Clinical factors influencing clinicians` decision to treat tuberculosis in
advertisement
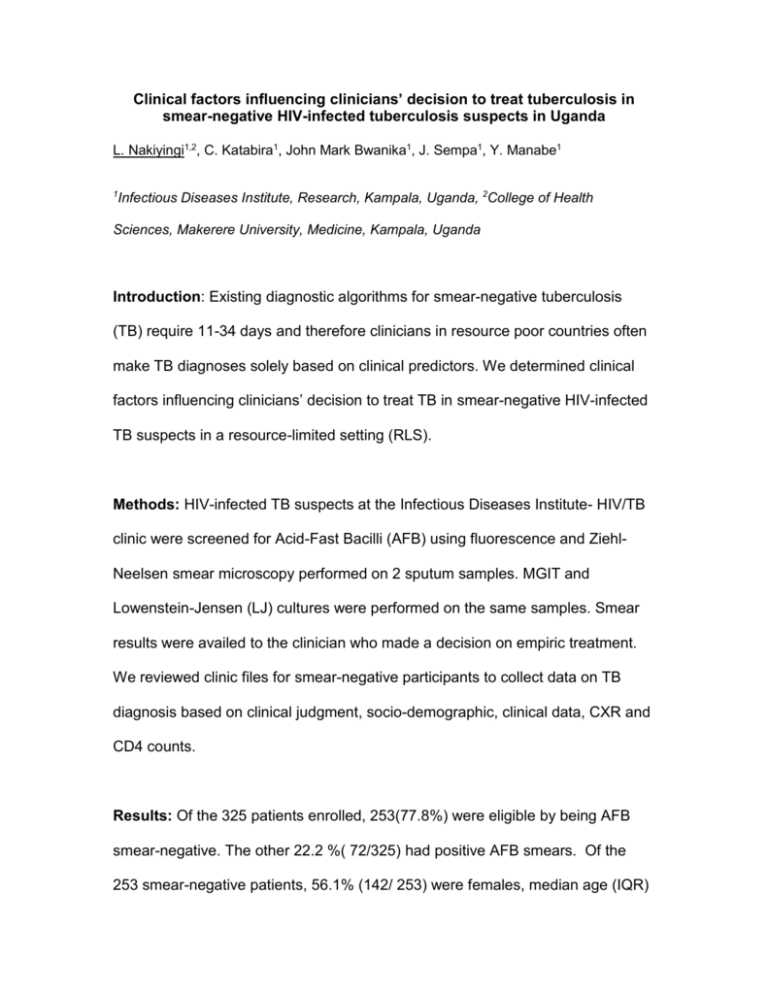
Clinical factors influencing clinicians’ decision to treat tuberculosis in smear-negative HIV-infected tuberculosis suspects in Uganda L. Nakiyingi1,2, C. Katabira1, John Mark Bwanika1, J. Sempa1, Y. Manabe1 1 Infectious Diseases Institute, Research, Kampala, Uganda, 2College of Health Sciences, Makerere University, Medicine, Kampala, Uganda Introduction: Existing diagnostic algorithms for smear-negative tuberculosis (TB) require 11-34 days and therefore clinicians in resource poor countries often make TB diagnoses solely based on clinical predictors. We determined clinical factors influencing clinicians’ decision to treat TB in smear-negative HIV-infected TB suspects in a resource-limited setting (RLS). Methods: HIV-infected TB suspects at the Infectious Diseases Institute- HIV/TB clinic were screened for Acid-Fast Bacilli (AFB) using fluorescence and ZiehlNeelsen smear microscopy performed on 2 sputum samples. MGIT and Lowenstein-Jensen (LJ) cultures were performed on the same samples. Smear results were availed to the clinician who made a decision on empiric treatment. We reviewed clinic files for smear-negative participants to collect data on TB diagnosis based on clinical judgment, socio-demographic, clinical data, CXR and CD4 counts. Results: Of the 325 patients enrolled, 253(77.8%) were eligible by being AFB smear-negative. The other 22.2 %( 72/325) had positive AFB smears. Of the 253 smear-negative patients, 56.1% (142/ 253) were females, median age (IQR) 38 (31- 44) years and median CD4 (IQR) 291(150 -482) cells/mm3. 85/253 (33.6%) were treated for TB based on clinical judgment while 168(66.4%) were not treated. 30(35.3%) of the 85 patients that were treated for TB turned out culture positive while 18(10.7%) of the I68 that were not treated turned out culture positive. On multivariate analysis, abnormal CXR [P<0.001,OR 12.8, 95% CI (3.40-48.46)] and advanced HIV clinical stage [ P=0.036, OR 4.05, 95% CI (1.09-15.02)] were significantly associated with clinical decision to treat for TB in smear-negative HIV-infected patients. The sensitivity and specificity of clinical judgment was 62.5% and 73.7% respectively when compared to sputum culture. Conclusion In RLS, CXR findings and severity of HIV significantly influence clinical decision to treat for TB in smear-negative HIV-infected patients. However, the accuracy of clinical judgment is poor. Accurate, rapid, point-of-care diagnostics are needed.