Telehealth in Tissue Viability Excellence for every patient every time
advertisement
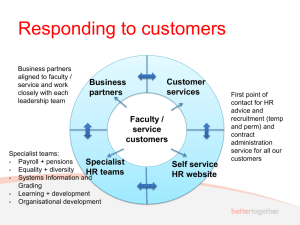
Telehealth in Tissue Viability Excellence for every patient every time Professor David Gray Department of Tissue Viability ,NHS Grampian Tissue Viability Practice Development Unit, Birmingham City University I have seen that in any great undertaking it is not enough for a man to depend simply upon himself Isna la-wica Teton Sioux Early discharge/ preventing re admission Early discharge/ preventing re admission Joined Up Working Non specialists delivering specialist treatments remotely Cross Referal Acute Hospital Patient admitted or develops pressure ulcer post admission Referral made via form sent via NHS Mail. Images from Medical Illustration Call to mobile to alert Specialist Option 2 Ward called by Specialist Option 1 Referral made to relevant specialist Images referral discussed with ward Verbal feedback provided Written treatment plan and review date emailed back to 3 members of ward team Reviewed in person or via Telehealth on set date Update images via Medical Illustration Acute Hospital Service Lessons Learned • Software a powerful tool for the users • Self explanatory , easy to use • Safe and Effective But • Barrier to wider usage/access • Not integrated Way Forward Interim • NHS Mail • Proforma • Standardized images • Teleconference Medium Term • SCI Store • Paperless tissue vaibility Conclusion • Technology is being used as an aide to delivery of care • It has the potential to be a barrier to involvement • Keeping it as simple as possible provides the grates chance of success Patient has or develops wound Reviewed by DN/PN/GP/Care Home Apply Wound Management Pathway Devise Treatment Plan Set Objectives Obs not met Refer to Tissue Viability via E Clinic Direct Referal to Vascular Timeline Apply Wound Bundle Appointment at Regional Tissue Viability Clinic Follow up at Regional Tissue Viability Clinic Treatment plan and review via E Clinic Discuss with Specialist direclty e.g Dermatology or Chronic Oedema