Bacterial infections are a major cause of morbidity and
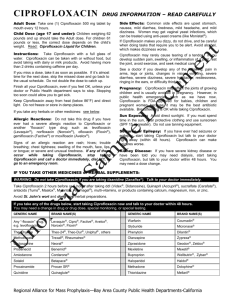
advertisement

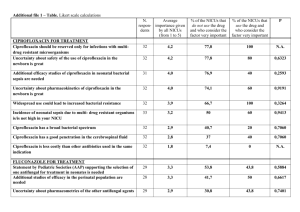
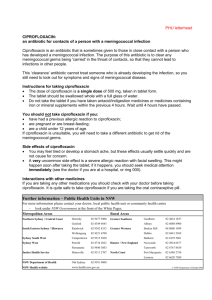
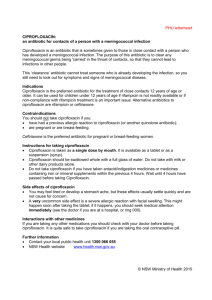
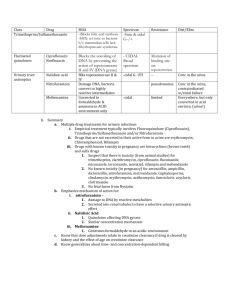
THE IMPACT OF PROPHYLACTIC CIPROFLOXACIN ON INFECTIVE OR FEBRILE EPISODES IN PATIENTS UNDERGOING AUTOLOGOUS STEM CELL TRANSPLANT Emma Crocombe, Julie Blundell and Adewale Adeyemo. Department of Pharmacy and Haematology, Royal Cornwall Hospital, Truro. Introduction Bacterial infections are a major cause of morbidity and mortality in patients following autologous stem cell transplant. Antibiotic prophylaxis started at the time of chemotherapy may reduce infection-related mortality, febrile episodes and bacteraemia1,2. In our hospital oral ciprofloxacin is used for prophylaxis in myeloma and lymphoma patients post-autologous stem cell transplant. This antibiotic has been associated with selecting resistant organisms; with Clostridium difficile-associated diarrhoea (CDAD) and has been linked to the rising incidence of methicillin-resistant Staphylococcus aureus (MRSA) infections3,4. Furthermore it has been our impression that many patients still require intravenous antibiotics. Aim To determine whether the administration of prophylactic ciprofloxacin had any effect on subsequent infective or febrile episodes in patients following autologous stem-cell transplant. Method We did a retrospective study of the last 22 patients undergoing autologous stem-cell transplant in our hospital. We reviewed hospital notes and drug charts to establish the duration of ciprofloxacin therapy and whether patients required intravenous antibiotics. We checked microbiology results for positive blood cultures and antibiotic sensitivities of isolates. Results Twenty of the twenty-two patients became pyrexial and alternative intravenous antibiotics were started. Two patients remained on ciprofloxacin and did not require any other antibiotics. There were eleven positive blood cultures: nine coagulase negative staphylococci, one methicillin-resistant Staphylococcus, and one Stenotrophomonas spp. Five of the isolates were resistant to ciprofloxacin. One patient developed CDAD. Conclusion This study suggests ciprofloxacin prophylaxis may not reduce the number of febrile incidents. It does not prevent coagulase negative staphylococcal bacteraemia and resistant strains, including MRSA may be selected. There may be a lower incidence of gramnegative sepsis but resistant strains may be a problem. We may now reconsider our policy of routine ciprofloxacin prophylaxis in this patient group. REFERENCES 1. Gafter-Gvili A, Fraser A, Paul M and Leibovici L. Meta-analysis: Antibiotic prophylaxis reduces mortality in neutropenic patients. Ann Intern Med 2005; 142: 979-995. 2. Krupova Y, Novotny J, Sabo A, Mateicka F and Krcmery V. Aetiology, cost of antimicrobial therapy and outcome in neutropenic patients who developed bacteraemia during antimicrobial prophylaxis: a case-control study. Int J Antimicrob Agents 1998; 10: 313-316. 3. Gafter-Gvili A, Paul M, Fraser A and Leibovici L. Effect of quinolone prophylaxis in afebrile neutropenic patients on microbial resistance: systematic review and meta-analysis. J Antimicrob Chemother 2007; 59: 5-22. 4. ME, Harris AD, Perencevich E, Roghmann M-C. Fluoroquinolone use and Clostridium difficile-associated diarrhea. Emerg Infect Dis 2003; 9(6). Available from: URL: http://www.cdc.gov/ncidod/EID/vol9no6/02-0385.htm THE IMPACT OF PROPHYLACTIC CIPROFLOXACIN ON INFECTIVE OR FEBRILE EPISODES IN PATIENTS UNDERGOING AUTOLOGOUS STEM CELL TRANSPLANT Emma Crocombe, Julie Blundell and Adewale Adeyemo. Department of Pharmacy and Haematology, Royal Cornwall Hospital, Truro. Emma Crocombe Pharmacy Department Royal Cornwall Hospital Truro TR1 3LJ Telephone: 01872 252984 Fax: 01872 223438 Email: emma.crocombe@rcht.cornwall.nhs.uk