Blue Box Stuff from Moore
advertisement

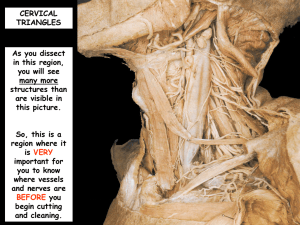
Blue Box Stuff from Moore The Head The pterion is at the lateral side of the skull, at the intersection of the frontal, parietal, sphenoid, and temporal bones. When the lateral side of the skull is fractured, the middle meningeal a. is ruptured, causing an epidural hematoma. The meningeal a. is on the interior side of the skull. The inferior alveolar branch of V3 enters the mandible through the mandibular foramen. It then becomes the mental nerve when it exits the mental foramen in the front of the mandible. The muscles of the face are innervated by the facial nerve. VII also innervates the posterior belly of the digastric and the stylohyoid. The buccal branch of VII innervates most of the facial muscles. VII lesions create paralysis of one side – they cannot close their lips [loss of buccal nerve] and close their eyelids [loss of temporal nerve]; the lacrimal glands do not work and they drool [due to paralysis of the orbicularis oris]; nor can they whistle or chew. Taste sensation in the anterior two thirds of the tongue is lost [loss of the chorda tympani branch of CN VII]. The posterior two thirds of the tongue receives taste fibers from the lingual branch of CN IX. VII supplies sensory innervation to the anterior two thirds of the tongue through its chorda tympani branch. It also runs through the parotid gland as it exits the stylomastoid foramen. The temporal branch supplies innervation to the frontalis muscle and the orbicularis oculi. The zygomatic supplies muscles to the zygomatic and infraorbital regions. The buccal branches supply muscles of the mouth and maxilla. The mandibular branch supplies muscles of the lower lip and chin, and the cervical branch supplies the platysma. V3 is the only branch of the trigeminal which carries motor fibers to the muscles of mastication, along with the mylohyoid and the anterior belly of the digastric. The other two branches are solely sensory. V1: Lacrimal, Supraorbital, Supratrochlear, Infratrochlear, anterior and posterior ethmoidal nerves. V2: Infraorbital, Zygomaticotemporal, Zygomaticofacial. V3: Auriculotemporal, Lingual, Buccal, Inferior Alveolar / Mental, Deep Temporal, Masseteric, Pterygoid, Mylohyoid. The inferior alveolar nerve may be damaged when the mandible is broken. The facial vein drains into the anterior jugular vein, but it also drains the cavernous sinus of the brain. Infections of the nose and upper lip and spread to the cavernous sinus through retrograde flow of blood up the vein. Lymph nodes of the head and neck: retroauricular, deep and superficial cervical, jugular-omohyoid, submandibular, submental, occipital, parotid, buccal, retropharyngeal [behind the roof of the mouth], jugulodigastric, and infrahyoid. The superficial cervical nodes lie alongside the external jugular vein. The rest drain structures of the scalp, face, and forehead. The medial portion of the lip, the tongue, and the floor of the mouth are drained by the submental lymph nodes. The submandibular lymph nodes drain the lateral portion of the lip. Efferent lymph vessels from the submental enter the submandibular, whose efferents enter the jugularomohyoid nodes. Infections in the scalp cannot spread posteriorly due to attachments of the occipitalis muscle to the superior nuchal ridge, nor can they spread laterally due to temporal fascia adherent to the zygomatic arch. They can, however, spread into the eyelids and root of the nose because the frontalis muscle attaches to skin and not fascia. When pressure in the compartment superior to the tentorium cerebelli exceeds that of the inferior compartment, the temporal lobe of the brain may be forced through the tentorial incisure, causing damage to that area. V, X, XII, C1-3 contribute sensory innervation to the dura. Intercranial bleeding: 1) Epidural hematoma. Caused by bleeding between the dura and the internal periosteum of the calvaria. Patient will have hit head, been lucid for several hours, then as pressure builds upon the brain, will lapse into a coma. Temporal lobe damage may occur as described above. 2) Subdural hematoma. Bleeding within the pericranium and the nervous dura, not underneath it. 3) Subarachnoid hemorrhage. Occurs with rupture of an intercranial artery. Patient presents with severe headache, stiff neck, and maybe loss of consciousness. Examination of the eye will reveal subhyaloid hemorrages between the retina and vitreous humor of the eye. Lumbar punctures will reveal blood in the CSF. 4) Intracerebral hemorrhage. Caused by rupture of an artery supplying the brain, often the middle cerebral artery. Paralysis often occurs when this artery ruptures because the motor cortex loses blood supply during a CVA. Bruising or bleeding of the brain results in swelling, and can result in loss of consciousness. Swelling may cause herniation of the cerebellum through the foramen magnum, compressing the midbrain and disturbing regulation of basic processes and perhaps death. Since the basilar and occipital sinuses have no valves, infections or cancerous cells can spread from the chest / abdominal cavity to the brain by way of the vertebral veins. Blood clots can also reach the brain from those areas without ever reaching the heart or lungs by running through the internal thoracic vein into the subclavian and then the vertebral veins. The cavernous sinus envelops the internal carotid, along with CN III, IV, V1, V2, and VI. If swelling compresses the cavernous sinus, these nerves are likely to be compressed as well, leading to paralysis of the lens and iris. (“Pupils fixed and dilated” – loss of ciliary nerve function). Damage to CN III not only impairs pupillary reflexes, but motor function to the superior, inferior, medial recti, and the inferior oblique but also to the levator palpebrae superiori. Thus the eyelid will droop (ptosis) in one with “third nerve palsy.” A gunshot wound to the eye will probably penetrate either inferiorly to the maxillary sinus, or superiorly into the middle cranial fossa and the temporal lobe of the brain. The meningeal layers extends up to the attachment of the eyeball. Increase in CSF pressure slows venous return, causing papilledema. Damage to the cervical sympathetic trunk can cause ptosis. To distinguish this from CN III, one must examine for the presence of the pupillary reflex. Paralysis of one or more extraocular muscles causes double vision. An aneurysm of the internal carotid can compress the optic nerve and cause ipsilateral (same side) loss of vision. There is partial decussation of nerve fibers at the optic chiasma. Only half of the nerve fibers branch off to the contralateral side. The Neck Posterior triangle: trapezius laterally, sternocleidomastoid medially, clavicle inferiorly. Superficially, it is covered by fascia and skin, while deep it is lined with a fascial carpet of fascia derived from the splenius capitis, levator scapulae, middle scalene, and posterior scalene. It contains the external jugular vein, part of the subclavian artery prior to entering the carotid sheath, CN XI, and the nerves of the cervical plexus. The subclavian artery gives off the thyrocervical trunk, which branches into the inferior thyroid a., the suprascapular a. [inferolateral] and the transverse cervical a. [superficially across the posterior triangle to scapular muscles]. The roots and divisions of the brachial plexus are also located in this triangle, and may be damaged in a stab wound to the shoulder area. The triangle is drained by the superficial cervical nodes, which then are drained by the supraclavicular nodes. This triangle is divided into the supraclavicular / subclavian triangle, bounded by the same two muscles medially and laterally, by the omohyoid superiorly, and the clavicle inferiorly, and the occipital triangle, bounded inferiorly by the omohyoid. XI crosses the occipital triangle. Heart failure raises venous blood pressure, causing the external jugular vein to be prominent over its entire course along the neck. This vein does not collapse due to attachment to the fascial carpet, which can create right side failure if air enters the vein if it is ruptured. Anterior triangle: This contains the strap muscles of the neck and the anterior jugular vein.. The carotid sheath, lies within this triangle, contains the internal jugular vein, the common carotid, CN X, and the ansa cervicalis. This sheath can also contain the deep cervical lymph nodes. Triangle is subdivided into the submandibular triangle, which contains the submandibular gland and lymph nodes, the mylohyoid, Wharton’s duct, and CN XII. The submental triangle contains the mylohyoid, its lymph nodes, The superior belly of the omohyoid, the posterior belly of the digastric, and the anterior border of the sternocleidomastoid bound carotid triangle. Within this triangle lies the carotid sheath, with the bifurcation of the common carotid at around C5. The carotid sinus is approximately at this level and is innervated by CN IX. The carotid sinus reacts to changes in blood pressure, while the carotid body is a chemoreceptor and detects levels of oxygen and carbon dioxide in the blood. CN IX also supplies it, along with branches from CN X. It forces us to breathe when arterial carbon dioxide levels are too high. The ansa cervicalis lies at about this level. The submental triangle contains the two mylohyoids, along with its lymph nodes. Veins in this area coalesce to form the paired anterior jugular veins. Mitral valve stenosis can result in elevated venous blood pressure, causing palpable venous pulses on the internal jugular vein. Flexors of the neck include the longus colli, longus capitis, rectus capitis anterior, rectus capitis lateralis. These are just anterior to the cervical spinal column. The former two lie along the length of the neck, with the longus colli being medial and the capitis being lateral. The latter two extend only from the occipital bone to the transverse process of the atlas. As their names imply, the lateralis is lateral, while the anterior is anterior. The cervical sympathetic chain runs just anterior to the longus colli muscle, posterior to the trachea and esophagus. The phrenic nerve runs anterior to the scalene anterior. It crosses the 1 st part of the subclavian a. on the left side, but the 2nd part of the subclavian a. over the scalene anterior on the right side. It is deep to prevertebral fascia. Preganglionic fibers synapse in the cervical sympathetic ganglia (inferior / stellate, vertebral, middle, and superior) and the postganglionic fibers exit the ganglia. The inferior ganglion is usually wrapped around the vertebral artery and may be fused to the first thoracic ganglion. Its postganglionic fibers go to the heart and to the vertebral plexus around the artery. The middle ganglion lies on the anterior aspect of the inferior thyroid artery. Its postganglionic fibers pass to the heart and the thyroid. The superior cervical ganglion is located at the level of the atlas and axis and is pretty good sized. It sends fibers to the cranial cavity, to the external carotid and the superior four cervical nerves. Severing this trunk eliminates sympathetic activity in the face and head. Most notably, Horner’s syndrome arises and presents with ptosis [paralysis of smooth muscle of levator palpebrae superiori], pupillary constriction [no sympathetic opposition to constriction], sinking of eye [partial paralysis of orbitalis muscle], vasodilation and lack of sweating in the face [no sympathetic innervation of sweat glands and capillaries]. Cancer from the thorax and abdomen can spread to the deep cervical lymph nodes and supraclavicular nodes. Thus, these lymph nodes are referred to as ‘sentinel’ lymph nodes. Tracheotomies are made midway between the laryngeal prominence and the jugular notch. The inferior thyroid veins (drain into brachiocephalics … the superior and middle thyroid vv. drain into the internal jugular v.), the left brachiocephalic vein, jugular venous arch, and pleurae can be damaged if the tracheotomy is made incorrectly. The thyroid is drained by prelaryngeal, pretracheal, then paratracheal lymph nodes, and innervated by the cervical sympathetic chain. Thyroidectomy can damage the recurrent laryngeal nerves or the external laryngeal nerves, and result in abolishment of speech / phonation. Accidental removal of the parathyroids can result in lack of serum calcium, resulting in muscle tetany. Fascial planes Investing fascia attaches to the superior nuchal line, the zygomatic arch, the inferior border of the mandible, and inferiorly to the anterior and posterior sides of manubrium of the sternum and the clavicles. Infections tend to be localized in this fascia, although they can pass to the mediastinum if it reaches the suprasternal space [between the two layers of investing fascia at the manubrium]. Pretracheal fascia – spread inferiorly to esophagus and posterior mediastinum. Also anterior to trachea and anterior mediastinum. Air can enter the neck if a slit in oral mucosa is made … this results in swelling of the neck area. Prevertebral fascia – fuses with anterior longitudinal ligament. The axillary sheath arises from this fascia. The pharynx The pharyngeal wall is composed of five layers: from anterior to posterior, the mucous membrane, the submucosa, the pharyngeal-basilar fascia, the muscular layer, and the buccopharyngeal fascia. The retropharyngeal space lies between the buccopharyngeal fascia and the prevertebral fascia. The pharyngeal constrictors are innervated by pharyngeal and superior laryngeal branches of CN X, as are the palatopharyngeus (hard palate to thyroid cartilage, just lateral to the midline raphe) and the salpingopharyngeus (from auditory tube to palatopharyngeus … it’s really thin). The stylopharyngeus is innervated by CN IX, and enters the muscular layer of the pharynx between superior and middle constrictors. The function of the latter three muscles is to elevate the larynx / pharynx during swallowing and speaking. The auditory tube opens at the nasal / nasopharyngeal junction. It runs superoinferiorly, opening just below a mucosal fold called the torus. The torus continues inferiorly into the salpingopharyngeal fold. On the superior border of the nasopharynx is the pharyngeal tonsil (adenoids when enlarged). The jugulodigastric lymph nodes enlarge when the tonsils become infected. During a (palatine) tonsillectomy, the structures in danger of being damaged include CN IX, on the lateral wall of the tonsil, the lingual nerve (CN V3 and VII) at the anterior of the tonsil, or the internal carotid. Bleeding from either the external palatine vein or the tonsillar artery causes hemorrhage during a tonsillectomy. Severe bleeding can be stopped by compression of the external carotid, which supplies the carotid. The external palatine vein descends from the soft palate and runs on the lateral surface of the tonsil. Foreign bodies that become lodged in the pharynx lodge in the piriform recesses on either side of the cricoid cartilage. If they pierce the pharynx, they can damage the internal laryngeal nerve, causing numbness of the laryngeal mucous membrane at the level of the vocal cords. Damage to the recurrent laryngeal nerves not only causes hoarseness / loss of speech, but also paralysis of the muscles of the epiglottic folds. This results in incomplete closure of the epiglottis over the tracheal aditus during swallowing. Thyroglossal cysts arise from the thyroglossal duct, the path the thyroid took when descending into the neck, and are generally along the midline, anywhere between the tongue and thyroid cartilage. Extrusion of the tongue will draw the cyst superiorly because the duct lies, in part, within the tongue and opens at the foramen cecum. An opening in the cyst into the neck is called a thyroglossal fistula. Branchial cysts are derived from the failure of the cervical sinus, second branchial groove, or second pharyngeal pouch to close during embryonic development. These cysts usually lie in the submandibular triangle, on the lateral side below the ear. Removal of these cysts can potentially damage the hypoglossal nerve (CN XII), which runs alongside the mandibular angle. This results in unilateral paralysis of the tongue, which presents as unilateral atrophy and deviation of the tongue towards the paralyzed side when extruded. A thyroid tumor moves up and down during swallowing because the prethyroid fascia is drawn superiorly during deglutition. Displacement of both recurrent and superior laryngeal nerves can occur as a result, creating hoarseness or loss of speech. The pain of an earache is carried by sensory fibers from CN IX, the tympanic branch.