Respiratory System
advertisement
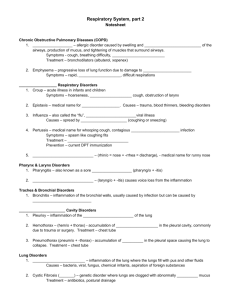
COPD: Chronic Obstructive Pulmonary Disease “Chronic or recurrent reduction in expiratory airflow within the lungs”. Lung disease. A medical “catch phase” of diagnoses for lung disease characterized by increased airway resistance, specifically prolonged forced exhalation. COPD usually manifests as a combination of chronic bronchitis, emphysema, asthma and bronchiectasis. Patients with COPD usually present with wheezing, hyperinflated lungs and a flat diaphragm “Barrel chest” Something is restricting them from getting air out of their lungs. Asthma Emphysema Bronchitis bronchiectasis ASTHMA Characterized by increased responsiveness of the trachea and bronchi to stimuli. Patients present with narrowing of bronchial airways [bronchospasm/bronchoconstriction]. A stimulus or “trigger” causes smooth muscle spasm, inflammation of mucosa and an increased production of mucus. Symptoms: “Wheezing, dyspnea, cough, and sputum” Patients present with an increased respiratory rate, accessory muscle use (to compensate), prolonged exhalation phase, wheeze and a productive or non-productive cough (there will be lots of mucus, may or may not come out, airways might be too narrow for it to come out). They tend to “trap air”. The Global Initiative for Asthma [1995] defines Asthma as: 1. Asthma – whatever the severity – is a chronic inflammatory disorder of the airway. 2. Airway inflammation is associated with airway hyper-responsiveness, airflow limitation, and respiratory symptoms. 3. Airway inflammation produces four forms of airflow limitation: acute bronchoconstriction (acute spasm of smooth muscle), swelling (edema) of the airway wall, chronic mucus plug formation, and airway wall remodeling (wall will try to thicken to protect itself). 4. Atopy, the predisposition for developing an IgE-mediated response (overactive histamines making the person oversensitive) to common environmental allergens, is the strongest identifiable predisposing factor for developing asthma. OR: People with allergies are more predisposed to asthma. 5. Considering Asthma an inflammatory disorder has implications for the diagnosis, prevention, and management of the disorder. Allergic/ Extrinsic Asthma: diagnosed under 35 y.o., exercise induced asthma, cold air etc, a know triggers to precipitate the attack (pollen, dust). Non Allergic / Intrinsic: over age 35. may be related to stress or occupational hazards (inhaled pollutants/chemicals). Pathophysiology: Hyperinflated lungs (air trapping in the lungs during exhalation) Edematous, inflamed lung mucosa (inner lining gets thicker w/tissue and fluid) Thickened basement membrane (bigger secretion producing cells/goblet) Enlarged mucus glands Increased number of goblet cells Hypertrophied and thickened bronchial smooth muscle (gets thicker and stronger, closes airways) Medical management: Medical management includes use of inhaled medications (“puffers” such as Ventolin and Atrovent), supplemental oxygen and education around identification of and avoidance of triggers, breathing and relaxation techniques etc. Inhaled medications can include bronchodilators (opens the airways), steroids (corticosteroids – to control inflammation), adrenalin, muscle relaxants, antihistamines and/or anti-inflammatories. Reducing triggers in the home is a start. Find out exactly what type of medications they use and what it is doing for them. This will tell you the severity of their asthma. Take for health history. If they have an attack during a MxTx, give them their puffer, talk about continuing or not. Depends on the client. The length / severity of an “attack” is always unpredictable (30 seconds to hours). An attack lasting several hours that is unresponsive to medical treatment is known as Status Asthmaticus = MEDICAL EMERGENCY. The sufferer will become fatigued and lethargic as their respiratory muscles tire, they will become cyanotic (trapped gases are absorbed, “new” airflow is obstructed), and may die. Long term effects of disease process: May not be able to do sports, go to smoky bars, hang out with family who wears lots of perfume, cant go to the park because of ragweed season. Social impact. Cardiovascular health will be poor. High blood pressure – heart has to work harder to pump blood for gas exchange. Enlarged lungs will compress on the heart and vessels. Physical / mechanical changes in costovertebral/intercostal, diaphragm muscles and thoracic cage. Musculoskeletal: o Increased use of accessory muscles of inspiration leading to shortening, overuse syndromes (TOS, forward head posture, TrP’s etc) and weakened cough. o Barrel chest, increased thoracic kyphosis, lumbar and cervical lordosis – global decrease in thoracic mobility. (increased risk of arthritis) Cardio-Vascular: o Increased risk of hypertension and heart failure due to increased resistance in lungs and pulmonary vessels. o Heart rate increases during “attacks” in attempt to maintain perfusion and oxygen delivery to tissues. o Medication may add stress to heart (adrenalin) Respiratory: o Lungs lose elasticity which can cause damage to alveoli (increased tension) o Net result is an increase in work of breathing and further dyspnea o Changes to lung parenchyma increase a clients susceptibility to congestion and infection. Emotional impact: o Dyspnea is frightening! Clients may associate deep breathing with an asthma attack – will then avoid deep breathing, revert to apical patterns. Clients will avoid activities and environments they feel may trigger an attack, limiting opportunity to participate in exercise and leisure activities (avoid outdoors due to allergies, humidity etc). Exercise itself may be a trigger as respiratory system is challenged. Disease process may lead to social isolation. Challenges with clients who have asthma: o Overuse / chronic strain of respiratory muscles o Postural dysfunction – kyphosis, lordosis in c-spine, forward head position, barrel chest, TOS (thoracic outlet syndrome) o Decreased mechanics of breathing – tight diaphragm, weak resp. muscles, postural dysfunction o Increased mucus production – chronic cough, mucous plugging o Increased SNS activation – working a TrP may be a trigger o Emotional stress o Use of face cradle may be claustrophobic and lead to respiratory distress o Pillowing and/or prone positioning may inhibit diaphragm function. o Allergens, sensitivities (essential oils, detergents, disinfectants) o Hypertension CHF/HTN o Constipation Things to think about: CI’s, medications Positioning: how do they sleep, it will be harder for them to breathe in prone it puts strain on the diaphragm. Seated/semifowlers may be better. Goals: o Decrease M tension / strain – normalize length and tone of affected MM. o o o o Normalize posture Improve mechanics of breathing Decrease SNS firing / general relaxation Facilitate secretion clearance (mucus) Treatment plan: o Diaphragmatic and pursed lip breathing exercises. Special breathing: pursed lip breathing – inhale normally, exhale with lips close together like a whistle. Keeps the lungs open, ribs open longer, because the mouth is smaller, less air can go out, the exhale is longer. It increases back pressure in airways to help prevent airway collapse and prolongs exhalation phase which facilitates gas release. o Hydro: facial steam (loosen mucus) depends on severity, humid air is difficult to breathe o Fascial work to decrease restrictions – posture, msk tension o Address tone/length/strength of resp and postural M. – swedish mx, indirect TrP, general relaxation work. o Maintain Thoracic mobilization – ROM, mobility and jt health – jt play, stretching, m length/tone. rhythmic mobs, rib mobilization o Tapotement – can loosen mucus, might also be a trigger o Address compensations, attempt to normalize respiratory function o Education – avoidance of triggers (allergens, heat, humidity etc) Changes to environment (air filters, hypoallergenic products etc) Adaptations to exercise programs EMPHYSEMA A chronic degenerative lung condition characterized by: o Abnormal enlargement of air spaces distal to the terminal bronchioles o Destruction of alveolar walls and capillary beds This leads to: o Dev. Of “bullae” = large “pockets” in lung tissue. Must be > 1cm. In diameter to be defined as Bullae. They cause an increase in overall lung volume., will compress adjacent “healthy” lung tissue, impairing ventilation and perfusion. They may be surgically removed both to reduce compression and to avoid “bursting” of bullae which may lead to a pneumothorax. Loss of lung elasticity. Causes: o Majority of cases are related to smoking (both primary and second-hand smoke)! o A sm. Percentage of cases are related to a genetic defect in the structure of the respiratory unit. o Pollution o Repeated respiratory infections (esp chronic bronchitis) Types: Centrilobar: destruction of respiratory bronchiole w/edema, inflammation and thickening of the bronchiolar wall. Most common in upper half of lungs. Effects men > women. Is rare in nonsmokers – is almost exclusively a disease of smokers. Panlobar: destructive enlargement of alveoli distal to the terminal bronchiole. Alveoli then become more prone to collapse during exhalation. Can be found throughout the entire lung. Most commonly due to smoking but is seen in groups w/genetic defect. Signs and Symptoms: o Slow insidious onset of dyspnea o Tachpynea – rapid, shallow respiration o Labored inspiration, forced exhalation This leads to overall poor gas exchange. Client will make attempts to over ventilate to compensate. Clients often require supplemental home oxygen as the disease process progresses. Clinical Presentation: Musculoskeletal: - Increased use of accessory muscles of inspiration leading to shortening and overuse syndromes (TOS, forward head posture, TrP’s etc) - Barrel chest, increased thoracic kyphosis, lumbar and cervical lordosis – global decrease in thoracic mobility. (increased risk of arthritis) - Diaphragm flattens (as lungs hyperinflate) – limits respiratory effort, compresses abdominal contents. Cardiovascular: - Increased risk of heart failure and hypertension due to increased resistance in lungs and pulmonary vessels Emotional Impact: - Fear of dyspnea - Fatigue, chronic hypoxia limits ADL’s - Leads to frustration, anger, low self esteem Clinical Considerations: o Address respiratory muscles for tone, length and strength o Maintain thoracic rom, mobility and joint health – jt play, stretching, muscle length/tone, rib mobs (compression not rib springing) o Address compensations, attempt to normalize respiratory function o Diaphragmatic and pursed lip breathing exercises o Promote general relaxation o o o o Education: - smoking cessation!! Awareness of individual modifications: CHF/HTN Pillowing and or prone positioning may inhibit diaphragm function.