SurgMCQ2Answers - University College Cork
advertisement
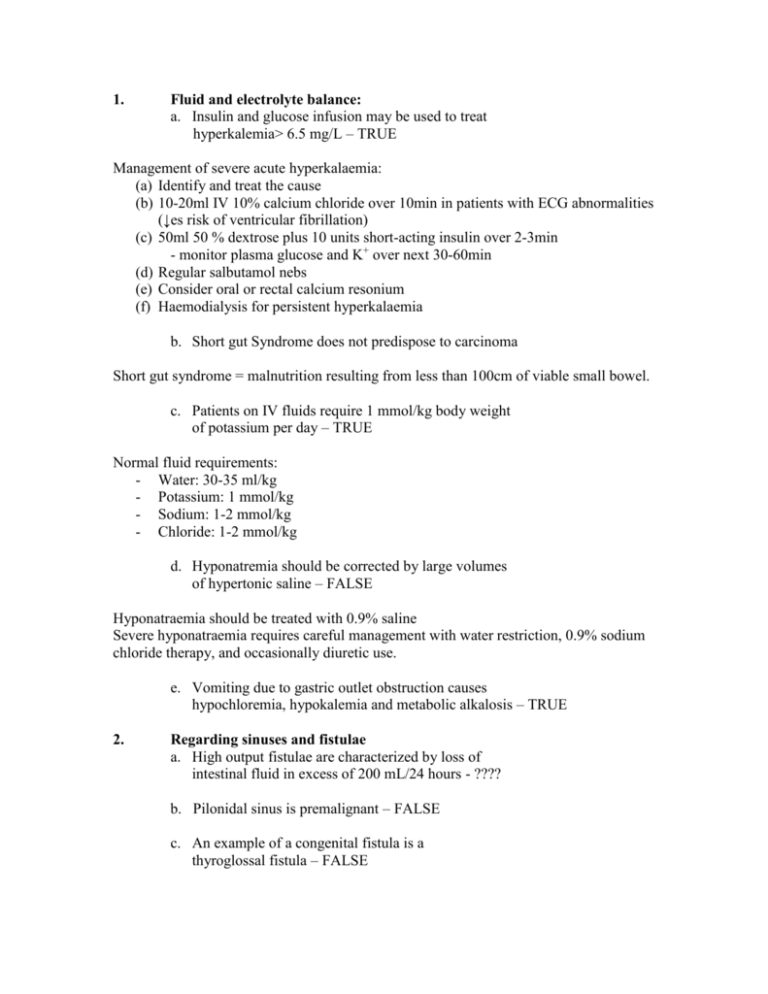
1. Fluid and electrolyte balance: a. Insulin and glucose infusion may be used to treat hyperkalemia> 6.5 mg/L – TRUE Management of severe acute hyperkalaemia: (a) Identify and treat the cause (b) 10-20ml IV 10% calcium chloride over 10min in patients with ECG abnormalities (↓es risk of ventricular fibrillation) (c) 50ml 50 % dextrose plus 10 units short-acting insulin over 2-3min - monitor plasma glucose and K+ over next 30-60min (d) Regular salbutamol nebs (e) Consider oral or rectal calcium resonium (f) Haemodialysis for persistent hyperkalaemia b. Short gut Syndrome does not predispose to carcinoma Short gut syndrome = malnutrition resulting from less than 100cm of viable small bowel. c. Patients on IV fluids require 1 mmol/kg body weight of potassium per day – TRUE Normal fluid requirements: - Water: 30-35 ml/kg - Potassium: 1 mmol/kg - Sodium: 1-2 mmol/kg - Chloride: 1-2 mmol/kg d. Hyponatremia should be corrected by large volumes of hypertonic saline – FALSE Hyponatraemia should be treated with 0.9% saline Severe hyponatraemia requires careful management with water restriction, 0.9% sodium chloride therapy, and occasionally diuretic use. e. Vomiting due to gastric outlet obstruction causes hypochloremia, hypokalemia and metabolic alkalosis – TRUE 2. Regarding sinuses and fistulae a. High output fistulae are characterized by loss of intestinal fluid in excess of 200 mL/24 hours - ???? b. Pilonidal sinus is premalignant – FALSE c. An example of a congenital fistula is a thyroglossal fistula – FALSE An example would be a branchial cyst d. Inefficient or non-dependent drainage is one of the factors leading to persistence of a sinus – TRUE e. A chronic subareolar abscess can lead to a mammary fistula – TRUE 3. Regarding thyroid and parathyroid neoplasms a. Follicular carcinoma of thyroid primarily spreads through lymphatics – FALSE P/C: solitary thyroid nodule in patients aged 30-50 years Lymph node metastases are much less common than haematogenous spread 20% of patients have deposits in the lungs, bone or liver Histology: malignant cells are arranged in solid masses with rudimentary acini Vascular and capsular invasion characterize this neoplasm and distinguish it from a benign follicular adenoma b. Parathyroid adenoma is the most likely cause of primary hyperparathyroidism – TRUE 90% of 1° hyperparathyroidism is due to an adenoma 10% are due to Hyperplasia (usually affecting all 4 glands) <1% from parathyroid carcinoma c. Hürthle cell carcinoma is a variant of papillary carcinoma of the thyroid – FALSE Hürthle cell carcinoma is a thyroid cancer of Hürthle cells Follicular cells are the cells of origin FNA can identify cells, but malignancy can be determined only by tissue histology (like follicular cancer) Lymphatic spread > haematogenous spread d. Phaeochromocytoma is detected by measuring urinary 5-HIAA levels – FALSE Phaeochromocytoma is a tumour of the adrenal medulla and sympathetic ganglion (from chromaffin cell lines) that produces catecholamines (norepinephrine > epinephrine) Phaeochromocytoma is detected by measuring: - vanillymandelic acid (VMA) - metanephrine - normetanephrine (all breakdown products of the catechols) e. Superior laryngeal nerve supplies cricothyroid muscle – TRUE Superior laryngeal nerve supplies the cricothyroid muscles (external branch), which tense the vocal cords, the internal branch supplies sensation above the cords The external branch can be damaged during ligation of the vascular pedicle at the upper pole of the thyroid → inability to tense the vocal cord results in a weak, hoarse deep voice 4. Regarding lesions of the breast a. A breast lesion is >5 cm in dimension - FALSE b. Tamoxifen should be prescribed for life to patients with breast cancer – FALSE Give tamoxifen for 5 years if premenopausal, and for 2 years if postmenopausal (plus aromatase inhibitor for 3 years) c. Axillary lymph node involvement is a weak predictor of outcome – FALSE The single most important prognostic factor is the number of axillary lymph nodes involved. d. Comedo DCIS is associated with lower recurrence rate – FALSE It is the most aggressive type e. Breast cancer metastasizes to lung more commonly than bone - ??? 5. Abdominal Aortic Aneurysms (AAA) a. Surgery is recommended for patients with AAA size > 6 cms – TRUE <5.5cm: the risks of surgery generally outweigh the risk of rupture Repair is considered when the AAA exceeds 5.5cm Repair: Prosthetic graft placement – with rewrapping of the native aneurysm adventitia around the prosthetic graft after the thrombus is removed Endovascular repair – repair of the AAA by femoral catheter placed stents b. 90% arise below renal arteries – FALSE 70% are infrarenal 30% occur in the rest of the abdominal aorta, the thoracic aorta or a combination of both is involved c. Ischemia of the colon is a peri-operative risk – TRUE Often the inferior mysenteric artery is sacrificed; if the collaterals are not adequate, the patient will have colonic ischaemia, typically occurs in the 1st week post-operative Signs: haem +ve stool, or bright red blood per rectum, diarrhoea, abdominal pain Diagnosis: Colonoscopy Treatment: 1. Resection of necrotic colon 2. Hartmann’s pouch or mucus fistula 3. End colostomy d. Mortality rate of ruptured AAA is 25% - FALSE Mortality rate is >50% Risk factors for rupture: - ↑ing aneurysm diameter - COPD - HTN - Recent rapid expansion - Large diameter - Symptomatic Signs of rupture → abdominal pain, pulsatile abdominal mass, hypotension e. Blue toe syndrome occurs in association with AAA - TRUE Blue toe syndrome = intermittent painful blue toes (or fingers) due to microemboli from a proximal arterial plaque 6. T/F: a. Carotid atheromatous disease is the commonest cause of strokes in the western world – TRUE b. Varicose veins are treated by femoral-popliteal bypass graft – FALSE Non-surgical: - Graduated elastic support stockings (Grade II compression) - Encourage weight loss and regular exercise Surgical: - - Injection sclerotherapy with 1% sodium tetradecyl sulphate (high recurrence rate), indicated for → post-op recurrence of veins, below knee varicosities if the LSV and SSV are not involved Ligation of the incompetent SFJ or SPJ with stripping of the involved vein and stab avulsion of varicosities Ligation of incompetent perforating vessels (with site of incompetence pre-op marked with Duplex) Subcutaneous endoscopic perforator surgery (SEPS) c. Chest pain is relieved by elevation of the foot – FALSE (what the hell!!!) d. Diabetic patient presenting with an ischemic foot may have an Ankle Brachial Pressure Index of 0.8 – TRUE The Ankle Brachial Pressure Index (ABPI) is the ratio of the systolic blood pressure at the ankle to the systolic blood pressure at the arm Normal ABPI >1.0 Claudicator ABPI <0.6 Rest pain ABPI <0.4 Patients with calcified arteries, esp. those with diabetes, can get false ABPI readings e. Cervical rib may present with wasting of the thenar muscles – TRUE Symptoms and signs: - Vascular symptoms → Raynaud’s phenomenon, venous thrombosis in the arm - Neurological symptoms → wasting of the small muscles of the hand, paraesthesiae on the inner upper aspect of the arm in the dermatomal distribution of T1. - May be palpable lump in the supraclavicular fossa 7. Regarding colorectal cancer a. Hereditary non-polyposis colorectal cancer is autosomal dominant – TRUE There are 2 types of AD HNPCC: - cancer family syndrome (CFS), which occurs with early onset at around 2030years and is associated with other adenocarcinoma esp. endometrial carcinoma and breast carcinoma - hereditary site-specific colonic cancer (HSSCC), which shows the same characteristics as CFS except for the extracolonic carcinomas b. Colorectal cancers develop before 40 years of age in familial adenomatous polyposis (FAP) – TRUE FAP: hundreds of adenomatous polyps within the rectum and colon that begin developing at puberty; all undiagnosed, untreated patients develop cancer by ages 40-50. Treatment: Total proctocolectomy and ileostomy Total colectomy and rectal mucosal removal (mucosal proctectomy) and Ileoanal anastomosis c. Polyps in Peutz Jeghers Syndrome are hyperplastic – FALSE Polyps are hamartomas d. The Familial Adenomatous Polyposis gene is on the short arm of chromosome 5 – TRUE The gene responsible is the APC gene, which is located on the long arm of chr 5 e. Hereditary nonpolyposis colorectal cancer accounts for 5% of colorectal cancer cases. - TRUE 8. Hernias a. Direct inguinal hernias pass through the internal ring – FALSE Direct herniae are due to weakness of the abdominal wall and may be precipitated by increases in intra-abdominal pressure (e.g. COPD, prostatism or chronic constipation) Protrudes through the transversalis fascia in the posterior wall of the inguinal canal Bounded by Hesselbech’s triangle: - Above: conjoint tendon - Below: inguinal ligament - Laterally: inferior epigastric vessels b. A femoral hernia is the most common hernia in females – FALSE Although 85% of femoral hernias occur in females, the most common hernia in females is indirect inguinal hernia c. Testicular atrophy may occur after inguinal hernia repair – TRUE Complications of surgery include: - haematoma (wound or scrotal) - Acute urinary retention - Wound infection - Chronic pain - Testicular pain and swelling leading to testicular atrophy - Hernia recurrence (about 5%) d. Inguinal hernias in children are treated by herniorraphy – FALSE Paediatric inguinal hernia repair: - High ligation of hernia sac (herniotomy) - No repair of the abdominal wall floor (i.e. no herniorraphy) e. Open appendicectomy is associated with an increased incidence of right sided indirect inguinal hernia – TRUE Other complications include: 9. Small bowel obstruction Enterocutaneous fistula Wound infection Infertility with perforation in women Stump abscess Pancreatitis a. Cholelithiasis is the commonest cause – FALSE Alcohol is the most common cause b. Cullen’s sign is associated with bruising in flanks – FALSE Cullen’s sign: Bluish discolouration of the periumbilical area due to retroperitoneal haemorrhage tracking around to the anterior abdominal wall through fascial planes (e.g. acute haemorrhagic pancreatitis) b. Steroids are not associated with acute pancreatitis – FALSE Causes of acute pancreatitis: ‘I GET SMASHED’ - Idiopathic - Gallstones - Ethanol - Trauma - Scorpion bite - Mumps (and other viruses) - Autoimmune - Steroids d. The treatment of sterile necrotizing pancreatitis in necrosectomy – TRUE Tx: antibiotics +/- surgical debridement e. A pseudocyst should be drained within 2 weeks of the acute attack – FALSE It takes 6 weeks for pseudocyst to ‘mature’ or become firm enough to hold sutures and most will resolve in this period of time if they are going to. Approx. 50% resolve spontaneously 10. Gallstones a. Ascending cholangitis requires emergency decompression of the Common Bile Duct - ?FALSE b. Choledochal cysts are associated with malignancy – TRUE Complications of choledochal cysts: Cholelithiasis, cirrhosis, carcinoma portal hypertension c. The five year survival rate of adenocarcinoma of gallbladder is less than 5% - TRUE d. Magnetic Resonance Cholangiography gives an accurate picture of the biliary tree – TRUE e. Gallstones can be dissolved by chenodoxycholic acid – TRUE Chenodoxycholic acid and ursodeoxycholic acid dissolve cholesterol gallstones but if medication is stopped, gallstones recur 11. Diverticular disease a. Bleeding from diverticular disease is characteristically plum colored – FALSE Diverticular disease: spontaneous onset, large volume, mostly fresh blood, previous history of constipation b. The treatment of diverticular disease is oral steroids – FALSE Treat with a high fibre diet Diverticulitis: IV fluids, NPO, broad-spectrum antibiotics with anaerobic coverage, NG suction (as needed) c. May arise in the rectum - TRUE c. Is best treated with a low residue diet – FALSE If low residue means low fibre then it is false!! d. May present with Urinary Tract Infection – TRUE Painful diverticulosis: LIF pain, constipation, diarrhoea Acute diverticulitis: malaise, fever, LIF pain and tenderness +/- palpable mass and abdominal distension Perforation: peritonitis + features of diverticulitis Large bowel obstruction: absolute constipation, distension, colicky abdominal pain, vomiting Fistula: to bladder (cystitis/pneumaturia/recurrent UTIs); to vagina (faecal discharge PV); to small intestine (diarrhoea) Lower GI bleed: painless spontaneous 12. Orthopaedics a. Smith’s fracture results in volar angulation of the radius – TRUE Smith’s fracture (AKA ‘Reverse Colles’ fracture) involves distal radial fracture with volar displacement and angulation, usually from falling on the dorsum of the hand (uncommon) b. A fractured neck of femur results in external rotation of the lower limb – TRUE Results in external rotation and leg adduction c. The radial nerve is often injured in fracture of the neck of humerus – FALSE Risk to the brachial plexus and axillary artery Fracture of shaft of humerus can cause radial nerve damage d. Bennett’s fracture involves distal end of radius – FALSE Bennett’s fracture: fracture-dislocation of the base of the 1st metacarpal with disruption of the carpometacarpal joint e. Supracondylar fracture of humerus may cause vascular complications – TRUE Keeping the elbow in extension after injury prevents brachial artery. Median and ulnar nerve palsies are rare complications 13. Trauma/Cardiothoracic a. In the initial management of the injured patient, control of hemorrhage should be the priority – FALSE Initial management should begin with Airway, Breathing and Circulation b. Right diaphragmatic rupture is more common than left – FALSE Can occur with blunt or penetrating trauma. Blunt trauma usually results in tears of the left posterolateral hemidiaphragm. Penetrating trauma may result in herniation years after injury as the defect gradually increases c. Fracture of left lower ribs may be associated with ruptured spleen d. A flail chest is commonly associated with Acquired Respiratory Distress Syndrome e. Tension pneumothorax is diagnosed on chest X-ray 14. Urology a. In suspected torsion of the testis, ultrasound may be of value – TRUE Diagnosis can be made by: Surgical exploration Ultrasound (solid mass) & Doppler flow study Nuclear study – cold Tc-99m scan b. Unilateral orchidopexy is the treatment of choice for torsion of the testis – FALSE Treatment includes surgical detorsion and bilateral orchidopexy to the scrotum c. Varicocele is more common on the right side - FALSE It is more common on the left side d. Varicocele is associated with oligospermia – TRUE e. Uric acid calculi are the most common types of renal calculi – FALSE Types of stones: (a) Calcium oxalate/calcium PO4 (75%) (b) Struvite (MgAmPh) (15%) (c) Uric acid (7%) (d) Cystine (1%) 15. Pleomorphic salivary adenoma a. Presents as a slowly growing painless lump – TRUE b. Can present with facial nerve weakness – TRUE c. Treatment includes radiotherapy – FALSE Treatment: excision with a cuff of normal tissue (superficial parotidectomy) d. Sentinel lymph node mapping is recommended – FALSE e. The minimum operation is a superficial parotidectomy – FALSE 16. Melanoma a. Ulceration of the primary lesion is associated with worsening of prognosis – TRUE Indicators of poor prognosis include: - Increasing age of the patient - Male patients - Melanomas on the trunk (esp. the back), scalp, hand and foot - Ulceration of the tumour - Depigmentation and amelanotic melanomas - Aneuploidy and high mitotic index b. A brisk tumour infiltrating lymphocyte response is associated with worse prognosis - ??? c. Clark’s level III implies invasion of the reticular dermis – FALSE Staging malignant melanoma → Clark’s level and Breslow’s thickness Clark’s level I II III IV V Extent of tumour Epidermis only Invades papillary dermis Fills papillary dermis Invades reticular dermis Subcutaneous invasion 5-year survival 98% 96% 94% 78% 44% Breslow Thickness 10-year survival 92% 50% 30% <40% (8 year survival <0.76 mm < 3 mm < 4 mm Lymph node involvement d. Suspicious lesions should be evaluated by initial incisional biopsy – FALSE Always consider excisional biopsy e. Sentinel lymph node mapping should be considered for lesions of intermediate depth (1-4 mm) – TRUE 17. Nerve injuries/Hand a. Flexor tendons require at least 6 weeks of immobilization for adequate healing and strength - ??? b. A compound fracture of metacarpal, sustained while punching an opponent in teeth, should be treated with antibiotics – TRUE c. Tinel’s sign is useful in monitoring progress following nerve repair – FALSE d. Ulnar nerve entrapment is more common at elbow than wrist – TRUE e. Normal sensation over the thenar eminence is consistent with carpal tunnel syndrome – FALSE 18. In head injury patients a. Patients with acute subdural hematoma present with a lucid interval – FALSE Symptoms & signs: Severe head injury. May be rapid deterioration. Signs of raised ICP. Localizing signs. Pupillary inequality. b. The lowest Glasgow Coma score possible is 3 – TRUE Glasgow Coma Scale (GCS) Responses Eye-opening response - Spontaneous - To voice - To pain Score 4 3 2 - None Best verbal response - Orientated - Confused - Inappropriate speech - Incomprehensible speech - None Best motor response - Obeys commands - Localises pain - Withdraws to pain - Flexion to pain - Extension to pain - None Total 1 5 4 3 2 1 6 5 4 3 2 1 3-15 c. Skull fracture is a risk factor for extradural hematoma – TRUE Extradural haematoma is a collection of blood between the skull and dura Usually occurs in association with a skull fracture as bone fragments lacerate meningeal arteries d. In a patient with decreased level of consciousness, skull X-ray is the investigation of choice – TRUE e. Normal intracranial pressure ranges between 10-30 mmHg – FALSE Normal intracranial pressure: 5-15cm H20, 0-15 mmHg 19. Delayed recovery of consciousness following general anesthesia may be caused by a. Intra-operative hypoxia - TRUE b. Carbon dioxide narcosis - TRUE c. Opioid premedication - FALSE d. Residual neuromuscular blockade - FALSE e. Hyperventilation - FALSE 20. Factors which increase the likelihood of aspiration of gastric content at the induction of anaethesia a. Increasing age - TRUE b. Anxiety - TRUE c. Chronic Obstructive Pulmonary Disease - FALSE d. Major Trauma – TRUE if leading to gastric emptying delay e. Pregnancy - TRUE High risk factors for regurgitation: - Oesophageal disease: pouch, stricture - Gastro-oesophageal sphincter abnormalities: hiatus hernia, obesity, drugs - Gastric emptying delay: trauma, pyloric stenosis, gastric malignancy, opiates, patient predisposition, anxiety, pregnancy, recent food intake - Abnormal bowel peristalsis: peritonitis, ileus (metabolic or drugs), bowel obstruction EXAM 3 Final Medical Surgical MCQ March, 1999 1. The following associations are true: a. Galen (AD 131-200) : A Greek b. Andreas Vesalius (1514-1564) :De Humanis Corporis Fabrica; c. Benjamin Alcock (1849) : Professor of Anatomy, Cork d. Ignaz Semmelweiss (1818-1865) : Postpuerpal sepsis e. Abraham Colles (1773-1843) : Orthopedic Surgeon, Cork True: Galen performed many audacious operations that were not again used for almost two millennia, including brain and eye surgery. To perform cataract surgery, Galen would insert a long needle-like instrument into the eye behind the lens. He would then pull it back slightly and remove the cataract. The slightest slip could cause permanent blindness. He was reknowned for his detailed knowledge of anatomy. True: Vesalius is often referred to as the founder of modern human anatomy. Publishing the landmark book, :De Humanis Corporis Fabrica in the 16th century. He corrected many of Galen’s errors, e.g. the main blood vessel of the body does not arise from the liver! True: The first Prof of anatomy in Cork. Described Alcock’s canal aka the pudendal canal. Sound familiar?! True: He was a Hungarian physician called the "savior of mothers" who discovered, by 1847 that the incidence of peurperal fevercould be drastically cut by use of hand washing standards in obstetrical clinics False: RCSI. As well as describing the Colles’ fracture He also described the membraneous layer of subcutaneous tissue of theperineum, which came to be known as Colles’ fascia. He also extensively studied theinguinal ligament, which is sometimes called Colles’ ligament. 2. Regarding Hypertrophic pyloric stenosis a. There is a predominance of males 4:1 (M:F) b. Stenosis occurs 4-6 weeks after birth c. Characteristically presents with blood stained projectile vomiting d. 0.45% saline solution is the resuscitation fluid of choice e. Hypokalemic hypochloremic metabolic acidosis chracterises the metabolic disturbance a. b. c. d. e. True True False True True Hypertrophy of the smooth muscle of the pylorus occurs in 1:750 births. There is a 4:1 male preponderance with first born males and those with a positive family history being at increased risk. The pylorus is normal in the first number of weeks with the development of symptoms anywhere from 2 weeks to 2 months. The vomitus is nonbilious as obstruction is proximal to the ampulla of vater. Biochemical analysis reflects dehydration with low Na, and a high urea. There is a low K and Cl (vomitus) and an increased bicarbonate. Regarding fluid deficit replacement Na deficits are generally about 80 mEq/L of fluid deficit, and K deficits are generally about 30 mEq/L of fluid deficit, Because 0.45% saline has 77 mEq Na per liter, it is generally an appropriate fluid choice. K replacement (usually by adding 20 to 40 mEq K per liter of replacement fluid) should not begin until adequate urine output is established. Definitive treatment is with Ramstedt’s pyloromyotomy (Division of circular smooth muscle fibers without dividing the mucosa). 3. Patients presenting with acute pancreatitis a. Hyperparathyroidism may be the underlying aetiology b. Onset of acute pancreatitis is associated with tetracycline therapy c. A normal serum amylase occurs in up to 30% of cases d. Characteristically have associated steatorrhea e. 60% of cases have detectable choledocholithiasis a. b. c. d. e. True True True False True Among the I “get smashed” causes of pancreatitis, hypercalcaemia and drugs are among the rarer causes. The most common causes are Gallstones (60%0, and alcohol (20%) Drugs definitely associated with acute pancreatitis include azathioprine, sulfonamides, sulindac, tetracycline, valproic acid, didanosine, methyldopa, estrogens, furosemide, 6- mercaptopurine, pentamidine, 5-aminosalicylic acid compounds, corticosteroids, and octreotide As serum amylase returns the normal within 48hrs, it is common for levels to be normal upon reaching hospital. Serum lipase levels are more sensitive, as serum lipase remains elevated longer. Epigastric pain radiating to the back with nausea and vomiting are common symptoms of acute pancreatitis, while epigastric pain radiating to the back eith steatorrhoes and weight loss are typical symptoms of chronic pancreatitis. 4. Regarding melanoma a. Juvenile melanoma (Spitz naevus) is a benign condition b. Breslow staging of <0.75mm has predicted 5 year survival of 95-100% c. Acral lentiginous melanoma is the rarest form of melanoma d. Overall males have a better prognosis e. Locoregional radiotherapy confers a significant survival benefit a. b. c. d. e. True True True False False Juvenile melanomas are clinically benign naevi that initially grow rapidly and are seen in exclusively in fair-skinned individuals. Breslow classification Thickness Thickness of 0.75 mm or less Thickness of 0.76-1.5 mm Thickness of 1.51-4 mm Thickness greater than 4 mm The staging of melanomas also involves the regional and distant spread. If lymph node positive – about 45% 5 year survival. Distant mets – about 10%. Poor prognostic factors include; Tumor thickness (worse prognosis in thicker lesions), Evidence of tumor in regional lymph nodes (stage III disease), Higher number of positive lymph nodes, Presence of distant metastasis (stage IV disease), Anatomic site (trunk and/or face lesions have worse prognoses than extremity lesions), Presence of ulceration, Male sex. Definitive treatment requires surgery. Adjuvant and biological therapy are still undergoing evaluation. 5. Risk factors for the development of colorectal carcinoma include: a. Chronic ulcerative colitis b. Peutz-Jeghers syndrome c. Gardners syndrome d. Juvenile polyps e. Previous cholecystectomy a. b. c. d. e. True True True True True After cholecystectomy, bile acids circulate continuously, increasing exposure to the degrading action of intestinal bacteria leading to the production of certain carcinogens. The lifetime risk of colorectal cancer in peutz is 10% 6. The natural history of colonic polyps a. The majority are premalignant b. Overall villous adenomatous polyps have a poorer prognosis than tubular polyps c. There is a higher incidence of rectosigmoid lesions than ascending colonic lesions d. 85% of adenomatous polyps are tubular in nature e. Hereditary polyposis coli is associated with duodenal and gastric polyps a. b. c. d. e. True True True The highest quoted figure I could find was 75% True The overwhelming majority of polyps pound on endoscopy are adenomas. A villous adenoma is three times more likely to become malignant than a tubular adenoma of a similar size. There is associated intestinal polyps in FAP, a major cause of death in FAP is periumpullary tumours in the duodenum. 7. Features of Charcots triad and Reynolds pentad include a. Right upper quadrant pain b. A palpable gall bladder c. Pyrexia d. Rigors e. Shock a. b. c. d. e. True False True False True Charcot’s triad is seen in cholangitis: a triad of fever, jaundice and right upper quadrant pain. Reynolds pentad is Charcot’s triad plus shock and mental status changes – Seen in patients with suppurative cholangitis. Courvoisier’s an enlarged non-tender gallbladder is due to obstruction of the common bile duct. Rigors is not in the pentad, it is a sign of pyrexia, but for pyrexia to diagnosed, objective measurement of the temperature is required. 8. In Inflammatory bowel disease secondary to Crohns Disease a. The rectum is usually involved b. Granuloma formation is characteristic c. There is a male predominance (M:F of 2:1) d. Restorative proctocolectomy potentially offers surgical cure for the disease e. Fistula tract formation is more suggestive of ulcerative colitis a. b. c. d. e. False True False False False 9. Toxic megacolon a. Is unique to ulcerative colitis b. Colonic perforation carries mortality of 50% c. Is best treated with high dose corticosteroids for at least 72 hours d. A gastrograffin enema may be diagnostic e. Occurs in 10% IBD patients a. False b. True c. True d. False e. True Toxic megacolon is the clinical term for an acute toxic colitis with dilatation of the colon. The hallmarks of toxic megacolon, a potentially lethal condition, are nonobstructive colonic dilatation larger than 6 cm and signs of systemic toxicity. The first criterion is radiographic evidence of colonic dilatation. The second criterion is any 3 of the following: fever (>101.5°F), tachycardia (>120), leukocytosis (>10.5), or anemia. The third criterion is any 1 of the following: dehydration, altered mental status, electrolyte abnormality, or hypotension Causes: The classic etiologies of toxic megacolon include the following inflammatory causes: Ulcerative colitis Crohn colitis Pseudomembranous colitis The many causes of infectious colitis, including the following, may lead to toxic megacolon: Salmonella species Shigella species Campylobacter species Yersinia species Clostridium difficile Entamoeba histolytica Cytomegalovirus Toxic megacolon also may be caused by the following: Radiation colitis Ischemic colitis Nonspecific colitis secondary to chemotherapy Avoid enemas as the risk of perforation is high. AXRs and/or abdominal CTs are necessary to follow the progression of the disease process. Medical management includes fluid resuscitation, broad spectrum antibiotic coverage and high dose steroids. If the patient is not improving after 72 hours, or if they are progressing, surgery is indicated. A subtotal colectomy is chosen as a total proctocolectomy is associated with increased complications in an acutely unwell patient. The major complication is perforation. 10. Regarding herniae a. The most common hernia in females in femoral b. Femoral herniae are classically located below and medial to the pubic tubercle c. Herniorrhaphy invariably necessitates herniotomy d. Inguinal hernia nearly always are congenital in origin e. An indirect inguinal hernia will protrude through Hasselbachs triangle a. b. c. d. e. False False False False False While femoral hernias are more common in women than in men, indirect inguinal herniae are still the most common hernia in the groin region. Femoral herniae are found below and lateral to the pubic tubercle. -rhaphy denotes surgical repair, while –otomy denotes an incision into a structue. While herniotomy is required in the repair of an indirect hernia, simple strengthening of hasselbach’s triangle with a simple mesh placedin the posterior wall of the inguinal canal. 11. The following are features of hyperparathyroidism a. Osteoporosis b. Polydipsia and polyuria c. A technetium-99m sestamibi isotope scan would be unhelpful d. Primary hyperparathyroidism is secondary to adenoma in >90% cases e. A positive Chvosteks sign is evident in 30% of cases a. b. c. d. e. True True False: would help in the localisation of any abnormally situated parathyroid glands. False: quoted at 80% False: Rare sign of hypercalcemia 12. Recognized abdominal surgical incisions include a. A Kochers incision b. A Commando incision c. A Battles incision d. A Gridiron incision e. A Mercedes Benz incision a. True: Right subcostal incision for open cholecystectomy b. False: Operation involving radical dissection of the face with a segmental mandibulectomy c. False: Battle’s sign – bruising over the mastoid in association with base of skull fracture d. True: Incision at McBurney’s point perpendicular to the imaginary line( you know the one!) e. True: Seen in liver transplant operations. 13. Thyroid neoplasia exhibits the following features a. Follicular thyroid carcinoma is the most common type b. When associated with MEN IIa, are medullary in origin c. Papillary thyroid carcinoma is often multifocal d. Hematogenous spread is a feature of follicular thyroid carcinoma e. Thyroid lymphoma is strongly associated with Hashimoto’s Disease a. False b. True: Medullary cancer has a poor prognosis. Genetic screening is now possible- ret proto-oncogene. Markers of medullary cancer – calcitonin. c. True d. True e. True: Primary thyroid cancers are usually of the NHL variety. 14. In patients with gastro-oesophageal reflux disease (GORD) a. The treatment is largely medical b. A hiatus hernia is found in over 70% cases c. The Belsey Mark IV procedure alleviates the symptoms d. A Nissen Fundoplication is the operation of choice e. The use of the Demeester scoring system is appropriate a. True b. False: Predisposing factors include the following: Muscle weakening and loss of elasticity as people age is thought to predispose to hiatus hernia, based on the increasing prevalence in older people. With decreasing tissue elasticity, the gastric cardia may not return to its normal position below the diaphragmatic hiatus following a normal swallow. Loss of muscle tone around the diaphragmatic opening also may make it more patulous. Hiatal hernias are more common in women. This may relate to the intraabdominal forces exerted in pregnancy. Burkitt et al suggest that the Western, fiber-depleted diet leads to a state of chronic constipation and straining during bowel movement, which might explain the higher incidence of this condition in Western countries. Obesity predisposes to hiatus hernia because of increased abdominal pressure. Conditions such as chronic esophagitis may cause shortening of the esophagus by causing fibrosis of the longitudinal muscles and, therefore, predispose to hiatal hernia. However, which comes first, the hiatal hernia worsening the reflux or the reflux-induced shortening of the esophagus, remains unknown. The presence of abdominal ascites also is associated with hiatal hernias c. True d. True: This is coming back into vogue, especially with the advent of laporascopic repair. There is a lower post op incidence of reflux. e. False: An old scoring system, overestimates the incidence of GORD 15. The following conditions are premalignant for oesophageal neoplasia a. Tylosis b. Plummer-Vinson Syndrome c. Barret’s oesophagus d. Achalasia e. Scleroderma a. b. c. d. e. True True True True False Tylosis with esophageal cancer: A genetic disorder characterized by thickening (hyperkeratosis) of the palms and soles, white patches in the mouth (oralleukoplakia), and a very high risk of oesophageal cancer. This is the only genetic syndrome known to predispose to Squamous cell carcinomaof the esophagus. The risk of developing esophageal canceris 95% by age 70. The syndrome is inherited in an autosomal dominant manner. Plummer Vinson syndrome usually occurs in elderly women. Post-cricoid oesophageal web and iron deficiency anaemia. 10% develop squamous cell carcinoma. Barrett’s; columnar metaplasia of the LES. Progression can be monitored with endoscopic ultrasound. Photodynamic therapy or laser therapy may be used for low-grade lesions. Management of the reflux with medication is vital. Achalasia increases the risk of squamous cell cancer through the prolonged time food remains in the oesophagus leading to chronic irritation of the mucosa. 16. Regarding intestinal obstruction necessitating inpatient management a. Large bowel obstruction is most commonly caused by neoplasia b. Small bowel obstruction is most commonly caused by incarcerated herniae c. Ogilvies syndrome is a reflection of an underlying mechanical obstruction d. A caecal volvulus is more common than a sigmoid volvulus e. A bird’s beak deformity on barium enema is characteristic of a sigmoid volvulus a. b. c. d. e. True False False False True Common causes of large bowel obstruction include; Cancer, sigmoid/caecal volvulus, diverticulitis and faecal impaction. Small bowel is more commonly caused by adhesions, however remember hernia(any abdominal type), intussusception, Crohn’s, Gallstone ileus, tumour, foreign body, TB. Ogilvie’s syndrome is a fancy term for pseudobstruction. Caused by eloctrolyte disturbance, certain drugs, recent surgery. Caecal volvulus is less common but the risk of gangrene is much higher as the ileocolic artery is often “strangled” The bird’s beak is seen at the distal part of the distal limb of the vovulus 17. The following occur in Leriche syndrome; a. Clubbing b. Claudication c. Lower extremity muscle wasting d. Impotence e. Paradoxically high ankle brachial indiced (ABIs) a. b. c. d. False True True True e. False Also known as Aortic bifurcation syndrome; The internal and external iliacs may be involved. It is described as a disturbance usually affecting young males caused by atheromatous involvement or occlusion of the abdominal aorta by a thrombus just above the site of its bifurcation. The main symptoms are inability to maintain penile erection, fatigue in the lower limbs, cramps in the calf area, ischemic pain of intermittent bilateral claudication; absent or diminished femoral pulse, pallor and coldness of the feet and legs. Onset usually between 30 and 40 years of age 18. In the management of burns: a. A splenectomy is indicated in Class I and II splenic injuries b. Kehrs sign may be found in patients with splenic injury c. An 80kg male with 20% burn surface area will require over 6L fluid in the first 24 hours of resuscitation. d. A liter of Hartmanns solution contains 130 mmol sodium e. A Hartmanns solution is a crystalloid isotonic solution a. False: b. True c. True: Modified Parkland formula for burns: The volume of replacement in the first 24 hrs = (Total body surface area of the burn) Weight(kg) 4 Half the volume is replaced in the first 8 hours and the rest over the following 16 hours. d. True e. True 19. The following are true: a. Volar angulation is a feature of the Smiths fracture b. A Bennett fracture is an intrarticular fracture c. A Colles fracture results in radial deviation d. A dinner fork deformity is characteristically found in Colles fracture e. The Lachman manoeuvre is useful in anterior shoulder dislocation a. True: AKA “reverse colles fracture”. Volar = Ventral b. True: Fracture and dislocation at the base of the first carpometacarpal joint. c. False: Unsure exactly what is meant by deviation. The radius is still aligned when looking from above d. True e. False: a manoeuvre to detect deficiencyof the anterior cruciate ligament; with the knee flexed 20 to 30degrees, the tibia is displaced anteriorly relative to the femur; a soft endpoint or greater than 4 millimeters of displacement is positive(abnormal). 20. Criteria for the diagnosis of the Systemic Inflammatory Response Syndrome (SIRS) include a. A wcc < 4/mm3 b. A temperature greater than 380C or rectal temperature <360C c. A heart rate greater than 90 bpm d. One positive blood culture e. The presence of >10% immature bands forms on a full blood count a. b. c. d. e. True True True False True SIRS is defined as 2 or more of the following variables: Fever of more than 38°C or less than 36°C Heart rate of more than 90 beats per minute Respiratory rate of more than 20 breaths per minute or a PaCO2 level of less than 32 mm Hg Abnormal white blood cell count (>12,000/L or <4,000/L or >10% bands) SIRS is nonspecific and can be caused by ischemia, inflammation, trauma, infection, or a combination of several insults. SIRS is not always related to infection. EXAM 4 : Unknown year, unknown college First two questions missing 3. Trauma a. Pneumothorax can be temporarily treated by inserting a 16 gauge cannula in the second intercostal space of the same side b. Fracture of the posterior cranial fossa is associated with Battle &#8217;s sign c. Ultrasound is the gold standard in the diagnosis of rupture of the thoracic aorta d. A flail chest is associated with pericardial effusion e. Coronary air embolisation is an unusual consequence of injury to the lung parenchyma A) T 14-16 guage needle 2nd ICS MCL. Drain siting 4-6th ICS anterior to MAL B) T bruising/discolouration of the mastoid due to tracking of blood due to fracture of the base of the skull. Some say posterior fossa other sources middle fossa Racoon eyes – Bruising around the orbits due to blood tracking from fracture of base of skull anterior cranial fossa. C) F Aortography is gold standard although ultrasound is used more frequently Idiopathic cystic medial degeneration The most common cause of ascending aortic aneurysms is a condition known as idiopathic cystic medial degeneration. The elastic fibers which make up the outer wall of the aorta normally break down as we age, making the aorta more prone to dilation. In some patients this process is accelerated resulting in early aneurysm formation. We presently do not know the exact mechanisms involved in this process (hence the term idiopathic). Cystic medial degeneration can also be the cause of aortic arch and descending thoracic aneurysms. It rarely is the cause of thoracoabdominal or abdominal aortic aneurysms. Atherosclerosis Atherosclerosis is the term used to describe hardening of the arteries. Smoking, high blood pressure and high cholesterol are the primary causes of atherosclerosis. Atherosclerosis typically results in blockages of arteries that deliver blood to the heart (coronary arteries), the legs (femoral arteries), or the brain (carotid arteries). The damage caused to the aortic wall by atherosclerosis can result in aneurysm formation. Genetic disorders Marfan syndrome is a genetic condition which is transmitted from parent to child that affects the connective tissues throughout the body. The defect is in the gene that makes fibrillin, a major elastic fiber protein found in the wall of the aorta. Nearly all patients with Marfan syndrome develop aneurysms of the ascending aorta and subsequent leakage of the aortic valve. These aneurysms are prone to rupture at smaller sizes when compared to aneurysms of other etiologies. The risk of aortic dissection is likewise significantly increased in Marfan syndrome. Patients with Marfan syndrome may also develop leakage of the mitral valve. Connective tissue abnormalities throughout the rest of the body can result in slender, tapering fingers, long arms and legs, curvature of the spine and eye problems. Certain families without specific genetic disorders may exhibit a strong history of aortic aneurysm formation. If a sibling or parent has been diagnosed with an aortic aneurysm, there may be an increased risk of aortic aneurysm formation in the patient. Aneurysms Associated with Aortic Dissection An aortic dissection results when the inner layer of the aorta separates from the middle layer of the aorta (see above). When this occurs within the ascending aorta it is frequently fatal unless emergency surgery is performed. However, in the descending aorta, an aortic dissection can typically be treated with medications. Nonetheless, the dissection weakens the aortic wall and the aorta is then prone to aneurysm formation. Chronic dissections need to be managed like all other aneurysms and surgery is indicated once a certain size is reached. Aneurysms Associated with Bicuspid Aortic Valve A bicuspid aortic valve is one which contains 2 leaflets instead of the usual three. Such valves are prone to both leakage and stenosis. A bicuspid aortic valve is composed of abnormal connective tissue. This same abnormal tissue also composes the ascending aorta making it susceptible to aneurysm formation. Patients with bicuspid aortic valves frequently have aneurysms of the ascending aorta and surgery on the aortic valve should involve replacement of the aorta should there be any aortic dilation. Other Causes Infection of the aortic wall (bacterial, syphilis, etc.) can rarely result in an aneurysm known as a "mycotic aneurysm." Inflammatory aortic aneurysms are a special type of aneurysm associated with a vigorous fibrotic and inflammatory response and require special surgical interventions. Takayasu's arteritis is an autoimmune inflammatory response which is typically found in Japanese patients and results in aneurysms of the ascending aorta and aortic arch. D) T Any blunt chest trauma can lead to an effusion due to changes in the secretion absorption balance. E) T Need to damage parenchyma, air passages and blood vessels to get an air embolus so I’m not completely sure if this is true. 4. Pharyngeal pouch a. It is a pulsion diverticulum arising from Killians dehiscence b. It appears as a swelling in the anterior triangle of the neck c. Presents as halitosis, regurgitation of food and dysphagia d. Is a congenital diverticulum e. Arises withing the superior pharyngeal constrictor muscle A) T Killans dehisence is located between the thyropharyngeus and the cricopharengeus and occurs due to increased cricopharyngeal pressure B) F Goes posteriorly and to the left C) T & gurgling, aspiration, lump in the neck, asymptomatic D) F Acquired pulsion diverticulaum due to incoordinate swallow and failure of relaxation of the cricopharyngeus E) See A Is posteromedial pulsion diverticulum through Killian's dehiscence Occurs between thyropharyngeus and cricopharyngeus muscles Both form the inferior constrictor of the pharynx Male : female ratio is 5:1 Usually only seen in the elderly Aetiology is unknown but upper oesophageal sphincter dysfunction may be important Clinical features Commonest symptoms are dysphagia, regurgitation and cough Recurrent aspiration can result in pulmonary complications A carcinoma can develop within the pouch Clinical signs are often absent A cervical lump may be present that gurgles on palpation 5. Carcinoma of the breast a. LCIS is more common than DCIS b. T2 lesions measure >5 cm in size c. Inflammatory breast cancer presents as erythema, warmth and edema of the involved breast d. Follow up of breast cancer involves measuring serum levels of Ca 19-9 e. Treatment of locally advanced breast cancer is mastectomy A) B) C) D) E) F other way around F 2cm-5cm T Erythema, Peau d’orange, brawny, oedematous, indurated F For pancreatic, gastric, colonic, ovarian F Majority systemic chemo. Surgery if it becomes operable 6. Nipple discharge a. Bloody nipple discharge is due to fibrocystic disease b. Serous discharge is due to duct papilloma in about ¾ of cases c. Chromophobe adenoma is a microadenoma d. Phenothiazines cause serous discharge e. Treatment of bloody nipple discharge is microdochotomy A) F Discharge is usually serous. Blood suggests malignancy. Other symptoms include lumpiness and discomfort B) T 50% of benign conditions and 90% all together. Unilateral more worrying. C) I can find this anywhere D) T E) F Depends on the aetiology of the discharge. Intraductal papilloma can be treated by excision of the affected segment of breast tissue - microdochectomy 7. Thyroid gland a. Graves disease is common in females b. Subacute (DeQuervains) thyroiditis is an autoimmune disease c. Papillary carcinoma, secondary to radiation, is multifocal d. Men IIA comprises medullary carcinoma, phaeochromocytoma(s) and parathyroid hyperplasia e. Medullary carcinoma is treated by total thyroidectomy and central neck dissection A) T 8:1 ratio B) T post viral autoimmune C) T also early lymphatic spread and poor prognosis D) T E) T MEN Type 1 is also known as Wermer's syndrome after Dr Paul Wermer, who described it in 1954: 1. Parathyroid hyperplasia/tumour causing hyperparathyroidism. 2. Pancreatic islet cell tumours causing hypoglycaemia (insulinoma) and Zollinger-Ellison syndrome (gastrinoma). 3. Pituitary adenoma which may cause pituitary hormone excess. The causative mutation is in the menin gene which encodes a nuclear protein that is believed to act as a tumor suppressor. Most cases of multiple endocrine neoplasia type 1 are inherited in an autosomal dominant pattern. MEN syndrome types 2 and 3 have their basis in molecular genetics. Individuals can be tested for this genetic disorder reliably even when asymptomatic. The mutation is in the RET oncogene. Most cases of multiple endocrine neoplasia types 2 and 3 are inherited in an autosomal dominant pattern. Type 2 is also known as Sipple syndrome (after the American Dr John H. Sipple, who described it in 1961) and used to be called type 2A: 1. Medullary carcinoma of the thyroid which is associated with increased calcitonin secretion. A test for elevated calcitonin should be done after pentagastrin injection and/or calcium infusion, to ensure that all affected patients are detected. 2. Pheochromocytoma 3. Parathyroid hyperplasia/tumour causing hyperparathyroidism. 8. Regarding chronic peptic ulcers a. Type I ulcers occurs along the lesser curvature of the stomach b. Type III ulcers occur at or just proximal to the pylorus c. Peptic ulcers that bleed erode the right gastric artery d. Gastrojujenocolic fistula occurs after gastrectomy and Billroth II anastomosis e. Post gastrectomy cancer is associated A) T B) T Type I consisted of those cases in whom the ulcer was situated to the left of and above the gastric angulus (the angulus being defined as the lowest point of the lesser curvature), without macroscopic abnormalities of the prepyloric region, the pylorus or duodenum; these cases were associated with a low level of acid secretion and possibly hyposecretion of mucus. Type II consisted of those cases in which a gastric ulcer to the left of the angulus was associated with, and probably secondary to, an ulcer or its scar in the pylorus or duodenum; these patients were moderate and sometimes hypersecretors of acid. Type III included all gastric ulcers on or near the pylorus, and might be combined with a duodenal ulcer or a Type II gastric ulcer proximally; these patients usually had hypersecretion of acid. Type III was subdivided as follows: (1) ulcers within one inch (2.54 cm) of the pylorus, called true prepyloric ulcers; (2) ulcers to the right of the angulus but further than 2.54 cm from the pylorus, called "other antral" ulcers. It was concluded that gastric ulcers near the pylorus and those occurring with a duodenal ulcer should be looked upon as a disease of acid hypersecretion; in these cases there was a marked blood group O predominance, the ulcers nearest the pylorus carrying the highest proportion of blood group O. Gastric ulcers in the body of the stomach, occurring in patients in whom the duodenum was normal, were usually characterized by acid hyposecretion; in these patients there was no evidence of group O preponderance, but in fact an excess of blood group A. The findings showed that the pathogenesis differed in different types of gastric ulcers. C) F Bleeding ulcer has not necessarily eroded through a major vessel. Mostly cystic artery and slenic artery. Gastroduodenal if duodenal perf D) F (Christian Albert Theodor Billroth, 1829 - 1894, German surgeon), subtotal gastrectomy and gastroenterostomy linking the gastric pouch to the jejunum distal to the ligament of Treitz. A looptype gastrojejunostomy connects the jejunum to the stomach in one continuous segment. The configuration can be a right to left or antiperistaltic loop (Fig.1) in which the afferent, or that part of the bowel bringing bile and bowel contents toward the stomach, is first anastomosed to the right or lesser curvature portion of the stomach and is then carried across to the left side The colic bit of this looks wrong to me since the colon isn’t involved E) T Postgastrectomy gastritis is gastric atrophy developing after partial or subtotal gastrectomy (except in cases of gastrinoma). Metaplasia of the remaining corpus mucosa is common. The degree of gastritis is usually greatest at the lines of anastomosis. Several mechanisms are responsible: bile reflux, which is common after such surgery, damages the gastric mucosa; loss of antral gastrin decreases stimulation of parietal and peptic cells, causing atrophy; and vagotomy may result in a loss of vagal trophic action. There are no specific symptoms of gastritis. Postgastrectomy gastritis often progresses to severe atrophy and achlorhydria. Production of intrinsic factor may cease with resultant vitamin B 12 deficiency (which may be worsened by bacterial overgrowth in the afferent loop). The relative risk of gastric adenocarcinoma appears to increase 15 to 20 yr after partial gastrectomy; however, given the low absolute incidence of postgastrectomy cancer, routine endoscopic surveillance is probably not cost effective, but upper GI symptoms or anemia in such patients should prompt endoscopy. 9. Crohn&#8217;s Disease a. Is predominantly a transmural disease b. Characteristic microscopic lesions are noncaseating granulomas c. Bloody diarrhea is the most frequent presentation d. Peri-anal disease is an infrequent presentation e. Toxic dilatation of the colon is a common finding A) B) C) D) E) T T in 50% of cases F UC. P/C episodic diarrhoea, abdominal pain, tenderness, lassitude,fever F Common ¼ with small bowel disease, ¾ with large bowel disease ?F Less common than in UC 10. Carcinoid tumour a. The most common location of a carcinoid tumour is the terminal ileum b. Appendiceal carcinoids frequently metastasise c. Urinary 5-HIAA is the most reliable test to confirm the diagnosis of carcinoid tumour d. Octreotide can successfully control the symptoms of diarrhea and flushing e. 5-HIAA is a metabolite of tyrosine A) F Mostly appendix. B) F Rare C) T D) T E) F Secrete 5HT, active amines and peptides. Liver mets rare. Carcinoid syndrome when metastasize because no longer inactivating. Leads to flushing, diarrhoea, bronchoconstriction, wheezing, red/purple discolouration of the face, pulmonary stenosis Tests. Urinary breakdown products of 5HT Treatment: Remove tumour, excise, enucleate or dearterialise Medical Octreotide 11. Appendicitis a. The commonest location of the appendix is in the pelvis b. Psoas sign is elicited by flexion of the right hip c. Is associated with a fecolith in 90% cases d. Laparoscopic appendicectomy has been shown to be superior to open appendicectomy for acute appendicitis e. Rovsigns sign is elicited by pressing in the left iliac fossa causing pain in the right iliac fossa A) F 74% retrocaecal, 21% Pelvic, 1.5 % subcaecal, 2% paracaecal, 5% Postilial, 1% preileal B) T C) F D) T I think E) T Prospective randomised multicentre study of laparoscopic versus open appendicectomy. Hellberg A, Rudberg C, Kullman E et al. Br J Surg 1999; 86: 48-53. Open appendicectomy is the 'gold standard' for the treatment of acute appendicitis. Although it is a generally safe operation, postoperative complications occur in about 10% of patients. Laparoscopic appendicectomy was first described in 1983. Reports of early studies were equivocal with few studies evaluating analgesic requirements and the length of hospital stay. The aim of this study was to compare laparoscopic with open appendicectomy with special emphasis on the postoperative recovery period. A total of 523 patients were randomised but because of withdrawals the outcome in 500 patients was reported; 244 in the laparoscopic and 256 in the open group. Patients undergoing laparoscopic appendicectomy recovered quicker than those undergoing open surgery but there was no difference in the duration of sick leave taken (11 vs. 14 days). Postoperative pain (at 24 hours, 7 and 14 days) was less after laparoscopic surgery and a functional index at one week after operation was more favorable in this group. Operating time was longer in the laparoscopic group ( 60 vs. 35 mins. p<0.01). Hospital stay and complications did not differ between the two group. In total 30 (12%) of laparoscopic procedures had to be converted to an open operation. It was concluded that laparoscopic appendicectomy is as safe as open appendicectomy and has the advantage of a more rapid recovery. advantages including faster recovery time, shorter hospital stay, lower risk of post operative infection, and smaller scars. 12. Colorectal cancer a. Adenomatous polyps account for more than 90% colorectal cancers b. High fibre diet, calcium and selenium have a cytoprotective effect c. Colonic cancer is part of Lynch II Syndrome d. FAP is inherited as an autosomal recessive pattern e. HPNCC is autosomal dominant A) F B) T From an epidemiological standpoint, there have been many studies linking calcium intake to colon cancer risk. Significant reductions in risk have been shown for the consumption of milk, dietary calcium and dairy products in general. Supplemental calcium in the diet or drinking water has been reported to decrease the colonic epithelial hyperproliferation induced by bile and fatty acids, enteric resection, a nutritional stress diet, and to suppress induction of the tumor-promotion enzyme ornithine decarboxylase. Calcium has also demonstrated an inhibitory effect on experimental colon carcinogenesis. Calcium's effects on epithelial cells have demonstrated decreased proliferation and induced cell differentiation with increasing levels of calcium in vitro, similar in vivo effects in rodent and human colon, and decreased carcinogen-induced colonic tumor formation in rodents.In human subjects at increased risk for colon cancer, oral calcium supplementation significantly reduced colonic epithelial cell proliferation in most of the studies, including four randomized clinical trials. Treatment with calcium supplements for 4 years appears to provide protection against recurrent colorectal adenomas -- the type of polyp that leads to cancer -- for up to 5 years after the supplements are stopped, new research shows. Beyond that point, however, no apparent effect is seen. Past epidemiological studies on selenium and colorectal cancer have had mixed results. However, a statistically significant reduction of colorectal cancer as secondary endpoint was noted in the Nutritional Prevention of Cancer trial (relative risk - 0.58) as was an overall reduction in colorectal adenomas. This was a doubleblind, placebo-controlled, clinical trial. C) T Hereditary nonpolyposis colorectal cancer (HNPCC) is subdivided into (1) Lynch syndrome I (site-specific colonic cancer) and (2) Lynch syndrome II (colonic cancer in association with other forms of cancer, particularly carcinoma of the endometrium and ovary, but also cancer of the pancreas) D) F Dominent. APC gene Chr 5. 25% are sporadic new germ line mutations. >100 polyps E) T 5% colorectal cancer. Increase in endometrial, gastric, overian, upper urinary tract and small intestine malignancy hMSH2 on chr 2p hMLH1 on chr 2q 13. Cholelithiasis a. Biliary colic occurs only with stones in the common bile duct b. Merrizi&#8217;s syndrome is associated with cholestatic jaundice c. Charcot&#8217;s triad includes jaundice, rigors and palpable gallbladder d. Chenodeoxycholic and ursodeoxycholic acid are used for dissolution of cholesterol stones e. For symptomatic cholelithiasis laparoscopic cholecystectomy is the operation of choice A) Most commonly hartmann’s pouch B) T Mirizzi's syndrome is a rare cause of acquired jaundice. It is caused by chronic cholecystitis and large gallstones resulting in stenosis of the common bile duct. Multiple and large gallstones can reside chronically in the Hartmann's pouch [1] of the gallbladder, causing inflammation, necrosis, scarring and ultimately fistula formation into the adjacent common bile duct (CBD). As a result, the CBD becomes obstructed by either scar or stone, resulting in jaundice. Mirizzi syndrome has no consistent or unique clinical features that distinguish it from other more common forms of obstructive jaundice. Symptoms of recurrent cholangitis, jaundice, right upper quadrant pain, and elevated bilirubin and alkaline phosphatase may or may not be present. Acute presentations of the syndrome include pancreatitis or cholecystitis. CT scan or ultrasonography usually make the diagnosis. Often, ERCP is used to define the lesion anatomically prior to surgery. The treatment of choice is surgical excision of the gallbladder, and reconstruction of the common hepatic duct and common bile duct. C) F Pain Pyrexia Jaundice. Courvoisier- Palpable gallbladder & jaundice unlikely due to stone D) T Rarely used now. Used if unimpaired gallbladder fxn and small or medium sized radiolucent stones and mild symptoms and not amenable to other treatment. Also for prevention of recurrent biliary tract stones post cholecystectomy. 14. Pancreatitis a. Foxs sign is discoloration of groins b. Alcohol is an aetiological factor for the development of acute pancreatitis c. A Ransons criteria of 7-8 is associated with mortality of 50% d. Steatorrhea is associated with acute pancreatitis e. A chain of lake appearance is pathognomonic of chronic pancreatitis A) T Cullen’s discolouration around umbilicus. Grey-turners flank discolouration B) T GET SMASHED C) F The Ranson criteria and other severity scoring systems, e.g. Glasgow, APACHE II, enable early diagnosis of severe acute pancreatitis. This can be defined as the presence of three or more of the following criteria within 48 hours of admission: age above than 55 years blood glucose above 10 mmol/L - no history of diabetes white cell count above 15 x 10^9 / L LDH above 600 IU/L aspartate transaminase above 200 u/L corrected calcium less than 2.0 mmol/L blood urea above 16 mmol/L - no improvement with intravenous fluids decreasing haematocrit arterial pO2 less than 8 kPa (60 mm Hg) metabolic acidosis serum albumin less than 32 g/L N.B. the serum amylase value is not one of the criteria. The mortality per postive criterion: NUMBER OF POSITIVE CRITERIA o 0-2 <5% mortality o 3-4 20% mortality o 5-6 40% mortality o 7-8 100% mortality D) F more associated with chronic due to the development of pancreatic insufficiency. E) This is something to do with strictures seen within the pancreas. Not sure if its pathognomonic. 15. Vascular a. The mortality rate of ruptured AAA is 40% b. Ultrasound can reliably meaure the size and site of AAA c. Ruptured AAA may present as pain in the renal angle d. Surgery is recommended for patients with AAA > 6cm diameter e. Spinal cord ischemia is an infrequent complication A) F It way higher than this. Between 80-90% but figure vary B) F US good but only accurate to within .5 cm C) T Can present with all sorts of weird and wonderful and sometimes vague abdominal pain. D) F 5cm in women. 5.5cm in men E) T a. Clamping aorta above renal arteries >20-30 minutes, or ligation of lower vessels puts cord at risk b. AAA repair has 5-20% risk of neurological deficits c. Aneurysmal aortic dissection also causes spinal ischemia – grey matter ischemia, white matter adequately supplied by longitudinal anastomotic network 16. Peripheral vascular disease a. Normal ankle-brachial ratio is <0.75 b. Thromboendarterectomy is the operation of choice for aortoiliac occlusive disease c. Rest pain is relieved by elevation of the foot d. Impotence is a common phenomenon associated with occlusive disease of the distal aorta and iliac vessels e. Sympathectomy provides good symptomatic relief of rest pain A) Healthy 1. IC 0.5-0.9. Critical <0.5 B) Rarely done. PTA or aortobifem C) F raising leg decreases flow to the leg further making the pain worse D) T Inflow Disease: Aortoilliac Occlusive Disease Also known as Leriche's Syndrome, Bilateral leg diminished pulses throughout Slow wound healing legs, Impotence E) T In some cases, sympathectomy, which removes neurogenic vasoconstriction, can be very helpful and should be offered to selected patients with severe disease and those who are not candidates for revascularization. 17. Paediatric surgery a. Hirschprungs disease is caused by absence of ganglion cells in the Auerbachs plexus b. High imperforate anus is treated by colostomy followed by sacroperineal or abdominosacral pull through of the proximal colon c. Congenital hypertrophic pyloric stenosis is common in female infants d. Meckels Diverticulum is best diagnosed by 99m Technetium scan e. Idiopathic intussussception occurs in a 6 to 9 month old infant A) T Hirschsprung's disease is the result of a. congenital aganglionosis of Auerbach's. plexus at the muscularis layer of the distal colon B) T Surgery depends on the type of imperforate anus defect.With a high imperforate anus, a colostomy (to divert the path of stool) is usually done. The infant with a high lesion is therefore given time to grow until definitive repair can be done with a pull-through operation (in which the rectum is "pulled down" and sewn into a newly-made anal opening in the perineum). After surgery, the newly-formed anus needs to be dilated regularly for several months until a soft, mature scar is obtained. The colostomy can then be closed. C) F boys 5 times more commonly than girls D) T Regarded as the gold standard E) T 6 to 36 months is an accepted timeframe 18. Orthopedics a. Colles fracture results a fall on an outstretched hand with the wrist in flexion b. Fractured ribs invariably cause a pneumothorax c. The leg is externally rotated in fracture of neck of femur d. Fracture of the humeral shaft may cause injury to the radial nerve e. Fat embolism following multiple fractures is associated with petichial skin rash A) F A Colles' fracture is a fracture of the distal radius bone. It is named after Abraham Colles (17731843), an Irish surgeon who first described this in 1814.The fracture is most commonly caused by people falling forward onto a hard surface and breaking their fall with extended, outstretched hands - falling with wrists flexed would lead to a Smith's fracture. It usually occurs about an inch or two proximal to the radio-carpal joint with posterior and lateral displacement of the distal fragment resulting in the characteristic dinner fork like deformity. Colles fracture is common in people with osteoporosis, second only to vertebral fractures. B) F There would be a hell of a lot of people going around with air in their chest if this was the case. C) T On inspection, the injured led lies in a position of external rotation and there is shortening of the leg. The attachment of the capsule to the distal fragment prevents excessive external rotation of the leg. On palpation, there is tenderness over the anterior and lateral aspects of the hip joint. The greater trochanter is elevated on the injured side. All movements are extremely painful except in the rare case of an impacted type of fracture. D)T Most humeral fractures near the shoulder occur at the surgical neck. Mid shaft humeral fractures are almost always the result of direct trauma (less often due to a fall), are either transverse or oblique, and are displaced due to muscular action. Radial nerve injury is the main complication. E) T The post-traumatic fat embolism syndrome is a multisystem disorder characterized by pulmonary and neurologic dysfunction, pyrexia, and a petechial rash 19. Urology a. The majority of bladder tumours are squamous cell carcinomas b. Renal cell carcinoma is always treated with adjuvant chemotherapy c. The most common urinary calculi are triple phosphate stones d. Testicular tumours commonly metastasize to the groin lymph nodes e. Fracture of the bony pelvis leads to injury to the membranous urethra A) F Transitional cell B) F Only used in high risk. Stage I Renal Cell Cancer Treatment of stage I renal cell cancer may include the following: Surgery (radical nephrectomy, simple nephrectomy, or partial nephrectomy). Radiation therapy as palliative therapy to relieve symptoms in patients who cannot have surgery. Arterial embolization as palliative therapy. A clinical trial of a new treatment. Information about ongoing clinical trials is available from the NCI Web site. Stage II Renal Cell Cancer Treatment of stage II renal cell cancer may include the following: Surgery (radical nephrectomy or partial nephrectomy). Surgery (nephrectomy), before or after radiation therapy. Radiation therapy as palliative therapy to relieve symptoms in patients who cannot have surgery. Arterial embolization as palliative therapy. A clinical trial of a new treatment. Information about ongoing clinical trials is available from the NCI Web site. Stage III Renal Cell Cancer Treatment of stage III renal cell cancer may include the following: Surgery (radical nephrectomy). Blood vessels of the kidney and some lymph nodes may also be removed. Arterial embolization followed by surgery (radical nephrectomy). Radiation therapy as palliative therapy to relieve symptoms and improve the quality of life. Arterial embolization as palliative therapy. Surgery (nephrectomy) as palliative therapy. Radiation therapy before or after surgery (radical nephrectomy). A clinical trial of biologic therapy following surgery. This summary section refers to specific treatments under study in clinical trials, but it may not mention every new treatment being studied. Information about ongoing clinical trials is available from the NCI Web site. Stage IV and Recurrent Renal Cell Cancer Treatment of stage IV and recurrent renal cell cancer may include the following: Targeted therapy alone or after biologic therapy. Biologic therapy alone or after surgery (nephrectomy) to reduce the size of the tumor. Arterial embolization as palliative therapy to relieve symptoms and improve the quality of life Radiation therapy as palliative therapy to relieve symptoms and improve the quality of life. Surgery (nephrectomy) as palliative therapy. Surgery (radical nephrectomy, with or without removal of cancer from other areas where it has spread). A clinical trial of chemotherapy. C) Calcium oxalate is the commonest. Also calcium phosphate, triple phosphate, urate and cystine D) F To para-aortic more commonly. To groin if invade scrotal skin. E) T The membranous urethra is prone to injury from pelvic fracture because the puboprostatic ligaments fix the apex of the prostate gland to the bony pelvis and thus cause shearing of the urethra when the pelvis is displaced. 20. Skin cancer b. Kaposis Sarcoma is a tumour of vascular endothelial origin c. Xeroderma Pigmentosa is an autosomal recessive disease d. Sunlight exposure is the principle cause of basal cell carcinoma and squamous cell carcinoma e. Superficial spreading melanoma has the worst prognosis f. Squamous cell carcinoma is not sensitive to radiotherapy A) T Kaposi sarcoma is a cancer of blood vessels that was considered very rare before the start of the AIDS pandemic. It is now the most frequent cancer to develop in people with AIDS, affecting about 20% overall. Kaposi sarcoma is associated with: Infection with human herpes virus 8 (KSHV) in men who have sex with men. It can also occur in heterosexuals. Data is emerging that non-sexual modes of transmission can occur. Genetic factors Hormonal factors B) T inherited inability of the skin to repair DNA damage from ultraviolet light. A sunburn that does not heal following minimal sun exposure Blistering following minimal sun exposure Cutaneous telangiectasia Increasing irregular pigmentation of the skin Crusting of the skin Scaling of the skin Oozing raw skin surface Discomfort when exposed to bright light (photophobia ) Neurologic changes are sometimes noted B) T C) F Four Types of Melanoma 1. Superficial spreading melanoma (about 70% of diagnosed cases) the most frequent melanoma types, begins from primary radial growth, preceding the invasion. Better prognosis 2. Nodular melanoma (about 15% of diagnosed cases) bad prognosis because of invasive growth. 3. Lentigo maligna melanoma (about 10% of diagnosed cases) 4. Acral lentiginous melanoma (about 5% of diagnosed cases) most widespread form at black people, located mostly on feet, mycoses, nail beds; disease is similar to precancerous melanoma, but has more aggressive current. D) T The treatment for a SCC depends upon its type, its size and location, the number to be treated, and the preference or expertise of the doctor. Excision The lesion is cut out and the skin is stitched up. This is the most common treatment for invasive SCC. Cryotherapy Dermatologists sometimes use liquid nitrogen with a special technique. This may be suitable for small or flat lesions of in situ SCC or thickened solar keratoses. Shave, curettage, & cautery (and other similar techniques) Many skin cancers can be successfully treated by shaving off or scraping out the lesion then cauterising the base. The wound usually heals rapidly without the need for stitches. More complex surgery Patients with larger lesions or one in a difficult site may be referred to a dermatologist or plastic surgeon, who may create a flap or graft to repair the defect after excision. Mohs micrographic surgery may be necessary. Radiotherapy - Radiation treatment can be used for some skin cancers, usually on the face. may be added after surgery of a high-risk SCC. It can add measurably to the cure rate. It is probably used less often than it should be. Occasionally, radiation is used as the sole treatment in inoperable tumors, or in those that have already spread. 5-Fluorouracil cream This cytotoxic cream applied for several weeks often clears in situ SCC. It causes a vigorous skin reaction that may ulcerate. Sometimes the lesion recurs months or years later, when it may be treated the same way or by another method. Imiquimod Imiquimod is an immune response modifier in a cream base. Applied five times weekly for six to sixteen weeks, it will clear most patches of in situ SCC but is not yet registered for this purpose. Photodynamic therapy Photodynamic therapy (PDT) refers to treatment with a photosensitiser (a porphyrin chemical) that is applied to the affected area prior to exposing it to a strong source of visible light. The treated area develops a "burn" and then heals over a couple of weeks or so. EXAM 5: Unknown year, UCC. Why 1. Regarding Gastric Surgery a. Early postprandial dumping is due to hypoglycemia b. Recurrent ulcers after treatment of duodenal ulcer are secondary to excessive acid production c. Patients may develop a diamorphic blood picture d. Blind loop syndrome is common in antecolic anastomosis A – False Late postprandial dumping is due to hypoglycaemia. Early postprandial dumping is due to shift of osmotic fluid into the jejunum which can occur following a billroth type procedure. B – True C – True Iron deficiency occurs due to loss of hypochloric acid and B12 deficiency secondary to loss of intrinsic factor production. The net result is a combination of a microcytic anaemia and megaloblastic anaemia. D – False A polya gastrectomy is more likely to cause a blind loop syndrome due to the use of a roux en Y procedure. The duodenal stump is oversewn (leaving a blind loop). A Billroth procedure is simply a partial gastrectomy and re-anastomosis. 2. Gastrointestinal polyposis syndrome a. Hereditary nonpolyposis colorectal cancer is autosomal dominant b. Colorectal cancers develop before 40 years of age in familial adenomatous polyposis (FAP) c. Polyps in Peutz-Jeghers Syndrome are hyperplastic d. Turcotts syndrome is gastrointestinal polyps with CNS tumors e. Hereditary nonpolyposis colorectal cancer accounts for <5% of cases A – True Lynch syndrome, previously called hereditary nonpolyposis colorectal cancer, is characterized by an autosomal dominant mode of inheritance of colorectal cancer and is the most common form of hereditary colon cancer, comprising approximately 5% of all colorectal cancers. B – True The mean age of diagnosis of colorectal cancer in FAP is 40 years of age. FAP is caused by inheritance of a germ line mutation in the APC gene. FAP is characterized by the appearance of hundreds to thousands of adenomas of the colon during adolescence (average age at polyp formation is approximately 15 y) and a nearly 100% risk of colon cancer C – False Peutz-Jeghers syndrome is an autosomal dominant inherited disorder characterized by intestinal hamartomatous polyps in association with mucocutaneous melanocytic macules D – True A rare, hereditary syndrome, characterized by brain tumors (glioblastoma, astrocytoma, or spongioblastoma) associated with colonic adenomatous polyposis. The polypi vary in number from hundreds to thousands and in size; occasionally they are found in the stomach and small intestine. In the fourth and fifth decades of life they are liable to become malignant. Other features include Cafe-au-lait spots, cutaneous port wine stain, diarrhoea, as well as focal nodular hyperplasia. Inheritance is autosomal recessive. The symptoms are most often in the second decade of life. Turcots syndrome has been divided in three groups depending on the number and character of the colonic polyps E – True 3. Salivary glands a. Pleomorphic adenoma is the most common benign tumour of the submandibular gland b. Mikulic’s Syndrome refers to the bilateral enlargement of lacrimal and salivary glands c. Sialothiasis is almost exclusively a problem of the submandibular gland d. Incisional biopsy is performed in all salivary gland tumours e. Lingual nerve can be damaged in surgery on submandibular gland A – True Occurs most frequently in the parotid gland. Propensity for recurrence if not removed with surrounding cuff of tissue. It accounts for 90% of parotid tumours in adults. Other benign tumours include Warthins tumour and haemangiomas. Warthins tumour is almost exclusive to the parotid gland; it causes a smooth swelling in the tail of the gland that feels cystic. The malignant tumours of the salivary glands are adenoid cystic carcinoma, acinic cell carcinoma and muco-epidermoid tumours. B – True This is a variant of Sjogrens Syndrome. C – True 80% of salivary calculi arise in the submandibular gland due to the mucoid nature of its saliva, which can become inspissated. Calculi can form in the parotid gland also. The flow of saliva from the affected gland becomes obstructed which results in painful swelling of the gland during salivation. The swelling usually resolves over an hour or thereabouts. Confirm by X-ray, as most are radio opaque. Calculi arises distal in the duct can be easily removed under local anaesthesia through the mouth. Stones arsing more proximal in the duct can often require submandibular gland excision. D – False Risk of neuropraxia, axontemesis or neurotemesis. E – True The submandibular gland can be excised for calculus disease or chronic infection. The gland is approached externally and care must be taken not to damage the marginal mandibular branch of the facial nerve or the lingual nerve. 4. Hernias a. Direct inguinal hernias pass through internal ring b. A femoral hernia is the most common hernia in females c. Testicular atrophy may occur after inguinal hernia repair d. Inguinal hernias in children are treated by hernioraphy e. Littres hernia contains Meckel’s diverticulum A – False A hernia is an abnormal protrusion of all or part of a viscus through a defect in the wall of the cavity in which it is normally contained. Inguinal hernias can be split into direct and indirect. Indirect are more common in children especially premature male infants due to persistence of the processus vaginalis. Due to the persistence of the communication between the abdominal cavity and scrotum, visceral herniation can occur through the internal ring and external ring of the inguinal canal into the scrotum. In the differentiation of an inguinal – scrotal mass you cannot get above an indirect hernia. Direct hernias conversely are more common in elderly men. A visceral protrusion occurs through the region known as Hesselbachs triangle. This is medial to the inferior epigastric vessels. B – False Femoral hernias are more common in females however the commonest hernia in females still remains inguinal. C – True A recognised intraoperative complication is injury to the spermatic vessels resulting in atrophy or acute necrosis of the testes. D – True E - True 5. Abdominal Aortic Aneurysms a. Surgery is recommended for patients with AAA size > 6 cms b. 90% arise below renal arteries c. Ischemia of colon is common d. Mortality rate of ruptured AAA is 25% e. Blue toe syndrome occurs in association with AAA A – True An aneurysm is a permanent localised abnormal dilatation of a blood vessel. AAA occur in 5% of people over 65 years old. M: F ratio = 6:1. The majority are caused by atherosclerotic disease. 5% are inflammatory aneurysms. The risk factors are atherosclerosis, hypertension, smoking, male gender, advanced age and connective tissue disorders. Most are asymptomatic and are picked up during routine physical exam. The classic triad of a ruptured AAA is abdominal pain, pulsatile abdominal mass and hypotension. Aneurysms grow by approximately 3mm / year. The risk factors for rupture are large diameter, increasing size, recent expansion, hypertension, symptomatic and COPD. At 5cm the risk of rupture is 4%. At 5-7cm the risk of rupture is 7% per year and greater than 7cm, the risk of rupture is approximately 20% / year. Surgeons intervene from 5.5cm and greater. B – True 90% are infrarenal in origin.20% of patients with an AAA also have a peripheral aneurysm. C – True Colonic ischaemia can occur post repair of an AAA as the inferior mesenteric artery is often sacrificed. If the collaterals are insufficient the patient will have colonic ischaemia. The signs of colonic ischaemia are heme positive stool or bright red blood per rectum, diarrhoea and abdominal pain. The study of choice is colonoscopy. The ischaemia typically manifests in the first week. The treatment of necrotic sigmoid colon from colonic ischaemia is resection of the necrotic colon, hartmanns pouch or mucous fistula and end colostomy. D – False If two patients present to hospital with a ruptured AAA, one will go out the back door and the other the front door! 50% mortality. Elective repair has a 4% mortality rate. E – True As an AAA has a mural thrombus associated with it, fragments of the plaque can embolise distally and cause a so-called thrash foot. 6. Vascular a. Carotid atheromatous disease is the commonest cause Of strokes in the western world b. Varicose veins are treated by femoral-popliteal bypass graft c. Rest pain is relieved by elevation of the foot d. Normal ABI is greater than 0.90 e. Cervical rib may present with wasting of thenar muscles A – False The commonest cause of CVA in the world is cerebral infarction, which can be secondary to a thrombus or an embolism. B – False Varicose veins can be treated conservatively or surgically. Surgical means include high saphenous ligation, avulsion of varicosities and vein stripping. C – False Rest pain is suggestive of critical limb ischaemia secondary to chronic arterial insufficiency of the lower limb. The pain when present at night is relieved by hanging the affected leg over the edge of the bed, or else by sleeping while sitting in a chair. Rest pain when present for two weeks requiring analgesia is an indication for operative intervention. D – False Normal ABPI is 1, intermittent claudication = .9 to .6, rest pain = .6 to .3 E – False A cervical rib may impact the lower roots of the brachial plexus, C8 and T1. This causes in addition to unequal radial pulses, a palpable rib in the neck and potential distal emboli, wasting of the hypothenar eminence. 7. Orthopedics a. Smith’s fracture results in volar angulation of the radius b. A fractured neck of femur results in lateral rotation of the lower limbs c. The radial nerve is injured in fracture of neck and humerus d. Bennett’s fracture involves distal end of radius e. Supracondylar fracture may cause vascular complications A – True This is an uncommon fracture that results from falling on the dorsum of the hand. It is known as a reverse colles fracture – distal radial fracture with volar angulation as against dorsal angulation, which is colles fracture. B – True Fractures of the proximal femur occur in elderly females from minor trauma. Most have type 2 osteoporosis. The history is that the patient tripped over the carpet or tripped over the pavement. Now they have pain in the hip. Shortening, adduction and external rotation occurs. The movements are painful and weight bearing is usually impossible. Beware of hypothermia. C – True Yes the radial nerve courses through the spiral groove at the posterior aspect of the humerus. Net result is wrist drop. D – False Bennett’s fracture is a fracture dislocation of the base of the first metacarpal with disruption of the carpometacarpal joint. E – True Supracondylar fractures of the humerus can result in forearm compartment syndrome. This is increased pressure in an osteofacial compartment that can lead to ischaemic necrosis. The final sequelae of forearm compartment syndrome is Volkmanns contracture. This is contracture of the forearm flexors from replacement of dead muscle with fibrous tissue. 8. Fluid and electrolyte balance a. Insulin and glucose infusion may be used to treat hyperkalemia >6.5 mg/L b. Short gut syndrome doesn’t predispose to carcinoma c. Patients on IV fluids require 1mmol/kg body potassium per day d. Hyponatremia should be corrected by large volumes of hypertonic saline e. Adult burns victims require 2L fluid in 24 hours A – True An elevated serum potassium of 6.5mg/L is an emergency. Hyperkalaemia and its effects can easily be observed on the ECG. Tall tented T waves, widened PR interval, widened QRS, flattening of the P waves, sine waves appearance and V Fib. To prevent this we need to decrease the potassium level. Firstly stabilise the cardiac membrane by giving 10ml of 10% calcium gluconate repeating as necessary. Calcium resonium is given. 20u of ActRapid in 50ml of 50% glucose is given to force the potassium into the cells. Salbutamol 2.5mg can also be considered. Once the patient is stabilised treat the cause of the hyperkalaemia such as acute renal failure, crush injury, injudicious fluid replacement etc. B – True All short bowel syndrome refers to is malnutrition secondary to less than 100cm of viable small bowel. C – True A simple fluid regime is 3L per day. 1L of .9%NaCl. This contains your daily sodium requirement. Two litres of 5% dextrose. Add 20mmol of KCL to each bag and infuse it at 125ml / hour. D – False Rapid correction of hyponatraemia by high doses of hypertonic saline is asking for trouble. The net movement of water from the intracellular compartment to the extracellular compartment results in CPM or central pontine myelinolysis. E – False The fluid requirements for a burns victim is calculated using the parkland formula. 4 x % burns x weight (kg). This is the quantity of fluid that has to be replaced using .9%NaCl over a 24-hour period. Half of this is given in the first 8 hours the remainder over 16 hours. 9. Regarding sinuses and fistulas a. High output fistulas are characterized by loss of intestinal fluid in excess of 200 mL/24 hours b. Pilonidal sinus is premalignant c. An example of congenital fistula is thyroglossal cyst d. Inefficient or nondependent drainage is one of the factors leading to persistence of an abscess e. A chronic subareolar abscess leads to a mamillary fistula A – False A fistula is an abnormal connection between two epithelial lined surfaces. A high output fistula is characterised by > 500ml/day. The predisposing factors and factors that maintain the patency of a fistula are: High ouput, intestinal destruction, short segment fistula, foreign body, radiation, infection, epithelization, neoplasm and distal obstruction. B – False A sinus is a blind ending tract lined by granulation tissue that opens onto an overlying epithelial lined surface. This chronic infection is caused by penetration of hairs into the skin and subcutaneous tissues. Infection leads to pilonidal abscesses. The sinus leads to a cavity filled with hair and granulation tissue. Common sites include posteriorly in the midline over the sacrococcygeal area and natal cleft. Also can occur between fingers in hairdressers. C – False A thyroglossal cyst is an embryological remnant of the thyroid gland that present as a cystic midline swelling generally in a patient < 20 years old. It can occur anywhere from the foramen caecum of the tongue to the thyroid gland. It moves on swallowing and tongue protrusion. It is harmless but generally is excised due to its propensity to become infected. D – True An abscess is a localised collection of fluid / pus within a tissue. Abscesses wall themselves off with granulation tissue. The treatment of an abscess is to incise and drain. ‘If there is pus let it out’. On of the factors, which lead to the persistence of an abscess – chronic abscess is failure to remove the inciting stimulus. E - True 10. Carcinoma of the breast a. T3 breast lesion is >5 cm in dimension b. Tamoxifen should be prescribed for life to patients with breast cancer c. Axillary lymph node involvement is a weak predictor of outcome d. Comedo DCIS is associated with low recurrence rate e. Breast cancer rarely metastasizes to bone A – True This is not a real question. Professor Redmond specifically said that he doesn’t know the TNM staging off the top of his head. B – False Stupid question. Expose a woman to an increased risk of endometrial carcinoma, DVT, PE – come on!!! C – False Axillary lymph node involvement ipsilaterally instantly confers a 50% survival chance. No lymph nodes = 80% five year survival. D – False Comedo DCIS is the most aggressive histologic subtype. It is associated with a risk of subsequently developing ductal carcinoma in the same breast E - False 11. Pancreatitis a. Cholelithiasis is the commonest cause b. Cullen’s sign is associated with bruising in flanks c. Steroids are not associated with acute pancreatitis d. The treatment of sterile necrotizing pancreatitis is always surgery e. A pseudocyst should be drained within 2 weeks of the acute attack A - True Biliary disease account for 40% of cases of acute pancreatitis. The risk of pancreatitis is inversely proportional to the size of the stone. It’s lodgement at the sphincter of oddi is postulated to cause a rise in intra-ductal within the pancreas, blocking the drainage of the pancreatic juices into the duodenum. This rise in pressure may damage the ductal epithelial lining allowing pancreatic autodigestion. Interestingly biliary microlithiasis is thought to be responsible for 70% of idiopathic pancreatitis. The other causes of pancreatitis can be remembered from the mneumonic ‘I Get Smashed’= Idiopathic, Gallstones, Ethanol, Trauma, Steroids, Mumps (Viral agents), Autoimmune, Scorpion stings, Hyperlipademia, Hpercalcaemia, ERCP, Drugs (Thiazides, steroids, asparginase etc). B – False Cullen is the aptly called ‘umbilical black eye’. Grey Turners sign is bruising in the flanks. The aetiology of Grey Turners Sign is retroperitoneal haemorrhage tracking / dissecting through tissue planes. Cullens sign results from haemoperitoneum. These are rare signs. Also if present they are diagnostic of a sub category of pancreatitis namely severe necrotizing pancreatitis. C – False ‘S’ in the mneumonic. Drug induced pancreatitis is a rare occurrence. D – False Surgery is required in infected necrotizing pancreatitis to remove non-viable tissue. In sterile necrotizing pancreatitis there is always the fear of superimposed infection. Some departments will use an imipenem / cilastin combination due to its affinity for pancreatic tissue. This has been shown to reduce the incidence of bacterial infection in some cases. However secondary fungal infection is still a worrisome complication. If asked in finals, just remember that the use of antibiotics in pancreatitis is controversial. However if you are going to administer an antibiotic use an imipenem. E – False By definition, peripancreatic fluid collections persisting for more than 4 weeks are termed acute pseudocysts. Pseudocysts lack an epithelial layer and, thus, are not considered true cysts. In addition, the term cyst is also a misnomer, as most of these collections are filled with necrotic debris and not fluid. A more descriptive term for these collections may be organized necrosis. Most of these can be followed clinically. When pseudocysts are symptomatic (i.e., associated with pain, bleeding, or infection) or are larger than 7 cm and are rapidly expanding in an acutely ill patient, intervention is indicated. 12. Gallstones a. Ascending cholangitis requires emergency decompression of the CBD b. Choledochal cysts are associated with malignancy c. The five year survival rate of adenocarcinoma of GB is less than 5%? d. Magnetic resonance cholangiogram gives accurate picture of biliary tree e. Gallstones can be dissolved by ursodeoxycholic acid A – True Cholangitis presents with Charcot’ Triad of symptoms (fever, pain and jaundice). If supparative inflammation is present then Reynolds Pentad (fever, pain, jaundice, confusion and hypotension). This condition usually results from secondary infection of stagnant biliary fluid as a consequence of long standing stasis due to cholelithiasis. The medical management is hydration, analgesia and IV antibiotics. Due to the often-present high biliary pressures there is defective secretion of antibiotics. Decompression is as a consequence necessary. This is done endoscopically. Traditionally this was done with emergency surgery involving common bile duct exploration and T tube placement. Now reserved for failed endoscopic cases. B – True Choledochal Cysts are found in children. They are one of the differentials of prolonged neonatal jaundice of the conjugated variety. 67% have been discovered by the age of 10 years. Other means of presentation include cholangitis or recurrent bouts of pancreatits. They are three times more common in females. More common in Asia. The aetiology is not completely understood. One postulated theory is that there is a malunion of the pancreatic and common bile duct with a propensity towards relux of pancreatic juices and enzymes back into the CBD, resulting in weakness of the wall. This may allow the development of the cyst. The risk of development of cholangiocarcinoma is 2.5 – 15%. Dreaded complication. C – True Gallbladder carcinoma is the fifth most common cancer of the GIT. 90% of cases are associated with cholelithiasis. They typically present in the persons 60’s. They often arise in the so-called porcelain gallbladder. Gallbladder cancer is four times more common in females. Early stage presentation is similar to cholelithiasis or with a degree of biliary dyskinesia. Most GB adenocarcinomas unfortunately present late with metastasis. D – True MRC is an effective non-invasive diagnostic modality for biliary tract pathology. E – True In patients with established cholesterol gallstones, treatment with ursodeoxycholic acid at a dose of 12-15 mg/kg daily may result in gradual gallstone dissolution. This intervention typically requires 6-18 months and is successful only with small, purely cholesterol stones. Patients remain at risk for gallstone complications until dissolution is completed. Dissolution fails in many cases. Moreover, after discontinuation of treatment, most patients will form new gallstones over the subsequent 5-10 years. Ursodeoxycholic acid reduces cholesterol saturation of bile, both by reducing liver cholesterol secretion and by reducing the detergent effect of bile salts in the gallbladder (thereby preserving vesicles that have a high cholesterol carrying capacity). 13. Meckles diverticulum a. Is found in 2% of the population b. Is a “true” diverticulum? c. Contains ectopic tissue in 50% cases d. Is a remnant of vitello-intestinal duct? e. May mimic as acute appendicitis A – True Meckels diverticulum obeys the ‘rule of twos’. It is two inches long, located two feet proximal to the ileocaecal valve, found in two percent of the population and contains two types of mucosa. B – True Why? Because it contains all three layers of the bowel wall. A diverticulum in contrast which is an outpouching of the bowel typically located in the sigmoid colon contains an attenuated muscle coat and so is a false diverticulum. C – True D – True E - True 14. Trauma a. In the initial management of the injured patient, control of hemorrhage should be the priority b. Right diaphragmatic rupture is more common than left c. Fracture of left lower ribs may be associated with rupture of the spleen d. A flail chest is commonly associated with ARDS e. Liver or splenic injuries always require operative intervention A – False The predicatable order of the primary survey that reinforces the fact that life threatening injuries kill in a predictable order is: Airway control with cervical spine protection. Breathing with oxygenation and ventilation. Circulation with haemorrhage control. Disability or neurologic status. Exposure of patient with temperature control. B – False The left diaphragm is lower than the right so intuitively is more susceptible to penetrating thoracic trauma. Any penetrating injury below the level of the nipples may injure the diaphragm. Thoracoscopy is indicated to evaluate the diaphragm of interest. C – True The spleen lies longitudinally along the 9-11th ribs on the left of the chest. D – True It is not the flail chest that causes the problem. These patients almost invariably have an underlying lung contusion, which in itself can cause acute respiratory distress syndrome. This is diagnosed by an acute onset of hypoxaemia, pulmonary infiltrates and non cardiogenic pulmonary oedema (PCWP <19mmHg). Supportive therapy is indicated with CPAP. E – False Firstly the word always is in the question. The liver has a unique ability to establish spontaneous haemostasis even with extensive injuries. For this reason the majority of liver injuries in haemodynamically stable patients can be managed non-operatively. A greater percentage of splenic injuries require operative intervention due to their propensity to bleed. 15. Thoracic/Neurosurgery a. A chest drain is usually inserted in the 4th/5th intercostal space in the mid-axillary line b. Thorascopic sympathectomy is the treatment of hyperhydrosis of the hands c. CT scan of the brain is indicated in depressed skull fracture d. A GCS < 8 is an indication for endotracheal intubation e. Tension pneumothorax is diagnosed on chest X-ray A – True The purpose of the chest drain is either drainage or opposition of the pleural surfaces. B – True Serious procedure, which is reserved for cases that are refractory to conservative treatment such as iontophoresis or BOTOX injections. C – True When a depressed skull fracture is present there is a 1 in 3 chance that an extra-axial haematoma has formed that will need neurosurgical evacuation. Also the depressed skull fragment will require elevation. If the dura mater has been torn then give prophylactic antibiotics. D – True E – False Yes a pneumothorax will be seen on CXR with the appearance of the so-called ‘black lung’ and mediastinal shift. However if the patient has a tension pneumothorax and you wait for the results of the x ray, quite often the patient will have died in the intervening time. It is a clinical diagnosis based on the presence of diminished expansion, hyperresonance to percussion, absent breath sounds, tracheal deviation away from affected side, apex displacement and an obstructive shock appearance (tachycardia hypotension). Don’t procrastinate chest a venflon catheter and perform a needle aspiration now!!! 16. Endocrine a. Follicular carcinoma of thyroid primarily spreads through lymphatics b. Parathyroid adenoma is the most likely cause of hyperparathyroidism c. Hurtle cell carcinoma is a variant of papillary carcinoma of the thyroid d. Phaeochromocytoma is associated with MEN IIa e. Superior laryngeal nerve supplies cricothyroid muscle A – False This form of thyroid carcinoma occurs where endemic goitre is common. The median age of onset is the fifth decade of life. It spreads haematogenously and so has a worse prognosis. Lymphatic dissemination is uncommon B – True Hyperparathyroidism is divided into primary, secondary and tertiary variants. The most common cause of primary hyperparathyroidism is a solitary parathyroid adenoma. Carcinoma and hyperplasia is rare. C – False This comprises 5% of thyroid cancers. The cell of origin is the follicular cells. I131 is not taken up. FNAC is not useful, can only be confirmed by tissue histology. Spreads through lymphatics. D – True The multiple endocrine neoplasias are autosomal dominant pre malignant paraendocrinopathies. MEN type 1 is parathyroid hyperplasia + pituitary adenoma + pancreatic tumours. MEN type 2a is medullary carcinoma of thyroid + pheochromocytoma + parathyroid hyperplasia. MEN 2b is like MEN 2a but has neurocutaneous signs. E – True This can be damaged during thyroidectomy. The result is a quieter and deeper voice. Catastropic is opera singers! 17. Paediatrics a. Hydrocele in a child <1 year old necessitates surgery b. Pyloric stenosis presents within 10-12 weeks of life c. Mesenteric adenitis is an uncommon cause of abdominal pain in children d. An undescended testes may be found in the hilum of the spleen e. Children with pyloric stenosis have hypokalemic, hyperchloremic acidosis A – False A hydrocele is a collection of serous fluid in the processus vaginalis. It is divided into primary and secondary variants. Primary Hydroceles (Idiopathic) are large and tense. The underlying testis is normal. It causes scrotal swelling which is tense and transilluminates. The swelling is on the posterior and lateral aspect of the testis. If it persists beyond the first year of life then operative intervention is required. Intraoperatively the sac is identified, ligated and excised. Care is taken not to damage the cord structures. Even though one year is taken as the cut off for operative intervention, it has been proven that most primary hydroceles will resolve by 18 months. Secondary Hydroceles are smaller and the underlying testis is diseased. It is an exudative collection secondary to tumour or inflammation. Ultrasound of the testis will differentiate between a normal and abnormal testis. Aspiration of hydroceles is not a treatment modality with any longevity as the fluid collection recurs. B – True The aetiology of this condition is unknown. It is a familial condition. 85% occurs in male infants. 50% are first born infants. It is rare for the condition to present after 12 weeks of age; the usual presentation is at 3-4 weeks of age with projectile vomiting that doesn’t contain any bile (hence obstruction is proximal to the second part of the duodenum). The infant is ‘always hungry’, with a palpable ‘olive’ mass under the costal margin and visible peristalsis. Biochemistry shows a hypochloraemic hypokalaemic metabolic alkalosis. Following correction of the biochemical disturbance the surgical treatment is a Ramstedt’s Pyloromyotomy. The infant can be fed the next day. Results are excellent with a very low mortality rate. C – False This is a very common cause of abdominal pain in young children following an upper respiratory tract infection. The diagnosis often co-exists with appendicitis. Mesenteric adenitis can only be definitively confirmed at laparatomy or laparoscopy. With mesenteric adenitis the vomiting normally precedes the pain where as in appendicitis the vomiting follows the pain. D – True An ectopic testis is one that has strayed from the normal line of descent. The commonest position is the superficial inguinal pouch. Although rare ectopic testes and maldescended testes can occur intra-abdominally. E - False 18. Evidence based medicine a. Occult blood testing is a proven screening modality for colorectal carcinoma b. Endoscopic ultrasound accurately assess rectal tumour presentation c. Laparoscopic appendicectomy has revolutionized the treatment of acute appendicitis d. Sentinel lymph node biopsy is not yet a standard form of treatment for breast carcinoma world-wide e. Immunotherapy using interferon-alpha is of benefit in Stage III malignant melanoma A – True Evidence from RCTs is currently available for FOB testing. Screening every two years with home tests reduces mortality by 15-33%. However false positives are high (up to 10%) and there are problems with acceptability. B – False Useful technique in carcinoma of oesophagus C – False Laparoscopic appendicectomy reduces recovery time and incidence of wound infection but is associated with increased risk of intra-abdominal abscesses. D – True The USA doesn’t primarily rely on the technique. E – False Biochemotherapy refers to a combination of cytotoxic therapy and immunotherapy. The ECOG trial showed that this combination was useful for melanomas >4mm and surgically resected nodal metastases. 19. The following are associated with malignancy a. Acanthosis nigricans b. Thrombophlebitis migrans c. Ganglions d. Fourniers Gangrene e. Keratoacanthoma A – True This is the presence of velvety lesions typically found in the axillae and other flexor surfaces. Can be site in hyperinsulinism, visceral carcinoma and hyperandrogenism. B – True Migratory thrombophlebitis (Trousseau sign) and venous thrombosis occur in patients with pancreatic cancer C – False A ganglion cyst is a bump or mass that forms under the skin. Most commonly, ganglions are seen on the wrist (usually the back side) and fingers, but they can also develop around joints on the shoulder, elbow, knee, hip, ankle and foot. Ganglion cysts form when tissues surrounding certain joints become inflamed and swell up with lubricating fluid. They can increase in size when the tissue is irritated and often can "disappear" spontaneously. These masses or cysts appear to grow sometimes but they are not tumours or cancerous. D – False This is a rapidly progressive gangrene of the penis and scrotum without apparent cause. This condition, now known as Fournier gangrene, is defined as a polymicrobial necrotizing fasciitis of the perineal, perianal, or genital areas E – True Pertinent physical findings are limited to the skin. Lesions typically are solitary and begin as firm, roundish, skin-colored or reddish papules that rapidly progress to dome-shaped nodules with a smooth shiny surface and a central crateriform ulceration or keratin plug that may project like a horn (see Images 1-4). Most KAs occur on sun-exposed areas. The face, neck, and dorsum of the upper extremities are common sites. Truncal lesions are rare. Lesions usually are skin-colored to pinkish-red. Unaffected skin retains its normal appearance. Muir-Torre syndrome: KA may be a component of Muir-Torre syndrome, which is a cancer-associated genodermatosis with multiple sebaceous neoplasms (adenomas, epitheliomas, carcinomas), keratoacanthomas, and gastrointestinal malignancies (most commonly colon), although other carcinomas have been reported (genitourinary, pulmonary, endometrial). 20. Diverticular disease a. The most common cause of bleeding per rectum is diverticular disease b. The treatment of diverticular disease is oral steroids c. Is a premalignant condition d. Is best treated with a low residue diet e. Surgery is indicated in more than 50% of patients with diverticular disease A – True Diverticular has been quoted as the most common cause of lower gastrointestinal bleeding accounting for 60% of cases. 13% of causes are attributable to IBD and noninfectious gastroenteritis and colitis. 11% of cases are found to be anorectal in origin such as fissures and haemorrhoids. 9% neoplasia, 6% coagulopathy and 1% A-V malformations. B – False Diverticular generally doesn’t require any medical treatment except an increase in the fibre within one’s diet. If secondary complications occur such as diverticulitis then antibiotics may be required. Complications such as haemorrhage, obstruction, fistulae or abscess will require surgical intervention. C – False D – False Low residue / low fibre diet is the aetiology of diverticular disease. A low fibre diet is thought to be responsible for the raised intraluminal pressures in the sigmoid colon in these patients causing the false diverticulae at the sites of weakness. This is generally where the vasa recta penetrate the bowel wall. Hence the reason for the high incidence of haemorrhage. E – False The quoted figure is between 8 – 25%. EXAM 6: Unknown year, unknown location Questions 1-6 missing 7. Carcinoma of the lung is: a. Commonest cancer in our community F- skin cancer is the commonest cancer b. A tumour with 20% cure rate. ? F- depends on stage and grade, overall, prognosis is poor: only 50% patients with non-small cell lung CA without mets will survive 2 years c. Associated with better prognosis if oat cell in type F- oat cell (small cell) CA is associated with a particularly poor prognosis as disease is usually disseminated at presentation. d. Characterised by rising incidence in females T e. Most commonly developed from alveolar epithelium F-bronchial CA more common than alveolar cell CA 8. Brachial embolism a. Has more favorable prognosis than popliteal aneurysm ??? couldn’t find a reference for this b May be operated upon under local anesthesia ??? c. Is associated with mitral stenosis ?T- mitral valve stenosis is associated with systemic emboli so I assume this is true? d. Always leads to gangrene is not removed ?T but not if collateral blood supply present and sufficient e. Embolectomy should be associated with fibrinolytic therapy ?T- thrombolytic/anticoagulant therapy recommended but not sure what type of therapy is favoured 9. Oophrectomy for breast cancer a. Has now been abandoned as a form of therapy ?F- may be considered in pre-menopausal women with oestrogen receptor positive tumours if GnRH analogues cannot be used, may also form part of prophylactic surgery for women with a strong family history eg BRCA b. Is best done by irradiation of ovaries ?couldn’t find a definite answer for this c. Has been replaced by chemotherapy ?T-endocrine therapy has largely taken over with oestrogen receptor blockers (tamoxifen), aromatase inhibitors (anastrozole) or GnRH analogues being used instead. d. May reveal ovarian metastases T e. Should be followed by estrogen therapy if done at menopause ?F – depends on oestrogen receptor state of tumour and HRT should ideally be combination oestrogens & progesterones 10. In varicose veins: a. Communicating veins penetrate the deep fascia T b. The aim of sclerosant therapy is to thrombose the veins F- the vein is compressed for several weeks to avoid thrombosis and encourage the formation of granulation tissue which obliterates the vein lumen. c. More commonly involve the left lower limb ? d. Lateral leg is commoner site ulceration F-venous ulceration typically occurs just above the medial malleolus (gaiter area). Ulceration may occur secondary to chronic varicose veins due to longstanding venous hypertension and insufficiency e. May be familial T- Heredity is important in determining susceptibility to primary valvular failure, but the specific genetic factors responsible for varicosities have not yet been elucidated. Reflux at the saphenofemoral junction (SFJ) (where the superficial GSV joins the deep common femoral vein) is twice as likely when a parent had a similar condition. Monozygotic twins are concordant with regard to varicose veins in 75% of cases. The prevalence rate of varicose veins is 43% in female relatives of patients with varicose veins, but only 19% in male relatives. 11. In a contaminated traumatic wound: a. Local antibiotics are very helpful ?F- may be of use but systemic antibiotics needed eg benzylpenecillin/flucloxacillin/co amoxiclav +/- metronidazole b. Tetanus toxoid provides 100% against tetanus F-tetanus toxoid vaccination course: 3 vaccines given as part of 5 in 1 immunisations at 2, 4, and 6 months, booster recommended on starting school and again in early adulthood. A booster vaccine is given at time of injury if no booster within the last 10 years. Human tetanus immunoglobulin is also required in the partially or non-immune adult (this neutralises free tetanus toxin). c. Gas in tissues is pathognonomic of gas gangrene F- may be due to subcutaneous emphysema secondary to perforation of an air-containing viscus d. Following debridement the wound should be closed by sutures ?F- if contaminated wound should be left open to heal by secondary intention so it may be cleaned and debrided and to avoid the formation of a deep abcess. e. Tetanus antitoxin if indicated is preferable to human immune globulin F- this is horse antitetanus serum and may cause a local hypersensitivity reaction and may not be as effective 13. If a patient is cyanosed following tracheostomy with a cuffed tube, suspect a. Laryngeal edema F-this may occur after a cricothyroidotomy b. Intubation of right bronchus T-tube displaced,but uncommon c. Mucus blocking tube T d. Mucus blocking bronchi ?T e. Displacement of tube T 14. a. trachea b. c. d. rupture e. right. Tracheal shift to the left may be caused by Right pneumothorax T- if tension pneumothorax as these push the to the opposite side Nodular goiter T Collapse of right lung F-this will pull the trachea to the right Left sided emphysema ?F- may cause sub pleural bullae which may and cause a pnemothorax Right pneumonectomy F- if any deviation, it will be to the 15. A patient has pain over lower internal end of radius, extension and abduction of thumb a. This is due to a fractured lunate ??? b. May be caused by DeQuervain’s disease T- this causes pain over the styloid process of the radius, thickening of the tendons of abductor pollicis longus and extensor pollicis brevis. Also known as stenosing tenovaginitis c. May be due to Kohler’s disease F- this causes limp, pain in the tarsal region and navicular tenderness in 3-5 year olds. Dense deformed bone seen on radiograph, resolves with analgesia and rest,excellent prognosis. d. May be treated by steroid injection T – or NSAIDS, or release of the tendon sheath. e. Often results from unaccustomed use hand T 16. Patients with secondary thyrotoxicosis ???? I’m ignoring the word secondary,it makes no sense. a. Should never be treated with radioiodine T b. Tend to develop recurrent laryngeal nerve palsy ? c. Have thyroid antibodies in their blood ?T d. Usually have a diffusely enlarge goiter ?T e. Generally are in the 20-40 age group ?T c,d,e true if they mean grave’s disease. B true in case of malignancy causing hyperthyroidism 17. Circumcision is indicated in: a. Ammoniacal dermatitis F b. Non-retractile prepuce at one year F At 3 years of age 10% of boys are unable to fully retract the foreskin. By adolescence, 98-99% can fully retract their foreskin to expose the glans c. Prophylaxis of carcinoma of penis ?F d. Phimosis T e. Paraphimosis T – if non-resolving Although many families choose to have their male infants circumcised for cultural, religious, or hygienic reasons, only a few accepted medical indications are recognized: phimosis, paraphimosis, balanitis and posthitis. Circumcision is also recommended in male infants and toddlers who develop UTIs and children who require clean, intermittent catheterization to facilitate this procedure. 18. In carcinoma of larynx a. Hoarseness is a late symptom F- usually the first symptom b. Peak incidence is from 20-40 years F Laryngeal cancer most commonly affects men middle-aged or older who are smokers and who use alcohol. The peak incidence is in those aged 50-60 years. c. There is an association with cigarette smoking T d. There is association with occupation ? e. Distant metastases occur early F-usually spread is to cervical nodes 19. Shoulder dislocation a. Occurs from direct violence ?T b. Is not associated with any fracture F-may be associated with fractures of the neck of the humerus c. Commonly damages the axillary artery ?T d. If adequately immobilized following reduction recurrent dislocation is prevented ?F e. Should be X-rayed before reduction T- rules out co-existing fractures, may not be needed in cases of recurrent dislocation 21. a. foreign b. c. Ingested foreign bodies are likely to be arrested At crico-pharyngeus F- this is a common site for aspirated bodies At thoracic inlet T At aortic arch T d. At diaphragm T e. In stomach F- once they reach the stomach there is an 80-90% chance of the object passing on. Patients can usually localize foreign bodies in the upper esophagus but localize them poorly in the lower two thirds of the structure. The esophagus has 3 areas of narrowing: the upper esophageal sphincter (UES), which consists of the cricopharyngeus muscle; the crossover of the aorta; and the lower esophageal sphincter (LES). These areas are where most esophageal foreign bodies become entrapped. Structural abnormalities of the esophagus, including strictures, webs, diverticula, and malignancies, increase the risk of foreign body entrapment, as do motor disturbances such as scleroderma, diffuse esophageal spasm, or achalasia. Once a foreign body has reached the stomach, it has an 80-90% chance of passage. Objects longer than 6 cm may become entrapped by either the pylorus or the duodenal sweep, and objects larger than 2 cm in diameter also may fail to pass the pylorus. When a foreign body has reached the small bowel, the only structural impediment to passage is the ileocecal valve. Rarely, a foreign body may become entrapped in a Meckel diverticulum. Most complications of pediatric foreign body ingestion are due to esophageal impaction, usually at 1 of 3 typical locations. The most common site of esophageal impaction is at the thoracic inlet. Defined as the area between the clavicles on chest radiograph, this is the site of anatomical change from the skeletal muscle to the smooth muscle of the esophagus. The cricopharyngeus sling at C6 is also at this level and may "catch" a foreign body. About 70% of blunt foreign bodies that lodge in the esophagus do so at this location. Another 15% become lodged at the mid esophagus, in the region where the aortic arch and carina overlap the esophagus on chest radiograph. The remaining 15% become lodged at the lower esophageal sphincter (LES) at the gastroesophageal junction 22. Cancer of oesophagus a. Is associated with duodenal ulceration b. c. d. e. Presents with chest pain Is always a squamous cell carcinoma Has a bad prognosis Frequently presents with heartburn FFFTF a. Oesophageal ca risk factors: achalasia, caustic stricture, Barrett’s, alcohol, cigs, celiac dis, fe deficiency anaemia, male. Duodenal ulceration risk factors: H pylori, NSAIDs, steroids, cigs, Zoll-Ellison. Even though cigs are a common risk factor to both, I would still say false. b. Most commonly presents with dysphagia, progressing from solids to liquids. May also present with regurgitation, aspiration, or odynophagia. c. Can be Primary (adca, sq ca, leiomyosarcoma) or Secondary (direct invasion from lung or stomach). d. 70% not operable at dx. 5% 5yr survival. e. see b. 23. Carcinoma of the stomach a. Has a good prognosis b. Often presents with anorexia c. May be associated with previous gastric surgery d. Has rarely spread to lymph glands at time of prognosis e. Is always diagnosed by barium meal TFTFF a. Very subjective question! When confined to mucosa/submucosa without lymph nodes or distant mets, 5yr survival of 95-100%. b. May be subtle in early stages and present with dyspepsia, flatulence or indigestion. In more advanced case, can present with wt loss, anaemia, dysphagia, vomiting, epigastric or back pain. c. When the gastric mucosa is exposed to bile, there is an increased risk and this can occur after a gastroenterostomy. Other aetiologies include: Diet (malnutrition, high in nitrates nitrites and nitrosamines. Vitamins C/E thought to be protective), H pylori, Gastric Polyps, Chronic Gastric Ulcer Disease, chronic atrophic gastritis, intestinal metaplasia, gastric dysplasia, blood group A. d. Vast majority are late stage at diagnosis. e. Nope. OGD with biopsy is the way to go. 24. Infantile pyloric stenosis a. Presents with vomiting from birth b. Frequently results in acidosis c. Is readily diagnosed clinically d. Is usually cured by surgery e. Is associated with subsequent duodenal ulceration FFTTF a. Usually at 3-8 wks b. Hypochloraemic, Hypokalaemic metabolic ALKALOSIS. c. Yes.. visible peristalsis and a palpable “olive” (hypertrophied pyloris), Clinical diagnosis is possible in 70%. The rest are diagnosed on ultrasound. d. Ramstedt’s Pyloromyotomy: The serosa of the pyloris is cut with a scalpal and the muscle of the pyloris is cut down to the mucosa. e. I can’t find an answer to this one anywhere so I’ll say false. 25. The gastric antrum a. Secretes acid b. Is responsible for secretion of gastrin c. Is responsible for production of intrinsic factor d. Is important in the mechanism of gastric emptying e. Is denervated by truncal vagotomy FTFTT a. Parietal cells are located in the body b. G-cells which secrete gastrin are in the antrum. There is a decrease in gastrin production with a truncal vagotomy, which contributes to the decreased parietal cell acid secretion. c. see a. d. The mechanical roles of the antrum are the grinding of food and the propulsion of small amounts of chyme towards the duodenum when the pyloric sphincter is relaxed. e. Truncal vagotomy, unlike highly selective vagotomy, involves the vagal innervation of the antrum (as well as the rest of the stomach). The main problem with truncal is that the pyloris is denervated and doesn’t relax thereafter.. and a drainage procedure must be carried out, like a Bilroth. 26. Meckel’s diverticulum a. Arises from the foregut b. May cause massive gastrointestinal bleeding c. Is associated with carcinoma of the small bowel d. May cause intussusception e. Is an acquired lesion TTFTF a. It is a remnant of the vitello-intestinal duct and lies on the anti-mesenteric border of the ileum. b. Heterotopic gastric epithelium sectretes HCl. This may cause peptic ulceration and is the commonest cause of melaena in children. c. Can’t find any literature saying that it is. d. Other causes of intussusception include: hyperplasia of Peyer’s patches, polyp. carcinoma, lymphoma. e. It is congenital 27. Crohn’s disease a. b. c. d. e. Is predominantly a mucosal disease Always requires surgery Is associated with the development of fistulae Often involves the perianal region Rarely recurs following adequate surgical management FFTTF a. Transmural b. Avoid if possible c. Other causes of fistulae: Foreign body, Radiation, Inflammation, Epithelialisation, Neoplasm, Distal obstruction (FRIEND). Fistula is an abnormal communication between two epithelialised surfaces. e. Surgery is non curative 28. a. b. c. d. e. The terminal ileum is responsible for the absorption of: Vitamin B12 Vitamin C Bile acids Fat Iron TFTFF B12 and Bile acids. However, terminal ileal resection will deplete the bile acid stores and lead to impaired lipid absorption. This is secondary though and I don’t think that makes this answer true. 29. Ulcerative colitis: a. Occurs predominantly in those over 50 b. Usually involves rectum c. May be precipitated by stress d. May result in colonic cancer e. Always responds to steroids FTFTF a. Max incidence is 20-40 yr olds. b. Rectum and sigmoid are principally affected. c. I don’t think so. d. 5-10% of patients with colitis for 20 yrs will develop malignant change. e. Surgery is required when medical treatment fails. 30. Diverticular disease a. Involves predominantly the sigmoid colon b. Is pre-cancerous c. May result in massive bleeding per rectum d. Responds to low residue diet e. Is more common in elderly TFTFT a. Sigmoid is most common site. It becomes pregressively less common as you move proximally. c. Diverticulosis bleeds, and it can be massive. d. I think fibre is a residue. High fibre, low fat is the advice. e. 60% of 60yr old Americans. Only 10-20% of those become symptomatic. 31. Large bowel cancers a. Is the most common cause of large bowel obstruction b. Is the most common cause of vesico-intestinal fistula c. Most commonly occurs is recto-sigmoid d. Rarely develops from colonic polyps e. Has a bad prognosis F?TFF a. Diverticulitis is more common b. It is a cause of fistula but I don’t know if it’s the most common. c. Sigmoid is the most common site. d. Villous polps are the worst. e. Duke’s A has a 90% 5yr survival. 32. Chronic perianal disease may be secondary to: a. colonic diverticular disease b. Gastrointestinal tuberculosis c. Polyposis coli d. Carcinoma of recto-sigmoid e. Crohn’s disease FTFFT 33. a. b. c. d. e. In obstructive jaundice Serum alkaline phosphatase is normal Oral cholecystogram is of value The gallbladder is palpable There is splenomegaly Vitamin K absorption is impaired FFTFT a. Obstructive: increase Alk Phos and GGT b. CCK causes gallbladder contraction.. not a good idea. c. Courvoisiere’s Law: Jaundice and a palpable gallbladder.. unlikely to be due to stones. However, pancreatic ca can obstruct and cause a palpable GB. This qs is true if you interpret it as “can be palpable”. Usually isn’t though. d. e. Decreased bile salts reaching the intestine -> impaired fat absorption. 34. Nephroblastomas: a. is radio-sensitive b. Requires early surgery c. Responds to chemotherapy d. Has a good prognosis over the age of ten e. Usually metastasizes to bone T?TFT a. Surgical resection and chemo is the treatment of choice. Radiotherapy is reserved for residual disease.. which implies that it is sensitive to radiotherapy (even though it’s not used). b. ? c. Actinomycin D and vincristine is used. d. No. The earlier it presents, the better the prognosis. e. Most common metastatic sites are lung, liver and bone. 35. Benign prostatic hyperplasia may result in: a. Acute epididymo-orchitis b. Bladder stone c. Hematuria d. Bladder diverticulum e. Testicular atrophy ?TFTF c. Unless there is a stone d. Obstruction -> increased bladder pressure -> Diverticulae. The diverticulae are predisposed to urinary stasis and subsequent UTI or stone formation.