Management of pressure area care 2mb
advertisement
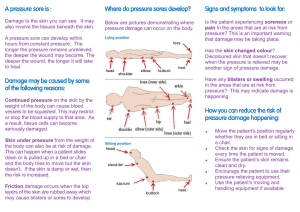
Practice No. 139 Reference: 10/06 Version 3 Page 1 of 8 New Practice note February 2008 NMC Code of Professional Conduct GSCC Code of Practice for Social Care Workers Marsden Manual pf Clinical Nursing Procedures Management of Pressure Area Care The ethos of care within Hampshire County Council Residential, Nursing and Day Care Services, holds the safeguarding of the well being and independence of the service user as a primary purpose of care. This summarises the arrangements for maintaining the well being and independence of vulnerable residents and other service users by managing the care of ‘pressure’ areas within the multi-disciplinary team. Whilst elderly and disabled persons may be more vulnerable to developing pressure injuries, these are generally preventable. Treating a pressure sore is far more difficult than preventing one. The aim of pressure care is to identify factors that predispose to the compromise of the tissue viability of an individual, and to eliminate or minimise those factors. A pressure sore is caused by unrelieved pressure on the skin, by friction or by ‘tearing/shearing’ forces. Pressure, the single most important factor in the development of sores, occurs mainly when the individual remains unmoved for inappropriate periods or exerts repeated pressure in one area, such as when using poorly adjusted mobility aids. It mainly affects the skin. Friction and ‘tearing’ forces are created by repetitive movement, such as sliding down in the bed or the use of poor moving and handling techniques, and causes damage to and distortion of the underlying tissue. Almost half of all pressure sores develop over the sacrum and about a fifth on the heels. Other areas at significant risk of damage are the buttocks and the hips. Whilst an individual may not complain of discomfort, this does not necessarily indicate s/he is not at risk, but may be the result of a lack of sensation or awareness which increases the risk of developing pressure sores. Factors which increase the vulnerability of a service user may include : Reduced mobility preventing normal adjustments to posture and position. Incontinence which can lead to skin damage and infection and will need to be managed alongside pressure area care. Poor nutrition and / or hydration, affecting normal repair and replacement of skin. Chronic ill health causing poor circulation, poor nutrition and damage to the skin. Incorrect moving and handling techniques. Medication such as steroids which have the effect of decreasing the thickness of the skin. Pain and stress which also compromise tissue viability and may be particularly relevant to new residents and those recently hospitalised. 1. 2. Care of potential pressure problems The Registered manager will ensure that staff are trained in the identification and care of pressure areas and the correct use of the assessment tools and specialist equipment. (Copies of the Braden assessment and wound care plan and pressure care checklist are attached at the end of this document.) The Registered manager may also delegate responsibility for tissue viability care to a designated member of the management team. Care of existing or developing pressure sores Before Admission The pre admission assessment should determine the presence of existing or potential sores and how they are being treated. On Admission or on development of a sore At all times it is necessary to obtain the consent of the service user to assessment and treatment, to keep them, their advocate/family and all other relevant persons, informed of progress and changes and to record all discussions and actions in the service user’s personal file. Where this is not possible all staff must comply with the requirements of the Mental Capacity Act 2005. All decisions must be made in the best interests of the service user. A Body Map should be completed to show the following :o The position and size of the sore – this can be indicated on paper, but is best supported by a photograph of the sore which should include a verifiable measuring scale. i.e. ruler o The depth and severity of the sore o The condition of the surrounding tissue o If there is any exudate and of what type A Risk Assessment must be made, using the Braden Scale for Predicting Pressure Sore Risk. This tool is the most appropriate for use with older persons and will inform decision making on the most appropriate action to be taken to protect tissue viability. Staff should be aware that should they need to refer to the PCT specialist, it may also be necessary to provide a Waterlow score. The Service User’s G.P. must be informed to enable a review of health and medication. A swab should be taken for analysis to determine the existence of any infection. An incident report must be completed, under ‘clinical incident’, upon admission or as soon as the sore is detected, and the report copied to the nurse advisor for attention. 3. In residential care without nursing cover, it will be necessary to seek the specialist advice of the PCT Tissue Viability Nurse. In Day Care, it will be necessary to refer the situation to the Care Manager for specialist advice, whilst ensuring that tissue viability is protected during day care activities. Occupational Therapy assessment will be part of the multi disciplinary assessment, to identify the most suitable type of equipment to address the specific needs of the service user. Use of specialist equipment Residential Care For service users in residential care, the District Nurse assigned to the service user will arrange the ordering of pressure relieving mattresses and cushions. Nursing Care For service users in nursing care, pressure relieving mattresses and cushions can be requested from the Joint Equipment Store. An order form can be found online and requests emailed. Day Care For service users in Day Care, equipment should accompany the service user following assessment arranged by the designated Care Manager. 4. Care Planning All assessments, multi disciplinary decisions and actions to be taken must be recorded in the service user’s personal file. Care planning should be holistic and address all areas of the service user’s daily living activities. Care plans must include wound care planning with regular monitoring and review of pressure areas and sores. Use of specialist equipment should be monitored for effectiveness and the need for re-assessment. The Care plan should be reviewed in all areas on a regular agreed basis or as necessary as needs change. AT RISK (15-18)* MANAGE MOISTURE FREQUENT TURNING MAXIMAL REMOBILIZATION PROTECT HEELS MANAGE MOISTURE, NUTRITION AND FRICTION AND SHEAR PRESSURE-REDUCTION SUPPORT SURFACE IF BED- OR CHAIR-BOUND * If other major risk factors are present (advanced age, fever, poor dietary intake of protein, diastolic pressure below 60, haemodynamic instability) advance to next level of risk USE COMMERCIAL MOISTURE BARRIER USE ABSORBENT PADS OR UNDERWEAR THAT WICK & HOLD MOISTURE ADDRESS CAUSE IF POSSIBLE OFFER BEDPAN/URINAL AND GLASS OF WATER IN CONJUNCTION WITH TURNING SCHEDULES MODERATE RISK (13-14)* MANAGE NUTRITION TURNING SCHEDULE USE FOAM WEDGES FOR 30E LATERAL POSITIONING PRESSURE-REDUCTION SUPPORT SURFACE MAXIMAL REMOBILIZATION PROTECT HEELS MANAGE MOISTURE, NUTRITION AND FRICTION AND SHEAR * If other major risk factors present, advance to next level of risk INCREASE PROTEIN INTAKE INCREASE CALORIE INTAKE TO SPARE PROTEINS. SUPPLEMENT WITH MULTI-VITAMIN (SHOULD HAVE VIT A, C & E) ACT QUICKLY TO ALLEVIATE DEFICITS CONSULT DIETICIAN HIGH RISK (10-12) MANAGE FRICTION & SHEAR INCREASE FREQUENCY OF TURNING SUPPLEMENT WITH SMALL SHIFTS PRESSURE REDUCTION SUPPORT SURFACE USE FOAM WEDGES FOR 30E LATERAL POSITIONING MAXIMAL REMOBILIZATION PROTECT HEELS MANAGE MOISTURE, NUTRITION AND FRICTION AND SHEAR ELEVATE HOB NO MORE THAN 30E USE TRAPEZE WHEN INDICATED USE LIFT SHEET TO MOVE PATIENT PROTECT ELBOWS & HEELS IF BEING EXPOSED TO FRICTION VERY HIGH RISK (9 or below) OTHER GENERAL CARE ISSUES ALL OF THE ABOVE + USE PRESSURE-RELIEVING SURFACE IF PATIENT HAS INTRACTABLE PAIN OR SEVERE PAIN EXACERBATED BY TURNING OR ADDITIONAL RISK FACTORS *low air loss beds do not substitute for turning schedules NO MASSAGE OF REDDENED BONY PROMINENCES NO DOUGHNUT TYPE DEVICES MAINTAIN GOOD HYDRATION AVOID DRYING THE SKIN Assessment of skin condition when re-positioning a Service User Consider all pressure areas Including hands and elbows knees and heels Is there any redness of the skin ? Is the skin broken ? Yes Ensure the skin is clean using plain warm water and patting dry, re-position the service user and re-assess the pressure area in 30 minutes. Ensure that any pressure relieving equipment is functioning correctly. No Ensure the skin is clean using plain warm water and patting dry and re-position the service user. Consider if the time between repositioning can be extended. On re-assessment, is the skin still red ? Yes Check that any pressure relieving equipment is functioning correctly Reduce the time interval between repositioning Ensure the skin is clean and dry as before No Resume re-positioning at the time intervals indicated in the care plan. TISSUE VIABILITY CARE PLAN RESIDENT NAME NAMED NURSE PROBLEM NO. WOUND ASSESSMENT DIAGRAM Body Maps on reverse indicate Site of wounds Wound depth (cm) cm AIM DRESSING RATIONALE ALLERGIES PLAN Cleansing Agent Primary Care Skin Care Secondary Dressing Frequency of dressing Change If wound has not healed within 6 weeks, re-assess. Consider referral to district nurse or tissue viability nurse and record actions.