Review of Conscious Sedation Techniques in the Department of
advertisement
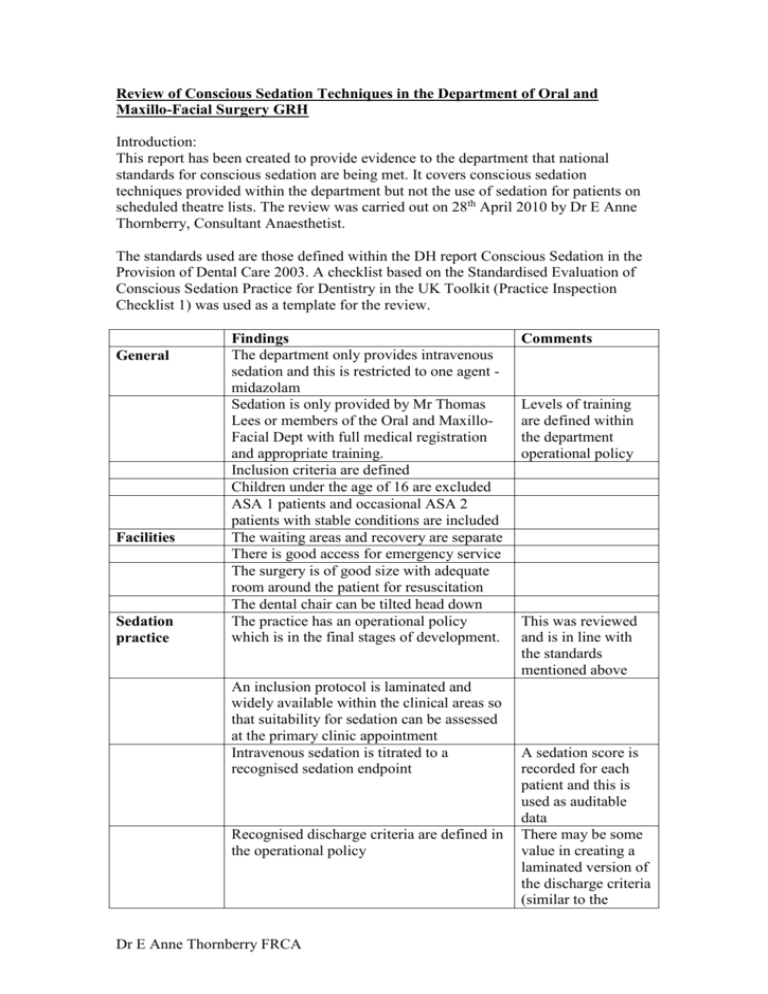
Review of Conscious Sedation Techniques in the Department of Oral and Maxillo-Facial Surgery GRH Introduction: This report has been created to provide evidence to the department that national standards for conscious sedation are being met. It covers conscious sedation techniques provided within the department but not the use of sedation for patients on scheduled theatre lists. The review was carried out on 28th April 2010 by Dr E Anne Thornberry, Consultant Anaesthetist. The standards used are those defined within the DH report Conscious Sedation in the Provision of Dental Care 2003. A checklist based on the Standardised Evaluation of Conscious Sedation Practice for Dentistry in the UK Toolkit (Practice Inspection Checklist 1) was used as a template for the review. General Facilities Sedation practice Findings The department only provides intravenous sedation and this is restricted to one agent midazolam Sedation is only provided by Mr Thomas Lees or members of the Oral and MaxilloFacial Dept with full medical registration and appropriate training. Inclusion criteria are defined Children under the age of 16 are excluded ASA 1 patients and occasional ASA 2 patients with stable conditions are included The waiting areas and recovery are separate There is good access for emergency service The surgery is of good size with adequate room around the patient for resuscitation The dental chair can be tilted head down The practice has an operational policy which is in the final stages of development. An inclusion protocol is laminated and widely available within the clinical areas so that suitability for sedation can be assessed at the primary clinic appointment Intravenous sedation is titrated to a recognised sedation endpoint Recognised discharge criteria are defined in the operational policy Dr E Anne Thornberry FRCA Comments Levels of training are defined within the department operational policy This was reviewed and is in line with the standards mentioned above A sedation score is recorded for each patient and this is used as auditable data There may be some value in creating a laminated version of the discharge criteria (similar to the inclusion protocol) and displaying it in the recovery area to provide consistency if temporary recovery staff are required to work in the department. The patients are seen by the surgeon involved before discharge All patients are provided with emergency contact information which is also provided to their escorts All patients have an escort Documentation Written information about preoperative preparation and post-operative expectations are given to the patient in the first clinic appointment when a decision is made for sedation A pre-operative check list is completed by nursing staff immediately prior to the procedure Specific post-operative instructions are given to the patient after the procedure and explained to the escorting adult. A 2 sided proforma is used to record medical and dental history, dental treatment required, pre-operative and intra-operative vital signs, site of IV cannulation, drug therapy given and dental treatment completed Consent is obtained and recorded using the generic Trust consent form The patients are monitored throughout using Details of IV an NIBP and pulse oximeter sedation techniques The equipment is regularly serviced and the service is up to date Supplementary oxygen is given during the procedure via nasal cannulae and piped oxygen There is a backup supply of O2 in a cylinder Piped suction is available with a backup It may be worth electrical suction considering a portable/battery suction pump in case of a need to evacuate a patient A full Trust resuscitation trolley complete Dr E Anne Thornberry FRCA Drugs Support staff with self-inflating bag, AED and emergency drugs is present in recovery and easily accessible from the surgery. Drugs are in date and regularly checked by staff and the Trust pharmacist. The only sedative used is midazolam 1 mg/ml Flumazenil is available Appropriate labels are available Some nurses have completed the National Reported verbally – Course for Sedation for Dental Nurses evidence not inspected All staff complete mandatory BLS training Reported verbally – annually evidence not inspected The patients are recovered by one of two nurses who are trained theatre nurses with recovery competences A review of the individual practice of Mr Thomas Lees was carried out at his request to support his appraisal Thomas Lees Name Qualifications BDS MFDS Intravenous sedation Conscious sedation techniques used 2-3/week therefore approximately 100 - 150 Log book seen Number of sedation cases carried out per annum 1 day theory update at the Eastman 2009 Verbal report – Training SAAD course evidence not specific to ALS – 4 year cycle inspected conscious BLS annually sedation/CPD Up to date with personal reading of current guidelines and standards Does not provide sedation for children Children under 16 Treats ASA 1 and occasional stable ASA 2 ASA grades patients e.g. stable asthmatics. Keeps a logbook of cases including details Problems of Clinical of sedation scoring; assessment of operating acquiring patient Governance conditions; quality of recovery of patients feedback discussed. Evidence of auditing records and presenting Suggest prospective to department. requests for feedback would be simpler than retrospective. Dr E Anne Thornberry FRCA Conclusions: The department has developed a robust operational policy, which complies with all the mandatory and recommended national standards for intravenous conscious sedation in dentistry. My brief inspection of current practice provided evidence that processes are in place to ensure that all these standards can be met and that these processes are being followed satisfactorily. The only minor exception is that portable suction is not available for use in the rare event of having to evacuate a patient, whilst still sedated. Dr E Anne Thornberry FRCA





![[Appendix C]](http://s3.studylib.net/store/data/005840900_1-2a6d1af025bed06052ca365eccd16150-300x300.png)