20030131BWomens Hlth-Infertility Law
advertisement

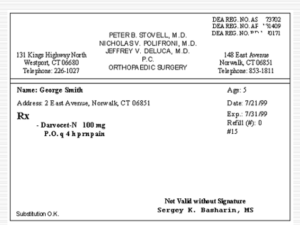
Jefferson Lewis et. Al. School Employees’ Healthcare Plan Impact of New York State Insurance Laws Enacted 2002 Mandatory Compliance Infertility Law-Applicable July 1, 2003 (or next Plan amendment date whichever is sooner) Treatment of Infertility Current Provision: 35. Medicines and Drugs (Traditional Option Only) c. Covered Drug Expenses. [Fertility Drugs not listed as covered expenses] E. Prescription Drug Expense Benefits (Provider Choice Option Only ) 1. Covered Prescription Drug Expenses. [Fertility Drugs not listed as covered expenses] 2. Pre-authorization Requirements The following lists the drugs that currently require pre-authorization. Fertility and contraceptive drugs for treatment of organic conditions. (Reproduction and birth control purposes not Covered) 8. Prescription Drug Expense Exclusions. e. Infertility or fertility medications unless to treat correctable medical conditions otherwise Covered by the Plan. Plan Exclusions 7. Drugs/Infertility/Birth Control/Vitamins/Supplements. Medicines or drugs that can be purchased without a Physician's prescription, contraceptive (birth control) drugs and devices, infertility drugs, or vitamins and supplements, including nutritional supplements or food products, whether or not obtainable by prescription. Exceptions: Diabetic drugs and Supplies; birth control drugs and infertility or fertility medications that are used to treat correctable medical conditions otherwise Covered by the Plan; prenatal prescription vitamins; certain Aminoacidopathies formula, enteral formula or modified food products specifically shown as Covered Expenses. 27. Infertility/Reproduction/In-vitro/Artificial Insemination. Services or Supplies relating to reproduction, artificial insemination, in vitro fertilization procedures or other artificial conception procedures. Services or Supplies relating to treatment of infertility or reproduction unless to treat correctable medical conditions otherwise Covered by the Plan. Documentation of correctable medical conditions must be presented to the Claims Administrator. Effective July 1, 2003 (Includes changes in the Law for Contraceptive Coverage-See Women’s Health Law shown below) Treatment of Infertility. Benefits are available for services or supplies related to treatment of infertility for Covered Persons, ages 21-44 years old (or any age for treatment of correctable medical condition otherwise covered by the Plan that results in infertility). Coverage includes diagnosis and treatment of infertility as part of a Physician’s overall plan of care and includes the following when rendered by qualified Healthcare Providers: Jefferson Lewis et al School Employee’s Healthcare Plan Impact of Women’s Health /Infertility Insurance Laws 1 a. Surgical or medical procedures that would correct the malformation, disease or dysfunction resulting in infertility; and b. Diagnostic tests and procedures provided to determine infertility or that are necessary in connection with any surgical or medical infertility treatments including, but not limited to, hysterosalpingogram, hysteroscopy, endometrial biopsy, laparascopy, sono-hysterogram, post coital tests, testis biopsy, semen analysis, blood tests, and ultrasound; and c. Prescription drugs approved by the Federal Food and Drug Administration for use in the diagnosis and treatment of infertility. Coverage will be provided in accordance with the standards and guidelines established and adopted by the American College of Obstetricians and Gynecologist and the American Society for Reproductive Medicine. Note: For Covered Persons, any age, Plan covers the diagnosis and treatment of other correctable medical conditions covered by the Plan even if that condition results in infertility. This includes prescription fertility drugs used in the treatment of that condition. 35. Medicines and Drugs (Traditional Option Only) c. Covered Drug Expenses. The quantity of each drug purchased at a drug store will be limited to a 90-day supply at a time. The mail service Pharmacy is usually limited to a 90-day supply of maintenance drugs. Prescription refills will be paid for up to one (1) year from the date of the original prescription. Unless otherwise excluded, Allowable Fees for the following drugs are eligible for Comprehensive Expense Benefits when found Medically Necessary for the treatment of an Illness or Injury, according to Plan provisions. 1) 2) 3) 4) 5) Medications that require a prescription by a licensed Physician and are Federal legend drugs. Compounded medications containing at least one prescription ingredient. Prenatal prescription vitamins when taken during Pregnancy. Prescription contraceptive drugs or devices. Prescription drugs used in treatment of infertility for persons who are ages 21-44 years old. E. Prescription Drug Expense Benefits (Provider Choice Option Only ) 1. Covered Prescription Drug Expenses. The maximum quantity of each Covered drug purchased at one time will be limited to a 34-day supply or 100-dosage unit, whichever is greater. Mail service drugs will be limited to a maximum quantity of a 90-day supply. Prescription refills will be paid for up to one (1) year from the date of the original prescription. Unless otherwise shown, all drugs must be found Medically Necessary and ordered, in writing, by the attending licensed healthcare Provider legally authorized to prescribe the drugs a. Medications that require a written prescription by a legally authorized licensed healthcare Provider and are and are Federal legend drugs. b. Compounded medications containing at least one prescription ingredient in therapeutic amounts. c. Prenatal prescription vitamins when taken during Pregnancy, Vitamin B-12 when ordered due to pernicious anemia, other single entity vitamins are excluded. d. Prescription contraceptive drugs or devices Infertility drugs for persons under age 21 and older than 44 years old. e. Prescription drugs used in treatment of infertility for persons who are ages 21-44 years old. 2. Pre-authorization Requirements The following lists the drugs that currently require pre-authorization. Infertility drugs for persons under age 21 and older than 44 years old. Aminoacidopathies Formula; Enteral Formula and Modified Food Products. (Normal nutritional supplements or elective supplements are not Covered) Jefferson Lewis et al School Employee’s Healthcare Plan Impact of Women’s Health /Infertility Insurance Laws 2 Growth hormones Lovenox Biotech drugs (i.e., Capaxone) Insulin Pumps 8. Prescription Drug Expense Exclusions. e. Infertility or fertility medications for persons under age 21 or older than age 44. Exception: For Covered Persons, any age, Plan covers prescription infertility drugs used for treatment of other correctable medical conditions covered by the Plan even if that condition results in infertility. Plan Exclusions 7. Drugs/Infertility/Vitamins/Supplements. Medicines or drugs that can be purchased without a Physician's prescription; infertility drugs for persons under age 21 or older than age 44; or vitamins and supplements, including nutritional supplements or food products, whether or not obtainable by prescription. Exceptions: Diabetic drugs and Supplies; prenatal prescription vitamins; certain Aminoacidopathies formula, enteral formula or modified food products specifically shown as Covered Expenses. For Covered Persons, any age, Plan covers prescription infertility drugs used for treatment of other correctable medical conditions covered by the Plan even if that condition resulted in infertility. 27. Infertility/Reproduction/In-vitro/Artificial Insemination. Services or Supplies relating to reproduction, artificial insemination, in vitro fertilization procedures or other artificial conception procedures; Services or Supplies relating to treatment of infertility for persons under age 21years or older than age 44. Exception: For Covered Persons, any age, Plan covers treatment of other correctable medical conditions even if that condition resulted in infertility. Documentation of correctable medical conditions must be presented to the Claims Administrator. Women’s Health Law-Applicable July 1, 2003 (or next Plan amendment date whichever is sooner) Mammography Screening Current provision needs to be updated to allow an annual mammography from age 40 and to allow any age with prior personal history or who have a first degree relative with prior history. Current Provision: 3. Mammography Screening. Benefits are available for routine mammography screening when rendered in a Hospital Outpatient setting, clinic or Physician's office. Coverage is limited to the following conditions: a. Mammography, recommended by Physicians for Covered Persons, at any age, with a personal medical history of breast cancer, or whose mother or sister has a history of breast cancer; b. A single baseline mammography for Covered Persons 35-39 years of age; c. One mammography every two years for Covered Persons 40-49 years of age, or more frequently upon recommendation of a doctor; d. An annual mammography for Covered Persons 50 years of age or older. e. In no event, will the Plan pay more than one routine mammography screening in any 12 consecutive months. Effective July 1, 2003: Jefferson Lewis et al School Employee’s Healthcare Plan Impact of Women’s Health /Infertility Insurance Laws 3 3. Mammography Screening. Benefits are available for routine mammography screening when rendered in a Hospital Outpatient setting, clinic or Physician's office. Coverage is limited to the following conditions: a. Mammography, recommended by Physicians for Covered Persons, at any age, having a prior history of breast cancer or who have first degree relative with a prior history of breast cancer; b. A single baseline mammography for Covered Persons 35-39 years of age; d. An annual mammography for Covered Persons 40 years of age or older. e. In no event, will the Plan pay more than one routine mammography screening in any 12 consecutive months. Annual Cervical Screening Current Plan Provision complies with the law. No change in the Plan is necessary. Bone Mineral Density Measurement Current Plan does not have provision for Bone Mineral Density Measurement. Effective July 1, 2003. 6. Bone Mineral Density Measurement and Tests. Benefits are available for Bone Mineral Density Measurement and Tests that meet the criteria of the Federal Medicare Program and the National Institutes of Health including, but not limited to, dual-energy absorptiometry. The attending physician must order the testing. Coverage is limited to once every two years (more frequently if found medically necessary) for the following conditions: a. Women who are being treated for low estrogen levels and are at clinical risk for osteoporosis, based on their medical history and other findings. b. Men and women whose x-rays show previous fractures. c. Men and women on prednisone or steroid-type drugs or who are planning to begin such treatment or other drug regiment posing a significant risk of osteoporosis. d. Men and women diagnosed with primary hyperparathyroidism. e. Men and women being treated with a drug for osteoporosis, to see if it is working. f. Men or women with symptoms or conditions indicative of the presence, or the significant risk, of osteoporosis; diagnosed as having osteoporosis or having a family history of osteoporosis; g. With lifestyle factors to such a degree as posing a significant risk of osteoporosis; or h. With such age, gender and/or other physiological characteristics which pose a significant risk of osteoporosis. Traditional Option Schedule of Benefits Preventive/Wellness Care Covered Services Scheduled Benefit Allowance Routine Bone Density Screening Limited to once every two years for routine screening based on age sex and family history. Medically Necessary screening covered separately Diagnostic xrays or Diagnostic lab. Full Benefits Jefferson Lewis et al School Employee’s Healthcare Plan Impact of Women’s Health /Infertility Insurance Laws 4 Provider Choice Schedule of Benefits Covered Services Bone Density Measurement/Test Network Out of Network Limited to once every two years for routine screening based on age sex and family history. Medically Necessary screening covered separately under Diagnostic x-rays or Diagnostic lab. Full Network Benefits 80%, after Deductible Contraceptives Current Provisions: 35. Medicines and Drugs (Traditional Option Only) c. Covered Drug Expenses. [Contraceptive Drugs not listed as covered expenses] d. Drug Expense Exclusions. 5) Contraceptives, medicines, drugs, and devices used for birth control. (May be purchased at a Participating Pharmacy at a discounted allowance, but are not paid by the Plan) Exception: Birth control drugs that are used to treat correctable medical conditions otherwise Covered by the Plan E. Prescription Drug Expense Benefits (Provider Choice Option Only ) 1. Covered Prescription Drug Expenses. [Contraceptive Drugs not listed as covered expenses] 2. Pre-authorization Requirements The following lists the drugs that currently require pre-authorization. Fertility and contraceptive drugs for treatment of organic conditions. (Reproduction and birth control purposes not Covered) 8. Prescription Drug Expense Exclusions. c. Contraceptives, medicines, drugs, and devices used for birth control. However, Plan covers drugs to treat correctable medical conditions otherwise Covered by the Plan. Plan Exclusions 7. Drugs/Infertility/Birth Control/Vitamins/Supplements. Medicines or drugs that can be purchased without a Physician's prescription, contraceptive (birth control) drugs and devices, infertility drugs, or vitamins and supplements, including nutritional supplements or food products, whether or not obtainable by prescription. Exceptions: Diabetic drugs and Supplies; birth control drugs and infertility or fertility medications that are used to treat correctable medical conditions otherwise Covered by the Plan; prenatal prescription vitamins; certain Aminoacidopathies formula, enteral formula or modified food products specifically shown as Covered Expenses. Effective July 1, 2003: 35. Medicines and Drugs (Traditional Option Only). (Includes changes in the Law for Infertility Coverage shown previously) Jefferson Lewis et al School Employee’s Healthcare Plan Impact of Women’s Health /Infertility Insurance Laws 5 c. Covered Drug Expenses. The quantity of each drug purchased at a drug store will be limited to a 90-day supply at a time. The mail service Pharmacy is usually limited to a 90-day supply of maintenance drugs. Prescription refills will be paid for up to one (1) year from the date of the original prescription. Unless otherwise excluded, Allowable Fees for the following drugs are eligible for Comprehensive Expense Benefits when found Medically Necessary for the treatment of an Illness or Injury, according to Plan provisions. 1) 2) 3) 4) 5) Medications that require a prescription by a licensed Physician and are Federal legend drugs. Compounded medications containing at least one prescription ingredient. Prenatal prescription vitamins when taken during Pregnancy. Prescription contraceptive drugs or devices. Prescription drugs used in treatment of infertility for persons who are ages 21-44 years old. d. Drug Expense Exclusions. [ Remove exclusion “ 5) ” ] E. Prescription Drug Expense Benefits (Provider Choice Option Only ) 1. Covered Prescription Drug Expenses. The maximum quantity of each Covered drug purchased at one time will be limited to a 34-day supply or 100-dosage unit, whichever is greater. Mail service drugs will be limited to a maximum quantity of a 90-day supply. Prescription refills will be paid for up to one (1) year from the date of the original prescription. Unless otherwise shown, all drugs must be found Medically Necessary and ordered, in writing, by the attending licensed healthcare Provider legally authorized to prescribe the drugs. a. Medications that require a written prescription by a legally authorized licensed healthcare Provider and are and are Federal legend drugs. b. Compounded medications containing at least one prescription ingredient in therapeutic amounts. c. Prenatal prescription vitamins when taken during Pregnancy, Vitamin B-12 when ordered due to pernicious anemia, other single entity vitamins are excluded. d. Prescription contraceptive drugs or devices. e. Prescription drugs used in treatment of infertility for persons who are ages 21-44 years old. 2. Pre-authorization Requirements The following lists the drugs that currently require pre-authorization. Infertility drugs for persons under age 21 and older than 44 years old. Aminoacidopathies Formula; Enteral Formula and Modified Food Products. (Normal nutritional supplements or elective supplements are not Covered) Growth hormones Biotech drugs (i.e., Capaxone) Lovenox Insulin Pumps 8. Prescription Drug Expense Exclusions. [ Remove Exclusion “c.”] Plan Exclusions 7. Drugs/Infertility/Vitamins/Supplements. Medicines or drugs that can be purchased without a Physician's prescription; infertility drugs for persons under age 21 or older than age 44; or vitamins and supplements, including nutritional supplements or food products, whether or not obtainable by prescription. Exceptions: Diabetic drugs and Supplies; prenatal prescription vitamins; certain Aminoacidopathies formula, enteral formula or modified food products specifically shown as Covered Expenses. For Covered Persons, any age, Plan covers prescription infertility drugs used for treatment of other correctable medical conditions covered by the Plan even if that condition resulted in infertility. Jefferson Lewis et al School Employee’s Healthcare Plan Impact of Women’s Health /Infertility Insurance Laws 6