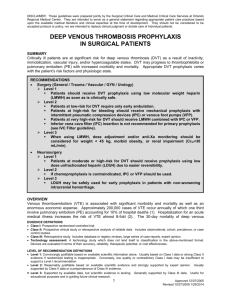
DVT Prophylaxis - Society of Trauma Nurses
advertisement
CHILDREN’S HOSPITAL OF WISCONSIN Guidelines for DVT Prophylaxis in Trauma Patients DVT prophylaxis – Page 1 The following information is intended as a guideline for the management of dvt prophylaxis in children after trauma. Management of the actual patient may require a more individualized approach. A. Background 1. The incidence of developing deep vein thrombosis (DVT) or pulmonary emboli (PE) in children after trauma increases with the number of thrombotic risks factors. B. Prophylaxis Indications: 1. For trauma patients admitted to the PICU: a. Patients 13 years and older should receive prophylaxis. b. Patients < 13 years should receive prophylaxis if 4 or more risk factors are present (section B.3). 2. For trauma patients admitted to general floors: a. Patients 13 years and older should receive prophylaxis if 3 or more risk factors are present (section B.3). b. Patients < 13 years should not routinely receive prophylaxis, however the presence of certain risk factors such as previous thrombosis or ongoing thrombophilia may warrant prophylaxis. 3. Risk Factors for DVT in Pediatric Trauma Patients: a. Expected decreased mobility > 5d, including bedrest, paralysis/paresis, non-weight bearing, cast or other rigid immobilization b. GCS < 9 c. CVL d. Spinal Cord Injury e. Complex lower extremity fracture f. Operative pelvic fracture g. Use of inotropes h. CPR during resuscitation i. Exogenous Estrogen j. Chronic Inflammatory State: eg.Inflammatory bowel disease, rheumatoid arthritis k. Current malignancy l. Known Thrombophilia m. History of Previous Clot C. Delay chemical prophylaxis for: - Page DVT prophylaxis a. Intracranial Bleed b. Solid Organ Injury c. Planned surgical Intervention / invasive procedure within the next 12-24 hours* d. Heparin Allergy e. Renal Failure - consult hematology for alternate anticoagulation or dosing *Note: Discuss with medical service performing the planned procedure whether to delay initiation, or hold dose(s) if patient already on prophylaxis. See section D. 3. below. 1. Patients who are high-risk for thrombosis and meet these exclusion criteria, should not receive chemical prophylaxis: a. Screen for thrombosis with duplex ultrasound of upper and lower extremities between day 5 and 7 or on transfer out of ICU or to rehabilitation service. b. Sequential compression device (SCD)( full leg or foot pumps) to be used in patients with contraindication to anticoagulation. 2. Risk factors and exclusion criteria should be reassessed daily and prophylaxis initiated if the patient’s exclusion criteria resolve based on status of injury stability and recovery . 3. It is important that lines of communication remain open between services, and that delayed or altered operative schedules not lead to extended delay of anticoagulation (> 24 hours). D. Prophylaxis Dosing: 1. Enoxaparin (LMWH) 0.5 mg/kg SQ BID a. No need to follow levels b. Superior to SQ unfractionated heparin for prophylaxis. 2. Duration of anticoagulation a. Generally until discharge b. If the patient is transferred (eg from PICU to floor) but risks for DVT remain, prophylaxis should continue. c. Routine prophylaxis after discharge is generally not indicated except in certain situations, such as spinal cord injury and prolonged immobilization DVT prophylaxis – Page 3 3. Adjusting dosing scheduled for planning invasive procedures: i. Any spinal or epidural procedure: the preceding 2 doses of LMWH should be omitted. For example, if a patient is to have a lumber puncture on Tuesday morning, they should miss their dose of LMWH the night prior to, and morning of, the lumbar puncture. ii. Orthopedic surgery: the dose of LMWH just prior to the procedure should be omitted. iii. Other major surgeries: the preceding 2 doses of LMWH should be omitted. iv. Minor procedures such as line placement: hold the dose of LMWH prior to procedures in a compressible site, and administer following the procedure if within a few hours of the scheduled dose. v. Restart LMWH 8-12 hours after surgery if the risk of bleeding is low. Consult Hematology with any questions regarding dosing around planned interventions. E. F. Hematology consult: 1. Consult hematology for the following conditions: a. Development of thrombosis b. Thrombocytopenia with anticoagulation c. Renal failure d. Other concerns Thrombosis: 1. Imaging for thrombosis (Doppler ultrasound) is indicated if the patient develops extremity erythema, venous congestion, edema, unexplained pain or persistant CVL dysfunction. 2. Imaging for pulmonary emboli (Chest CT with contrast) if shortness of breath or hypoxemia occurs. Developed and written by the Trauma Program at the Children’s Hospital of Wisconsin. Bibliography 1. 2. Andrew et al, Venous Thromboembolic Complications (VTE) in Children: First Analysis of the Canadian Registry of VTE. Blood. Volume 83, 1994. Rogers et al, EAST guidelines. Journal of Trauma July 2002 - Page DVT prophylaxis 3. 4. Vavilala et al. Risk Factors for Venous Thromboembolism in Pediatric Trauma Journal of TRAUMA. Volume 52, 2002. Azu et al. Venous Thromboembolic Events in Pediatric Trauma Patients: Is Prophylaxis Necessary? Journal of TRAUMA. vol 59, 2005. Revised: 04/08 Disclaimer for Release of Children’s Hospital and Health System Form Documents Children’s Hospital and Health System (CHHS) does not make any representation with respect to any sort of industry recognized standard of care for the particular subject matter of this/these document(s). Additionally, CHHS form documents are subject to change, revision, alteration and/or revocation without notice. DVT prophylaxis – Page 5