Rheumatic Diseases Clinics of North America - Volume 25, Issue 2 (May 1999) Copyright © 1999 W. B. Saunders Company
315
Osteoarthritis
VITAMINS AND ARTHRITIS
The Roles of Vitamins A, C, D, and E
MaryFran Sowers PhD
Laurie Lachance MPH
This work was supported by the following grants: NIH R01-AR41837-01; NIH 1UO1 NR04061; NIH P60AR-20557; and Public Health and Aging Training Grant, NIA T32AG00134.
Department of Epidemiology, University of Michigan, Ann Arbor, Michigan
Address reprint requests to
MaryFran Sowers, PhD
The University of Michigan
Department of Epidemiology
Room 3073 SPH I
109 South Observatory
Ann Arbor, MI 48109-2029
Interactions between all of the major joint tissues, including articular cartilage,
synovium, and subchondral bone, have been implicated in the pathogenesis of
osteoarthritis (OA). [24] [53] [69] The pathogenetic mechanisms underlying the
development of OA are not fully understood; likewise, those factors that sustain or
impede the progression of OA are poorly identified. Nevertheless, patients
frequently have sought explanations for the development and progression of OA in
dietary practices and nutritional deficiencies from either their health care provider
or popular media. Enticing promises have been offered over the decades for
inexpensive nutritional supplements that will end the individual's misery. Currently,
there is much attention directed toward the use of antioxidant vitamins, and of
vitamin D, as a means of preventing or ameliorating the pain and disability of OA.
This attention is driven, in part, by our expanding appreciation of nutrition factors,
particularly the vitamins, that contribute to oxidate processes and bone turnover
that may be intrinsic to the development and progression of OA.
Vitamins A, C, and, E are the major antioxidants in the diet or in dietary
supplement products that have been identified as having a potential for antioxidant
activity in the processes associated with OA. Vitamin D also may play an important
role in OA by way of bone.
316
mineralization and cell differentiation--roles that parallel the actions of vitamin A
and vitamin C.
There are at least four possible pathways in which these nutrients can influence OA:
protection against oxidative damage; modulation of the inflammatory response;
cellular differentiation; and biologic actions related to bone and collagen synthesis.
This article briefly discusses these vitamins and pathways using research derived
from animal models, tissue cultures, clinical studies, and epidemiologic studies.
Protection Against Oxidative Damage
Oxygen radicals have been identified as potent agents in the destruction of cartilage and
connective tissue. [8] [43] [68] Multiple roles have been suggested. There is evidence that cells
within joints produce reactive oxygen species (ROS) and that the attendant oxidative
damage is physiologically important in OA. [42] [54] For example, ROS have been shown to
cause depolymerization of hyaluronic acid, [45] [64] and degradation of proteoglycans and
type II collagen. [20] [26] [33] This seems to occur by direct action and, indirectly, by activation
of latent collagenase. [17] [34] [43] [44] An increase in levels of proteolytic enzyme in the
synovial fluid has been observed, [3] [4] [14] and is thought to be, at least in part, because of
damage of the chondrocyte membrane [20] [45] by oxidative species. [20] [22] [47] [56]
The roles of nutrients in the OA processes are complex because of the interactive system
in which they operate. For example, reactive oxygen species are produced endogenously
in normal metabolism, and exogenously as a consequence of toxins, infection, injury,
radiation, and excessive exercise. [38] Although mechanisms exist within the body to
protect tissues from excessive oxidative action, production of ROS can overwhelm those
modulating factors. In those instances in which anabolic and catabolic activities become
unbalanced, tissue damage can result, especially in extracellular spaces where antioxidant
enzymes are not as prevalent.
When free radicals attack polyunsaturated fatty acids (PUFA) in membrane lipids, they
create lipid peroxides, which spontaneously decompose to form lipid radicals. PUFAs,
with their double bonds, are readily attacked by free radicals and oxidized to lipid
peroxides, which have the capacity to damage cells. The free radicals produced by lipid
peroxidation, peroxyl radicals, are capable of removing hydrogen from adjacent fatty acid
side chains, thereby propagating a chain reaction known as lipid peroxidation. A single
initiating event can lead to hundreds of such events (Fig. 1) . [38]
The production of free radicals also can be the consequence of tissue damage associated
with arthritis. [37] Oxidative stress is believed to contribute to the progression of arthritis
rather than the initiation of disease.
317
Figure 1. Lipid peroxidation. ROS = reactive oxygen species; PUFA = polyunsaturated fatty acids; OA =
osteoarthritis.
Modulation of the Inflammatory Response
Reactive oxygen species are generated by, and are an integral part of, the immune
response. Antioxidants are important modulators of these responses and prevent
excessive damage to tissues and cells.
With injury and tissue damage, mast cells release inflammatory mediators that increase
vascular permeability and permit complement and cells to enter tissues from the
circulation. The mast cells also promote the activity of polymorphonuclear neutrophils
(PMNs). The activities of PMNs and mast cells create an acute inflammatory response
that leads to removal of damaged tissues and cells, tissue repair, and healing. Once
macrophages are engaged, there is a potential for further cell-mediated response
involving natural killer (NK) cells. These activities can lead to phagocytosis and chronic
inflammation.
Chondrocytes are normally surrounded by an extracellular matrix (ECM) and a repair
process is initiated when this matrix is removed. Degradation and loss of the articular
cartilage matrix is a central feature of OA. This loss of matrix is accompanied by an
increased synthesis of matrix molecules, a process thought to be involved in matrix
repair. [38] [39] [49]
In the presence of lipid peroxidation, arachidonic acid cascade products (i.e.,
prostaglandins, leukotrienes) release proinflammatory lipid peroxides that may cause
vascular leakage, chemotaxis, and adherence
318
of polymorphonuclear leukocytes. In turn, these may promote the generation of reactive
oxygen species and release of proteolytic enzymes that degrade collagen, proteoglycan,
and other components of the cartilage matrix. [19]
Cellular Differentiation
Vitamin A and vitamin D are now recognized as fundamental elements of cellular
maturation and cellular differentiation. Retinoic acid, an oxidized form of vitamin A,
regulates embryonic development and the differentiation of epithelial and mesenchymal
tissues throughout life. [67] Vitamin D has a role in the differentiation of keratocytes [23] [52]
and monocytes into macrophages. [1] [6] [41] Vitamin D also appears to act upon Tlymphocytes, which produce a variety of lymphokines, including the potent bone
resorbing agent, osteoclast activating factor. [40]
Additional Biologic Actions
Independent of their protective effect on ROS and modulation of the immune response,
these vitamins have well-described biologic roles related to OA. For example, vitamins A
and D have essential roles in bone development and maintenance of epithelial tissue, and
vitamin C has an essential role in the production of collagen.
Nutrients and Osteoarthritis
It is noteworthy that there are multiple mechanisms through which nutrients can have an
effect on either the initiation or progression of OA. For the most part, however, studies in
this area have been limited to laboratory investigations in tissue culture systems and
await extension into clinical or epidemiologic populations. On the other hand, the basic
research data on these nutrients (and their potential for ameliorating disease) have been
evoked inappropriately as scientific disguises for marketing strategies. Nonetheless, their
potential importance to OA reinforces the need for well-developed investigations in both
affected clinical and at-risk populations.
VITAMIN A AND THE CAROTENOIDS
Vitamin A occurs naturally in two forms: active, fat-soluble retinol, which is generally
derived from animal tissues; and a water-soluble precursor, provitamin A, also known as
beta-carotene, which is derived from plants and converted to retinol by the liver in
approximately a 3 to 1 ratio. Retinol circulates in the blood and is selectively absorbed by
cells as it is needed. Within the cells, retinol is converted to one of its two other active
forms: retinal or retinoic acid. The rate of conversion is dependent on the vitamin A and
protein status of the individual. The
319
Figure 2. Conversion of beta-carotene to retinol (vitamin A, aldehyde).
relative amounts of carotenoids directly absorbed and metabolized to vitamin A in the
intestine vary greatly (Fig. 2) . [11]
The Recommended Daily Allowance (RDA) for vitamin A is given in retinol equivalents
(RE) of active retinol (1 RE 1 mug 3.33 IU). One RE of beta-carotene is 6 mug
10 IU. The adult male RDA for vitamin A is 1000 RE per day and 800 RE per day for
an adult female. Vitamin A is found as retinol in foods such as liver, egg yolk, milk, and
other dairy products, whereas beta-carotene is found in dark green and yellow vegetables
and fruits. [11] [61]
Although vitamin A toxicity is not common, it can occur when excess amounts of
supplements or major dietary sources, such as liver, are consumed. beta-carotene, on the
other hand, is rarely considered toxic, but can accumulate, giving the skin an orangeyellow hue.
Role of Vitamin A and Carotenoids in Oxidative Stress
Recent studies have demonstrated the antioxidant functions of beta-carotene and
carotenoids, in general, and their effective ability to scavenge singlet oxygen. [11]
Carotenoids are known to scavenge and deactivate free radicals both in vitro and in vivo.
Evidence from in vitro experiments [10] [11] [28] [61] suggests that beta-carotene may exert other
antioxidant effects, including inhibition of lipid peroxidation. Whereas some antioxidants
prevent the initiation of lipid peroxidation, beta-carotene controls the chain reactions by
trapping free radicals, complementing the action of other antioxidant molecules.
320
Carotenoids have the capacity to modulate the enzymatic activities of lipoxygenases. [10]
Because the end products of lipoxygenase activity are proinflammatory and
immunomodulatory molecules, there can be many biologic consequences of regulation of
the activity of this enzyme by carotenoids. [28]
Another carotenoid, lycopene, is less abundant in the diet than beta-carotene. Like betacarotene, however, it is a singlet oxygen quencher and therefore can act also as an
antioxidant. Little data on this carotenoid are presently available. [27]
Vitamin A and the Immune Response
Depending upon the particular compound, dosage, and method of administration, [78]
vitamin A, its precursors, and synthetic derivatives can stimulate or inhibit various
aspects of the cellular and humoral immune response. [76]
beta-carotene has been shown to stimulate rat lymphocyte mitogenesis in vivo. [12] In vitro
studies of the actions of beta-carotene have demonstrated that it increases the numbers of
human NK cells and T-helper cells. [2] [77] Animal studies have shown that carotenoids
enhance immune function independent of any provitamin A effect. [9] [10] Carotenoids have
been shown to enhance macrophage function, [9] thereby modulating the production of
reactive oxygen species and controlling actions of other immune cells.
Using animal models, Pasatiempo et al [62] have shown that normal antibody function is
impaired in early stages of vitamin A deficiency. Bowman et al [16] have shown decreases
in NK cell activity and in interferon (IFN) production in the presence of vitamin A
deficiency.
Much of the research on the effects of carotenoids on human immune responses has been
limited to beta-carotene. Watson et al [77] reported that supplementation of healthy older
adults with 30 to 60 mg a day of beta-carotene for 2 months significantly enhanced the
percentage of leukocytes in peripheral blood with cell receptors indicative of NK cells
and of lymphocytes with interleukin-2 (IL-2) receptors. In that study, plasma levels of
beta-carotene, but not of retinol, were significantly elevated, suggesting that modulation
of the immune system may have been induced by carotenoid activity rather than by the
action of vitamin A. [77]
Vitamin A and Cell Differentiation
Vitamin A (as retinol or its activated metabolites) is now recognized as a fundamental
factor for growth and cell differentiation. Recent research has shown retinoic acid, an
oxidized form of vitamin A, is a key regulator of embryonic development and of the
differentiation of epithelial and mesenchymal tissues throughout life. [67]
321
Other Biologic Actions of Vitamin A
Vitamin A has essential roles in bone development, the development and maintenance of
epithelial tissue, normal reproduction, and vision. By virtue of its effect on protein
synthesis and bone cell differentiation, it is necessary for growth and development of
skeletal and soft tissues. Vitamin A also plays a role in maintaining normal epithelial
structures, including the differentiation of basal cells into mucous epithelial cells. [52]
Vitamin A and Osteoarthritis
Although there is great potential for a role of vitamin A in OA, there is virtually no
literature that has reported a protective association of dietary or supplemental retinol or
beta-carotene in relation to the initiation or progression of OA.
VITAMIN C (ASCORBIC ACID)
Vitamin C, the antiscorbutic vitamin, [52] is chemically the least complex of the vitamins.
Although plants and many mammals are able to synthesize ascorbic acid from glucose
and galactose, humans, monkeys, and guinea pigs do not synthesize vitamin C from
intrinsic sources. Ascorbic acid is easily absorbed from the small intestine into the blood
by an active mechanism and probably also by diffusion. Average absorption is 90% for
intakes between 20 to 120 mg; however, at very high intakes, such as 12 g, which are
often self-medicated, absorption is <20% (Fig. 3) .
The RDA of 60 mg for adults is based on the amount needed to prevent the onset of
scorbutic symptoms for 4 weeks and provide a margin of safety. An increased intake of
vitamin C is required to maintain normal plasma or cellular levels in the presence of
acute emotional or environmental stress, such as trauma, fever, infection, or elevated
environmental temperatures. Sources of dietary vitamin C include citrus fruits and juices,
such as oranges and grapefruit, potatoes, tomatoes, broccoli, red peppers, and cooked
collard and mustard greens.
Figure 3. Vitamin C (reduced and oxidized forms).
322
Role of Vitamin C in Oxidative Stress
In human plasma, ascorbate is the only endogenous antioxidant that can completely
protect the lipids from detectable peroxidation damage induced by aqueous peroxyl
radicals. [29] Ascorbate is thought to trap virtually all peroxyl radicals in the aqueous phase
before they can diffuse into the plasma lipids [29] ; however, once the ascorbate
antioxidative capacity has been expended, the remaining water-soluble antioxidants,
urate, bilirubin, and the protein thiols, can trap only part of the aqueous peroxyl radicals.
The peroxyl radicals that escape these remaining antioxidants in the aqueous phase
diffuse into the plasma lipids, where they initiate lipid peroxidation. Other antioxidants
are able to slow the rate at which lipid peroxidation occurs, whereas ascorbate can
prevent initiation of detectable lipid peroxidation by aqueous peroxyl radicals. [29] For this
reason, vitamin C has been referred to as the first line of defense [29] and has been
identified as a scavenger of several radicals. [35]
Ascorbate reacts rapidly with both superoxide and peroxyl radicals and even more rapidly
with hydroxyl radicals. [13] [21] It also scavenges singlet oxygen, reduces thiol radicals, and
combines rapidly with hypochlorous acid at sites of inflammation. Vitamin C is also
believed to have a role in sparing or recycling of alpha-tocopherol (vitamin E) [58] [73] and
has been shown to spare carotenoids [73] in vitro. It plays a vital role in maintaining the
balance between oxidative products and the various cellular antioxidant defense
mechanisms. The interdependency of such reactions involves ascorbic acid, vitamin E,
selenium, catalase, and glutathione. [19] It is known that ascorbate can switch from anti- to
pro-oxidant activity, depending on its concentration and the presence of free transition
metal ions [7] [50] [59] ; however, in plasma, transition metal ions are tightly bound and
unavailable for free radical reactions. [19] [35] [36] [37]
The antioxidant protection afforded by ascorbate does not correlate linearly with its
concentration in the presence of unrestricted intake. With increasing concentrations of
ascorbate, its efficiency for scavenging free radicals declines. Data from the work of Frei
et al [29] suggest that an increase in the RDA for ascorbate from the current 60 mg to
approximately 150 mg (to maximize the total body pool of ascorbate) would be beneficial
to human health.
Vitamin C and the Immune Response
Frei et al [30] have described plasma ascorbate as being outstandingly effective against the
oxidants released from activated polymorphonuclear leukocytes. Vitamin C may promote
resistance to infection by altering the immunologic activity of leukocytes, the production
of interferon, the inflammatory response, or the integrity of the mucous membranes. [21]
Ascorbate has been shown to have a major influence on phagocyte mobility and
chemotaxis. [21] Before particle ingestion, phagocytes exhibit a marked increase in
metabolic activity known as the respiratory burst. Oxygen consumption is greatly
increased and much of this extra oxygen
323
is converted to reactive oxygen metabolites. The ROS are released into the phagosome to
be used for killing phagocytosed microorganisms; however, ROS are also released to the
exterior of the cell, where they may damage adjacent normal tissue. [76]
Data from guinea pigs (which, like humans, do not synthesize vitamin C) have suggested
that vitamin C intake is a critical factor in the development of the immune response. [76]
These models confirm the role of vitamin C in phagocyte cell function and suggest
effects on cytokine production.
Subclinical ascorbate deficiency can be relatively common, even in affluent societies. [21]
[72] Physiologic stress may cause a sharp drop in ascorbate levels, and may occur partly as
a result of leukocyte migration to sites of tissue injury. [21] Increasing dosages of vitamin C
in human volunteers were found to increase neutrophil chemotaxis. [5] Vitamin C may act
at more that one level of the immune response, and at least some of these interactions
involve specific regulation of the cytokine network.
Vitamin C and Osteoarthritis
Vitamin C acts as an electron donor in the synthesis of type II collagen, a primary
structural component of cartilage. Vitamin C is involved in the hydroxylation of proline
to form hydroxyproline in the synthesis of collagen. [63] It also plays a part in
glycosaminoglycan synthesis through its role as a carrier of sulfate groups. [69] Depletion
of sulfated proteoglycans from the extracellular matrix of articular cartilage is one of the
earliest manifestations of OA. The higher levels of matrix-degrading enzymes that have
been shown to be present in the diseased tissue are thought to play a major role in this
loss. [69] Deficiency of vitamin C, therefore, could be related to the reduced mechanical
integrity of the extracellular matrix of articular cartilage and the increased matrix
turnover rate in OA. [13] [29]
Schwartz et al [70] studied the development of surgically induced OA in guinea pigs that
were given either high or low (but nonscorbutic) dietary levels of vitamin C. They
reported that guinea pigs maintained on high dietary levels of vitamin C developed lesssevere OA. The cartilage surfaces in the surgically modified joints showed less loss of
cartilage, less pitting and ulceration, and less eburnation in the animals receiving higher
dietary levels of vitamin C. In normal articular cartilage, ascorbate significantly increased
the biosynthesis of sulfated proteoglycans and inhibited the activity of acid phosphatase.
[71]
These properties of vitamin C presumably contributed to the increased formation and
stability of proteoglycans that successfully counteracted the erosion of cartilage during
development of OA in this animal model.
VITAMIN E (alpha-TOCOPHEROL)
Dietary vitamin E includes the tocopherols--alpha, beta, gamma, and delta--and the
tocotrienols, whose most important chemical characteristic is their
324
antioxidant property. Absorption of vitamin E is relatively inefficient, ranging between
20% and 80%. This vitamin is stored in liver and, to a large extent, in fatty tissues.
In food, vitamin E acts to prevent the peroxidation of PUFAs. It enhances the activity of
vitamin A by preventing its oxidation in the intestinal tract. At the cellular level, by
scavenging free radicals that contain oxygen, vitamin E seems to protect cellular and
subcellular membranes from damage. In the absence of vitamin E, free radicals catalyze
peroxidation of the PUFAs that constitute structural components of tissue membranes.
The requirement for vitamin E depends on the amount of PUFA consumed, which varies
widely among individuals. Seed oils, particularly wheat germ oil, are the richest source of
vitamin E, although lesser amounts occur in fruits, vegetables, and animal fats. Peanut,
olive, coconut, and fish oils are poor sources of the vitamin.
Vitamin E as an Antioxidant
Vitamin E is a fat-soluble vitamin with a highly flexible structure, facilitating its
antioxidant function. The hydrophobic terminal of the vitamin can attach in the lipid
bilayer of the cell membrane. The terminal with a hydroxylated aromatic ring can then be
located near the water-membrane interface, where it is available to donate an electron to
those atoms with unpaired orbits. [18] [60]
Vitamin E has several isomeric structures, but alpha-tocopherol is the isomer with the
greatest biologic activity. An electron from the hydroxyl group at the active site can be
transferred, converting alpha-tocopherol to its radical form, alpha-tocopheroxyl. Unlike
the radical forms of some molecules, the alpha-tocopheroxyl radical is very stable,
because of the nature of its ring structure. The propagation of excessive free radicals by
vitamin E is controlled by oxidizing alpha-tocopheroxyl to alpha-tocopheryl quinone or
by reducing it back to its alpha-tocopherol form in the presence of vitamin C (Fig. 4) . [18]
Vitamin E acts as an antioxidant by preventing lipid peroxidation from entering the
chaining process in the propagation phase. Like vitamin C, vitamin E is a sacrificial
antioxidant; its antioxidant capacity is therefore expended after it has scavenged a certain
number of radicals. [27] The effects of vitamin E and those of selenium, sulfur amino acids,
polyunsaturated fatty acids, and other antioxidants are interdependent. [57]
Figure 4. alpha-Tocopherol.
325
Vitamin E may be beneficial to the body's host defense mechanisms by preventing the
infection-induced increase in production of tissue prostaglandins from arachidonic acid.
Prostaglandin production requires an active oxygen species, and lipid peroxides can
stimulate synthesis by providing an oxygen species.
[57]
Goetzl [32] reported that vitamin E bidirectionally modulated the activity of the
lipoxygenase pathway of human neutrophils in vitro and that normal plasma
concentrations of vitamin E enhanced the lipoxygenation of arachidonic acid, whereas
higher concentrations exerted a suppressive effect, consistent with the role of alphatocopherol as a hydroperoxide scavenger. When endothelial cells are exposed to
oxidative stress, they synthesize more PGI2 , which may be a protective response against
injury. [15] Meydani et al [57] have shown that vitamin E supplementation in mice increases
lung PGI2 synthesis.
Vitamin E and the Immune Response
The mounting of an immune response requires membrane-bound, receptor-mediated
communication between cells and between protein and lipid mediators. This can be
directly or indirectly affected by tocopherol status, although the precise mechanism is not
known. [57] Previous work has shown that free radical and lipid peroxidation reactions play
a part in cellular damage. [79]
Evidence from animal models shows that vitamin E is protective against environmental
pollutants, decreases thrombosis, reduces the formation of certain carcinogens, and
enhances almost every aspect of the immune response. The resistance to infection,
specific antibody responses, splenic plaque-forming cells, in vitro mitogenic responses of
lymphocytes, reticuloendothelial system clearance, and phagocytosis all are altered by
vitamin E deficiency. Increases in tocopherol intake have a positive impact on these
processes. [57]
Studies in humans indicate that healthy individuals eating "normal" diets show a
significant decrease in markers of cell damage, such as lipid peroxidation and pentane
output, when they supplement their diets with vitamin E. [48] [75] These studies suggest that
the average diet may not provide adequate protection against free-radical damage.
Vitamin E and Osteoarthritis
There have been few studies of vitamin E activity in relation to OA. In a cross-over
study, 29 OA patients were randomly assigned to treatment with tocopherol, 600 mg a
day for 10 days, or to the placebo group.
326
Machtey et al [51] found that 52% of those receiving vitamin E experienced marked relief
of pain, as compared with only 1 patient (4%) in the placebo group.
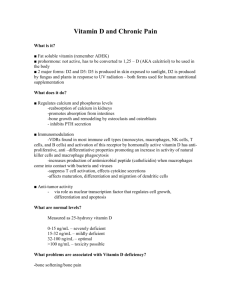
VITAMIN D
The precursors of vitamin D are present in sterol fractions of animal and plant tissues in
the form of 7-dehydrocholesterol and ergosterol, respectively. Both precursors require
ultraviolet irradiation for conversion to the provitamin form (D3 , cholecalciferol, and D2 )
and both provitamins require conversion in the kidney to the metabolically active form.
The plant form is of interest primarily as a food additive (Fig. 5) . [52]
The RDA for vitamin D is 10 mug (400 IU) for children beyond 6 months of age, young
adults up to 25 years of age, and pregnant and lactating women. For adults 25 years and
older, the RDA is 5 mug. The normal adult is presumed to obtain sufficient vitamin D
from exposure to sunlight and the incidental ingestion of small amounts in foods.
Because vitamin D is fat soluble, hypervitaminosis D can occur from excess consumption
of supplements, including fish oils. [52]
Figure 5. Structural formulae and conversion of provitamin D to vitamin D.
327
Vitamin D and Osteoarthritis
Relatively little is known of the direct actions of vitamin D and its metabolites in arthritis.
It is likely that vitamin D metabolites are concerned with normal cartilage integrity, [25] but
specific metabolic actions are not well defined.
It has been shown that cultured chondrocytes convert vitamin D to its active forms. [25] [31]
Fairney et al [25] found significant amounts of 25-OH-D and 24, 25-(OH)2 -D in samples of
synovial fluid from patients with OA and rheumatoid arthritis (RA). Serum levels of 25OH-D were, on average, twice as great as those in synovial fluid from the same patient.
The investigators suggested that the composition of synovial fluid is consistent with it
being a dialysate of plasma into which hyaluronan is secreted by the synovial membrane.
Therefore, the presence of vitamin D metabolites in synovial fluid may simply reflect the
serum values. In contrast, analyses of 24, 25-(OH)2 -D in samples of synovial fluid and
serum suggested local production of that metabolite in the synovium, rather than only
diffusion into the joint space from serum. No differences were noted between results of
assays of synovial fluid from patients with OA and those with RA.
Interest in vitamin D increased when, in 1996, the Framingham Study investigators
reported that a relative deficit of vitamin D, as determined by dietary intake and serum
levels, predisposes patients to OA of the knee. [55] They reported that persons with low
intake of dietary vitamin D (3-170 IU/day) and lower serum levels of vitamin D (4.9-24.0
ng/mL) were approximately three times more likely to exhibit progression of established
knee OA than those having higher intakes of dietary vitamin D (400-1600 IU) and higher
levels of serum vitamin D (36.0-79.0 ng/ml). They found no evidence, however, that
these lower dietary intakes and lower serum levels influenced the risk for development of
OA in a previously normal knee.
It is not surprising that vitamin D intakes or serum levels correlate with progression of
knee OA, because both are well-known phenomena correlated with the aging process. It
is surprising, however, that including measures of bone mineral density in statistical
models did not alter the association between vitamin D and OA, especially when the
investigators suggested that bone status was a potential mechanism through which
vitamin D might influence the progression of OA.
Defining whether investigators are describing the initiation or progression of OA is vital
to the interpretation of this association between vitamin D and OA. It has been observed
for a while now that individuals with OA are more likely to have greater bone mineral
density (BMD), and that they had that higher BMD before their presentation with
radiographically defined OA. Adequate vitamin D status, either as a result of dietary
intake or appropriate sunlight exposure, is typically a component of normal BMD, but
has not been described as a component of higher BMD. Thus, it is consistent that the
Framingham investigators [55] found no protection for vitamin D with the development of
incident OA.
328
This study, which has stimulated much interest from practitioners and patients, in truth
merely highlights the need to study the role of nutrition with a clear sense of the
multifactorial nature of OA and the multiple roles that a specific nutrient may have in
cellular physiology.
Vitamin D, the Immune Response, and Osteoarthritis
One possible explanation for the role vitamin D may have played in the progression of
OA among the Framingham study subjects lies in vitamin D's potential to contribute to
the immunologic response to inflammatory products. Progression of OA associated with
a chronic and insidious inflammatory state has not been investigated relative to vitamin
D, but studies from the other more inflammatory arthritides may be informative.
Peripheral blood lymphocytes and synovial fibroblasts from patients with rheumatoid
arthritis possess specific receptors for 1, 25-(OH)2 -D, although the role of the metabolite
in these cells is unknown. [41] Studies of the extrarenal metabolism of 25-(OH)-D show
that 1, 25-(OH)2 -D is synthesized in vitro by normal human macrophages activated with
interferon gamma [46] or bacterial lipopolysaccharides. [65] Hayes et al [41] have speculated
that activated macrophages in patients with arthritis synthesize 1, 25-(OH)2 -D within the
affected joints. These investigators examined synovial fluid samples from 45 patients
with knee effusions and showed that synovial fluid cells were capable of synthesizing the
active vitamin D metabolite 1, 25-(OH)2 -D and that activated macrophages appeared to
be responsible for much of the 1, 25(OH)2 -D synthesized. Although the significance of
the ability of macrophages from patients with inflammatory arthritis to synthesize 1, 25(OH)2 -D is not clear, Hayes et al [41] speculate that the importance may be greater when
the cells are present within the synovial membrane, and thus adjacent to the sites of tissue
damage and bone erosion within the joint, than when they are present in the synovial
fluid.
Overall, specific receptors for 1, 25-(OH)2 -D on normal human monocytes, activated
lymphocytes, and peripheral blood lymphocytes and synovial fibroblasts from patients
with rheumatoid arthritis [41] suggest a physiologic role for the metabolite in joint disease.
Many of the reported effects of 1, 25-(OH)2 -D may be relevant to OA. For example, it
appears to inhibit proliferation of B and T lymphocytes and to reduce interleukin-2
production by activated T lymphocytes in vitro. [74] Although synthesis of 24, 25-(OH)2 D
has been demonstrated in normal human macrophages [66] and in articular cartilage and
chondrocyte cultures, [31] Hayes et al did not find evidence of synthesis of 24, 25-(OH)2 D
in synovial fluid cells of the 45 patients with knee effusions described previously. [41]
Vitamin D, Cell Differentiation, Bone, and Immunologic Responsiveness
Vitamin D plays multiple roles that ultimately may have an effect in OA. The hormonal
form of vitamin D (1, 25-(OH)2 -D) inhibits collagen
329
synthesis by osteoblasts and promotes bone resorption. Hormonal vitamin D therefore
may contribute to OA status insofar as OA is determined by bone mineral density. In
addition, 1, 25-(OH)2 -D promotes differentiation of monocytes into macrophages and the
fusion of macrophages into multinucleated giant cells. These giant cells can have
multiple functions, including a humoral immunological response and stimulation of bone
resorbing activity by osteoclasts. [41] 1, 25-(OH)2 -D also acts upon T lymphocytes,
producing a variety of lymphokines, including the potent bone resorbing agent osteoclast
activating factor. [40] Within the synovial fluid and synovium 1, 25-(OH)2 -D thus may
have complex paracrine and immunoregulatory functions. [41] It is also important to note
that these roles are played by the hormonal form of vitamin D, a form that is only
indirectly associated with measures of dietary vitamin D intake, sunlight exposure, and
serum levels of 25-hydroxyvitamin D.
SUMMARY
There are at least four mechanisms whereby the nutrient vitamins A, C, D, and E may be
related to the processes that impede or give rise to OA. These nutrient vitamins have
major roles in modulating oxidative stress, participating in immune responses, and
contributing to cell differentiation. There is a substantial need to understand the
contribution of these nutrients to OA, because they may provide important insight into
ameliorating the initiation and progression of the disease. Simultaneously, greater
understanding will add rationality to an area of potential intervention that is often based
on anecdote.
Investigation will be complex; there is the need to select appropriate systems. Typical
animal model systems used in the study of OA are inappropriate because most animals
can synthesize ascorbic acid. There is the need to disaggregate, as much as possible, the
numerous subsets of OA and the plethora of processes that contribute to that
heterogeneity. Certainly, there is the need to recognize the interdependency of the actions
of each of these nutrients at the cellular level. Furthermore, humans rarely consume these
nutrients as independent products. For example, watermelon is a primary source of both
ascorbic acid and beta-carotene. Failure to address these complexities denies the scientist
the opportunity to advance our understanding of health and disease processes. More
importantly, failure to address these complexities denies the person with OA the
opportunity to address his or her own health.
References
1. Abe
E, Miyaura C, Tanaka H, et al: 1alpha,25-Dihydroxyvitamin D3 promotes fusion of mouse alveolar
macrophages both by direct mechanism and by spleen cell-mediated indirect mechanisms. Proc Natl Acad
Sci USA 80:5563, 1983 Abstract
2. Alexander
M, Newmark H, Miller G: Oral beta-carotene can increase the number of OKT4 positive cells
in human blood. Immunology 9:221, 1985
3.
330
Ali SY, Evans L: Enzymatic degradation of cartilage in osteoarthritis. Federation Proceedings 32:1494,
1973
4. Ali
SY, Evans L, Stainthorpe E, et al: Characterization of cathepsins in cartilage. Biochem J 105:549,
1967 Citation
5. Anderson
R, Dosthuizen R, Maritz R, et al: The effect of increasing weekly doses of ascorbate on certain
cellular and humoral immune functions in normal volunteers. Am J Clin Nutr 33:71, 1980 Abstract
6. Bar-Shavit
Z, Teitlebaum SL, Reitsma P, et al: Induction of monocytic differentiation and bone
resorption by 1, 25-Dihydroxyvitamin D3 . Proc Natl Acad Sci USA 80:5907, 1983 Abstract
7. Barber
AA, Bernheim F: Lipid peroxidation: Its measurement, occurrence, and significance in animal
tissues. Advances in Gerontology Research 2:355-403, 1967
8. Bates
EJ, Lowther DA, Handley CJ: Oxygen free-radicals mediate an inhibition of proteoglycan synthesis
in cultured articular cartilage. Ann Rheum Dis 43:462, 1984 Abstract
9. Bendich
A: Beta-carotene and the immune response. Proc Nutr Soc 50:263, 1991 Citation
10. Bendich
A: Biological functions of dietary carotenoids. Ann NY Acad Sci 691:61, 1993
11. Bendich
A, Olson JA: Biological actions of carotenoids. FASEB J 3:1927, 1989 Abstract
12. Bendich
A, Shapiro SS: Effects of beta-carotene and canthaxanthin on immune response of the rat. J
Nutr 116:2254, 1986 Abstract
13. Block
G, Menkes M: Ascorbic acid in cancer prevention. In Moon TE, Micozzi MS (eds): Nutrition and
Cancer Prevention: Investigating the Role of Micronutrients. New York, Marcel Dekker, 1989, p 341
14. Bollet
AJ, Bonner WM, Nance JL: The presence of hyaluronidase in various mammalian tissues. J Biol
Chem 238:3522, 1963
15. Boogaerts
MA, Van de Brock J, Deckmyn H, et al: Protective effect of vitamin E on immune triggered
granulocyte mediated endothelial injury. Thromb Haemost 51:89, 1984 Abstract
16. Bowman
TA, Goonewardene IM, Pasatiempo AM, et al: Vitamin A deficiency decreases natural killer
cell activity and interferon production in rats. J Nutr 120:1264, 1990 Abstract
17. Burkhardt
H, Schwingel M, Menninger H: Oxygen radicals as effectors of cartilage destruction. Arthritis
Rheum 29:379, 1986 Abstract
18. Burton
GW: Vitamin E: Antioxidant activity, biokinetics, and bioavailability. Ann Rev Nutr 10:357,
1990
19. Burton-Wurster
N, Butler M, Harter S, et al: Presence of fibronectin in articular cartilage in two animal
models of osteoarthritis. J Rheumatol 13:175, 1986 Abstract
20. Chrisman
OD, Ladenbauer-Bellis IM, Panjabi M: The relationship of mechanical trauma and the early
biochemical reactions of osteoarthritic cartilage. Clin Orthop 161:275, 1981
21. Cunningham-Rundles
WF, Berner Y, Cunningham-Rundles S: Interaction of vitamin C in lymphocyte
activation: Current status and possible mechanisms of action. In Cunningham-Rundles S (ed): Nutrient
Modulation of the Immune Response. New York, Marcel Dekker, 1993, p 91
22. Del
Maestro RF: An approach to free radicals in medicine and biology. Acta Physiol Scand 492:153,
1980
23. DeLuca
H: Vitamin D. Nutrition Today 28:6, 1993
24. Dendrick
DK, Goldstein SA, Brandt KD, et al: A longitudinal study of subchondral plate and trabecular
bone in cruciate-deficient dogs with osteoarthritis followed up for 54 months. Arthritis Rheum 36:1460,
1993 Abstract
25. Fairney
A, Straffen AM, May C, et al: Vitamin D metabolites in synovial fluid. Ann Rheum Dis 46:370,
1987 Abstract
26. Freeman
MAR: The pathogenesis of primary osteoarthrosis, an hypothesis. In Apley AG (ed): Modern
Trends in Orthopaedics, vol 6. London, Butterworths, 1972, p 40
27. Frei
B: Proceedings of a symposium: Health promotion and disease prevention: The role of antioxidant
vitamins. Discussion. Am J Med 97(suppl 3A):22S, 1994 Abstract
28. Frei
B: Reactive oxygen species and antioxidant vitamins: Mechanisms of action. Am J Med 97(suppl
3A):5S, 1994 Abstract
29. Frei
B, England L, Ames BN: Ascorbate is an outstanding antioxidant in human blood plasma. Proc Natl
Acad Sci USA 86:6377, 1989 Abstract
30.
331
Frei B, Stocker R, Ames BN: Antioxidant defenses and lipid peroxidation in human blood plasma. Proc
Natl Acad Sci USA 85:9748, 1988 Abstract
31. Garabedian
M, Lieberherr M, N'Guyen TM, et al: The in vitro production and activity of 24,25dihydroxycholecalciferol in cartilage and calvarium. Clin Orthop 135:241, 1978
32. Goetzl
EJ: Vitamin E modulates lipoxygenation of arachidonic acid in leukocytes. Nature 288:183, 1980
Abstract
33. Greenwald
RA: Degradation of cartilage proteoglycans and collagen by superoxide radical. Arthritis
Rheum 19:799, 1976
34. Greenwald
RA, Mox WW: Inhibition of collagen gelation by action of the superoxide radical. Arthritis
Rheum 22:251, 1979 Abstract
35. Halliwell
B: Antioxidants and human disease: A general introduction. Nutr Rev 55(Suppl):S44, 1997
Citation
36. Halliwell
B, Aruoma OI: DNA damage by oxygen-derived species: Its mechanism and measurement in
mammalian systems. FEBS Lett 281:9, 1991 Abstract
37. Halliwell
B, Gutteridge JM, Cross CE: Free radicals, antioxidants, and human disease: Where are we
now? J Lab Clin Med 119:598, 1992 Citation
38. Halliwell
B, Gutteridge JMC: Free Radicals in Biology and Medicine. Clarendon, Oxford, 1985
39. Hamerman
D: The biology of osteoarthritis. N Engl J Med 320:1322, 1989 Citation
40. Haussler
MR, Donaldson CA, Allegretto EA, et al: New actions of 1,25-Dihydroxyvitamin D3 : Possible
clues to the pathogenesis of postmenopausal osteoporosis. In Christiansen C, Arnaud CD, Nordin BEC, et
al (eds): Osteoporosis. Copenhagen International Symposium on Osteoporosis, June 3-8, 1984, pp 725-736
41. Hayes
ME, Denton J, Freemont AJ, et al: Synthesis of the active metabolite of vitamin D, 1,25(OH) 2 D3 ,
by synovial fluid macrophages in arthritic diseases. Ann Rheum Dis 48:723, 1989 Abstract
42. Henrotin
Y, Deby-Dupont G, Deby C: Active oxygen species, articular inflammation and cartilage
damage. EXS 62:308, 1992 Abstract
43. Henrotin
Y, Deby-Dupont G, Deby C, et al: Production of active oxygen species by isolated human
chondrocytes. Br J Rheum 32:562, 1993
44. Imlay
JA, Linn S: DNA damage and oxygen radical toxicity. Science 240:1302, 1988 Abstract
45. Kaiki
G, Tsuji H, Takanobu Y, et al: Osteoarthrosis induced by intra-articular hydrogen peroxide
injection and running load. J Orthop Res 8:731, 1990 Abstract
46. Koeffler
HP, Reichel H, Bishop JE, et al: Gamma-interferon stimulates production of 1,25dihydroxyvitamin D3 by normal human macrophages. Biochem Biophys Res Commun 127:596, 1985
Abstract
47. Leibovits
BE, Siegel BV: Aspects of free radical reactions in a biological system: Aging. Journal of
Gerontology 35:45, 1980
48. Lemoyne
M, Van Gossum A, Kurian R: Breath pentane analyses as an index of lipid peroxidation: A
functional test of vitamin E status. Am J Clin Nutr 46:267, 1987 Abstract
49. Loeser
RF, Carlson CS, McGee MP: Expression of beta1 integrins by cultured articular chondrocytes
and in osteoarthritic cartilage. Exp Cell Res 217:248, 1995 Abstract
50. Machlin
LJ, Bendich A: Free radical tissue damage: Protective role of antioxidant nutrients. FASEB
1:441, 1987
51. Machtey
I, Ouaknine L: Tocopherol in osteoarthritis: A controlled pilot study. J Am Geriatr Soc 26:328,
1978 Abstract
52. Mahan
LK, Escott-Stump S (eds): Krause's Food, Nutrition, and Diet Therapy, ed 9. Philadelphia, WB
Saunders, 1996, p 85
53. Mankin
HJ, Brandt KD: Pathogenesis of osteoarthritis. In Kelley WN, Harris ED Jr, Ruddy S, et al
(eds): Textbook of Rheumatology, ed 4. Philadelphia, WB Saunders, 1993
54. McAlindon
T, Felson DT: Nutrition: Risk factors for osteoarthritis. Ann Rheum Dis 56:397, 1997
Citation
55. McAlindon
TE, Felson DT, Zhang Y, et al: Relation of dietary intake and serum levels of vitamin D to
progression of osteoarthritis of the knee among particpiants in the Framingham study. Ann Intern Med
125:353, 1996 Abstract
56. McCord
JM: The superoxide free radical: Its biochemistry and pathophysiology. Surgery 94:412, 1983
Abstract
57. Meydani
SN, Blumberg JB: Vitamin E and the immune response. In Cunningham-Rundles
332
S (ed): Nutrient Modulation of the Immune Response. New York, Marcel Dekker, 1993, p 223
58. Niki
E, Saito T, Kawakami A, et al: Inhibition of oxidation of methyl linoleate in solution by vitamin E
and vitamin C. J Biol Chem 259:4177, 1984 Abstract
59. Niki
E, Yamamoto Y, Takahashi M, et al: Free radical-mediated damage of blood and its inhibition by
antioxidants. J Nutr Sci Vitaminol (Tokyo) 34:507, 1988 Citation
60. Packer
L: Protective role of vitamin E in biological systems. Am J Clin Nutr 53:1050S, 1991 Abstract
61. Parker
RS: Carotenoids in human blood and tissues. J Nutr 119:101, 1989 Abstract
62. Pasatiempo
AMG, Taylor CE, Ross AC: Vitamin A status and the immune response to pneumococcal
polysaccharide: Effects of age and early stages of retinol deficiency in rats. J Nutr 121:556, 1990
63. Peterkofsky
B: Ascorbate requirement for hydroxylation and secretion of procollagen: Relationship to
inhibition of collagen synthesis in scurvy. Am J Clin Nutr 54(suppl):1135S, 1991 Abstract
64. Puig-Parellada
P, Planas JM: Synovial fluid degradation induced by free radicals. Biochem Pharmacol
27:535, 1978 Citation
65. Reichel
H, Koeffler P, Bishop JE, et al: 25-Hydroxyvitamin D3 metabolism by lipopolysaccharidestimulated normal human macrophages. J Clin Endocrinol Metab 64:1, 1987 Abstract
66. Reichel
H, Koeffler HP, Norman AW: Synthesis in vitro of 1,25 by interferon-gamma-stimulated normal
human bone marrow and alveolar macrophages. J Biol Chem 262:10931, 1987 Abstract
67. Ross
CR: Vitamin A and protective immunity. Nutrition Today 27:18, 1992
68. Schalkwijk
J, Van Der Berg WB, Van De Putte LB, et al: Hydrogen peroxide suppresses the
proteoglycan synthesis of intact articular cartilage. J Rheumatol 12:205, 1985 Abstract
69. Schwartz
ER, Adamy L: Effects of ascorbic acid on arysulfatase activities and sulfated proteoglycan
metabolism in chondrocyte cultures. J Clin Invest 60:96, 1977 Abstract
70. Schwartz
ER, Leveille CR, Stevens JW, et al: Proteoglycan structure and metabolism in normal and
osteoarthritic cartilage of guinea pigs. Arthritis Rheum 24:1528, 1981 Abstract
71. Schwartz
ER, Oh WH, Leveille CR: Experimentally induced osteoarthritis in guinea pigs: Metabolic
responses in articular cartilage to developing pathology. Arthritis Rheum 24:1345, 1981 Abstract
72. Ten
State Nutrition Survey in the United States 1968-1970. US Center for Disease Control, US
Department of Health, Education and Welfare Publication No. (HSM) 72-8132, 1972
73. Thomas
WB, Holt PG: Vitamin C and immunity: An assessment of the evidence. Clin Exp Immunol
32:370, 1978 Abstract
74. Tsoukas
CD, Provvedini DM, Manolagas SC: 1,25-Dihydroxyvitamin D3 : A novel immunoregulatory
hormone. Science 224:1438, 1984 Abstract
75. Van
Gossum A, De Cuyper J, Ooms H, et al: Assessment of lipid peroxidation in humans by breath
pentane output measurement. Acta Gastroenterol Belg 55:245, 1992 Citation
76. Watson
RR, Earnest DL, Prabhala RH: Retinoids, carotenoids, macrophage activation. In CunninghamRundles S (ed): Nutrient Modulation of the Immune Response. New York, Marcel Dekker, 1993, p 63
77. Watson
RR, Prabhala RH, Plezia PM, et al: Effects of beta-carotene on lymphocyte subpopulation in
elderly humans: Evidence for a dose response relationship. Am J Clin Nutr 53:90, 1991 Abstract
78. Watson
RR, Rybski J: Immunomodulation by retinoids and carotenoids. In Chandra RK (ed): Nutrition
and Immunology. New York, Wiley-Liss, 1988, p 87
79. Yoshikawa
T, Tanaka H, Kondo M: Effect of vitamin E on adjuvant arthritis in rats. Biochemical
Medicine 29:227, 1983
Email to Colleague Print Version
Copyright © 2008 Elsevier Inc. All rights reserved. - www.mdconsult.com
Bookmark URL: /das/journal/view/0/N/10752987?ja=145634&PAGE=1.html&issn=0889-857X&source=