BUN 17, creatinine 1. Random blood sugar 118. WBC 12.3, hemoglobin 10.8, hematocrit 32, platelets 141. EKG: Normal sinus rhythm. No acute ST-T changes noted. ASSESSMENT: The patient is an 83-year-old male with a history of advanced left knee osteoarthritis status post left total knee replacement postoperative day #2, experiencing persistent hiccups and symptoms of gastritis, which is more likely secondary to current analgesics. He is also noted to have postoperative mild iron deficiency anemia. He has a history of coronary artery disease and hypertension which is well controlled currently with his routine home medications. RECOMMENDATIONS: I agree with IV hydration and will add oral proton pump inhibitor along with IV Reglan as needed for hiccups, nausea, and vomiting. I also agree with resuming his routine home medications and hold anti-hypertensives for systolic blood pressure less than 100. To monitor hemoglobin and hematocrit closely and repeat CBC in a.m. and will continue his other current hospital medications. Dr. Tuch, I appreciate the opportunity to participate in the care of this patient postoperatively, and I will be happy to answer any questions regarding his condition and management.