Skill 4. Blood Pressure - Delmar Cengage Learning
advertisement
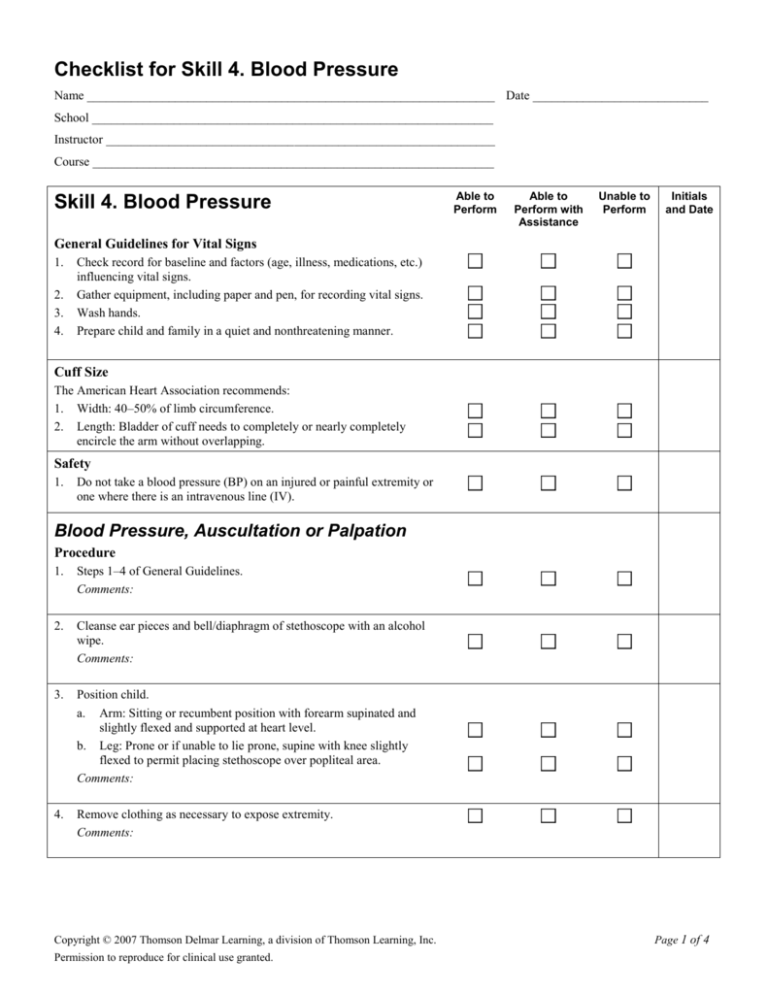
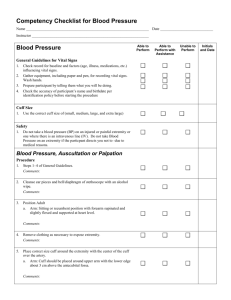
Checklist for Skill 4. Blood Pressure Name _________________________________________________________________ Date ____________________________ School ________________________________________________________________ Instructor ______________________________________________________________ Course ________________________________________________________________ Skill 4. Blood Pressure Able to Perform Able to Perform with Assistance Unable to Perform Initials and Date General Guidelines for Vital Signs 1. 2. 3. 4. Check record for baseline and factors (age, illness, medications, etc.) influencing vital signs. Gather equipment, including paper and pen, for recording vital signs. Wash hands. Prepare child and family in a quiet and nonthreatening manner. Cuff Size The American Heart Association recommends: 1. Width: 40–50% of limb circumference. 2. Length: Bladder of cuff needs to completely or nearly completely encircle the arm without overlapping. Safety 1. Do not take a blood pressure (BP) on an injured or painful extremity or one where there is an intravenous line (IV). Blood Pressure, Auscultation or Palpation Procedure 1. Steps 1–4 of General Guidelines. Comments: 2. Cleanse ear pieces and bell/diaphragm of stethoscope with an alcohol wipe. Comments: 3. Position child. a. Arm: Sitting or recumbent position with forearm supinated and slightly flexed and supported at heart level. b. Leg: Prone or if unable to lie prone, supine with knee slightly flexed to permit placing stethoscope over popliteal area. Comments: 4. Remove clothing as necessary to expose extremity. Comments: Copyright © 2007 Thomson Delmar Learning, a division of Thomson Learning, Inc. Permission to reproduce for clinical use granted. Page 1 of 4 Skill 4. Blood Pressure 5. Place correct size cuff around the extremity with the center of the bladder cuff over the artery. a. Arm: Cuff should be placed around upper arm with the lower edge about 3 cm above the antecubital fossa. b. Leg: Cuff should be placed around the mid thigh with the lower edge about 2 cm above the popliteal space. Comments: 6. Locate the artery by palpation. Comments: 7. Palpate a pulse distal to the cuff, e.g., brachial or radial. Close air valve and rapidly inflate cuff to 30 mm Hg above where pulse no longer felt or above expected systolic blood pressure. Comments: Able to Perform Able to Perform with Assistance Unable to Perform Initials and Date 8. Place stethoscope gently over artery. NOTE: To obtain a blood pressure reading by palpation, keep fingers on a distal pulse. Comments: 9. Open the valve and slowly release the air, permitting the pressure to drop 2–3 mm Hg per heart beat while auscultating for BP sounds or palpating for a pulse. NOTE: Do not reinflate cuff without letting cuff totally deflate. Comments: 10. Obtain a blood pressure reading. a. Auscultation. 1. Systolic pressure: The pressure at which you first hear sounds. 2. Diastolic pressure: The American Heart Association recommends the onset of muffling as the diastolic pressure in children up to 13 years of age; the pressure when sounds become inaudible is the diastolic pressure in children > 13 years of age. b. Palpation: Continue to slowly release pressure until a pulse is felt. This is the systolic pressure. The diastolic pressure is recorded as P, e.g., 100/P. The systolic pressure obtained by palpation is 5–10 mm Hg lower than that obtained by auscultation. NOTE: If using a mercury manometer read at eye level. Comments: 11. Do not leave the cuff inflated for a prolonged period. Comments: 12. Deflate the cuff rapidly and completely and remove from the arm. Comments: Copyright © 2007 Thomson Delmar Learning, a division of Thomson Learning, Inc. Permission to reproduce for clinical use granted. Page 2 of 4 Skill 4. Blood Pressure Able to Perform Able to Perform with Assistance Unable to Perform Initials and Date 13. Wait 2 minutes before taking another blood pressure. Comments: Blood Pressure, Electronic Procedure 1. Steps 1–4 of General Guidelines. Comments: 2. Set up machine according to instructions: a. Plug in monitor/machine. b. Connect dual air hose to back of monitor. c. Connect correct size cuff by screwing the pressure cuff’s tubing into the other end of the air hose. Comments: 3. Place cuff. (See step 5 of Blood Pressure, Auscultation or Palpation.) Comments: 4. Turn machine on and follow manufacturer’s instructions. Comments: 5. Obtain reading. Comments: 6. Remove cuff. Comments: Blood Pressure, Flush Flush is used to obtain a BP reading on a newborn or small infant when BP difficult or impossible to obtain by other means. Procedure 1. Place infant in a recumbent position. Comments: 2. Apply cuff snugly and smoothly to distal arm, with outer edge at the wrist or to the distal leg with the outer edge at the ankle. Comments: 3. Elevate extremity above heart level. Comments: 4. Wrap the extremity distal to the cuff with an elastic bandage. Begin with the finger or toes and progress to the edge of the cuff. Comments: Copyright © 2007 Thomson Delmar Learning, a division of Thomson Learning, Inc. Permission to reproduce for clinical use granted. Page 3 of 4 Skill 4. Blood Pressure 5. Inflate the cuff to 150–200 mm Hg. Comments: 6. Remove elastic bandage. The hand or foot should appear pale in color and exsanguinated. Comments: 7. Lower the pressure in the cuff by 5 mm Hg and leave there for 3–4 seconds. Repeat process until flushing observed in the pale extremity, i.e., a sudden pink color appears below the edge of the cuff and spreads distally. Comments: 8. Reading is taken at point flushing appears. This is the mean arterial pressure. To be accurate, an assistant is needed to observe for flushing while you monitor the pressure gauge. Comments: 9. Repeat the procedure at least twice to confirm the reading. Comments: Able to Perform Able to Perform with Assistance Unable to Perform Initials and Date Documentation 1. 2. 3. 4. 5. Blood pressure reading. Method used. Site. Size of cuff. Who notified if findings of concern. Comments: Copyright © 2007 Thomson Delmar Learning, a division of Thomson Learning, Inc. Permission to reproduce for clinical use granted. Page 4 of 4